Abstract
Background:
Postoperative sore throat (POST) is a known complication following general anesthesia requiring endotracheal intubation. Its incidence ranges from 21% to 65% and remains the eighth most undesirable postoperative event. Various measures have been tried to decrease the incidence of sore throat with various success rates.
Aim:
This study aimed at reducing the incidence of POST with ketamine and magnesium sulfate nebulization.
Settings and Design:
This study is a prospective randomized, double-blinded study.
Materials and Methods:
After Institutional Ethics Committee approval and written informed consent, 80 patients who fulfilled the inclusion and exclusion criteria were randomly divided into two groups to receive magnesium sulfate 250 mg in 5 ml saline in Group A and ketamine 50 mg in 5 ml saline nebulization in Group B before the start of general anesthesia. All patients received standard anesthesia protocol. After extubation, all patients were enquired about the incidence and severity of sore throat at 0, 2, 4, 6, and 24 h.
Statistical Analysis Used:
Paired t-test and Wilcoxon signed-rank test were used to compare hemodynamic variables and Chi-square test to compare the incidence and severity of sore throat.
Results:
There were no differences in the demographic profile, duration of laryngoscopy, time taken to intubate, and duration of surgery between the two groups. The incidence and severity of sore throat were significantly decreased in ketamine group at 4 and 6 h when compared to magnesium sulfate group.
Conclusion:
Nebulization with ketamine 50 mg significantly decreases the incidence of POST when compared to magnesium sulfate 250 mg.
Keywords: Endotracheal intubation, general anesthesia, ketamine, magnesium sulfate, nebulization, postoperative sore throat
INTRODUCTION
Postoperative sore throat (POST) is a common occurrence following general anesthesia with endotracheal intubation although clinicians often regard it as a minor complication. The incidence of POST is estimated to be 21%–65% in different studies.[1,2,3] Irritation and inflammation of the airway are considered to be the causes of POST.[4] Although considered a minor complication, it may cause a significant patient morbidity, dissatisfaction, and increased the length of hospital stay.
Various pharmacological and nonpharmacological methods have been tried to decrease the incidence of POST with varying success rates. Some of them include beclomethasone gel,[4] magnesium sulfate gargle,[5] ketamine gargle,[5,6,7] ketamine nebulization,[8,9] magnesium sulfate nebulization,[8,10] lidocaine spray,[11] smaller size endotracheal tubes, minimizing cuff pressure to <20 mmHg,[12] and minimizing laryngoscopy attempts.
Among the interventions, the use of ketamine gargle or lozenges has the highest success rates.[5,6,7] The problem with gargle or lozenges is the bitter taste of the drug and the risk of aspiration while gargling which may lead to serious complications. Hence, the administration of the drug through aerosol route gained popularity among anesthesiologists with good acceptance from the patients.
It is known that N-methyl-D-aspartate (NMDA) receptors have a role in nociception and inflammation.[13,14] NMDA receptors are found not only in the central nervous system but also in the peripheral nervous system and spinal cord. The antinociceptive and the anti-inflammatory properties of ketamine[6,7] and magnesium sulfate[13,14,15,16,17] with the available data suggest that both have a potential role in reducing POST. Hence, this study is aimed at using the aerosol route of magnesium sulfate and ketamine and to find its effectiveness in preventing POST.
