Abstract
Objective
African-American children and adolescents experience an undue burden of disease for many health outcomes compared to their White peers. More research needs to be completed for this priority population to improve their health outcomes and ameliorate health disparities. Integrating hip hop music or hip hop dance into interventions may help engage African-American youth in health interventions and improve their health outcomes. We conducted a review of the literature to characterize hip hop interventions and determine their potential to improve health.
Methods
We searched Web of Science, Scopus, PsycINFO, and EMBASE to identify studies that assessed hip hop interventions. To be included, studies had to (1) be focused on a psychosocial or physical health intervention that included hip hop and (2) present quantitative data assessing intervention outcomes. Twenty-three articles were identified as meeting all inclusion criteria and were coded by two reviewers. Articles were assessed with regards to sample characteristics, study design, analysis, intervention components, and results.
Results
Hip hop interventions have been developed to improve health literacy, health behavior, and mental health. The interventions were primarily targeted to African-American and Latino children and adolescents. Many of the health literacy and mental health studies used non-experimental study designs. Among the 12 (of 14) health behavior studies that used experimental designs, the association between hip hop interventions and positive health outcomes was inconsistent.
Conclusions
The number of experimental hip hop intervention studies is limited. Future research is required to determine if hip hop interventions can promote health.
Keywords: Health behavior, Health literacy, Mental health, Adolescents, Hip hop
Introduction
Although African-Americans constitute only 13% of the US population, they suffer disproportionately from higher rates of disease and mental health problems [1–4]. African-American youth (children and adolescents) have higher rates of obesity, sexually transmitted infections, HIV, and diagnoses of conduct disorder than their White counterparts [5–7]. Furthermore, African-American youth are more likely than their White counterparts to suffer from negative consequences related to their health behaviors [8–10]. These differences are present even when the rates of their behaviors are comparable to or lower than Whites [9]. For example, African-American youth report drinking less frequently and consuming smaller amounts of alcohol than White youth but have higher rates of alcohol-related problems [8–10]. Moreover, recent research on the risk of suicide for African-American youth compared to White youth documents the severity of mental health disparities among African-American youth. The suicide rate among African-American youth doubled between 1993 and 2012 but decreased among White youth [11].
Moreover, for some African-American youth, these disparities exist in the context of inequalities, including few socioeconomic resources and poorer access to care compared to their White counterparts [12, 13]. For instance, African-American youth have less access to services for substance use disorders and comorbid mental health conditions [14]. The presence of disparities and inequities highlights a need for increased attention to interventions that address the physical and mental health of African-American youth.
African-American youth are in need of culturally competent interventions that address mental health and health behaviors because of their unique risk factors for mental health and physical health problems [15]. For instance, a recent study assessed the relationship between community violence and behavioral health outcomes in a sample of African-American adolescents who were predominately low-income and lived in an urban setting [16]. The authors reported an association between community violence exposure and poorer mental health, delinquent behaviors, substances, and risky sexual behaviors [16]. Other research has demonstrated an association between perceived racial discrimination and problem behaviors in preadolescent African-American youth [17]. Therefore, it is important that African-American youth have access to engaging interventions that resonate with their experiences.
Moreover, some research indicates that interventions that reflect the culture of a target population are more effective than standard treatments [18, 19]. Therefore, it is evident that there is a need to consider new strategies when developing interventions for African-American youth and that these interventions should consider African-American youth culture for improved engagement and health outcomes.
Integrating rap or hip hop music, a component of hip hop culture, into evidence-based treatments or developing new treatments is a potential strategy to engage African-American youth in health interventions. Hip hop culture emerged in The Bronx borough of New York City in the early 1970s and became the voice of African-American and Puerto Rican youth [20]. Hip hop culture is comprised of four elements, rap music, DJing, graffiti writing, and breakdancing [21]. Through lyrics spanning an array of often-ignored subjects from oppression to family, rap artists offer gritty perspectives relatable to many ethnic minorities and disenfranchised youth [22]. In addition to its musical influence, hip hop culture shapes communication, fashion, and other forms of cultural expression, particularly among African-Americans and Latinos [23].
Moreover, rap music is one of the most popular forms of music in America and is particularly popular among African-Americans [24]. Tyson [25] assessed music preferences among African-American adolescent boys. He reported that 97% reported “liking”rap music, and more than 50% reported buying at least one new CD a month [25]. According to the most recent Recording Industry Association of America 10-year consumer poll conducted among the general population (1998–2008), rap was the second most popular genre of music during that decade behind rock [26]. In 2015, based on an analysis by Spotify, a digital streaming service, of over 20 billion songs, “hip hop music” was the most popular musical genre globally among the general population [27].
Given that hip hop culture resonates so strongly with youth, it is plausible that using elements of hip hop (e.g., music and dance) could increase engagement and retention in health interventions. Indeed, there is a growing interest in the use of hip hop in health interventions. Recently, hip hop has been used to facilitate large-scale interventions. For instance, The Food and Drug Administration’s (FDA) Fresh Empire Campaign (https://freshempire.betobaccofree.hhs.gov) targets the hip hop peer group by using hip hop artists and hip hop culture as a way to prevent tobacco use among multicultural youth [28]. Extensive evaluation of Fresh Empire is ongoing and will assess the effectiveness of this large-scale intervention.
Theories for using hip hop for health literacy include the Theory of Reasoned Action (TRA) and Social Cognitive Theory [29]. TRA posits that a person’s behavior is determined by his or her intention to perform the behavior and that intentions are a function of attitudes and subjective norms [30]. Social Cognitive Theory (SCT) suggests that behavior is a function of personal (e.g. cognitive) and environmental factors [31]. Self-efficacy, the extent to one believes in his or her own ability, is a key element of SCT [31]. The developers of a program that aims to improve stroke knowledge among elementary school students note that their hip hop-based intervention was developed using TRA and SCT as a framework. Their program aims to increase self-efficacy and facilitate intentions to call 911 or communicate with their parents about stroke [29].
Theories for using hip hop for health behavior change are limited and not discussed in detail in the health behavior intervention studies that utilized hip hop [32–34]. However, some researchers have suggested that hip hop music is relevant in the context of behavior change because hip hop is a powerful form of social communication, social influence, and social norms [35]. Furthermore, some researchers argue that hip hop is a persuasive form of communication because it is engaging, repeatable, and participatory [35]. In some research studies, the use of hip hop is not theory-driven but instead used to facilitate engagement in response to participant preference [33]. For instance, the Hip-Hop to Health Jr. intervention team developed a hip hop DVD to facilitate physical activity in response to a request from the parents of participants and community partners (M. Fitzgibbon, Ph.D. oral conversation, January 25, 2017).
For nearly two decades, social scientists have explored methods for integrating rap music into therapeutic interventions with adolescents, specifically ethnic minorities [36, 37]. Through its varied subject matter, rap offers unique opportunities to engage youth and address presenting problems historically met with resistance [22]. There are numerous theoretical and conceptual articles that discuss how hip hop can be used to facilitate psychotherapy [38–43]. For instance, using hip hop to treat psychopathology is aligned with the discipline of music therapy. In music therapy, a therapist systematically uses music experiences (e.g., listening to music) to facilitate therapeutic discussions about topics such as emotions, memories, and identity issues [44]. More recently, clinicians have integrated models of music therapy with traditional psychological theoretical orientations, including psychodynamic, behavioral, and humanistic orientations [22].
To our knowledge, there has not been a literature review that summarizes types of hip hop health interventions, research methodologies, populations targeted, behaviors targeted, and the potential for hip hop to improve outcomes. The current paper seeks to fill this gap by conducting a scoping review of research studies that used hip hop in health interventions.
Methods
The authors conducted a scoping review of peer-reviewed journal articles that utilized hip hop interventions for health [45]. Scoping reviews differ from systematic reviews because they allow for mapping the existing evidence base with broad search criteria to address broad research questions [45]. Further, scoping reviews do not restrict or assess study quality [45]. The scoping review approach was chosen for this study to identify hip hop intervention targets (e.g., mental health) and to inform future systematic reviews.
Inclusion and Exclusion Criteria
The authors consulted with an Information Specialist at the National Cancer Institute to optimize search keywords and databases. The search ((“hip hop” or “hip hop” or “Brap”) AND (“health” or “intervention” or “therapy”)) was performed in Web of Science, Scopus, PsycINFO, and EMBASE. These four databases were selected to locate results across multiple fields including psychology, social sciences, medicine, and health. These searches produced a total of 3586 results. After removing duplicates and any publications that were not peer-reviewed journal articles, a total of 2201 articles were assessed. The literature search was conducted from September 2016 to January 2017. We included papers that were published by January 2017.
