Abstract
Introduction:
Hypertension is an important noncommunicable disease of global significance. Low-sodium salt substitutes (LSSS) are increasingly being used for hypertensive persons. The sodium content of these salts is reduced by substituting varying proportion of sodium with potassium.
Materials and Methods:
The present study was done to assess the awareness of ideal salt intake, knowledge of the availability of LSSS, their indications, and contraindications among 165 doctors of Mangalore, Dakshina Kannada.
Results:
The knowledge of correct upper limit of salt as 5 g/day was present in 46.7% of the participants and that for the availability of LSSS in 71%. Knowledge about the mechanism of sodium reduction with potassium substitution was found to be correct in 17.6% participants. LSSS were prescribed by 31 (18.8%), and 118 (71.5%) participants did not know about their contraindications in patients with renal disease, cardiac problems, and diabetes and patients on K-sparing diuretics and painkillers.
Conclusions:
The study underlines the importance of knowledge about salt reduction, LSSS, their indications, and contraindications in doctors. Regulated availability of these salts and widespread information for the primary care physicians to prevent mishaps following their use is recommended.
Keywords: Hypertension, low-sodium salt, potassium, sodium-restricted diet
INTRODUCTION
Noncommunicable diseases (NCDs) were responsible for 68% of the global deaths in 2012, and more than 80% of these were in low- and middle-income countries.[1] Globally, all the countries are at different points in their progress towards the presentation and control of NCDs due to variable socioeconomic conditions and the phase in epidemiological transition. Hence, voluntary global targets have been prepared so that all countries can benefit from a comprehensive response. Of the nine global targets, the WHO recommends a relative reduction of 30% salt/sodium intake in the population with optimum salt intake recommended as 5 g/day.[1] Salt reduction has a definitive role in the control of blood pressure of patients on treatment for hypertension.[2]
According to a systematic review and meta-analysis, the prevalence of hypertension was 33% in urban and 25% in rural Indians.[3] Exact mean population intake of salt is difficult to estimate, but the overall mean intake according to a systematic review varied from 5.2 to 42.3 g/day (mean of 10.98, 95% confidence interval 8.57–13.40).[4] Modest reduction in the salt intake for 4 weeks or more can have a significant effect on hypertensive and normotensive individuals which can reduce stroke deaths by 14%, coronary deaths by 9% in hypertensives, and 6% and 4% in normotensive individuals, respectively.[5]
Potassium in diet not only leads to reduction in blood pressure but also has beneficial effects such as reduction in stroke, renal (vascular, glomerular and tubular) damage and calcium excretion.[6] Fruits and vegetables are the best natural sources of the potassium. Apart from these, there are some salts that have higher potassium and lower sodium called as low-sodium salt substitutes (LSSS). These have been demonstrated to reduce blood pressure by studies in China and Tibet as well as by a recent meta-analysis.[7,8,9]
While higher potassium intake is beneficial, it is important to remember certain conditions where higher potassium intake can lead to hyperkalemia or renal damage. These include, renal failure, diabetes mellitus, obstructive uropathy, or chronic intake of non-steroidal anti-inflammatory drugs and angiotensin converting enzyme inhibitors.[10,11]
With global salt reduction guidelines in place and many salt substitutes available in the Indian market, in the shops as well as in the e-commerce marketplaces, the present study explores the awareness among the health-care professionals regarding the quantum of salt reduction, various strategies available for doing so, and the situations where the use of LSSS can be harmful. The objectives were to assess the knowledge and awareness regarding ideal salt intake and some key facts about LSSS.
MATERIALS AND METHODS
Study setting
The present study was conducted among the doctors of Mangalore in Dakshina Kannada. There are seven medical colleges, one district hospital and Employee State Insurance Hospital each and about eight large private hospitals.
