Summary
Background
Breast cancer occurrences in developing countries are gradually matching caucasian levels. Since early detection is linked to reductions in morbidities and mortality, affordable screening techniques like breast self-examination (BSE) becomes imperative in these resource-limited economies. Ascertaining the Knowledge, Attitudes, and Practices (KAP) of breast cancers and BSE among young adult females will help provide baseline information for early and targeted interventions.
Method
A cross sectional survey involving 432 female senior secondary school students in Otuocha Educational Zone of Anambra State, Nigeria.
Results
A total of 321 (74.3%) valid questionnaires were returned. Mean age was 16.79 ± 1.48 years. Even though 84.6% and 55.2% had respectively heard about breast cancer and BSE, and the ‘General Knowledge’ of breast cancer was high (75.2%), specifics on ‘Risk Factors’ (41.5%) and ‘Symptoms’ (46.1%) were poor.
Knowledge on correct BSE ‘Techniques’ was 52.9%, but few know when to commence (43.1%), the right frequency (31.5%), or the right timing (24.6%). A large majority (73.6%) had positive attitudes, but only 6.1% practice it monthly, while 55.3% had never done it at all. No significant predictors of Knowledge and Practice of BSE was identified.
Conclusion
Health campaigns on BSE and breast cancers should provide specific details on techniques, risk factors and symptoms, while emphasizing on the right methods, timing and frequency. The positive attitudes identified raise optimism that health interventions would be effective and can have long term benefits. If possible, BSE and breast cancer teachings should be included in the secondary school academic curricula of resource-limited countries.
Keywords: Breast self-examination, BSE, Breast cancer, Women, Secondary schools, Knowledge, Attitude, Practice
Introduction
Besides lung and non-melanoma skin cancers, breast cancer is the commonest malignancy worldwide, constituting 11.9% of all cancers [1], with a male to female ratio of 1:67 [2]. It is the 5th commonest cause of deaths from cancers worldwide, accounting for 571,000 deaths in 2015 [3]. Its incidence among women has reportedly been on a steady increase, from 1:20 in 1960, to the current 1:8 [4].
Breast cancer reduces the life expectancy of affected population aged 31 and 50 years [5, 6], 3.5% of which are expected to die [6]. Early detection is associated with lower morbidities and mortalities [7], so it is not a surprise that 85% [8] to 95% [7, 9], of affected patients survive with early detection, while only 56% [8] survive if diagnosed late.
Two key facilitators of early detection are health education and screening [10]. Screening methods include breast self-examination (BSE), clinical breast examination (CBE), and mammography [11]. Even though CBE and mammography in developing countries are becoming increasingly available in recent years [7], their wide scale utilization in these resource-limited economies are poor due to significant financial and manpower limitations. Conversely, BSE offers a simple, cheap, and non-invasive screening option [10, 12, 13].
Breast cancers, unlike most others, occur in an organ (breast) that is easily visible [9, 14], and BSE is the visual and manual examination of breasts for lumps, bumps, and skin changes over nipples and breasts [4]. Monthly BSE is recommended from age 20 [4], Even though its efficacy in preventing breast cancer deaths is unproven [15, 16], it remains a free, painless and easy-to-practice technique, which helps improve body awareness, allowing changes potentially indicative of breast cancer to be picked up early [17, 18]. Alongside other screening methods, BSEs can improve outcomes and reduce mortality by as much as 25% [19].
Even though traditionally, Caucasian women have higher ocurrences, breast cancer incidence is reportedly rising in populations with previously low cases (mainly developing countries like Nigeria). This is presumably because more women increasingly adopt western lifestyles [6, 20] like the use of tobacco and alcohol, as well as the attainment of tetiary education by most females, which results in late marriages and delayed first pregnancies (> 30 years) [10].
Delayed presentations >3 months are considered prolonged [2], but notably, only 20%-30% of Caucasians delay this long, as against 70% of African women [2, 21, 22]. Overall, affected Africans present at least a decade earlier than their Caucasian counterparts [20], during which time their lesions are bigger, [23, 24] more aggressive [25-28], advanced [29], and with poor prospects of long-term survivals [23, 30]. Five-year survival rates of breast cancers in Nigeria is < 10% compared to the 70% from developed countries [13, 22]. These racially-observed variations may not be solely due to socioeconomic differences [28], but largely attributable to the lack of early detection programmes and poor diagnostic and treatment facilities [5, 10, 14].
Even though the mean age of presentation in Nigeria is 42 to 44 years [2, 26, 31], prognosis in younger patients aged < 40 years is poor [32], and early screening and detection is vital [17]. While reports vary, one study found that 12% of the cancers in Nigeria are among those aged < 30, the youngest being a 16 year old [33]. Another paper reported occurrences in patients aged 14-96 years, with 70% among 26-50 year olds and cumulative frequencies of 0.8% at ≤ 20 years and 3.3% at < 25 years [21]. These statistics suggest that breast cancer should not be neglected among the under 30s. Therefore, ascertaining their KAP regarding breast cancers and BSE provides baseline information valuable to concerned stakeholders in the design and implementation of targeted interventions aimed at early disease prevention [34], improving survival rates [4, 35, 36] and quality among survivors [37].
Unfortunately, only a handful of studies have ever looked at BSE among Nigerian secondary school students [10, 32, 38] and young undergraduates [37], and none has ever looked at South-East Nigeria, an area culturally and socially different from the rest of the country. This study reduces this knowledge gap, and contributes to the growing literature regarding early preventive approaches to breast cancer in resource-limited environments exemplified by a developing country like Nigeria.
Methods
SETTING AND PARTICIPANTS
The participants included all female final year high school (called senior secondary school or SSS-3) students in the 26 government-owned schools within the Otuocha Post Primary Schools Service Commission (PPSSC) Educational Zone of Anambra State, Nigeria. The Otuocha PPSSC is one of the six Educational Zones in the State, [39] and covers three of the state’s 21 Local Government Areas (LGAs), which include Anambra East, Anambra West, and Ayamelum. Anambra State is one of Nigeria’s 36 states, and is predominantly inhabited by Christians of the “Igbo” tribe located in the South Eastern part of the country, in West Africa. It has a projected 2016 population of 5,527,800 (based on the 2006 census) [40].
INCLUSION AND EXCLUSION CRITERIA
Participants must be female final year (SSS-3) students enrolled in one of the eligible secondary schools as at the time of the study. Boys and students in privately-owned schools were excluded. Overall, 10 schools with 190 students were eligible from Anambra East LGA, 7 schools (with 92 students) from Anambra West LGA, and 9 schools (with 150 students) from Ayamelum LGA. Two schools (one each from Anambra East and Ayamelum LGAs) were all-boy schools, and these were excluded, leaving a total of 24 schools and 432 participants.
STUDY DESIGN
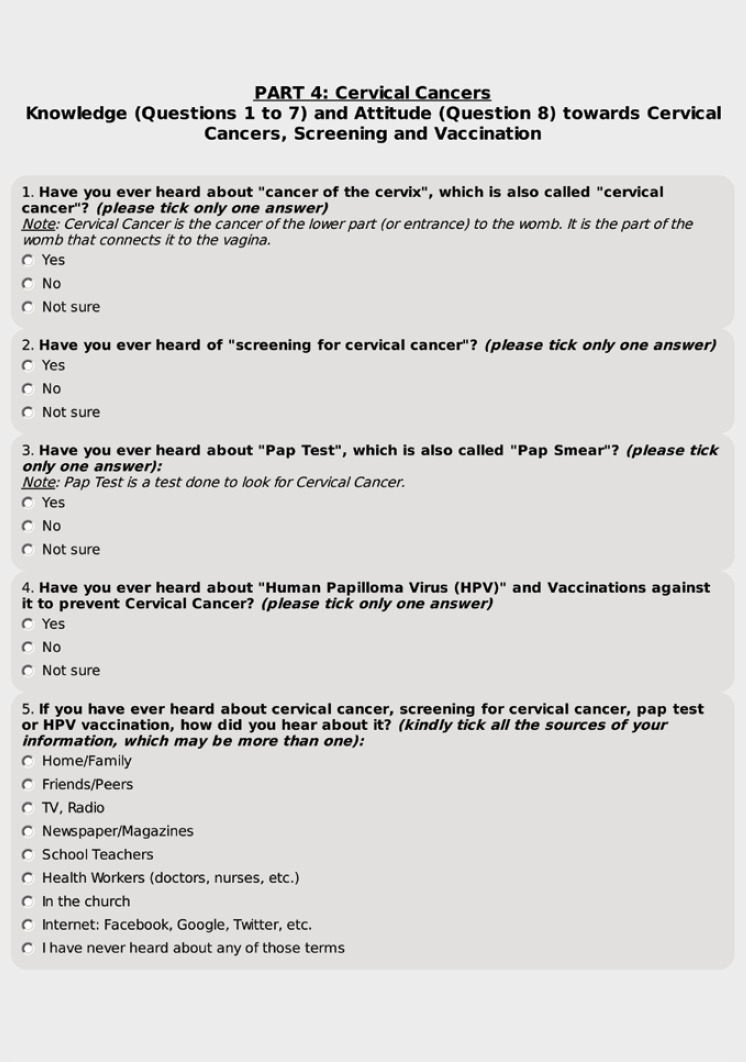
This study is a Cross Sectional, self-completed, questionnaire-based survey targeting all eligible participants, and is part of a larger study that explored the KAP of the participants regarding Breast Cancer, BSE and Cervical Cancers. Cervical cancer was not covered in this paper.