The authors included empirical, peer-reviewed journal articles published in English (Fig. 1). Titles, abstracts, and/or complete manuscripts were reviewed to determine if they met the following criteria: (1) focused on a psychosocial or physical health intervention that included hip hop (e.g., rap music, or hip hop dance) as a component and (2) included quantitative data describing the outcomes of the hip hopbased intervention. Theoretical and conceptual articles were excluded.
Fig. 1.
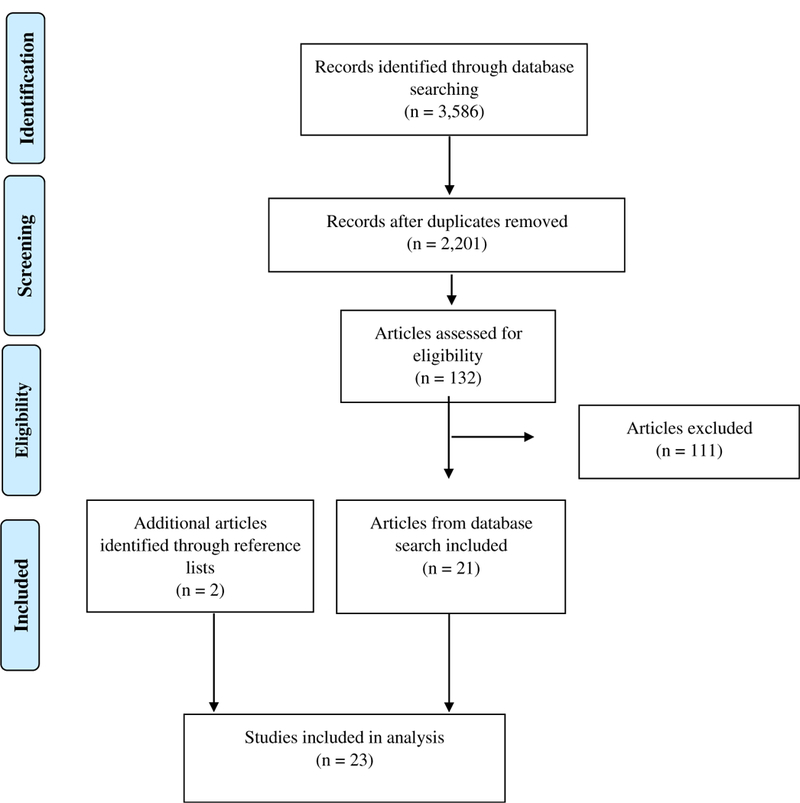
Search results and included articles
From a review of search result titles, 2069 articles were not related to hip hop or rap music and were excluded based on the title alone. From the 132 articles that had titles that appeared to meet inclusion criteria, abstracts were reviewed to confirm that the results fit within the scope of this review. Twenty-one of these articles were determined to fit eligibility criteria and were coded by a research team member for several features including target behavior, design/analysis of the study, intervention design, summary of measures, and results. Two additional articles were identified from reference lists in an article that was found from search results but was not an included article [46], yielding a total of 23 articles.
Two authors acted as coders, with each article being coded by a primary coder and reviewed by a secondary coder. Major sections of the codebook included intervention target, sample characteristics, study design, analysis, intervention conditions, measures, and results. The studies were organized by the following intervention targets: (1) health literacy, (2) health behavior, and (3) mental health. Mental health studies were those that included any psychopathology or mental well-being target (e.g., self-esteem). Health behavior studies included any intervention that tried to improve health by targeting a health risk factor (e.g., eating habits). Health literacy interventions included any studies that tried to increase knowledge about a health condition. Studies with multiple targets were organized by their dominant targets as determined by reviewers (e.g., [35, 47]).
Results
Descriptors of the 23 research studies that met criteria for inclusion in this review are summarized in Table 1. Given variations in study design and the fact that many studies did not use control groups, we could not make direct comparisons between studies, combine findings, or conduct a quantitative meta-analysis. Below we present a narrative summary and evaluation of hip hop interventions grouped by the type of health target with a focus on main findings.
Table 1.
Characteristics of studies that examine hip hop-based interventions for health promotion
| Author | Year | Intervention target | Sample characteristics | Design/analysis | Intervention | Measures | Results |
|---|---|---|---|---|---|---|---|
| Williams et al. [34] | 2008 | Health literacy |
N = 582 middle school students Groups: treatment group only Race/Ethn: majority Latino Age: 9 to 11 Setting: school |
Design: pre-test/post-test Follow-up period: post-test and 3 months |
Treatment: “Hip Hop Stroke” 3, 1-h sessions about stroke risk and symptoms that incorporated hip hop music and dance. Sessions took place at school. Music created by Doug E. Fresh Control: no control group used |
Questionnaires of stroke knowledge | Stroke localization: 20% correct before intervention, 93% correct immediately afterward, and 86% correct after 3-month delay; p = 0.001b The term “brain attack”: 16% pre-test, 95% immediate, 86% delayed; p = 0.001 Call 911 for stroke: 78% pre-test, 99.8% immediate, 98% delayed; p = 0.001 FAST stroke symptoms (facial droop and slurred speech) were better retained than non-FAST symptoms (headache and blurred vision) at 3 months (p = 0.001) |
| Williams et al. [45] | 2012 | Health literacy |
N: 71 parents of children who participated in Hip Hop Stroke Groups: treatment group only Race/Ethn: 72% non-Hispanic Black and 24% Hispanic Age: children aged 9 to 12 Setting: school |
Design: one-group pre-test/post-test Follow-up: no follow-up after post-test | Treatment: children participated in Hip Hop Stroke Program; parents assisted children with homework components. This study looked at parental recall of stroke information communicated by their child Control: no control group used |
Stroke symptoms Action plan FAST mnemonic |
Stroke localization changed from 51% baseline to 85% post-intervention, p < .01 Before the intervention, 3.9% of parents were able to identify the 5 cardinal stroke symptoms compared with 29.6% post-intervention (p < 0.001) The FAST mnemonic was known by 2.7% of participants before the intervention vs. 41% after post-intervention (p < 0.001) |
| Williams et al. [47] | 2012 | Health literacy | Children from 2 schools in Central Harlem N = 104 students completed both pre-tests and immediate post-tests and 85 completed pre-tests, immediate post-tests and delayed protests Groups: treatment group only Race/Ethn: 75% non-Hispanic black and 25% Hispanic Age: 9 to 11 Setting: school |
Design: one-group pre-test/post-test Follow-up: immediate post-test and 15-month delayed post-test | Treatment: a multimedia stroke literacy intervention—three 1-h assembly-style sessions over 3 consecutive days. The program includes rap music, cartoons, a video game, and homework activities. Control: no control group used |
Stroke knowledge Intent to call 911 for stroke |
Intent to call 911 increased immediate post-test (85.6% correct, x2 = 17.86, p = 0.0005) and 15 months delayed post-test (71.76% correct, x2 = 15.47, p = 0.0015) compared to pre-test (55.8% correct) Stroke localization increased immediate post-test (91.4% correct, x2 = 61.08, p < 0.0001) and delayed post-test (80% correct, x2 = 43.46, p < 0.0001) compared to pre-test (36.54% correct) Knowledge of signs and symptoms, increased immediate post-test (M = 5.30, SD 0.095, t (206) = 12.12, p < 0.0001) and delayed post-test (M = 4.73 SD = 1.07, t(187) = 7.99, p < 0.0001) compared to post-test (3.24, SD = 1.45) |
| Williams et al. [48] | 2014 | Health literacy |
N = 210 Groups: treatment group only Race/Ethn: 65% Hispanic Age: children aged 9 to 12 Setting: school/home |
Design: one-group pre-test/post-test Follow-up: immediate post-test and 7-week delayed post-test | Treatment: children assembled in a school computer lab and played a stroke education game for 15 min and completed an immediate post-test. Children were given a card with information to access the game at home and then participated in a delayed (7 weeks) post-test. Control: no control group used |
Stroke action (calling 911) Knowledge of stroke symptoms Stroke localization in the brain stroke alias |
Knowledge of stroke symptoms increased significantly between pre-test and immediate post-test (p < 0.05)c Stroke localization increased significantly between pre-test and immediate post-test (p < 0.05)c Knowledge of 3 symptoms (sudden imbalance, sudden facial droop, and sudden headache) increased between immediate post-test and delayed post-test (p < 0.05)c |
| Noble et al. [46] | 2015 | Health literacy |
N = 75 students participated in pre-tests and 68 completed post-tests Groups: treatment group only Race/Ethn: majority African-American (exact demographics not reported) Age: 9–11 Setting: school |
Design: one-group pre-test/post-test design Follow-up period: immediate post-test and 3 month delayed post-test |
Treatment: Three 60-min sessions over 3 days; songs, dance, skits, animated films Control: no control group used |
Alzheimer’s disease (AD) knowledge Personal/family experience with AD |
AD knowledge improved from pre-test to post-test: localization—brain: 74% correct pre-test compared to 89% post-test (x2 = 5.2, p = 0.02), and 86% 3-month delay (x2 = 3.0, p = 0.09) Localization—remembering = 62% correct pre-test compared to 94% post-test (x2 = 19.6, p < 0.001), and 91% 3-month delay (x2 = 15.7, p < .001) Localization—hippocampus = 10% correct pre-test compared to 83% post-test (x2 = 70.9, p < .001), and 78% 3-month delay (x2 = 62.2, p < 0.001) Sign and symptom: M = 2.4, SD = 1.4 pre-test compared to 5.4, SD = 0.08 post-test (t = 13.9, p < 0.001), and 4.17, SD = 1.3-month delay (t = 10.1, p < .001) |
| Ware et al. [49] | 2015 | Health Literacy |
N = 50 Groups: video (rap) counseling session group (n = 26); verbal counseling session group (n = 24) Race/Ethn: not directly reported Age: 18–51 years old Setting: university |
Design: randomized controlled trial Follow-up period: immediate post-test (immediately following presentation) |