Study design and sample
It was a cross-sectional study conducted between July and September 2017. Assuming the prevalence of right knowledge about salt and salt substitutes to be 50% (no appropriate baseline reference study available), using the formula 4pq/L2, an absolute allowable error as 10%, about 10% nonenrollment rate, and 1.5 design effect (owing to two-stage random sampling), the sample size was 165 doctors. Three medical colleges, one government hospital, and four private hospitals were thus selected. The required number of doctors was enrolled by simple random sampling from each of these. Out of total 625 doctors, 165 doctors were thus enrolled in the study.
Inclusion and exclusion criteria
Operationally, only health-care providers or doctors involved in active patient care were enrolled in the study. Preclinical and para-clinical doctors, except community medicine, were excluded from the study. This was done assuming that the participants from clinical and community medicine were engaged in screening, diagnosis, or direct patient care which requires counseling for salt reduction and possible use of LSSS.
Data collection
Interview was conducted with eligible participants using predesigned semi-structured questionnaire at a mutually convenient time. Anonymity of the study participants was maintained to enhance the participation rate and to ensure confidentiality. Details about age, gender, specialty, and health-care setting were collected. Interview schedule included questions to assess the knowledge about salt restriction in hypertension, LSSS, and their indications and contraindications.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) for Windows, version 16.0., SPSS Inc., Chicago, IL, USA. Results are expressed as frequencies and proportions for categorical variables and mean and standard deviation for continuous variables. Chi-square test was applied to assess the differences in knowledge across various study variables. Two-sided P < 0.05 was considered as statistically significant.
Ethics approval
Approval of the Institutional Review Board and Ethics Committee of Yenepoya University was obtained before the commencement of the study. Informed written consent was taken from all the study participants for voluntary participation. All information collected was kept private and confidential.
RESULTS
A total of 165 doctors participated in the study. About 60% of the participating doctors were males. The mean age of the participants was 34.6 years (SD: 10.7 years). There were 76 (46%) from internal medicine, 40 (24%) from obstetrics and gynecology, 28 (17%) from community medicine, 7 (4%) nephrologists, and rest from pediatrics and emergency medicine. There were 126 doctors (76.4%) from medical colleges, 20 (12.1%) from government district hospital, and rest from private hospitals.
Details regarding awareness about salt and LSSS are described in Table 1. Less than half of the participants were aware about correct upper limit for daily salt intake as being 4–6 g/day (77; 46.7%). Indian foods were rated as either moderately high in salt content (88; 53.3%) or very high (75; 45.5%). Hundred and seventeen (70.9%) participants were aware about the availability of various brands of LSSS, but 102 (87.2%) could not name any of the LSSS available in the Indian market. For access to LSSS, 141 (85.5%) said that it is available in retail shops, 106 (64.2%) reported its availability in medical shops, and 121 (73.3%) participants said that it can be purchased from online markets. While 72 (43.6%) did not know exact indication for the use of LSSS, 87 (52.8%) reported that it is used in hypertension. Only 29 (17.6%) participants knew that potassium is used for reduction in sodium content in these salts and only 31 (18.8%) had prescribed them during their clinical practice.
Table 1.