QUESTIONNAIRE
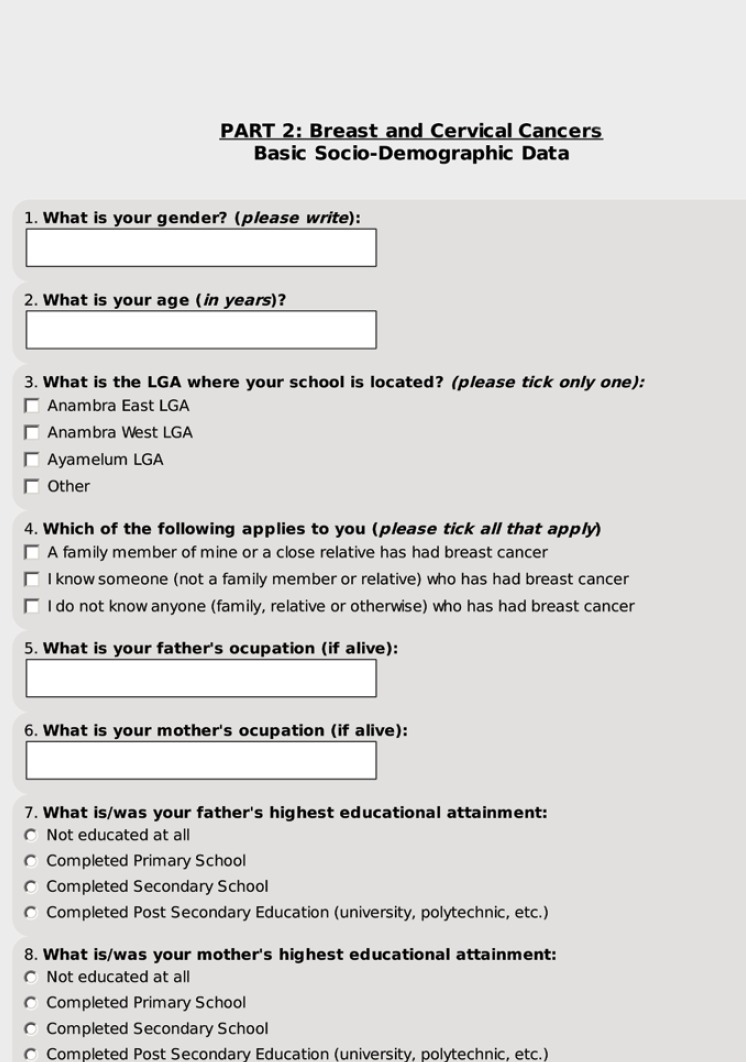
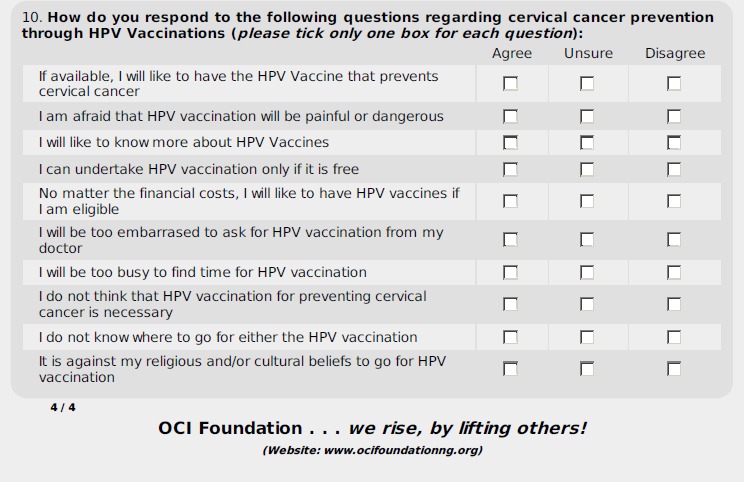
This was developed from validated questions adapted from previous publications [4, 14, 32, 41]. However, given that some of the wordings were modified to suit our participants, the document was piloted using 20 SSS-3 students in different PPSSCs in Anambra State. Feedbacks from them, along with inputs from professional colleagues, were used to develop the final Questionnaire (Annex 1).
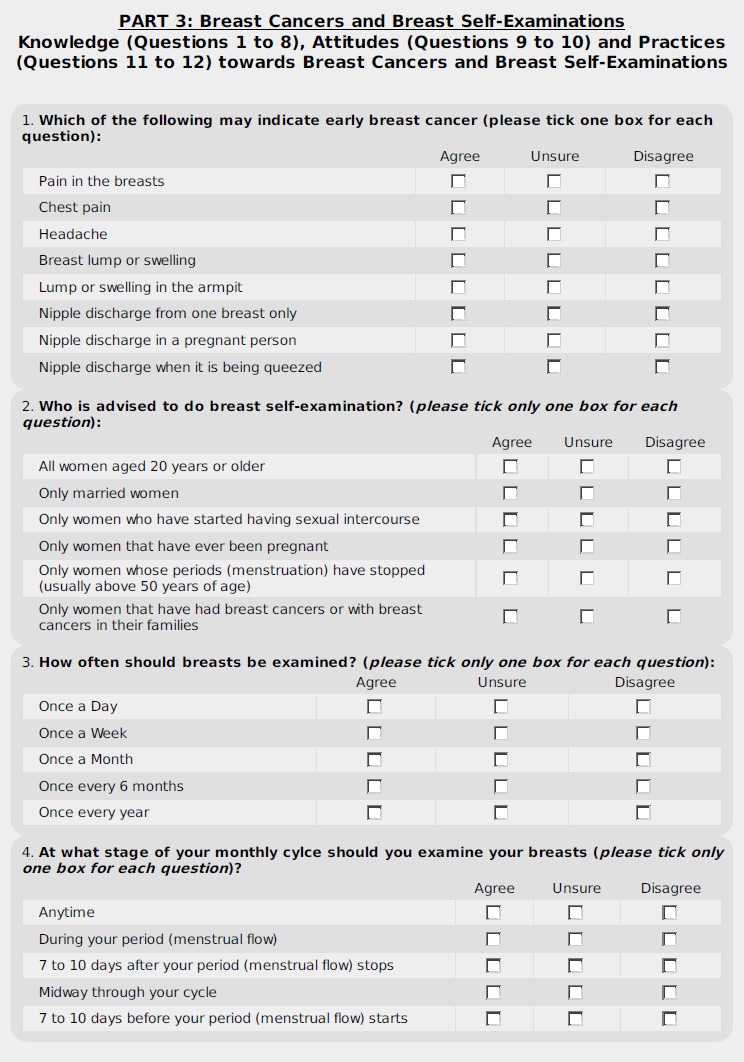
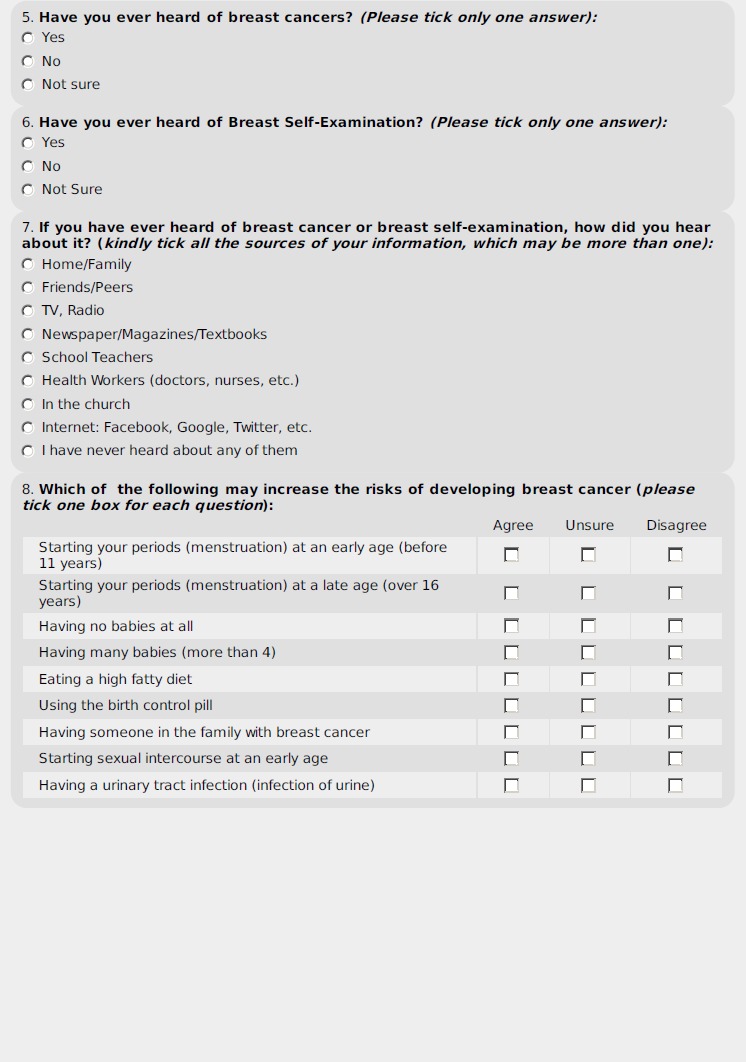
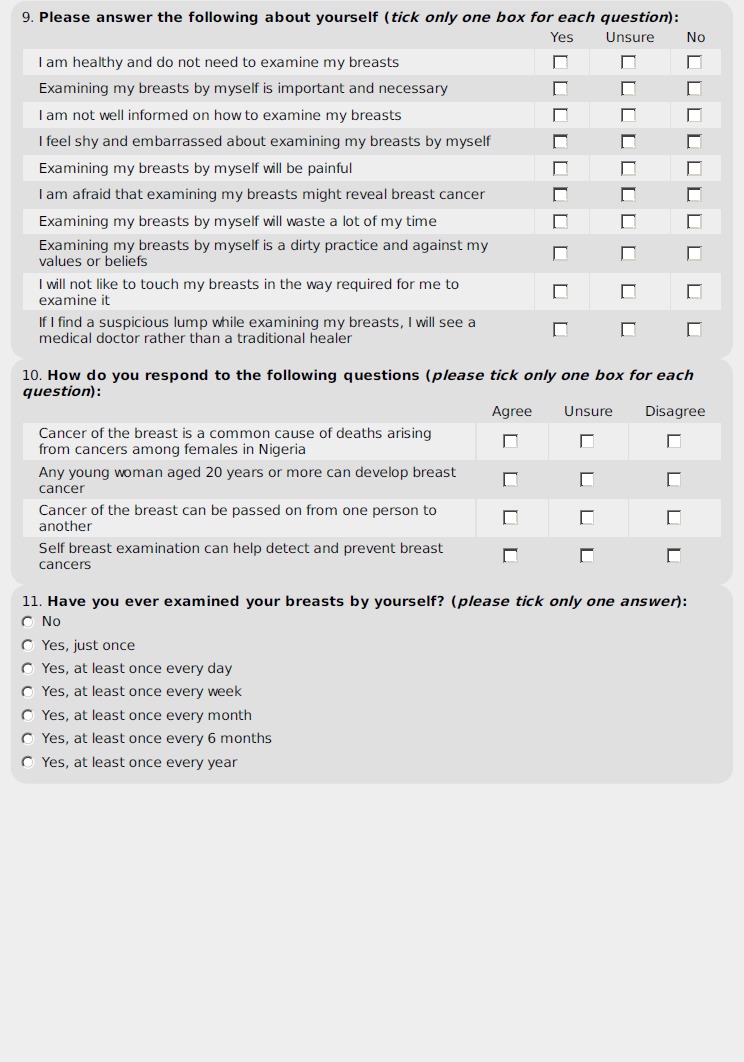
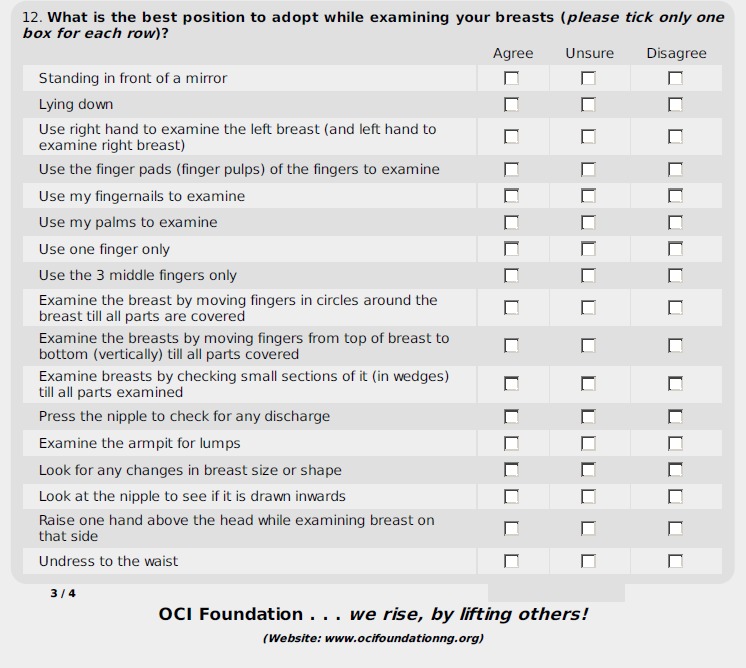
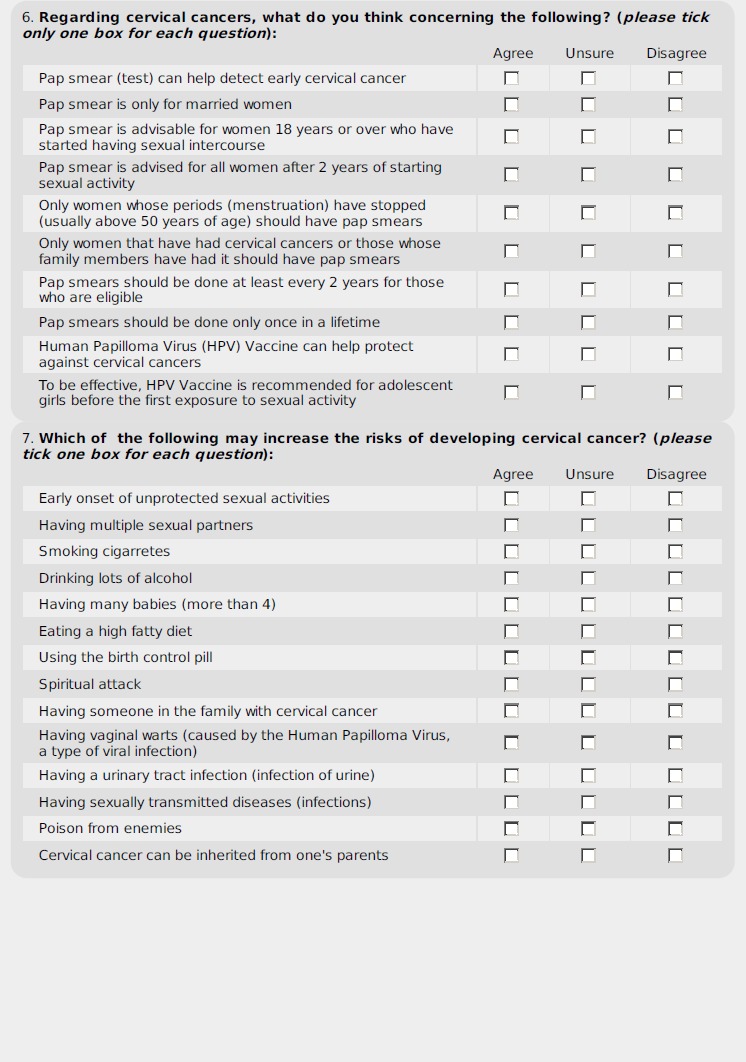
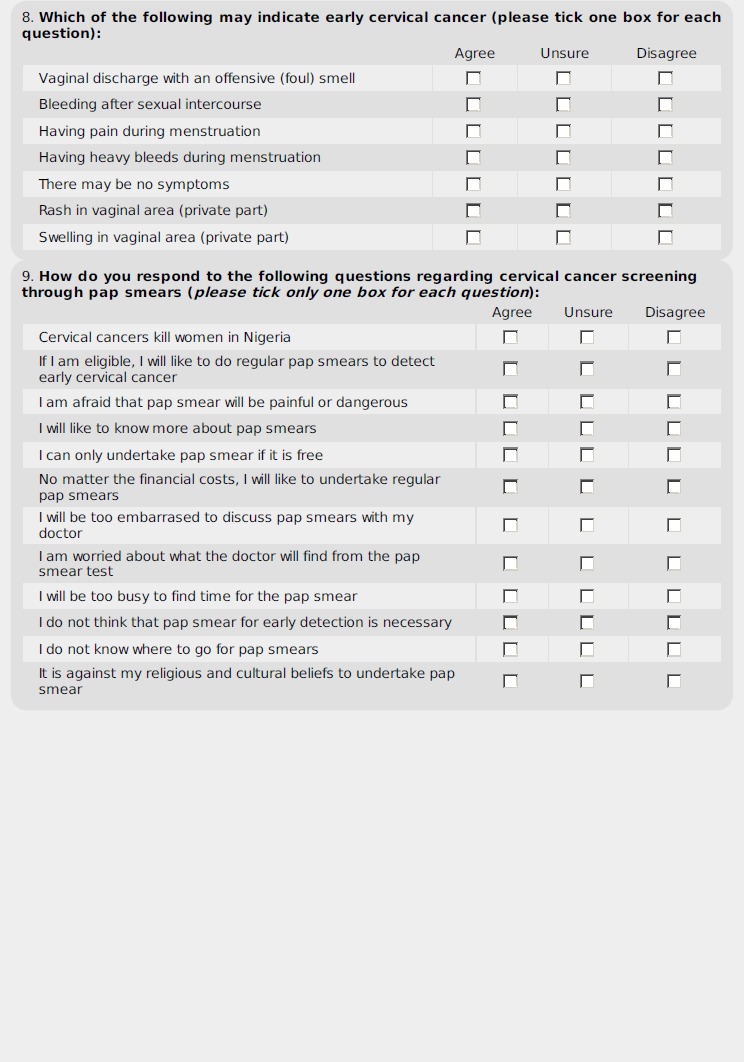
The questionnaire was divided into four parts. Part 1 contained the Introduction and Consent, while Part 2 (8 questions) covered the basic respondent demographics. Part 3 (12 questions) collects information on the participants’ KAP on Breast Cancers and BSE. Under this Part 3, Knowledge questions for Breast Cancers were explored with Question Numbers 1 (Early Symptoms), 8 (Risk Factors) and 10 (General). BSE was covered by other questions in Part 3 as follows: General Knowledge (Number 2); Knowledge of BSE Methods (Questions 3, 4 and 12); Attitudes and Practices (Questions 9 and 11 respectively). Questions 5, 6 and 7 explored those that have heard about breast cancers and BSE, as well as their sources. To eliminate responses based on speculations by the participants, some of the questions were worded negatively, while others were presented positively.