Treatment: participants watched Coumadin Rap Song (CRS) YouTube Video (4 min in length) Control: scripted counseling cessation where a pharmacist presents the same information about Coumadin (4 min in length) |
Knowledge of Coumadin (10 questions) | Score changes between pre-test and post-test did not differ significantly between the video-based rap counseling and the verbal-based counseling (p = 0.18) The video-based rap counseling group showed significant improvements in 3 individual questions between pre-test and post-test (p = 0.019, p = 0.002, p = 0.046) The verbal-based counseling group showed significant improvements in 4 individual questions between pre-test and post-test (p = 0.028, p = 0.004, p = 0.036, p = 0.018) |
| Cella et al. [60] | 1992 | Health behaviors |
N = 309 students Groups: treatment group only Race/Ethn: majority African-American (58%) and Latino (19%) Age: 11.9 (range 10–14) Setting: school |
Design: 1-group pre-test/post-test design Follow-up period: after each assembly |
Treatment: two 40-min assemblies held at each school. The first focused on the delivery of anti-smoking messages and included 12-min rap video about quitting smoking. The second was a rap contest where the children delivered the anti-smoking messages to their peers. Control: none |
Smoking attitudes and behavior | No difference in smoking behavior between pre-test (3.2%) and post-test (5.7%) No difference in negative attitudes toward smoking between pre-test (49.2) and post-test (49.5) |
| Quirk et al. [59] | 1993 | Health behaviors |
N = 214 young women Groups: rap video vs. standard video Race/Ethn: 49% Caucasian; 35.5% Latino Age: 14 to 25 Setting: family health centers |
Design: randomized controlled trial Follow-up period: post-intervention and 1-month follow-up |
Treatment: peer-delivered AIDS prevention intervention (AIDS rap videotape and several brochures). Control: health care provider-delivered AIDS prevention intervention (used patient-centered counseling) |
AIDS prevention knowledge AIDS prevention attitudes AIDS prevention behavior |
Both groups showed increases in knowledge between pre-intervention and post-intervention (p < 0.03) For the participants who returned for a 1-month follow-up information was retained over time for basic AIDS facts (p < 0.004), preventing sexual transmission (p < 0.002) and preventing IV drug transmission (p < 0.001) There were no overall changes in attitudes or behaviors reported at post-test or follow-up |
| Sussman et al. [52] | 1995 | Health behaviors | Study 1 N = 267 Groups: rap video vs. soap opera video Race/Ethn: 41% African-American; 45% Latino Age: mean age 12.3 Setting: school |
Design: randomized controlled trial at classroom level Follow-up Period: immediate post-test | Treatment: rap video Control: soap opera video |
Smoking knowledge Intention to smoke Smoking refusal assertion self-efficacy Attitudes toward video Video-specific content knowledge |
At post-test, about 25% of participants indicated they intended to smoke in the future or were uncertain about smoking in the future, with no difference by condition (p > 0.1) |
| Study 2 N = 450 Groups: videos vs. discussion Race/Ethn: 31% African-American; 56% Latino Age: mean age 12.6 Setting: obstetrics clinic |
Design: randomized controlled trial at classroom level Follow-up Period: immediate post-test, 3-month follow-up | Treatment: viewed rap and soap opera videos Control: discussed smoking prevention |
Video questions (video group only) Response to being asked to smoke Future smoking plans Difficulty of refusing a cigarette from a best friend |
In the video group, the soap opera video was liked more than the rap video (X2s ≥ 7, ps ≤ 0.01) No pre-test-post-test changes were observed across conditions for those who had already smoked (p > 0.01) Intention to smoke changed significantly in both conditions for non-smokers (t values ranged from −3.75 to −7.81, all ps < 0.001). At the 3-month follow-up, a decrease in intention to use was observed across all smoking statuses and both conditions (ps > 0.1) |
|||
| Connelly et al. [53] | 1996 | Health behaviors |
N = 60 pregnant teenagers Groups: rap video vs. standard video Race/Ethn: African-American Age: 14 to 18 Setting: obstetrics clinic |
Design: two-group pre-test/post-test design Follow-up Period: post-video viewing | Treatment: rap music video “You and Baby Too!” narrated by a 20-year-old African-American male Control: “Building Better Babies” educational video. Narrated by a 40-year-old White female |
Nutrition education | No significant difference in learning post-test between rap video group (pre-test: M = 14.7, post-test, M = 23.3) and standard video group (pre-test: M = 15.37, post-test M = 24.53) Significant improvement in post-test scores regardless of method p ≤ .0001 |
| Fitzgibbon et al. [51] | 2005 | Health behaviors |
N = 409 (197 intervention and 212 control) Groups: 1 treatment (6 schools) and 1 control (6 schools) Race/Ethn: majority Black with 12.7% Latino in the control group Age: intervention group = 4.05 years, control group = 4.233 Setting = 12 head start programs |
Design: randomized controlled trial Follow-up period: 1 and 2 years |
Treatment: child component (45-min class 3 times a week for 14 weeks; 20-min lesson, 20 min of physical activity) and parent component (weekly newsletter, homework) Control: child component (general health intervention; 20-min class once a week for 14 weeks) and parent component (weekly newsletter) |
BMI, diet (total fat, SFA, dietary fiber), TV viewing, exercise frequency, and exercise intensity | No difference in adjusted BMI mean change scores between intervention (M = .06, SE = 0.05) and control group (M = 0.13, SE = 05) immediately following intervention Intervention condition had smaller increases in adjusted BMI at the year 1 post-intervention follow-up (intervention: average increase in adjusted BMI change scores 0.06 kg/m2, control: average increase in adjusted BMI 0.59 kg/m2, p = 0.012) Intervention condition had smaller increases in adjusted BMI change scores at the year 2 post-intervention follow-up (intervention average increase in adjusted BMI change scores 0.54 kg/m2, control average increase in adjusted BMI 1.08 kg/m2, p = 0.022) No difference in adjusted BMI z score at any time follow-up time Food intake/physical activity outcomes were not significant, except for saturated fat intake at year 1. Intervention condition consumed a smaller percentage of dietary saturated fat than control condition (intervention = 11.6% saturated fat, control group = 12.8% saturated fat, p = 0.002) |
| Fitzgibbon et al. [54] | 2006 | Health behaviors |
N = 389 (196 intervention and 193 control) Groups: 1 treatment (6 schools) and 1 control (6 schools) Race/Ethn: majority Latino (89% control and 73% intervention group) Age: intervention group = 4.23 years, control group = 4.25 Setting: 12 head start programs |
Design: randomized controlled trial Follow-up period: 1 and 2 years |
Treatment: child component (45-min class 3 times a week for 14 weeks; 20-min lesson, 20 min of physical activity) and parent component (weekly newsletter, homework) Control: child component (general health intervention; 20-min class once a week for 14 weeks) and parent component (weekly newsletter) |
BMI, dietary intake, physical activity | Immediate post-intervention changes in BMI z or BMI z change score not different by intervention (BMI = 0.11 kg/m2 intervention vs. 0.13 kg/m2 control, p = 0.89) (BMI Z = 0.07 intervention vs. 0.05 control, p = .85) At 1-year follow-up, no difference between groups in BMI or BMI z score change score (intervention = 0.33 kg/m2, control = 0.48 kg/m2, p = 0.46) (BMI Z = 0.00 intervention vs. 0.07 control, p = 0.56) 2-year follow-up no difference between groups in BMI or BMI z score change score (intervention = 0.46 kg/m2, control = 0.70 kg/m2, p = 0.34) (BMI Z = −.13 intervention vs. 0.00 control, p = 0.34) No difference in adjusted BMI z score at any time follow-up time Food intake/physical activity outcomes were not significantly different by group |
| Lemieux et al. [36] | 2008 | Health behaviors |
N = 306 high school students Groups: 1 treatment school, 2 control schools Race/Ethn.: majority Black and Latino Age: high school (average age was 16) Setting: high school |
Design: quasi-experimental: (no random assignment) Follow-up period: 3 months |
Treatment: health classes, hip hop music HIV intervention. Six students wrote, recorded, and disseminated intervention. Song “Life is too Short” addressed attitudes and social norm about sex and emphasized condom use. CDs distributed, in class presentation Control: health class only, HIV transmission and prevention information |
Attitudes about condom use HIV prevention behaviors (condom use and HIV testing) |