Awareness about salt and low sodium salt substitutes
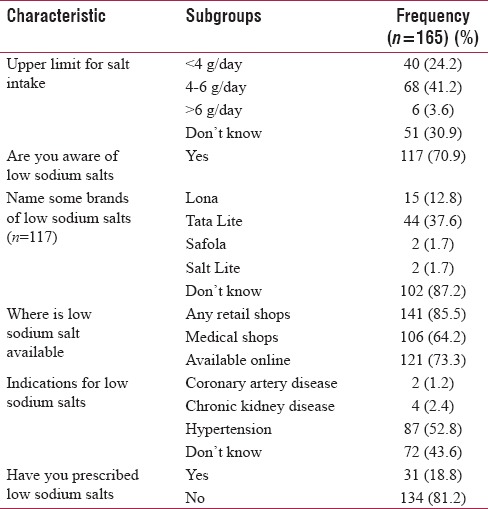
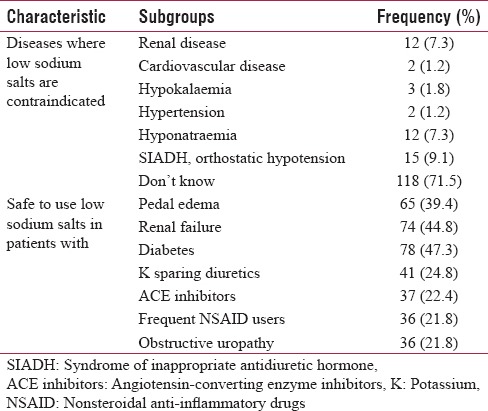
Table 2 describes the awareness about the safety of the use of LSSS. Hundred and eighteen (71.5%) participants did not know about contraindications. Others said that it is contraindicated in renal disease (12; 7.3%), cardiovascular diseases (2; 1.2%), hypokalemia (3; 1.8%), and hyponatremia (12; 7.3%). Specialty was significantly associated with knowledge of the WHO recommendation of salt intake and how sodium was reduced in LSSS (P < 0.05). There was no association between specialty and prescription practice of LSSS (P = 0.16).
Table 2.
Awareness about safety of low sodium salt substitutes (n=165)
DISCUSSION
LSSS are very easily available in the Indian market. While there are many methods to reduce the sodium content of the salt, one of the most commonly used mechanisms is replacing part of sodium with potassium which is beneficial for most patients with hypertension.[6] The benefits of potassium in hypertensive persons are well known. These include, reduction in the risk of stroke, prevention of renal damage (demonstrated in rats), reduction in ventricular arrhythmias in patients with heart disease, cardiac failure and left ventricular hypertrophy.[6,7,8,12] Studies have shown its effectiveness in reducing blood pressure in general population as early as in a randomized controlled trial in 1994.[13] The intervention arm received salt with sodium, potassium, and magnesium in the ratio of 8:6:1 and resulted in mean reduction in systolic blood pressure by 7.6 mmHg and diastolic by 3.3 mmHg.
The present study was an exploratory study to understand the awareness among doctors from various specialties who are likely to use these salt substitutes in their patients. Since it was not being prescribed by more than 80% of the participants, not many knew about the various brands available in the market. However, a striking finding was that only few knew the exact mechanism by which sodium content of the salt is reduced. This lack of knowledge regarding the exact mechanism is reflected in poor awareness about the conditions in which these salt substitutes are to be avoided. These conditions were not known to 70% of the participants. The participants were asked about individual diseases and conditions when salt substitutes with increased potassium are likely to harm, and the awareness was found to be poor. This could be because <20% were actually prescribing these.
Renal complications are common in patients suffering from chronic hypertension where high potassium can be harmful. Easy availability of supplements and food items with high potassium in general market without necessary information and education of stakeholders is likely to be detrimental to the health of these patients.[11] Due to known problems in patients with chronic kidney disease and heart disease, these patients are excluded even from the trials of LSSS. This is being done in spite of the close monitoring that is done when compared to field setting. This itself raises serious questions about the availability of LSSS in general market.[14] They should be avoided in patients with chronic kidney disease and cardiac problems and patients on angiotensin II receptor blockers, potassium-sparing diuretics, and nonsteroidal anti-inflammatory drugs.[10] Moreover, the study finds suboptimal awareness about harmful effects of potassium in specific diseases in medical community. The knowledge of potential serious adverse effects in consumers is likely to be poorer due to inadequate consumer warnings.[15] Clear guidelines regarding when to use LSSS and when they are contraindicated need to be framed and put up clearly on the packages for the sake of consumers and providers. Published literature so far has not explored this in terms of knowledge or utilization surveys in India and other countries. Only case reports of patients with specific comorbidities suffering from ill-effects of LSSS have been generally reported.[10,11]
Limitations of the study
The study was done in health-care providers of a single city, and hence, the generalization of findings for the larger medical graternity should be done with caution.