Part 4 of the Questionnaire had 10 major questions, and explored the Knowledge and Attitudes on Cervical Cancers, which are not covered in this paper.
The final, validated tool was dispatched and returned within one week from September 18th 2017 through the Zonal Director to the various school principals, with each school getting exactly the number for their eligible students.
DATA ENTRY AND ANALYSIS
All analysis were with IBM® SPSS version 25.0. Most responses to the questions and sub-questions in Part 3 had options of ‘Yes or Agree’, ‘Not Sure or Unsure’ and ‘No or Disagree’. For positive questions, these attracted scores of 3, 2 or 1 respectively, and were reversed accordingly for all negative items. Percentages were worked out and interpreted in line with the methods of a previous publication,4 with ‘≥70%’ indicating Excellent, while ‘50-69%’ and ‘< 50%’ signify Moderate and Poor respectively.
The Binary Logistics Regression (BLR) was used to explore statistical associations,. Three Independent (Predictor) Variables and Three Dependent (Outcome) Variables were tested, with variables dichotomized as necessary. The three Predictor Variables include each of the “educational status of father and mother (‘Primary/Not at all’ Versus ‘Secondary/Tertiary’)” and “Knowledge of family member or anyone with breast cancer (Yes or No)”. The three Outcome Variables include: “Whether BSE has ever been practised”, “If BSE is Practised Monthly”, and “If BSE is practised 7-10 days after periods”. The responses to each Outcome Variable was dichotomized to “Yes or No”. All associations with p-values of < 0.05 are significant.
Results
A total of 390 out of the 432 dispatched questionnaires were returned, but only 321 had enough components completed to warrant inclusion in the analysis. This gives a 74.3% response rate.
THE BASIC RESPONDENT CHARACTERISTICS (TAB. I)
Tab. I.
Demographics and characteristics of female senior secondary school students in State Government-owned schools of Otuocha Educational Zone, Anambra State, Nigeria.
| S/N | Respondent variable | Various components | Number | Percent |
|---|---|---|---|---|
| 1. | Age Details (n = 317) |
Mean | 16.79 | |
| Mode | 17 | |||
| Median | 17.00 | |||
| Standard deviation | 1.475 | |||
| Range | 12 (13-25) | |||
| 2. | Local Government Area (n = 307) |
Anambra East | 158 | 51.5 |
| Anambra West | 57 | 18.6 | ||
| Ayamelum | 92 | 30.0 | ||
| 3. | Knowledge of someone with breast cancer (n = 290) |
Yes: family member affected | 12 | 4.1 |
| Yes: none family member | 40 | 13.8 | ||
| No: I know no affected person | 238 | 82.1 | ||
| 4. | Mother’s highest educational attainment (n = 312) |
Not educated at all | 31 | 9.9 |
| Completed primary school | 119 | 38.1 | ||
| Completed secondary school health | 123 | 39.4 | ||
| Completed post-secondary education (university, polytechnic, etc.) | 39 | 12.5 | ||
| 5. | Father’s highest educational attainment (n = 307) |
Not educated at all | 29 | 9.4 |
| Completed primary school | 117 | 38.1 | ||
| Completed secondary school | 118 | 38.4 | ||
| Completed post-secondary education (university, polytechnic, etc.) | 43 | 14.0 | ||
| 6. | Source of information regarding BSE* and breast cancers (This questions allowed respondents to tick multiple answers) |
Television/radio | 162 | 50.5 |
| School teachers | 158 | 49.2 | ||
| Health workers (doctors, nurses, etc.) | 148 | 46.1 | ||
| Newspaper/magazines/textbooks | 138 | 43.0 | ||
| Friends/peers | 113 | 35.2 | ||
| Internet (Facebook, Google, Twitter, etc.) | 102 | 31.8 | ||
| Home/family | 101 | 31.5 | ||
| Church | 51 | 15.9 | ||
| Not sure | 16 | 5.0 | ||
| 7. | Ever heard of BSE? (n = 315) |
Yes | 174 | 55.2 |
| No | 114 | 36.2 | ||
| Not sure | 27 | 8.6 | ||
| 8. | Ever heard of breast cancer? (n = 318) | Yes | 269 | 84.6 |
| No | 43 | 13.5 | ||
| Not sure | 6 | 1.9 |
*BSE: Breast self-examination
The ages range from 13-25 years (Mean of 16.79 ± 1.48). Only 4.1% have a family member that had been affected with breast cancer, while 82.1% know no one that is affected, be it a family member or anyone else. About 84.6% has heard about breast cancer, while 55.2% has heard about BSE.
The best sources of information include Television/Radio (50.5%), school teachers (49.2%), health workers (46.1%), and the print media (43.0%).
GENERAL KNOWLEDGE, SYMPTOMS AND RISK FACTORS OF BREAST CANCER (TAB. II)
Tab. II.
Knowledge of breast cancer, its early symptoms, and its risk factors among female senior secondary school students in State Government-owned schools of Otuocha Educational Zone, Anambra State, Nigeria.