Marginally significant decrease in favorability of condoms among control but not treatment group (F (1, 249) 3.5, p = .08); time 1 = M = 4.15, SD = .61; time 2: M = 4.04, SD = .69). No change was found among participants in the treatment group (time 1: M = 3.96, SD = 0.63; time 2: M = 3.98, SD = .61) Marginally significant increase in perceived normative support among participants in the treatment condition (F (1, 240) = 3.2, p = 0.07) (time = M = 3.59, SD = .52; time 2: M = 3.68, SD= .58) whereas there was no change among participants in the control condition (time 1: M = 3.73, SD = .60; time 2: M = 3.69, SD = .66) Those in the treatment condition developed greater perception of vulnerability to HIV (F (1, 251) = 3.44, p = .06). No change among control condition Marginally significant interaction between time and condition on for HIV preventative behavioral skills (F (1, 252) 5.86, p = 0.02, 2.023, d = 0.46) Participants in the treatment condition increased (time 1: M = 3.59, SD = .60; time 2: M = 3.74, SD = .63), whereas participants in the control condition showed essentially no change (time 1 = 3.79, SD = .70; time 2 = 3.77, SD = .73) |
| Turner-Musa et al. [39] | 2008 | Health behaviors |
N = 68 middle school students Groups: treatment and control group Race/Ethn.: majority Black Age: middle school (mean age 13) Setting: after-school program |
Design: quasi-experimental (no intervention control) Follow-up period: 6 months |
Treatment: ten 2-h sessions of after-school substance abuse and HIV/AIDS prevention curriculum. Hip hop elements: creating a rap, discuss negative and positive characteristics of hip hop and it relates to HIV/AIDS preventions Faculty and staff of host schools participated in Hip Hop 101, a 4-h workshop Control: no intervention |
Survey of alcohol, tobacco, drug, HIV, sex, family, and school bonding. The survey assessed attitudes, beliefs, decision-making, and knowledge | No difference in 30-day drug use, attitudes toward drugs, drug risk perception, HIV/AIDS knowledge, and sexual efficacy between intervention and control groups at 6 months’ post-assessment (independent samples t test and chi-square)c Supplemental analysis: paired sample t tests indicated the intervention group participants had greater mean differences from baseline topost-survey assessments in drug risk perception, t = 2.06 (38), p < .05 and HIV/AIDS knowledge, t = 2.93 (38), p < 0.01. No mean differences for comparison group participants |
| Robinson et al. [58] | 2010 | Health behaviors |
N = 261 African-American girls and their parents/caregivers Groups: treatment and control group Race/Ethn.: African-American Age: 8 to 10 years old Setting: school, after school, and home |
Design: randomized controlled trial Follow-up period: 6, 12, 18, and 24 months |
Treatment: after-school hip hop, African and step dance classes and a home/family intervention to reduce screen media time Control: information-based health education |
BMI, fasting total cholesterol, LDL-cholesterol, incidence of hyperinsulinemia and depressive symptoms | Changes in BMI were not observed by group (adjusted mean difference = 0.04, CI = −0.18, 0.27) Fasting total cholesterol (adjusted mean difference = −3.49, CI = −5.28, −1.70), LDL-cholesterol (adjusted mean difference = −3.02, CI = −4.74, −1.31) hyperinsulinemia (RR = 0.35, CI = 0.13, 0.93) and depressive symptoms (RR = −0.21, CI = −0.42, −0.001) fell more per year in the treatment group than in the control group and there were effects by television viewing at baseline (p = 0.02) and having unmarried parents (p < 0.01) |
| Fitzgibbon et al. [55] | 2011 | Health Behaviors |
N = 68 middle school students Groups: treatment and control group Race/Ethn.: majority Black Age: middle school (mean age 13) Setting: after-school Program |
Design: randomized controlled trial Follow-up period: 1 year |
Treatment: child component (45-min class 2 times a week for 14 weeks; 20-min lesson, 20 min of physical activity). Parent component included a weekly newsletter and homework Control: child component (general health intervention; 20-min class once a week for 14 weeks) and parent component (weekly newsletter) |
BMI, dietary intake, physical activity | Immediate post-intervention changes in BMI z or BMI z change score not different by intervention (BMI = 0.11 kg/m2 intervention vs. 0.22 kg/m2 control, p = 0.17) (BMI Z = 0.08 intervention vs. 0.12 control, p = 0.28). No difference in adjusted BMI z score. Greater change in moderate to vigorous physical activity in intervention group (M = 109.9, SD = 2.0) compared to the control group (M = 102.5 SD = 2.0), p = 0.02 No difference between groups in diet and marginally significant difference in screen time (p = 0.05) with the intervention group reporting less screen time |
| Romero [35] | 2012 | Health behaviors |
N = 73 Groups: treatment group only Race/Ethn: 75% Mexican/Mexican American; 6% mixed ethnic heritage with Mexican descent; 4% American Indian Age: 11–16 (grades 6–9) Setting: school |
Design: one-group pre-test/post-test Follow-up period: no follow-up after post-test |
Treatment: 10 interactive 50-min lessons (twice a week during science/health classes) focusing on increasing physical activity and addressing neighborhood barriers; program based on Social Cognitive Theory, Critical Hip Hop Pedagogy, and feedback from stakeholders Control: no control group used |
Frequency of physical activity self-efficacy neighborhood barriers to physical activity |
Among girls, a significant increase in vigorous physical activity (pre-test 1.97 days of activity in a week, post-test 2.97 days of physical activity in a week, t (35) = −2.88 p < 0.05) and increased self-efficacy (pre-test score 2.75, post-test score 3.19, t (35) = −0.2.94 p < 0.05). No change in days spent dancing outside of Age: 11–16 (grades 6–9) Setting: school intervention, confidence in dancing, barriers to exercise, barriers in location, or neighborhood barriers Boys showed significantly decreased perceptions of neighborhood barriers (pre-test score 1.63, post-test score 1.43, p < 0.05). No change in physical activity, confidence, barriers to location, and barriers to exercise |
| Fitzgibbon et al. [56] | 2013 | Health behaviors |
N = 147 Groups: 1 treatment (2 schools) and 1 control (2 schools) Race/Ethn: Latino (945) Age: 4.51 Setting: 4 public schools |
Design: randomized controlled trial Follow-up period: 1 year |
Treatment: child component (45-min class 3 times a week for 14 weeks; 20-min lesson, 20 min of physical activity). This version had a Spanish language CD. Parent component included 30 min. Exercise session plus option 6 weekly classes on eating and exercise and weekly newsletter Control: child component (general health intervention; 20-min class once a week for 14 weeks) and parent component (weekly newsletter) |
BMI, dietary intake, physical activity | Immediate changes in BMI z or BMI z change score not different by intervention (BMI = 0.16 kg/m2 intervention vs. 0.09 kg/m2 control, p > .05) (BMI Z = 0.00 intervention vs. 0.03 control, p > 0.05) 1-year changes in BMI z or BMI z score change scores not different by intervention (BMI = −0.51 kg/m2 intervention vs. −0.68 kg/m2 control, p > 0.05) (BMI Z = −.51 intervention vs. −0.54 control, p > 0.05) 1-year change in adjusted BMI z change score was greater in control group (−0.43) compared to control (−0.65), p < 0.05 No difference in diet or physical activity |
| Kong et al. [57] | 2016 | Health behaviors |
N = 618 Groups: 1 treatment (9 schools) and 1 control (9 schools) Race/Ethn: majority African-American (94%) Age: 4.27 Setting: 18 public schools |
Design: randomized controlled trial Follow-up period: 1 year |
Treatment: child component (45-min class two times a week for 14 weeks; 20-min lesson, 20 min of physical activity). Parent component included a weekly newsletter and homework Control: child component (general health intervention; 20-min class once a week for 14 weeks) and parent component (weekly newsletter) |
BMI, dietary intake, physical activity | 1-year changes in BMI z or BMI z change score not different by intervention (BMI = 0.30 kg/m2 intervention vs. 0.43 kg/m2 control, p = 0.26) (BMI Z = 0.08 intervention vs. 0.10 control, p = 0.83) Intervention group had larger changes on the healthy eating index compared to the control group p = 0.02 |
| Williams et al. [50] | 2016 | Health behaviors |
N = mean total of 225 in two baseline sales but then various numbers for each sale (149 in immediate post-intervention; 133 in delayed sales) 5th graders (ages 8–11) Groups: intervention (2 schools) and control (1 school) Race/Ethn: not directly Reported Age: 3rd through 5th graders (ages 8–11) Setting: School |