MATERIALS AND METHODS
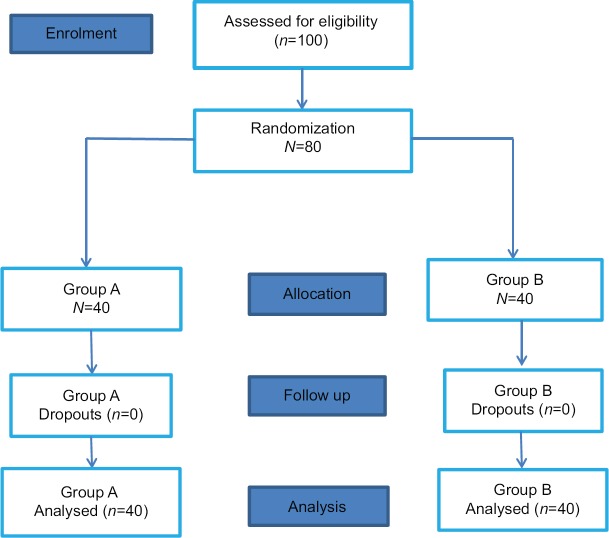
After Institutional Ethics Committee approval (IEC: RC/16/133 dated November 11, 2016); CTRI No. 2016/10/012497) and written informed consent, 80 patients with the American Society of Anesthesiologists (ASA) physical status classes I or II of either sex, aged 18–65 years, requiring general anesthesia with endotracheal intubation for elective surgery are included in the study. Patients who fulfilled the inclusion criteria and do not have any exclusion criteria such as surgery involving the oral cavity, nasopharynx, larynx and neck regions, surgery requiring prone position, surgery lasting more than 3 h, history of preoperative sore throat, common cold, anticipated difficult airway, any known allergies to study drug, recent non steroidal anti-inflammatory drugs use and pregnant patients were randomly divided into two groups, Group A and Group B using computer-generated random numbers [Figure 1].
Figure 1.
Consort flowchart
This study was a prospective, randomized, double-blind, comparative study conducted from September 2016 to December 2017 in our institution. The sample size was calculated based on the assumption that the incidence of POST is 65% from previous studies and to show a 50% reduction in the incidence at α-error of 0.05 and power 80%, and we required a sample size of 35 patients per group. On assuming 10% loss of follow-up, the sample size required was estimated to be 40 patients per group.
All patients were kept fasting overnight and premedicated with oral alprazolam 0.5 mg and ranitidine 150 mg on the night before surgery and on the morning of surgery. On arrival to the operating room, all patients were secured an intravenous (IV) line with 18G cannula on nondominant hand, and maintenance IV fluids were started. ASA standard monitors such as electrocardiogram, pulse oximetry, noninvasive blood pressure monitoring, and capnography were attached, and baseline parameters such as heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and oxygen saturation were noted prenebulization, postnebulization, and preinduction. Before the start of general anesthesia, all patients received nebulization with the study drug with a wall-mounted oxygen source at 10 L/min (50 psi pressure). The study drug was prepared by an anesthetist who is not part of the study.
Group A received nebulization with 250 mg magnesium sulfate in 5 ml NS
Group B received nebulization with 50 mg ketamine in 5 ml NS.
After 15 min of nebulization, patients were induced with injection midazolam 0.02 mg/kg, injection fentanyl 2 μg/kg, and injection thiopentone 5 mg/kg after preoxygenation with 100% oxygen for 3 min through handheld face mask. Tracheal intubation was facilitated with injection vecuronium 0.1 mg/kg. All male patients were intubated with Portex polyvinyl chloride tubes of size 8.0–8.5 mm ID and female patients with 7.0–7.5 mm ID. The tracheal cuff was inflated with air, and cuff pressure was maintained at 20 cm H2O by handheld cuff pressure manometer and thereafter for every 30 min till the end of surgery. The duration of laryngoscopy and time taken to intubate were noted. More than two attempts for intubation and any traumatic intubation were excluded from the study. After confirmation of tracheal tube position, anesthesia was maintained with 50:50 mixture of N2O and O2, sevoflurane 1%–2%, and intermittent doses of fentanyl and vecuronium. Thirty minutes before the end of surgery injection emeset 4 mg IV and injection diclofenac aqueous 75 mg IV was given. At the completion of surgery, with the patient adequately anesthetized, the oropharynx was gently suctioned, and the sevoflurane and N2O were turned off. Inspiratory oxygen concentration was increased to 100%. The neuromuscular blockade was reversed with neostigmine 50 μg/kg and glycopyrrolate 10 μg/kg after the return of spontaneous ventilation. During extubation, if the patient had excessive bucking, IV lignocaine 1.5 mg/kg would have been administered as a rescue measure and patient would be excluded from the study. After extubation, patient was shifted to the postanesthesia care unit for observation, and patients were assessed regarding the incidence and severity of POST at 0 h. The incidence of POST was assessed from the patients by asking the presence or absence of soreness in the throat, and patients who experienced any degree of throat pain was considered as having sore throat. The severity of POST was assessed by a four-point scale (0–3) as follows:
0 = no sore throat
1 = mild sore throat (complains of sore throat only on asking)
2 = moderate sore throat (complains of sore throat on his/her own)
3 = severe sore throat (change of voice or hoarseness, associated with throat pain).