| S/N | Description | Agree (%) |
Unsure (%) |
Disagree (%) |
Total scores** (average: 1 to 3) |
Correct scores* (% of average) |
|---|---|---|---|---|---|---|
| A. General knowledge on breast cancers (Q10, Part 3 of Questionnaire) | ||||||
| 1 | Breast cancer is a common cause of cancers deaths among Nigerian women (n = 318) | 242 (76.1)* | 53 (16.4) | 24 (7.5) | 854 (2.69) | 726 (85.0) |
| 2 | Any woman aged ≥20 can develop breast cancer (n = 317) | 179 (56.5)* | 88 (27.8) | 50 (15.8) | 763 (2.41) | 537 (70.4) |
| 3 | Breast cancer is transmissible (n = 314) | 56 (17.8) | 100 (31.8) | 158 (50.3)* | 730 (2.32) | 474 (64.9) |
| 4 | BSE can help detect and prevent breast cancers (n = 316) | 209 (66.1)* | 64 (20.3) | 43 (13.6) | 798 (2.53) | 627 (78.6) |
| Totals | 3,145 (2.49) | 2,364 (75.2) | ||||
| B. Knowledge of Risk Factors For Breast Cancers (Q8, Part 3 of Questionnaire) | ||||||
| 5 | Early onset of menstruation; < 11 years (n = 316) | 49 (15.5)* | 140 (44.3) | 127 (40.2) | 554 (1.75) | 147 (26.5) |
| 6 | Late onset of menstruation; > 16 years (n = 314) | 37 (11.8) | 164 (52.2) | 113 (36.0)* | 704 (2.24) | 339 (48.2) |
| 7 | Having no babies at all (n = 317) | 25 (7.9)* | 130 (41.0) | 162 (51.1) | 497 (1.57) | 75 (15.1) |
| 8 | Having many babies; > 4 (n = 309) | 21 (6.8) | 115 (37.2) | 173 (56.0)* | 770 (2.49) | 519 (67.4) |
| 9 | Eating a high fatty diet (n = 314) | 55 (17.5) | 161 (51.3) | 98 (31.2)* | 671 (2.14) | 294 (43.8) |
| 10 | Using the birth control pill (n = 305) | 57 (18.7) | 179 (58.7) | 69 (22.6)* | 622 (2.04) | 207 (33.3) |
| 11 | Having a family history of breast cancer (n = 313) | 85 (27.2)* | 109 (34.8) | 119 (38.0) | 592 (1.89) | 255 (43.1) |
| 12 | Early onset of sexual intercourse (n = 312) | 69 (22.1) | 144 (46.2) | 99 (31.7)* | 654 (2.10) | 297 (45.4) |
| 13 | Having a urinary tract infection (n = 313) | 79 (25.2) | 158 (50.5) | 76 (24.3)* | 623 (1.99) | 228 (36.6) |
| Totals | 5,687 (2.02) | 2,361 (41.5) | ||||
| C. Knowledge of early symptoms of breast cancer (Q1, Part 3 of Questionnaire) | ||||||
| 14 | Pain in the breasts (n = 319) | 164 (51.4) | 91 (28.5) | 64 (20.1)* | 538 (1.69) | 192 (35.7) |
| 15 | Chest pain (n = 313) | 59 (18.8) | 152 (48.6) | 102 (32.6)* | 669 (2.14) | 306 (45.7) |
| 16 | Headache (n = 309) | 66 (21.4) | 103 (33.3) | 140 (45.3)* | 692 (2.24) | 420 (60.7) |
| 17 | Breast lump (n = 314) | 141 (44.9)* | 118 (37.6) | 55 (17.5) | 714 (2.27) | 423 (59.2) |
| 18 | Lump in armpit (n = 309) | 67 (21.7)* | 145 (46.9) | 97 (31.4) | 588 (1.90) | 201 (34.2) |
| 19 | Unilateral nipple discharge (n = 314) | 103 (32.8)* | 139 (44.3) | 72 (22.9) | 659 (2.10) | 309 (46.9) |
| 20 | Nipple discharge in a pregnant person (n = 309) | 62 (20.1) | 148 (47.9) | 99 (32.0)* | 655 (2.12) | 297 (45.3) |
| 21 | Nipple discharge when squeezed (n = 313) | 73 (23.3) | 165 (52.7) | 75 (24.0)* | 628 (2.01) | 225 (35.8) |
| Totals | 5,143 (2.05) | 2,373 (46.1) | ||||
| Grand totals for breast cancer knowledge |
13,975 (2.19) 7,098 (50.8) |
|||||
-**Total Scores are derived by the sum of the following: Correct Responses (marked with *; multiply by 3) + Unsure (multiply by 2) + Incorrect (multiply by 1)
-Result Interpretation: ≥ 70% = Excellent knowledge; ≥ 50 to < 70% = Moderate knowledge; < 50% = Poor knowledge
-BSE = Breast Self-examination
Most respondents (75.2%) had an excellent ‘General Knowledge’ of breast cancer (Tab. IIA), but specific Knowledge on the ‘Risk Factors’ (41.5%; Tab. IIB) and ‘Early Symptoms’ (46.1%; Tab. IIC) were poor.
KNOWLEDGE, ATTITUDES AND PRACTICE OF BSE (TAB. III)
Tab. III.
Knowledge of Breast Self-Examination (BSE) among female senior secondary school students in State Government-owned schools of Otuocha Educational Zone, Anambra State, Nigeria.
| S/N | Description | Agree (%) |
Unsure (%) |
Disagree (%) |
Total scores** (average: 1 to 3) |
Correct scores* (% of average) |
|---|---|---|---|---|---|---|
| A. Knowledge of who should practice BSE (Q2, Part 3 of Questionnaire) | ||||||
| 1 | All women ≥20 years (n = 320) | 138 (43.1)* | 103 (32.2) | 79 (24.7) | 699 (2.18) | 414 (59.2) |
| 2 | Only married women (n = 313) | 36 (11.5) | 84 (26.8) | 193 (61.7)* | 783 (2.50) | 597 (73.9) |
| 3 | Only sexually active women (n = 317) | 55 (17.4) | 93 (29.3) | 169 (53.3)* | 748 (2.36) | 507 (67.8) |
| 4 | Only women that have been pregnant (n = 317) | 32 (10.1) | 117 (36.9) | 168 (53.0)* | 770 (2.43) | 504 (65.5) |
| 5 | Only post-menopausal women (n = 318) | 39 (12.3) | 109 (34.3) | 170 (53.5)* | 767 (2.41) | 510 (66.5) |
| 6 | Only women with positive family history of breast cancer (n = 319) | 77 (24.1) | 105 (32.9) | 137 (42.9)* | 698 (2.19) | 411 (58.9) |
| Totals | 4,465 (2.35) | 2,943 (65.9) | ||||
| B. Knowledge of BSE Frequency (Q3, Part 3 of Questionnaire) | ||||||
| 7 | Once a day (n = 314) | 72 (22.9) | 118 (37.6) | 124 (39.5)* | 680 (2.17) | 372 (54.7) |
| 8 | Once a week (n = 312) | 74 (23.7) | 131 (42.0) | 107 (34.3)* | 657 (2.11) | 321 (48.9) |
| 9 | Once a month (n = 314) | 99 (31.5)* | 127 (40.4) | 88 (28.0) | 639 (2.04) | 297 (46.5) |
| 10 | Once every 6 months (n = 311) | 51 (16.4) | 136 (43.7) | 124 (39.9)* | 695 (2.23) | 372 (53.5) |
| 11 | Once every year (n = 312) | 46 (14.7) | 112 (35.8) | 155 (49.5)* | 735 (2.35) | 228 (31.0) |
| Totals | 3,406 (2.18) | 1,590 (46.7) | ||||
| C. Knowledge of BSE Timing (Q4, Part 3 of Questionnaire) | ||||||
| 12 | Anytime during cycle (n = 317) | 133 42.0 | 108 (34.1) | 76 (24.0)* | 577 (1.82) | 228 (39.5) |
| 13 | During menstrual flow (n = 314) | 88 (28.0) | 130 (41.4) | 96 (30.6)* | 636 (2.03) | 288 (45.3) |
| 14 | 7 to 10 days after periods (n = 313) | 77 (24.6)* | 153 (48.9) | 83 (26.5) | 620 (1.98) | 231 (37.3) |
| 15 | Midway through your cycle (n = 312) | 49 (15.7) | 175 (56.1) | 88 (28.2)* | 663 (2.13) | 264 (39.8) |
| 16 | 7 to 10 days before period (n = 313) | 62 (19.8) | 157 (50.2) | 94 (30.0)* | 658 (2.10) | 282 (42.9) |
| Totals | 3,154 (2.01) | 1,293 (41.0) | ||||
| D. Knowledge of BSE Techniques (Q12, Part 3 of Questionnaire) | ||||||
| 17 | Standing in front of a mirror (n = 315) | 174 (55.2)* | 86 (27.3) | 55 (17.5) | 749 (2.38) | 522 (69.7) |
| 18 | Lying down (n = 311) | 77 (24.8)* | 139 (44.7) | 95 (30.5) | 604 (1.94) | 231 (38.2) |
| 19 | Use one hand to examine the opposite one, and vice versa (n = 312) | 149 (47.8)* | 118 (37.8) | 45 (14.4) | 728 (2.33) | 447 (61.4) |
| 20 | Use finger pads/pulps (n = 312) | 101 (32.4)* | 146 (46.8) | 65 (20.8) | 660 (2.12) | 303 (45.9) |
| 21 | Use fingernails to examine (n = 310) | 45 (14.5) | 135 (43.5) | 130 (41.9)* | 705 (2.27) | 390 (55.3) |
| 22 | Use palms to examine (n = 310) | 75 (24.2) | 137 (44.2) | 98 (31.6)* | 643 (2.07) | 294 (45.7) |
| 23 | Use one finger only (n = 311) | 51 (16.4) | 134 (43.1) | 126 (40.5)* | 697 (2.24) | 378 (54,2) |
| 24 | Use the 3 middle fingers only (n = 308) | 62 (20.1)* | 154 (50.0) | 92 (29.9) | 586 (1.90) | 186 (31.7) |
| 25 | Use circular motions till all parts are covered (n = 312) | 125 (40.1)* | 129 (41.3) | 58 (18.6) | 691 (2.21) | 375 (54.3) |
| 26 | Use vertical motions till all parts covered (n = 313) | 117 (37.4)* | 143 (45.7) | 53 (16.9) | 690 (2.20) | 351 (50.9) |
| 27 | Examine breasts in wedges till all parts examined (n = 311) | 103 (33.1)* | 162 (52.1) | 46 (14.8) | 679 (2.18) | 309 (45.5) |
| 28 | Press the nipple to check for any discharge (n = 312) | 126 (40.4)* | 133 (42.6) | 53 (17.0) | 697 (2.23) | 378 (54.2) |
| 29 | Examine the armpit for lumps (n = 305) | 108 (35.4)* | 134 (43.9) | 63 (20.7) | 655 (2.15) | 324 (49.5) |
| 30 | Look for any changes in breast size or shape (n = 310) | 167 (53.9)* | 105 (33.9) | 38 (12.3) | 649 (2.42) | 501 (77.2) |
| 31 | Look at shape of nipples (n = 312) | 123 (39.4)* | 147 (47.1) | 42 (13.5) | 705 (2.26) | 369 (52.3) |
| 32 | Raise one hand above the head while examining breast on that side (n = 313) | 147 (47.0)* | 111 (35.5) | 55 (17.6) | 718 (2.29) | 441 (61.4) |
| 33 | Undress to the waist (n = 311) | 86 (27.7)* | 135 (43.4) | 90 (28.9) | 618 (1.99) | 258 (41.7) |
| Totals | 11,464 (2.19) | 6,057 (52.9) | ||||
| Grand totals for BSE knowledge |
22,489 (2.18) 11,883 (52.84) |
|||||
-**Total scores are derived by the sum of the following: Correct responses (marked with *; multiply by 3) + Unsure (multiply by 2) + Incorrect (multiply by 1)
- Result interpretation: ≥ 70% = Excellent knowledge; ≥ 50 to < 70% = Moderate knowledge; < 50% = Poor knowledge
Only one single question each correctly represented the ‘Knowledge on who should do BSE’, its ‘Frequency’, and its ‘Timing’, and all three responses were poor. Only 43.1% know that any woman above the age of 20 years should practice BSE (Tab. IIIA), while less than one-third (31.5%) know that it should be done monthly (Tab. IIIB). Only one-quarter (24.6%) know that BSEs are best carried out about one week after the monthly periods cease.