Design: quasi-experimental design (no intervention control) Follow-up period: immediate post-intervention food sale, 7-day post-intervention food sale, and 12-day post-intervention food sale |
Treatment: assembly-style program, three 1-h sessions on 3 consecutive days (uses music and tries to present healthy choices as “cool” choices) Control: no intervention |
Individual food item chosen Calories in food itemchosen |
In the intervention group, there was a 20% decline of calories (baseline = 179 cal, immediate post-test 144 cal, 20% reduction, p < 0.01) in selected foods No change in control group (baseline = 167 cal, immediate post-test = 186 cal) |
| Staum [42] | 1993 | Mental health |
N = 12 Groups: treatment group only Race/Ethn: not reported Ages: 5 to 14 Setting: residential facility for homeless youth |
Design: one-group post-assessment only Follow-up period: responses measured daily (days 1–40); no follow-up after last session |
Treatment: alternating non-music verbal counseling sessions and musical counseling sessions. The program was 1 h each day for 40 days (5 days a week for 8 weeks) Control: no control group used |
Problem-solving skills | No change in problem-solving skills after music sessions compared to verbal counseling sessions No test statistics or p values reporteda |
| Tyson [40] | 2002 | Mental health |
N = 11 (5 in treatment group and 6 in comparison group) Groups: treatment group (hip hop therapy) and comparison group (regular therapy sessions) Race/Ethn: majority African-American Ages: 15.4 (SD = 0.5) Setting: residential facility for homeless youth |
Design: pre-test/post-test comparison group Follow-up period: no follow-up after last session |
Treatment: hip hop therapy group sessions; development of group rules/goals; listening to part of a rap song and then discussion reactions/thoughts/feelings led by PI. All songs had themes relating to self-identity, peace, unity, cooperation, and group progress Control: standard group sessions with concentration on self-concept enhancement and improved peer relations |
Index of peer relations Self-concept | Intervention group had a decrease in negative peer relations scores (pre-test group mean 38.40, SD = 4.56) and post-test 36.80, SD = 5.02, t (4) = 3.14, p = .035; not significant when controlling for pre-test No significant change in peer relations for comparison group (pre-test group mean = 41.33, SD = 3.50, post-test = 40.33, SD = 3.44, t (4) = 2.24, p = 0.076) No change in self-concept for either group, p > 0.05 |
| Olson-McBride and Page [41] | 2012 | Mental health |
N = 18 across three groups (group 1 = 6; group 2 = 7; group 3 = 5) Groups: 3 therapy groups—two from alternative schools and one from a transitional living program (all groups received the same intervention) Race/Ethn: majority African-American (17/18), 1 White Age: group 1 = 14.85, group 2 = 17.29, group 3 = 15 Setting: alternative school and transitional living program |
Design: one-group post-assessment only Follow-up period: no follow-up |
Treatment: 9 group sessions (each lasting 45–60 min) based on Maki and Mazza’s R.E.S. model—Rap and R&B music was used in the sessions (at least 2 session group members selected music, the remaining were selected by the facilitator) Control: no control group used |
Measures of self-disclosing statements | The number of self-disclosure statements varied across the 3 groups over the 9 sessions. For example, at session 1, 11.94% of statements included self-disclosure for group 1 compared to 23.08% for group 2 and 9.91% for group 3. The authors did not formally test differences in disclosures |
M mean, SD standard deviation, Ethn ethnicity
The authors report conducting statistical tests but did not report test statistics or p values
The authors did not report the chi-square statistics
Test statistics and p values were not reported
Health Literacy
Six studies focused on improving youth understanding of diseases and medication [32, 48–52] (Table 1). Five studies took place in an elementary school setting and one in a university (see Table 1). In four studies, the authors collected data from students between ages 8 and 12 [32, 48, 49, 51] and in one study data was collected from parents of children aged 9 to 12 [50]. In the final study, data was collected from college students aged 18 to 51 [52]. The sample sizes of the studies with elementary students ranged from 75 to 582 [32, 48, 49, 51]. The study with parents of elementary students had a sample size of 71 [50]. The study with college students had 50 participants [52]. All interventions that were delivered in elementary schools included students that were majority African-American and Latino (Ware [52] did not report race or ethnicity). Five studies used a one-group pre-post-test design [32, 48–51] and one study used a randomized controlled trial [52].
Five health literacy studies were conducted by the same authors and used similar programs. Three studies were based on the hip hop stroke literacy program [32, 50, 51]. The Hip Hop Stroke program is a multimedia program that includes hip hop music and a dance program that aims to teach children the symptoms of stroke and to call 911. These studies aim to increase the likelihood that children will contact emergency response systems if a family member has a stroke and to encourage children to talk to their family members about stroke [50]. The program includes rap music, cartoons, a video game, a comic, and role play. One study focused specifically on the Hip Hop Stroke video game [49]. The video game was synced to a hip hop song with educational lyrics about stroke [49]. The fourth study used the Old-School Hip Hop program which was designed to increase Alzheimer’s disease health literacy among children [48]. This program used dance, role play skits, a rap about Alzheimer’s disease, and animated films. The aim of this program is to encourage youth to implement safety measures for loved ones affected by Alzheimer’s disease. Participants in the final study were randomized to either a Coumadin Rap Song (CRS) YouTube® video or verbal patient counseling about Coumadin. The aim of this study was to determine if a Coumadin rap song could improve students’ ability to comprehend complex medication regimens. The CRS involves two pharmacists rapping about 16 educational points ranging from food-drug interactions to pharmacokinetics [52]. Participants in the control group received the same information formatted in a scripted 4-min counseling session [52].
Studies that assessed the effect of Hip Hop Stroke on children’s stroke literacy indicated that students increased their stroke literacy knowledge compared to baseline [32, 51]. The study that focused on the Hip Hop Stroke video game also reported that students increased their stroke knowledge compared to baseline [49]. Parents’ knowledge about stroke literacy also increased compared to baseline [50]. Similarly, Alzheimer’s disease knowledge increased compared to baseline [48]. The study that used the Coumadin Rap Song reported that both groups increased their knowledge, but there were no statistically significant differences by group [52].
Health Behaviors
Fourteen studies focused on a variety health behaviors including obesity, physical activity, HIV prevention behaviors, substance use, tobacco use, and food choices [34, 35, 47, 53–63] (Table 1). Among the nine studies that focused on diet and/or physical activity, eight studies utilized school as a location for recruitment and implementation: these studies took place in school, preschool, and afterschool settings [34, 53–57, 60, 61]. The other study took place in an obstetrics clinic that provided care to pregnant teenagers [59]. The remaining five (of 14) health behavior studies focused on tobacco, HIV/AIDS, and substance abuse and took place in schools, a family health center, and an after-school program [35, 47, 58, 62, 63].
Among all health behavior studies there were a wide range of ages including preschool-aged [54, 55, 57, 60], elementary school-aged [53], middle school-aged [34, 56, 58, 61, 63], high school-aged students [35, 47, 59], and youth ranging from 14 to 25 [62]. The samples included youth that were majority African-American [47, 54, 56, 59–61], African-American and Latino [35, 58, 63], Latino, [34, 55, 57], or Caucasian [62] (Williams and colleagues [53] did not report race/ethnicity). Overall, these studies have sample sizes ranging from 60 to 618. Four studies utilized a quasi-experimental design [35, 47, 53, 59], two studies used a one-group pre-test/post-test design [34, 63], and eight studies utilized a randomized controlled trial design [54–58, 60–62].