Thereafter, patients were assessed for incidence and severity of POST at 2, 4, 6, and 24 h. Any side effects such as a cough, nausea, and vomiting were also noted.
Statistical analysis
All the relevant patient data were entered in Microsoft Excel sheet and statistical analysis was done using SPSS version 20.0 (IBM Corp, Armonk, NY, USA). The demographic data were expressed as means and standard deviation. Duration of laryngoscopy, time taken to intubate, and duration of surgery were expressed as mean and standard deviation and significance were assessed using the Mann–Whitney test. The number of attempts to intubate was assessed using Chi-square test. The hemodynamic variables such as HR, SBP, and DBP were expressed as mean and standard deviation and significance were assessed using paired t-test and for SBP using Wilcoxon signed-rank test. The incidence and severity of sore throat significance were assessed using Chi-square test.
RESULTS
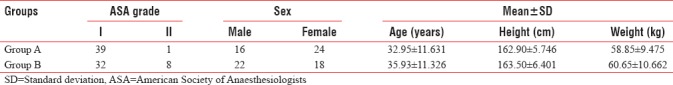
The distribution of demographic data between the two groups was comparable, and there were no significant differences [Table 1].
Table 1.
Distribution of demographic data among the groups
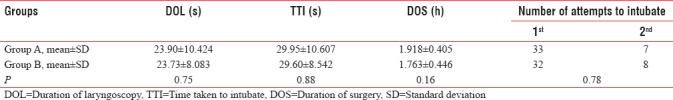
The duration of laryngoscopy, time taken to intubate, and the duration of surgery were 23.90 ± 10.424 s, 29.95 ± 10.607 s, and 1.92 ± 0.41 h in Group A and 23.73 ± 8.08 s, 29.60 ± 8.542 s, and 1.76 ± 0.45 h in Group B, respectively. In Group A, 33 patients were intubated in the first attempt and 7 patients in the second attempt, while in Group B, 32 patients in the first attempt and 8 patients in the second attempt. These values were comparable between the groups and it was not statistically significant (P > 0.05) [Table 2].
Table 2.
Comparison of duration of laryngoscopy, time taken to intubate, duration of surgery and number of attempts taken to intubate
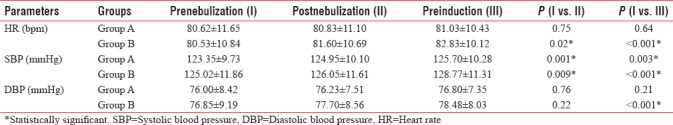
The hemodynamic parameters such as HR, SBP, and DBP during prenebulization were 80.62 ± 11.65 beats per minute (bpm), 123.35 ± 9.73 mmHg, and 76.00 ± 8.42 mmHg in Group A and 80.53 ± 10.84 bpm, 125.02 ± 11.86 mmHg, and 76.85 ± 9.19 mmHg in Group B, respectively. During postnebulization HR, SBP, and DBP were 80.83 ± 11.10 bpm, 124.95 ± 10.10 mmHg, and 76.23 ± 7.51 mmHg in Group A and 81.60 ± 10.69 bpm, 127.05 ± 11.61 mmHg, and 77.70 ± 8.56 mmHg in Group B, respectively. During preinduction the HR, SBP, and DBP were 81.03 ± 10.42 bpm, 125.70 ± 10.28 mmHg, and 76.80 ± 7.35 mmHg in Group A and 82.83 bpm, 128.27 ± 11.31 mmHg, and 78.48 ± 8.03 mmHg in Group B, respectively. There was statistically significant (P < 0.05) increase in HR and SBP in Group B when compared to Group A during postnebulization and preinduction comparing to prenebulization [Table 3].
Table 3.