Multiple positive and negative questions explored the ‘Knowledge on Techniques of BSEs’ (Tab. IIID), and the average revealed a level that is just Moderate (52.9%).
‘Attitude’ to BSE is Excellent (73.6%; Tab. IV), but, as shown in Table V, about 55.3% of the respondents had never practised BSE, while only 6.1% do so at the correct monthly frequency.
Tab. IV.
Attitudes to Breast Self-Examination (BSE) among female senior secondary school students in State Government-owned schools of Otuocha Educational Zone, Anambra State, Nigeria.
| S/N | Description (Question 9; Part 3 of the Questionnaire) |
Agree (%) |
Unsure (%) |
Disagree (%) |
Total scores** (average: 1 to 3) |
Correct scores* (% of average) |
|---|---|---|---|---|---|---|
| 1 | I am healthy and do not need to examine my breasts (n = 319) | 119 (37.3) | 68 (21.3) | 132 (41.4)* | 651 (2.04) | 396 (60.8) |
| 2 | Examining my breasts by myself is important and necessary (n = 317) | 216 (68.1)* | 55 (17.4) | 46 (14.5) | 804 (2.54) | 648 (80.6) |
| 3 | I am not well informed on how to examine my breasts (n = 318) | 148 (46.5) | 65 (20.4) | 105 (33.0) | NB: This item was not scored and not part of the calculations | |
| 4 | I feel shy and embarrassed about examining my breasts by myself (n = 318) | 61 (19.2) | 54 (17.0) | 203 (63.8)* | 778 (2.45) | 609 (78.3) |
| 5 | Examining my breasts by myself will be painful (n = 314) | 57 (18.2) | 95 (30.3) | 162 (51.6)* | 733 (2.33) | 486 (66.3) |
| 6 | I am afraid that examining my breasts might reveal breast cancer (n = 314) | 61 (19.4) | 88 (28.0) | 165 (52.5)* | 732 (2.33) | 495 (67.6) |
| 7 | Examining my breasts by myself will waste a lot of my time (n = 311) | 54 (17.0) | 79 (24.9) | 184 (58.0)* | 764 (2.41) | 552 (72.3) |
| 8 | Examining my breasts by myself is a dirty practice and against my values or beliefs (n = 318) |
56 (17.6) | 69 (21.7) | 193 (60.7)* | 773 (2.43) | 579 (74.9) |
| 9 | I will not like to touch my breasts in the way required for me to examine it (n = 318) |
76 (23.9) | 74 (23.3) | 168 (52.8)* | 728 (2.29) | 504 (69.2) |
| 10 | If I find a suspicious lump while examining my breasts, I will see a medical doctor rather than a traditional healer (n = 316) |
230 (72.8)* | 44 (13.9) | 42 (13.3) | 820 (2.59) | 690 (83.8) |
| Grand totals for bse attitude | 6,738 (2.19) | 4,959 (73.6) | ||||
-**Total scores are derived by the sum of the following: Correct responses (marked with *; multiply by 3) + Unsure (multiply by 2) + Incorrect (multiply by 1)
-Result Interpretation: ≥ 70% = Excellent knowledge; ≥ 50 to < 70% = Moderate knowledge; < 50% = Poor knowledge
Tab. V.
Practice of Breast Self-Examination (BSE) among female senior secondary school students in State Government-owned schools of Otuocha Educational Zone, Anambra State, Nigeria (n = 313).
| S/N | Have you ever practised BSE | Number | Percent |
|---|---|---|---|
| 1 | Never | 173 | 55.3 |
| 2 | Once ever | 47 | 15.0 |
| 3 | Once daily | 53 | 16.9 |
| 4 | Once weekly | 16 | 5.1 |
| 5 | Once monthly | 19 | 6.1* |
| 6 | Once six monthly | 2 | 0.6 |
| 7 | Once yearly | 3 | 1.0 |
*Correct practice
PREDICTORS OF BSE (TAB. VIA-B-C)
Tabl. VI.
Influence of “parental educational attainment” and “the knowledge of someone with breast cancer” on the Practice, Frequency, and Timing of BSEs* among Senior Secondary School students in State Government-owned schools of Otuocha Educational Zone, Anambra State, Nigeria.
| S/N | Characteristic | Odds Ratio (OR) | Confidence Interval | p-value | |
|---|---|---|---|---|---|
| Lower | Higher | ||||
| A. Respondent knows someone with breast cancer (family or other) | |||||
| 1. | Have practised BSE* at least once before (n = 285) | 0.79 | 0.43 | 1.46 | 0.46 |
| 2. | Knows that BSE* is recommended to be done monthly (n = 284) | 1.12 | 0.58 | 2.17 | 0.74 |
| 3. | Knows that BSE* is recommended to be done 7-10 days after menses (n = 284) | 1.10 | 0.54 | 2.24 | 0.79 |
| B. Father’s education less than secondary/tertiary level | |||||
| 1. | Have practised BSE* at least once before (n = 301) | 0.78 | 0.50 | 1.24 | 0.30 |
| 2. | Knows that BSE* is recommended to be done monthly (n = 301) | 1.00 | 0.61 | 1.61 | 0.98 |
| 3. | Knows that BSE* is recommended to be done 7-10 days after menses (n = 301) | 1.06 | 0.63 | 1.80 | 0.82 |
| C. Mother’s education less than secondary/tertiary level | |||||
| 1. | Have practised BSE* at least once before (n = 306) | 0.90 | 0.58 | 1.42 | 0.66 |
| 2. | Knows that BSE* is recommended to be done monthly (n = 305) | 1.08 | 0.67 | 1.75 | 0.75 |
| 3. | Knows that BSE* is recommended to be done 7-10 days after menses (n = 306) | 1.07 | 0.64 | 1.80 | 0.80 |
*BSE: Breast self-examination.
No significant predictors of the Practice of BSE, or their Knowledge on its Frequency and Timing were identified.
Discussion
At 74.3%, the response rate from this study is decent, even though it is less than the 95.7% and the 91.7% recorded in similar studies of female secondary school students elsewhere in Nigeria [10] and Saudi Arabia [17] respectively. Also, the mean age (in years) of 16.79 ± 1.48 for the participants from our study bears a striking similarity to the rates from studies that looked at other Nigerian schools in Abuja [10] and Lagos [32], as well those from overseas studies of similar high school female students [42]. Our finding that only 4.1% of the respondents reported a positive family history of breast cancer is also consistent with the 4% reported in a previous Nigerian study [2]. These similarities to findings of previous publications, along with the decent response rate of this study, suggest that our findings might be representative, and hopefully, generalizable.