The type of hip hop intervention used varied across studies. Three studies involved watching a rap videotape about the health behaviors which included HIV [62], nutrition [59], and smoking [58]. Three studies included youth writing and performing their own rap song [35, 47, 63], and one study included listening to music during intervention sessions [53] to help make healthy choices appealing. Five studies utilized the Hip Hop to Health Jr. intervention which used rap music as part of a diet and physical activity intervention [54–57, 60]. In these studies, youth were provided a CD with rap songs about healthy eating and physical activity. Two studies used hip hop music and dance as a part of a physical activity intervention [34, 61].
Across these studies, the results varied with most of studies indicating no differences by group for primary outcomes. Fitzgibbon and colleagues [54] found that children in the hip hop intervention reported smaller increases in body mass index (BMI) at the 1- and 2-year follow-ups than their peers in the control group. They also reported mostly nonsignificant differences in reported health behavior (dietary, TV viewing, and exercise) outcomes. This finding contrasted with the other Hip Hop health Jr. studies which did not find differences in BMI at follow-up times that varied between immediately post-intervention and 2 years [55–57, 60]. However, two of these studies did report behavior changes related to diet and physical activity for the intervention group but not the control group [56, 60].
Among the other four studies [34, 53, 59, 61] that targeted physical activity and nutrition, one study reported results that differed by gender [34]. The physical activity intervention was successful in increasing female participants’ exercise and self-efficacy and male participants’ perceptions of neighborhood barriers to participating in physical activity. Connelly and colleagues reported no difference by group in nutrition education [59]. Robinson and colleagues reported lower fasting total cholesterol, LDL-cholesterol, hyperinsulinemia, and depressive symptoms in the treatment group compared to the control group [61]. However, they did not find any differences by group for BMI [61]. Williams and colleagues [53] found that children in the intervention condition purchased less calorically dense and unhealthy foods after the intervention.
Among studies that targeted smoking, one study reported no effect of the intervention by group [58] and a second study reported no change in smoking behavior or attitudes from pre- to post-test in the one group studied [63].
Among the three studies that targeted HIV/AIDS, one reported greater improvements in the intervention group and two reported no difference by group. Lemieux and colleagues [35] found that participants in the intervention condition were more likely to use condoms and have undergone an HIV test than those in the control condition. They also reported that decreases in favorability of condoms were observed among the control group but not the treatment group (the differences were marginally significant). Turner-Musa et al. [47] reported no difference in 30-day drug use, attitudes toward drugs, drug risk perception, HIV/AIDS knowledge, and sexual efficacy between intervention and control groups at 6 months’ post-assessment. Turner-Musa and colleagues [47] also reported that students who participated in the intervention were more knowledgeable about HIV/AIDS than participants in the control group at 6-month follow-up. Quirk and colleagues [62] reported no differences in AIDS prevention knowledge, attitudes, or behavior by group.
Mental Health
Three studies targeted aspects of mental health including problem-solving, self-esteem, and peer relations [25, 64, 65] (Table 1). The studies took place in residential treatment facilities for homeless youth and a transitional living program. Two studies targeted adolescent youth and one targeted youth ranging from young children to adolescence [25, 64, 65]. Two studies focused on African-American youth [25, 64] (Staum [65] did not report race/ethnicity). Overall, the studies had small sample sizes, ranging from 11 to 18. None of these studies used experimental designs. Two used a one-group post-assessment only design [64, 65], and one used a two-group pre- post-test design [25].
The use of hip hop varied across studies. Staum utilized a combination of music counseling sessions and non-music counseling sessions [65]. The 1-h music sessions involved singing rap songs as well non-rap music activities. Tyson had participants listen to rap songs and discuss their reactions, thoughts, and feelings to music [25]. Tyson chose music that related to self-identity, peace, unity, cooperation, and group progress [25]. Olson-McBride and Page had participants select hip hop music and used hip hop music to facilitate self-disclosure about experiences and emotions [64]. Participants also collaborated to write a poem [64].
In terms of results, Staum reported no change in problem solving skills in the non-music verbal counseling session and musical counseling session groups [65]. Tyson reported a significant decrease in peer relation scores (suggesting improved peer relations) post-intervention among those in the hip hop therapy group but not in the standard group [25]. The Index of Peer Relations (IPR) was used to measure the severity of peer-related problems [66]. However, this result was no longer significant when controlling for the peer relations scores pre-test. Olson-McBride and Page assessed self-disclosure statements among three therapy groups who received the same intervention. Groups 1 and 3 consisted of individuals with externalizing behaviors who were in an alternative school. Group 2 consisted of individuals who exhibited fewer externalizing behaviors than groups 1 and 3 who were placed in a transitional living program due to involvement in the child welfare system. Olson-McBride and Page reported that the number of participant self-disclosure statements (e.g., expressing feelings or sharing personal information) varied across the three groups and between group sessions [64]. For example, group 3 had a higher average percentage of self-disclosing statements compared to groups 1 and 2 [64]. They noted that this difference may be related to baseline externalizing behaviors.
Discussion
This review examined hip hop as a tool for facilitating engagement and improving outcomes in health behavior interventions, health literacy interventions, and mental health interventions. This literature extends over a 25-year period and includes studies with children, adolescents, and young adults. The populations that were studied were predominantly African-American and Latino youth. This review revealed that there were only 23 studies conducted over the 25-year period and that many studies utilized non-experimental designs. Therefore, it is difficult to draw conclusions due to threats to internal validity. Among the 12 (of 14) health behavior studies that used experimental designs, the hip hop intervention groups had improved outcomes compared to the control group on some measures in five studies [53, 54, 56, 60, 61]. All but one of the health literacy studies did not include a control group [32, 48, 50, 51]. In these studies, the authors reported improved health literacy after the intervention compared to baseline [32, 48, 50, 51]. In the one of six health literacy studies that used an experimental design, there were no significant differences by group [52]. Among the three mental health interventions, no studies used experimental designs and all had small sample sizes.
Future research in the areas of mental health and health literacy would strongly benefit from the use of appropriately powered experimental designs. It is noteworthy that health behavior studies, which typically used experimental designs and larger sample sizes than mental health studies, were conducted in schools and community-based programs. Researchers and clinicians developing hip hop mental programs should consider partnering with schools to reach a wide range of youth and obtain larger samples for research studies. Although recruiting clinical samples for intensive hip hop therapy interventions may prove difficult in the school setting, it may be possible to implement less intensive interventions that can reach a broader audience.
Moreover, the limited number of mental health studies included in this review does not reflect the full scope of how hip hop is used for mental health. We identified many studies that were not included because they were not in a peer-reviewed journal or did not report the results of an experiment (e.g., [43]). Several books and review articles [22, 23, 36] document that many practitioners have developed and implemented hip hop interventions for mental health. A recent book review documented several case studies of hip hop mental health interventions [37]. Overall, the authors of this book noted that hip hop interventions are a promising approach for mental health.
The lack of peer-reviewed hip hop mental health interventions may reflect the practice-research gap that exists between community practitioners and academic scholars. This gap limits opportunities to develop, evaluate, and disseminate culturally sensitive treatments, such as hip hop-based interventions. Several studies provide specific guidelines to facilitate successful collaborations between community mental health agencies and university researchers [67, 68]. For instance, Abdul-Adil and colleagues [69] provided a detailed university-community partnership model and described results from a mutually beneficial collaboration between the Disruptive Behavior Clinic at the University of Illinois-Chicago and the Community Mental Health Council in Chicago to develop evidence-based practices for youth with disruptive behaviors. Existing research on effective partnerships can be used to guide collaborations between university researchers and community practitioners who develop hip hop-based interventions. These partnerships are especially important for developing a body of scientific research for community-based hip hop interventions that have already demonstrated promise in the community, such as H.Y.P.E. [22].
There are several additional considerations for the health behavior studies (i.e., [34, 35, 47, 53–63]). First, it is difficult to isolate the effect of hip hop because most of these interventions are multicomponent. For instance, Lemieux et al. [35] reported an effect of a hip hop music HIV intervention. However, the intervention group participated in a multicomponent intervention that included having peer leaders develop a rap song and present it to their classmates. Therefore, it is unclear if having peer leaders promote HIV education or having youth listen to rap music about HIV prevention is the mechanism of change. Future studies should directly test whether hip hop contributes to the intervention above and beyond the basic elements. Second, results may differ by the way hip hop is used in an intervention. For instance, a rap video about a health behavior may be more effective than having adolescents develop a rap about health behavior. Future research should examine the difference between active uses of hip hop such as creating music vs. more passive uses such as watching a video. Third, some studies used control groups with no intervention or minimal control groups [35, 47]. In future research, authors should consider matching the intensity of the control intervention with the hip hop intervention. Fourth, the studies used multiple dependent variables and reported inconsistent findings. For example, Williams et al. [53] reported no significant change in purchased calories with labels alone but a 20% decline of calories and less unhealthy foods selected by participants. Future studies should control for multiple tests and specify the primary outcome.