Comparison of haemodynamic parameters during prenebulization, postnebulization and preinduction
The overall incidence of sore throat in Group A was 50% and in Group B was 25%. None of the patients complained of sore throat in both the groups in the immediate postoperative period at 0 h. In Group A, 4 patients and in Group B, 2 patients complained of sore throat at 2 h but not statistically significant (P = 0.154). At 4 h, 10 patients in Group A and 5 patients in Group B complained of sore throat and it was statistically significant (P = 0.013). At 6 h, 6 patients in Group A and 3 patients in Group B had sore throat, and it was statistically significant (P = 0.019). At 24 h, none of the patients in both the groups had sore throat [Figure 2].
Figure 2.
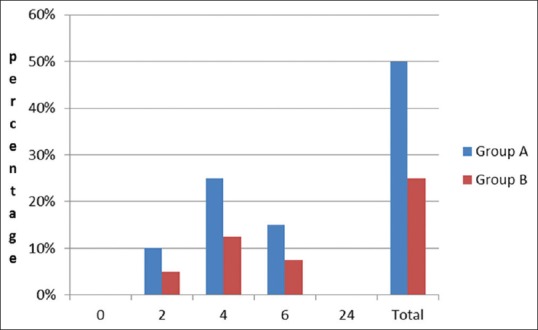
Incidence of sore throat among the two groups at different time intervals
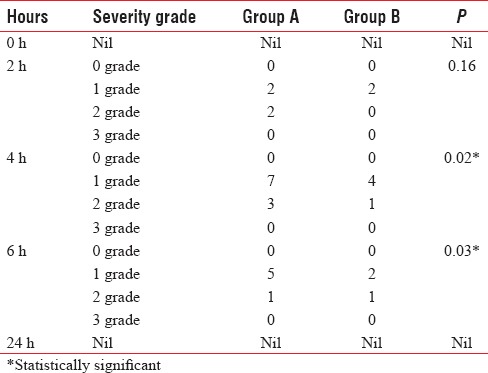
At 2 h, 2 patients in Group A and 2 patients in Group B had mild sore throat, while 2 patients in Group A had moderate sore throat (P = 0.160). At 4 h, 7 patients in Group A and 4 patients in Group B had mild sore throat while 3 patients in Group A and 1 patient in Group B had moderate sore throat (P = 0.020). At 6 h, 5 patients in Group A and 2 patients in Group B had mild sore throat, while 1 patient in Group A and 1 patient in Group B had moderate sore throat (P = 0.030). At 24 h, no patients had sore throat [Table 4].
Table 4.
Severity of sorethroat at different time intervals among the two groups
DISCUSSION
POST although a self-limiting complication following general anesthesia with endotracheal intubation, it continues to be an important concern for surgical patients. As perioperative physicians, we are entrusted with the deeds of decreasing the sufferings of surgical patients. When reviewing the literature for the prevention of POST, some nonpharmacological[12,18,19] and pharmacological interventions[4,5,6,7,8,9,10,11] have been tried with varying success rates. Nebulization is inexpensive, quick, convenient, and easy to administer also, which made this, the route of choice. In our study, we compared the effectiveness of ketamine and magnesium sulfate nebulization on POST.
A study done by Ahuja et al.[9] evaluated the effectiveness of nebulized ketamine on the severity of POST and concluded that ketamine nebulization significantly reduced the severity of POST at 4 h which is comparable to our study where the incidence and severity of POST were significantly lower in ketamine group at 4 and 6 h. A similar study also conducted by Aditya et al.[20] and found that ketamine nebulization significantly reduced the incidence and severity of POST in immediate postoperative period.
Yadav et al.[10] evaluated the effect of magnesium sulfate nebulization on POST at rest and swallowing and found that it significantly decreased the incidence of POST at 4 and 24 h. Borazan et al.[17] also conducted a similar study with magnesium sulfate lozenges and found that it significantly reduced the incidence and severity of POST. In our study, the incidence and severity of POST in the magnesium sulfate group were also decreased but not statistically significant when compared to ketamine group.
On comparing ketamine nebulization with magnesium sulfate nebulization in our study on the incidence and severity of POST, there was a significant decrease in the incidence and severity at 4 and 6 h in ketamine group (P < 0.05) which is comparable to the study conducted by Rajan et al.[8] where they compared ketamine with two different doses of magnesium sulfate (250 and 500 mg) nebulization on POST and found that ketamine and magnesium sulfate (500 mg) nebulization decreased the incidence of POST at 0, 2, and 4 h.