It is encouraging that over 4-in-5 (84.6%) and a little more than half (55.2%) of the respondents had respectively heard of breast cancer and BSE prior to our study. This would imply that a good knowledge base does exist for any health enlightenment campaign, since issues on these subjects would not be completely new. Interestingly, these proportions are consistent with levels reported in similar Nigerian studies from Abuja (100% on breast cancer and 58.5% on BSE) [10] and Lagos (97% on cancer and 56.4% on BSE) [32], but higher that the 37.9% of students that has heard about BSE in a Turkish study [42]. Cultural or religious differences may be responsible for the difference between the two nations.
Unfortunately, the fact that our participants have a moderate level of BSE awareness has not translated to reasonably high levels of Knowledge and Practice of BSEs. For instance, only 43.1% know that any woman above the age of 20 years should practice BSE, while one-third (31.5%) and one-quarter (24.6%) respectively know the correct Frequency and Timing. Even more disappointing is the fact that a much lower number (6.1%) actually do practice BSE on a monthly basis, while 55.3% had never practised it at all. These findings call for action, given the already-stated benefits of BSE in resource-limited economies like Nigeria, where it may be the only affordable screening measure available to millions of women. Compared to similar Nigerian studies, the 31.5% with proper knowledge of monthly BSEs is somewhat similar to the 36.4% found in Oyo State [38], but higher than the 18.8% reported from Abuja [10]. At 24.6%, the knowledge of the Timing of BSEs is much lower than the 51.8% from the Oyo State study [38], but higher than the 12.5% recorded in Abuja [10]. Similarly, the 6.1% that correctly practise BSE in our study is only slightly less than the 10.1% [10] and 14.5% [38] reported from the aforementioned studies, as well as the 19.0% found among slightly older undergraduates in a Nigerian University [37], while the 55.3% that had never practised BSE at all is similar to the 58.2% reported among a similar group of students in Oyo State, Nigeria [38].
Comparable overseas studies involving high school students of similar age and academic level also exist. Both of our findings on the knowledge of correct Frequency and Timing of BSEs were respectively higher than the 21.8% and 13.2% reported in a Turkish study [42], while the rate on actual practice of BSEs is nearly identical to the 6.7% [42] reported by the same Turkish study, but slightly higher than the 3.4% [17] from a Saudi Arabian study. International comparisons should be interpreted with caution though, given the likely difference in culture and religion among the two countries.
One more interesting finding on the knowledge of BSEs is that, when the responses of all the positive and negative questions are factored in (Tabl. IIIA), the general knowledge on BSE Practise moves from Poor (for the individual positive items), to Moderate level (65.9%). This shows that, even though the participants may have a poor knowledge of what is right, they seem to have a good idea of what is wrong regarding BSE. This observation has a huge implication for health education campaigns, since the emphasis has to be on promoting the right practices, and less so on potentially wrong ones. Comparisons reveal that these findings were broadly consistent with similar Nigerian [10, 38] and overseas [42] studies, which all either reported poor or moderate levels of knowledge (not practice) of BSEs.
A striking and very important finding of our work concerns the Attitude of the respondents towards BSE, where the 73.6% positive attitude is within the ‘Excellent’ range. A similar study in Abuja, Nigeria [10], also reported an 82.6% positive attitude. Combined, these high positive attitudes imply that, despite the low levels of knowledge and practise of BSEs in Nigeria, young females are keen to learn and follow recommendations, and, any well-designed and culturally-appropriate health intervention on BSEs, would be well received.
Regarding breast cancer, the poor levels of specific knowledge of the Risk Factors (41.5%) and Early Symptoms (46.1%) seem to agree with findings of similar groups in Nigeria [10],Turkey [42], and Saudi Arabia [17]. However, the seemingly high level of General Knowledge (75.2%) on breast cancer issues is likely to be due to the fact that we factored in both negative and positive knowledge. Again, these observations highlight the need for health educators to emphasize more on specific positive behaviours, rather than on more general and negative ones.
This study also found that nearly all sources of information for the participants on BSE and breast cancers were poor, with the best source (Television/Radio) benefitting just 50.5%. The rest of the sources, including information from school teachers, health workers, print media, church, internet, family, and peers, were all below 50%. This observation opens up a huge window of opportunity, as measures to involve school teachers and religious institutions (churches and mosques) in these campaigns will improve the reach and efficacy of the programs. This is recommended because school and religious events are popular in Nigeria, with 75.6% of Nigerians aged 15 to 24 years being literate [43], while 90% of the entire population identify as Christians or Muslims [44]. Unfortunately, other supposedly effective and popular means of information dissemination in the developed world (internet and electronic media), are not easily accessible to most Nigerians, due to poor power supply and high costs. Their role, for now, can only be complementary to schools and churches/mosques.
Finally, it is surprising that no significant associations were found between the participants’ knowledge of someone affected with breast cancer (family or otherwise) or their parents’ educational attainments, on the Knowledge of the Frequency and Timing of BSEs. Even though aspects of these none associations broadly agree with a study that showed no association between BSE and family history of breast cancer [42], as well as those of a few others [10, 17] that also found no association with age and other sociodemographic characteristics not covered in this work, these findings are generally not in line with majority of existing publications in this area. For instance, some previous studies have shown associations with family history of breast cancers [17, 37], knowledge of BSE [10, 42], and parental educational attainment [10].
STRENGTHS
The fact that all eligible participants were contacted, and a reasonably high response rate received, indicate that our findings are likely to be representative, and thus generalisable. Also, the incorporation of both positive and negative questions, which were accounted for in the analysis, minimized the potential impact of speculative responses thereby making the findings more reliable. Finally, the wordings of the questionnaire were in simple, plain language, with efforts made to ‘regularize’ medical terms, ensuring that the respondents would have understood the questions asked.
WEAKNESS
A higher response rate (≥ 90%) would have been welcomed, but, given that the responses are arguably representative and consistent with previously published data, the potential impact of this is likely to be minimal.
Conclusions
We conclude that, while most students have heard about breast cancer, the specific knowledge on its risk factors and early warning symptoms are poor, while the actual practise of BSE is very poor. While participants have an excellent attitude towards BSE, their Knowledge on its Timing and Frequency were poor, while that on Technique is only moderate. No significant predictors of BSE were identified, and popular sources of information are not in place for the respondents.
Recommendations
Firstly, health campaigns on breast cancer and BSE should be very specific on techniques, risk factors and symptoms, and emphasize more on the right methods, timing and frequency of the practices. Such programs are expected to be very effective and achieve long lasting impacts, given the hugely positive attitude of the respondents,
Secondly, more should be done to involve schools and religious institutions in the dissemination of information regarding breast cancers and BSE, given that these are popular and cheap avenues in Nigeria. In fact, including BSE and relevant breast cancers topics in the school curriculum of Nigerian (and overseas) senior secondary students is highly recommended, while religious institutions (churches and mosques), as well as healthcare workers, should be empowered to engage the masses on these issues.
Ethical considerations
Ethical clearance was obtained from the Griffith University Human Research Ethics Committee (GU Ref No: 2017/458). Participation was voluntary, and the Zonal Director in charge of the Otuocha PPSSC facilitated permissions for the study from the relevant State Agencies, school principals, the students and their parents.
Acknowledgements
We wish to acknowledge the support from Mrs Imelda Emeka, the Zonal Director of Education, Post Primary Schools Service Commission (PPSSC), Otuocha Zone of Anambra State, Nigeria.
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ANNEX 1
Footnotes
Conflict of interest statement
Both authors are involved in charity organizations which were involved in the delivery of a health symposium on breast cancer and BSE to female secondary students in Otuocha PPSSC, organized after the questionnaires for this study were returned.
Authors' contributions
Both authors contributed significantly in all aspects of the study.
References
- [1].Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin D, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136(5):E359-86. [DOI] [PubMed] [Google Scholar]
- [2].Anyanwu S. Breast cancer in eastern Nigeria: a ten year review. West Afr J Med 1999;19(2):120-125. [PubMed] [Google Scholar]
- [3].World Health Organization. WHO | Cancer. WHO 2017 2017-03-23 [cited 2017 November 20th]; Available from: http://www.who.int/mediacentre/factsheets/fs297/en/.