Overall, no conclusions can be drawn about the effect of hip hop health interventions on health literacy, health behavior, or mental health. This review highlights the need for research studies that use experimental designs in the areas of health literacy and mental health. The studies that used experimental designs suggest that hip hop interventions may not improve outcomes compared to control interventions. However, future research is needed because the impact of these interventions may vary across health behavior or may reflect other elements of the interventions. Future studies should also document characteristics of the intervention facilitator such as skill level and ethnicity to determine if these factors influence outcomes. Similarly, future research studies should explore how participant demographics relate to study outcomes. For instance, it is important to determine if some interventions are more appropriate for specific age groups.
Furthermore, several studies in the current review took place in socioeconomically disadvantaged schools around the country (e.g., Illinois, Georgia, Arizona, New York). Future studies should continue to examine the effectiveness of hip hop interventions in similar school settings around the country to reach youth who may have insufficient socioeconomic resources and limited access to healthcare. In addition, many studies (e.g., [51, 65]) lacked detail about which elements of their intervention used hip hop. Studies often provide a list of various intervention components (e.g., dancing, singing, video games), but it was often not clear which of these elements included hip hop. These details will be necessary for future reviews to determine the effectiveness of hip hop interventions.
In summary, this is the first study to our knowledge to synthesize empirical research on hip hop health interventions published in peer-reviewed journals. There is a growing interest in the use of hip hop to promote healthy behaviors, health literacy, and mental health. Future experimental studies can reveal if hip hop health interventions can facilitate engagement and improve the health of African-American and Latino youth who experience an undue burden of disease.
Acknowledgements
The authors thank Judy Grosberg for her assistance with identifying research articles.
Footnotes
Compliance with Ethical Standards
Conflict of Interest The authors have no conflicts of interest to declare.
References
- 1.CDC. Health disparities experienced by black or African Americans—United States. MMWR Morb Mortal Wkly Rep 2005;54(1):1–3. [PubMed] [Google Scholar]
- 2.Elster A, Jarosik J, VanGeest J, Fleming M. Racial and ethnic disparities in health care for adolescents: a systematic review of the literature. Arch Pediatr Adolesc Med 2003;157(9):867–74. [DOI] [PubMed] [Google Scholar]
- 3.DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Progress and opportunities in reducing racial disparities. CA Cancer J Clin 2016;2016 [DOI] [PubMed] [Google Scholar]
- 4.U.S. Census Bureau. Quick facts https://www.census.gov/quickfacts/table/PST045215/00 2016. Accessed 11/30/2016 2016.
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311(8):806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, et al. Mental health surveillance among children— United States, 2005 – 2011. MMWR Surveill Summ 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- 7.Whitmore SK, Kann L, Prejean J, Koenig LJ, Branson BM, Hall HI, et al. Vital signs: HIV infection, testing, and risk behaviors among youths—United States. Am J Transplant 2013;13(2):510–5. [DOI] [PubMed] [Google Scholar]
- 8.Mulia N, Ye Y, Greenfield TK, Zemore SE. Disparities in alcohol related problems among white, black, and Hispanic Americans. Alcohol Clin Exp Res 2009;33(4):654–62. doi: 10.1111/j.1530-0277.2008.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zapolski TC, Pedersen SL, McCarthy DM, Smith GT. Less drinking, yet more problems: understanding African American drinking and related problems. Psychol Bull 2014;140(1):188–223. doi: 10.1037/a0032113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Witbrodt J, Mulia N, Zemore SE, Kerr WC. Racial/ethnic disparities in alcohol-related problems: differences by gender and level of heavy drinking. Alcohol Clin Exp Res 2014;38(6):1662–70. doi: 10.1111/acer.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bridge JA, Asti L, Horowitz LM, Greenhouse JB, Fontanella CA, Sheftall AH, et al. Suicide trends among elementary school-aged children in the united states from 1993 to 2012. JAMA Pediatr 2015;169(7):673–7. [DOI] [PubMed] [Google Scholar]
- 12.Berdahl T, Owens PL, Dougherty D, McCormick MC, Pylypchuk Y, Simpson LA. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children’s health care quality. Acad Pediatr 2010;10(2):95–118. [DOI] [PubMed] [Google Scholar]
- 13.DeNavas-Walt C, Proctor B. Current population reports, income and poverty in the United States: 2014 Washington, DC: 2015. [Google Scholar]
- 14.Alegria M, Carson NJ, Goncalves M, Keefe K. Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. J Am Acad Child Adolesc Psychiatry 2011;50(1):22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gibbons FX, Roberts ME, Gerrard M, Li Z, Beach SR, Simons RL, et al. The impact of stress on the life history strategies of African American adolescents: cognitions, genetic moderation, and the role of discrimination. Dev Psychol 2012;48(3):722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Voisin DR, Patel S, Hong JS, Takahashi L, Gaylord-Harden N. Behavioral health correlates of exposure to community violence among African-American adolescents in Chicago. Child Youth Serv Rev 2016;69:97–105. [Google Scholar]
- 17.Bogart LM, Elliott MN, Kanouse DE, Klein DJ, Davies SL, Cuccaro PM, et al. Association between perceived discrimination and racial/ethnic disparities in problem behaviors among preadolescent youths. Am J Public Health 2013;103(6):1074–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chowdhary N, Jotheeswaran A, Nadkarni A, Hollon S, King M, Jordans M, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol Med 2014;44(06):1131–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nierkens V, Hartman MA, Nicolaou M, Vissenberg C, Beune EJ, Hosper K et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. A systematic review. PLoS One 2013;8(10):e73373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forman M, Neal MA. That’s the joint!: the hip-hop studies reader: Psychology Press; 2004. [Google Scholar]
- 21.Chang J Can’t stop won’t stop: a history of the hip-hop generation Macmillan; 2007. [Google Scholar]
- 22.Winfrey A Healing young people thru empowerment (H.Y.P.E.): a hip hop therapy program for black teenage boys Chicago: African-American Images; 2009. [Google Scholar]
- 23.Abdul-Adil JK. Modern rap music: mining the melodies for mental health resources. Journal of Youth Development 2014;9(2):149–52. [Google Scholar]
- 24.Hip Hop Nation: how the genre is turning it up in 2015 Nielsen; 2015. http://www.nielsen.com/us/en/insights/news/2015/hip-hop-nation-how-the-genre-is-turning-up-in-2015.html. Accessed 12/1/2016. [Google Scholar]
- 25.Tyson EH. Hip hop therapy: an exploratory study of a rap music intervention with at-risk and delinquent youth. J Poet Ther 2002;15(3):131–44. doi: 10.1023/a:1019795911358. [DOI] [Google Scholar]
- 26.Recording Industry Association of America. 2008 Consumer pro file; 2008. http://www.marketingfx.com/downloads/1485144251.61375300_3786a2c159/1999-2008_ConsumerProfile.pdf. Accessed February 9 2017. [Google Scholar]
- 27.Hooton C Hip-hop is the most listened to genre in the world, according to Spotify analysis of 20 billion tracks. The Independent 2015;14 [Google Scholar]
- 28.Printz C FDA launches tobacco use prevention campaign targeting multicultural youth. Cancer 2016;122(6):825-. [DOI] [PubMed] [Google Scholar]
- 29.Williams O, Leighton-Herrmann E, DeSorbo A, Hecht M, Hedmann M, Huq S et al. Hip hop stroke: study protocol for a randomized controlled trial to address stroke literacy. Journal of clinical trials 2015;5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fishbein M A theory of reasoned action: some applications and implications 1979. [PubMed]