Jain and Barasker[21] also conducted a similar study comparing ketamine and magnesium sulfate nebulization on POST and found that both decreased the incidence of POST when compared to control group but no significant difference between the ketamine and magnesium sulfate group.
The incidence of sore throat in the magnesium sulfate group was not significantly reduced when compared to ketamine group which is comparable to the study conducted by Rajan et al.[8] where they found that increasing the magnesium sulfate dose to 500 mg produced a similar effect of ketamine nebulization on reducing the incidence of POST. The dose of magnesium sulfate (250 mg) we used may not be sufficient to produce the desired effect and higher doses may require. There are no sufficient data to support our study, and more studies are required to support our hypothesis.
The hemodynamic parameters such as HR, SBP, and DBP showed statistically significant (P < 0.05) increase in ketamine group following nebulization which may be due to systemic absorption of the drug. However, a study done by Rajan et al.[8] did not show any difference in the hemodynamic variables on pre- and post-nebulization. Further studies are required to prove our results.
The proposed mechanism for the anti-inflammatory and antinociceptive effect of magnesium sulfate is thought to be by reducing the release of inflammatory mediators such as histamine, leukotrienes, and thromboxanes.[17] Magnesium also antagonizes NMDA receptors. It is also noted that the effect of magnesium was due to the direct contact of magnesium ions with the pharyngeal wall. Ketamine with its NMDA receptor antagonism produces profound antinociceptive and anti-inflammatory action by acting on peripheral NMDA receptors on the pharyngeal wall because the systemic administration of ketamine does not produce the same desired effect.[22]
There are a few limitations to our study, the dose we used was a fixed dose and the least effective dose is not known. We did not measure the serum levels of magnesium and ketamine to monitor the drug levels, and laryngoscopy was done by different anesthetists.
CONCLUSION
We conclude that nebulization with ketamine 50 mg before endotracheal intubation is more effective in preventing POST at 4 and 6 h than nebulization with magnesium sulfate 250 mg.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chandler M. Tracheal intubation and sore throat: A mechanical explanation. Anaesthesia. 2002;57:155–61. doi: 10.1046/j.1365-2044.2002.02329.x. [DOI] [PubMed] [Google Scholar]
- 2.Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. 2002;88:582–4. doi: 10.1093/bja/88.4.582. [DOI] [PubMed] [Google Scholar]
- 3.Loeser EA, Bennett GM, Orr DL, Stanley TH. Reduction of postoperative sore throat with new endotracheal tube cuffs. Anesthesiology. 1980;52:257–9. doi: 10.1097/00000542-198003000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Sumathi PA, Shenoy T, Ambareesha M, Krishna HM. Controlled comparison between betamethasone gel and lidocaine jelly applied over tracheal tube to reduce postoperative sore throat, cough, and hoarseness of voice. Br J Anaesth. 2008;100:215–8. doi: 10.1093/bja/aem341. [DOI] [PubMed] [Google Scholar]
- 5.Teymourian H, Mohajerani SA, Farahbod A. Magnesium and ketamine gargle and postoperative sore throat. Anesth Pain Med. 2015;5:e22367. doi: 10.5812/aapm.5(3)2015.22367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogata J, Minami K, Horishita T, Shiraishi M, Okamoto T, Terada T, et al. Gargling with sodium azulene sulfonate reduces the postoperative sore throat after intubation of the trachea. Anesth Analg. 2005;101:290–3. doi: 10.1213/01.ANE.0000156565.60082.7C. [DOI] [PubMed] [Google Scholar]