- [4].Omoyeni OM, Oluwafeyikemi PE, Irinoye OO, Adenike OO. Assessment of the knowledge and practice of breast self examination among female cleaners in Obafemi Awolowo University Ile Ife, Nigeria. IJCS 2014;7(1):239. [Google Scholar]
- [5].Harris JR, Lippman ME, Veronesi U, Willett W. Breast cancer. N Engl J Med 1992;327(6):390-8. [DOI] [PubMed] [Google Scholar]
- [6].Adebamowo C, Adekunle O. Case-controlled study of the epidemiological risk factors for breast cancer in Nigeria. Br J Surg 1999;86(5):665-8. [DOI] [PubMed] [Google Scholar]
- [7].Oluwatosin OA. Assessment of women’s risk factors for breast cancer and predictors of the practice of breast examination in two rural areas near Ibadan, Nigeria. Cancer Epidemiol 2010;34(4):425-8. [DOI] [PubMed] [Google Scholar]
- [8].Hallal JC. The relationship of health beliefs, health locus of control, and self concept to the practice of breast self-examination in adult women. Nurs Res 1982;31(3):137-42. [PubMed] [Google Scholar]
- [9].Tavafian S, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self-examination in a sample of Iranian women: an application of the Health Belief Model. BMC Women's Health 2009;9(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Isara A, Ojedokun C. Knowledge of breast cancer and practice of breast self examination among female senior secondary school students in Abuja, Nigeria. J Prev Med Hyg 2011;52(4). [PubMed] [Google Scholar]
- [11].Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2002;137(5_Part_1):347-60. [DOI] [PubMed] [Google Scholar]
- [12].Yakubu AA, Gadanya MA, Sheshe AA. Knowledge, attitude, and practice of breast self-examination among female nurses in Aminu Kano teaching hospital, Kano, Nigeria. Niger J Basic Clin Sci 2014;11(2):85. [Google Scholar]
- [13].Okobia MN, Bunker CH, Okonofua FE, Osime U. Knowledge, attitude and practice of Nigerian women towards breast cancer: A cross-sectional study. World J Surg Oncol 2006;4(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Doshi D, Reddy BS, Kulkarni S, Karunakar P. Breast self-examination: knowledge, attitude, and practice among female dental students in Hyderabad City, India. Indian J Palliat Care 2012;18(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Thomas DB, Gao DL, Ray RM, Wang WW, Allison CJ, Chen FL, Porter PH, Hu YW, Zhao GL, Pan LD. Randomized trial of breast self-examination in Shanghai: final results. J Natl Cancer Inst 2002;94(19):1445-57. [DOI] [PubMed] [Google Scholar]
- [16].Kösters JP, Gøtzsche PC. Regular self-examination or clinical examination for early detection of breast cancer. Cochrane Database Syst Rev 2003;(2):CD003373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Al-Haji KM, Moawed SA. Breast cancer, breast self-examination knowledge among female high school students in Riyadh city. ME-JN 2015;9(1):25-33. [Google Scholar]
- [18].Siahpush M, Singh GK. Sociodemographic variations in breast cancer screening behavior among Australian women: results from the 1995 National Health Survey. Prev Med 2002;35(2):174-80. [DOI] [PubMed] [Google Scholar]
- [19].Blamey RW, Wilson AR, Patnick J. ABC of breast diseases: screening for breast cancer. BMJ 2000;321(7262):689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Parkin DM, Muir CS. Cancer incidence in five continents. Comparability and quality of data. IARC Scientific Publications 1992(120):45-173. [PubMed] [Google Scholar]
- [21].Ihekwaba F. Breast cancer in Nigerian women. Br J Surg 1992;79(8):771-5. [DOI] [PubMed] [Google Scholar]
- [22].Okobia M, Osime U. Clinicopathological study of carcinoma of the breast in Benin City. Afr J Reprod Health 2001;5(2):56-62. [PubMed] [Google Scholar]
- [23].Neave LM, Mason BH, Kay RG. Does delay in diagnosis of breast cancer affect survival? Breast Cancer Res Treat 1990;15(2):103-8. [DOI] [PubMed] [Google Scholar]
- [24].Rossi S, Cinini C, Di Pietro C, Lombardi CP, Crucitti A, Bellantone R, Crucitti F. Diagnostic delay in breast cancer: correlation with disease stage and prognosis. Tumori 1990;76(6):559-62. [DOI] [PubMed] [Google Scholar]
- [25].Hisham AN, Yip C-H. Overview of breast cancer in Malaysian women: a problem with late diagnosis. Asian J Surg 2004;27(2):130-3. [DOI] [PubMed] [Google Scholar]
- [26].Adebamowo CA, Ajayi O. Breast cancer in Nigeria. West Afr J Med 1999;19(3):179-91. [PubMed] [Google Scholar]
- [27].Edino S, Ochicha O, Alhassan S, Mohammed A, Ajayi O. Clinico-pathological review of breast cancer in Kano. Niger J Surg 2000;7:70-5. [Google Scholar]
- [28].Newman LA, Alfonso AE. Age-related differences in breast cancer stage at diagnosis between black and white patients in an urban community hospital. Ann Surg Oncol 1997;4(8):655-62. [DOI] [PubMed] [Google Scholar]
- [29].Machiavelli M, Leone B, Romero A, Perez J, Vallejo C, Bianco A, Rodriguez R, Estevez R, Chacon R, Dansky C. Relation between delay and survival in 596 patients with breast cancer. Oncology 1989;46(2):78-82. [DOI] [PubMed] [Google Scholar]
- [30].Afzelius P, Zedeler K, Sommer H, Mouridsen H, Blichert-Toft M. Patient’s and doctor’s delay in primary breast cancer: Prognostic implications. Acta Oncol 1994;33(4):345-51. [DOI] [PubMed] [Google Scholar]
- [31].Khwaja M, Nirodi N, Lawrie J. Malignant tumours of the breast in Northern Savannah of Nigeria. East Afr Med J 1980;57(8):555-61. [PubMed] [Google Scholar]
- [32].Irurhe N, Raji S, Olowoyeye O, Adeyomoye A, Arogundade R, Soyebi K, Ibitoye A, Abonyi L, Eniyandunni F. Knowledge and awareness of breast cancer among female secondary school students in Nigeria. AJCR 2012;5(1):1-5. [Google Scholar]
- [33].Banjo A. Overview of breast and cervical cancers in Nigeria: are there regional variations. in Paper presentation at the International workshop on new trends in Management of breast and cervical cancers, Lagos, Nigeria. 2004. [Google Scholar]
- [34].Suh MA, Atashili J, Fuh EA, Eta VA. Breast self-examination and breast cancer awareness in women in developing countries: a survey of women in Buea, Cameroon. BMC Res Notes 2012;5(1):627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hermon C, Beral V. Breast cancer mortality rates are levelling off or beginning to decline in many western countries: analysis of time trends, age-cohort and age-period models of breast cancer mortality in 20 countries. Br J Cancer 1996;73(7):955-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Ghazali SM, Othman Z, Cheong KC, Lim KH, Wan M, Wan R, Kamaluddin MA, Yusoff AF, Mustafa AN. Non-practice of breast self examination and marital status are associated with delayed presentation with breast cancer. Asian Pac J Cancer Prev 2013;14(2):1141-5. [DOI] [PubMed] [Google Scholar]
- [37].Gwarzo U, Sabitu K, Idris S. Knowledge and practice of breast self-examination among female undergraduate students of Ahmadu Bello University Zaria, northwestern Nigeria. Ann Afr Med 2009;8(1). [DOI] [PubMed] [Google Scholar]
- [38].Adetule YC. Breast Self-Examination (BSE): a strategy for early detection of breast cancer in Nigeria. Ann Oncol 2016;27(suppl_9) doi: 10.1093/annonc/mdw575.020. [Google Scholar]
- [39].Anambra State PPSSC. PPSSC OTUOCHA ZONE. 2017. [cited 2018 11th December]; Available from: http://ppsscanambra.net/Otuocha.aspx
- [40].National Population Commission of Nigeria. Anambra (State, Nigeria) - Population Statistics, Charts, Map and Location. 2017. [cited 2017 30th Novemner]; Available from: http://www.citypopulation.info/php/nigeria-admin.php?adm1id=NGA004.
- [41].Segni M, Tadesse D, Amdemichael R, Demissie H. Breast self-examination: knowledge, attitude, and practice among female health science students at Adama Science and Technology University, Ethiopia. Gynecol Obstet (Sunnyvale) 2016;6(368):2161-0932.1000368. [Google Scholar]
- [42].Karayurt Ö, Özmen D, Çetinkaya AC. Awareness of breast cancer risk factors and practice of breast self examination among high school students in Turkey. BMC Public Health 2008;8(1):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].UNICEF. At a glance: Nigeria. 2013. [cited 2017 4th December]; Available from: https://www.unicef.org/infobycountry/nigeria_statistics.html#0.
- [44].US Department of State. Nigeria: International Religious Freedom Report 2009. 2009. [cited 2017 4th December]; Available from: https://www.state.gov/j/drl/rls/irf/2009/127249.htm