CONCLUSIONS
LSSS are available in the Indian market and are being increasingly considered for use by doctors and patients. But at the same time, the baseline awareness in the doctors for the cutoff to be used for diagnosing hypertension, the upper limit of salt intake, and advantages and disadvantages of LSSS needs careful attention. A possibility of including relevant information and warning on the packages and product information of such salts is desirable to prevent problems due to higher potassium content.
Financial support and sponsorship
This study was financially supported by the Indian Council of Medical Research short-term studentship award of 10,000 rupees.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors acknowledge the co-operation of the doctor participants and the Indian Council of Medical Research for supporting this under the short-term studentship.
REFERENCES
- 1.World Health Organization. Global Status Report in Non-Communicable Diseases 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 2.Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Systematic review of long term effects of advice to reduce dietary salt in adults. BMJ. 2002;325:628. doi: 10.1136/bmj.325.7365.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson C, Praveen D, Pope A, Raj TS, Pillai RN, Land MA, et al. Mean population salt consumption in India: A systematic review. J Hypertens. 2017;35:3–9. doi: 10.1097/HJH.0000000000001141. [DOI] [PubMed] [Google Scholar]
- 5.He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: A meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002;16:761–70. doi: 10.1038/sj.jhh.1001459. [DOI] [PubMed] [Google Scholar]
- 6.He FJ, MacGregor GA. Fortnightly review: Beneficial effects of potassium. BMJ. 2001;323:497–501. doi: 10.1136/bmj.323.7311.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.China Salt Substitute Study Collaborative Group. Salt substitution: A low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007;25:2011–8. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 8.Zhao X, Yin X, Li X, Yan LL, Lam CT, Li S, et al. Using a low-sodium, high-potassium salt substitute to reduce blood pressure among Tibetans with high blood pressure: A patient-blinded randomized controlled trial. PLoS One. 2014;9:e110131. doi: 10.1371/journal.pone.0110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng YG, Li W, Wen XX, Li Y, Hu JH, Zhao LC, et al. Effects of salt substitutes on blood pressure: A meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100:1448–54. doi: 10.3945/ajcn.114.089235. [DOI] [PubMed] [Google Scholar]
- 10.Doorenbos CJ, Vermeij CG. Danger of salt substitutes that contain potassium in patients with renal failure. BMJ. 2003;326:35–6. doi: 10.1136/bmj.326.7379.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perazella MA. Drug-induced hyperkalemia: Old culprits and new offenders. Am J Med. 2000;109:307–14. doi: 10.1016/s0002-9343(00)00496-4. [DOI] [PubMed] [Google Scholar]
- 12.Aaron KJ, Sanders PW. Role of dietary salt and potassium intake in cardiovascular health and disease: A review of the evidence. Mayo Clin Proc. 2013;88:987–95. doi: 10.1016/j.mayocp.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geleijnse JM, Witteman JC, Bak AA, den Breeijen JH, Grobbee DE. Reduction in blood pressure with a low sodium, high potassium, high magnesium salt in older subjects with mild to moderate hypertension. BMJ. 1994;309:436–40. doi: 10.1136/bmj.309.6952.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernabe-Ortiz A, Diez-Canseco F, Gilman RH, Cárdenas MK, Sacksteder KA, Miranda JJ, et al. Launching a salt substitute to reduce blood pressure at the population level: A cluster randomized stepped wedge trial in Peru. Trials. 2014;15:93. doi: 10.1186/1745-6215-15-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John SK, Rangan Y, Block CA, Koff MD. Life-threatening hyperkalemia from nutritional supplements: Uncommon or undiagnosed? Am J Emerg Med. 2011;29:1237.e1–2. doi: 10.1016/j.ajem.2010.08.029. [DOI] [PubMed] [Google Scholar]