- 7.Canbay O, Celebi N, Sahin A, Celiker V, Ozgen S, Aypar U. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. 2008;100:490–3. doi: 10.1093/bja/aen023. [DOI] [PubMed] [Google Scholar]
- 8.Rajan S, Malayil GJ, Varghese R, Kumar L. Comparison of usefulness of ketamine and magnesium sulfate nebulizations for attenuating postoperative sore throat, hoarseness of voice, and cough. Anesth Essays Res. 2017;11:287–93. doi: 10.4103/0259-1162.181427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahuja V, Mitra S, Sarna R. Nebulized ketamine decreases incidence and severity of post-operative sore throat. Indian J Anaesth. 2015;59:37–42. doi: 10.4103/0019-5049.149448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yadav M, Chalumuru N, Gopinath R. Effect of magnesium sulfate nebulization on the incidence of postoperative sore throat. J Anaesthesiol Clin Pharmacol. 2016;32:168–71. doi: 10.4103/0970-9185.173367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hung NK, Wu CT, Chan SM, Lu CH, Huang YS, Yeh CC, et al. Effect on postoperative sore throat of spraying the endotracheal tube cuff with benzydamine hydrochloride, 10% lidocaine, and 2% lidocaine. Anesth Analg. 2010;111:882–6. doi: 10.1213/ANE.0b013e3181d4854e. [DOI] [PubMed] [Google Scholar]
- 12.Ratnaraj J, Todorov A, McHugh T, Cheng MA, Lauryssen C. Effects of decreasing endotracheal tube cuff pressures during neck retraction for anterior cervical spine surgery. J Neurosurg. 2002;97:176–9. doi: 10.3171/spi.2002.97.2.0176. [DOI] [PubMed] [Google Scholar]
- 13.Lin CY, Tsai PS, Hung YC, Huang CJ. L-type calcium channels are involved in mediating the anti-inflammatory effects of magnesium sulphate. Br J Anaesth. 2010;104:44–51. doi: 10.1093/bja/aep336. [DOI] [PubMed] [Google Scholar]
- 14.Zhu MM, Zhou QH, Zhu MH, Rong HB, Xu YM, Qian YN, et al. Effects of nebulized ketamine on allergen-induced airway hyperresponsiveness and inflammation in actively sensitized Brown-Norway rats. J Inflamm (Lond) 2007;4:10. doi: 10.1186/1476-9255-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turpin F, Dallérac G, Mothet JP. Electrophysiological analysis of the modulation of NMDA-receptors function by D-serine and glycine in the central nervous system. Methods Mol Biol. 2012;794:299–312. doi: 10.1007/978-1-61779-331-8_20. [DOI] [PubMed] [Google Scholar]
- 16.Fawcett WJ, Haxby EJ, Male DA. Magnesium: Physiology and pharmacology. Br J Anaesth. 1999;83:302–20. doi: 10.1093/bja/83.2.302. [DOI] [PubMed] [Google Scholar]
- 17.Borazan H, Kececioglu A, Okesli S, Otelcioglu S. Oral magnesium lozenge reduces postoperative sore throat: A randomized, prospective, placebo-controlled study. Anesthesiology. 2012;117:512–8. doi: 10.1097/ALN.0b013e3182639d5f. [DOI] [PubMed] [Google Scholar]
- 18.McHardy FE, Chung F. Postoperative sore throat: Cause, prevention and treatment. Anaesthesia. 1999;54:444–53. doi: 10.1046/j.1365-2044.1999.00780.x. [DOI] [PubMed] [Google Scholar]
- 19.Joshi GP, Inagaki Y, White PF, Taylor-Kennedy L, Wat LI, Gevirtz C, et al. Use of the laryngeal mask airway as an alternative to the tracheal tube during ambulatory anesthesia. Anesth Analg. 1997;85:573–7. doi: 10.1097/00000539-199709000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Aditya AK, Das B, Mishra DK. Assessment of nebulized ketamine for reductions of incidence and severity of post-operative sore throat. Int J Med Health Res. 2017;3:130–2. [Google Scholar]
- 21.Jain S, Barasker SK. A comparative study of preoperative ketamine and MgSO4 nebulisation for incidence of post operative sore throat after endotracheal intubation. Int J Contemp Med Res. 2017;4:1356–9. [Google Scholar]
- 22.Park SY, Kim SH, Noh JI, Lee SM, Kim MG, Kim SH, et al. The effect of intravenous low dose ketamine for reducing postoperative sore throat. Korean J Anesthesiol. 2010;59:22–6. doi: 10.4097/kjae.2010.59.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]