- 31.Bandura A Human agency in social cognitive theory. Am Psychol 1989;44(9):1175. [DOI] [PubMed] [Google Scholar]
- 32.Williams O, Noble JM. ‘Hip-hop’ stroke: a stroke educational program for elementary school children living in a high-risk community. Stroke 2008;39(10):2809–16. doi: 10.1161/strokeaha.107.513143. [DOI] [PubMed] [Google Scholar]
- 33.Fitzgibbon ML, Stolley MR, Dyer AR, VanHorn L, KauferChristoffel K. A community-based obesity prevention program for minority children: rationale and study design for Hip-Hop to Health Jr. Prev Med 2002;34(2):289–97. doi: 10.1006/pmed.2001.0977. [DOI] [PubMed] [Google Scholar]
- 34.Romero AJ. A pilot test of the Latin active hip hop intervention to increase physical activity among low-income Mexican-American adolescents. Am J Health Promot 2012;26(4):208–11. doi: 10.4278/ajhp.090123-ARB-24. [DOI] [PubMed] [Google Scholar]
- 35.Lemieux AF, Fisher JD, Pratto F. A music-based HIV prevention intervention for urban adolescents. Health Psychol 2008;27(3): 349–57. doi: 10.1037/0278-6133.27.3.349. [DOI] [PubMed] [Google Scholar]
- 36.Elligan D Rap therapy: a culturally sensitive approach to psychotherapy with young African American men. J Afr Am Stud 2000;5(3):27–36. [Google Scholar]
- 37.Hadley S Yancy G Therapeutic uses of rap and hip-hop: Routledge; 2012. [Google Scholar]
- 38.Tyson EH. Rap music in social work practice with African-American and Latino youth. J Hum Behav Soc Environ 2004;8(4):1–21. doi: 10.1300/J137v08n04_01. [DOI] [Google Scholar]
- 39.Stephens T, Braithwaite RL, Taylor SE. Model for using hip-hop music for small group HIV/AIDS prevention counseling with African American adolescents and young adults. Patient Educ Couns 1998;35(2):127–37. doi: 10.1016/S0738-3991(98)00050-0. [DOI] [PubMed] [Google Scholar]
- 40.Kobin C, Tyson E. Thematic analysis of hip-hop music: can hip hop in therapy facilitate empathic connections when working with clients in urban settings? Arts Psychother 2006;33(4):343–56. [Google Scholar]
- 41.Travis R Jr, Deepak A. Empowerment in context: lessons from hip-hop culture for social work practice. J Ethnic Cult Diversity Soc Work 2011;20(3):203–22. [Google Scholar]
- 42.DeCarlo A The rise and call of group rap therapy: a critical analysis from its creator. Group Analysis 2013;46(2):225–38. [Google Scholar]
- 43.DeCarlo A, Hockman E. RAP therapy: a group work intervention method for urban adolescents. Soc Work Groups 2004;26(3):45–59. doi: 10.1300/J009v26n03_06. [DOI] [Google Scholar]
- 44.Gold C, Solli HP, Krüger V, Lie SA. Dose–response relationship in music therapy for people with serious mental disorders: systematic review and meta-analysis. Clin Psychol Rev 2009;29(3):193–207. [DOI] [PubMed] [Google Scholar]
- 45.Armstrong R, Hall BJ, Doyle J, Waters E. ‘Scoping the scope’ of a Cochrane review. J Public Health 2011;33(1):147–50. [DOI] [PubMed] [Google Scholar]
- 46.Hill MJ, Hallmark CJ, McNeese M, Blue N, Ross MW. Hip hop for HIV awareness: using hip hop culture to promote community-level HIV prevention. Sex Education 2014;14(2):128–43. doi: 10.1080/14681811.2013.852079. [DOI] [Google Scholar]
- 47.Turner-Musa JO, Rhodes WA, Harper PT, Quinton SL. Hip-hop to prevent substance use and HIV among African-American youth: a preliminary investigation. J Drug Educ 2008;38(4):351–65. [DOI] [PubMed] [Google Scholar]
- 48.Noble JM, Hedmann MG, Williams O. Improving dementia health literacy using the FLOW mnemonic: pilot findings from the Old SCHOOL hip-hop program. Health Educ Behav 2015;42(1):73–83. doi: 10.1177/1090198114537063. [DOI] [PubMed] [Google Scholar]
- 49.Williams O, Hecht MF, DeSorbo AL, Huq S, Noble JM. Effect of a novel video game on stroke knowledge of 9- to 10-year-old, low-income children. Stroke 2014;45(3):889–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams O, DeSorbo A, Noble J, Gerin W. Child-mediated stroke communication: findings from hip hop stroke. Stroke 2012;43(1): 163–9. doi: 10.1161/strokeaha.111.621029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Williams O, DeSorbo A, Noble J, Shaffer M, Gerin W. Long-term learning of stroke knowledge among children in a high-risk community. Neurology 2012;79(8):802–6. doi: 10.1212/WNL.0b013e3182661f08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ware KB, Thomas MC, Stajich GV, Macias-Moriarity LZ. Learning new tricks: an assessment of novel versus traditional patient counseling strategies. Curr Pharm Teach Learn 2015;7(5):584–9. [Google Scholar]
- 53.Williams O, DeSorbo A, Sawyer V, Apakama D, Shaffer M, Gerin W, et al. Hip Hop HEALS: pilot study of a culturally targeted calorie label intervention to improve food purchases of children. Health Educ Behav 2016;43(1):68–75. doi: 10.1177/1090198115596733. [DOI] [PubMed] [Google Scholar]
- 54.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr 2005;146(5): 618–25. doi: 10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 55.Fitzgibbon ML, Stolley MR, Schiffer L, Kong A, Braunschweig CL, Gomez-Perez SL, et al. Family-based hip-hop to health: outcome results. Obesity 2013;21(2):274–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fitzgibbon ML, Stolley MR, Schiffer LA, Braunschweig CL, Gomez SL, Horn L, et al. Hip-Hop to Health Jr. obesity prevention effectiveness trial: postintervention results. Obesity 2011;19(5):994–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fitzgibbon ML, Stolley MR, Schiffer L, Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity 2006;14(9):1616–25. [DOI] [PubMed] [Google Scholar]
- 58.Sussman S, Parker VC, Lopes C, Crippens DL, Elder P, Scholl D. Empirical development of brief smoking prevention videotapes which target African-American adolescents. Int J Addict 1995;30(9):1141–64. [DOI] [PubMed] [Google Scholar]
- 59.Connelly J, Berryman T, Tolley E. Rap video vs. traditional video for teaching nutrition. J Biocommun 1995;23(4):17–21. [PubMed] [Google Scholar]
- 60.Kong A, Buscemi J, Stolley MR, Schiffer LA, Kim Y, Braunschweig CL, et al. Hip-Hop to Health Jr. randomized effectiveness trial: 1-year follow-up results. Am J Prev Med 2016;50(2):136–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Robinson TN, Matheson DM, Kraemer HC, Wilson DM, Obarzanek E, Thompson NS, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med 2010;164(11):995–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quirk ME, Godkin MA, Schwenzfeier E. Evaluation of two AIDS prevention interventions for inner-city adolescent and young adult women. Am J Prev Med 1993; [PubMed]
- 63.Cella DF, Tulsky DS, Sarafian B, Thomas CR. Culturally relevant smoking prevention for minority youth. J Sch Health 1992;62(8): 377–80. [DOI] [PubMed] [Google Scholar]
- 64.Olson-McBride L, Page TF. Song to self: promoting a therapeutic dialogue with high-risk youths through poetry and popular music. Social Work with Groups 2012;35(2):124–37. doi: 10.1080/01609513.2011.603117. [DOI] [Google Scholar]
- 65.Staum MJ. A music/nonmusic intervention with homeless children. J Music Ther 1993;30(4):236–62. doi: 10.1093/jmt/30.4.236. [DOI] [Google Scholar]
- 66.Hudson W, Nurius P, Daley J, Newsome R. Index of peer relations (IPR) Tallahassee, FL: Walmyr Publishing Company; 1993. [Google Scholar]
- 67.Akintobi TH, Trotter JC, Evans D, Johnson T, Laster N, Jacobs D, et al. Applications in bridging the gap: a community-campus partnership to address sexual health disparities among African-American youth in the south. J Community Health 2011;36(3): 486–94. doi: 10.1007/s10900-010-9332-8. [DOI] [PubMed] [Google Scholar]
- 68.Frounfelker RL, Ben-Zeev D, Kaiser SM, O’Neill S, Reedy W, Drake RE. Partnering with mental health providers: a guide for services researchers. J Ment Health 2012;21(5):469–77. doi: 10.3109/09638237.2012.705923. [DOI] [PubMed] [Google Scholar]
- 69.Abdul-Adil J, Drozd O, Irie I, Riley R, Silas A, Farmer AD Jr, et al. University-community mental health center collaboration: encouraging the dissemination of empirically-based treatment and practice. Community Ment Health J 2010;46(5):417–22. doi: 10.1007/s10597-009-9250-3. [DOI] [PubMed] [Google Scholar]


