Abstract
Purpose
Aim of the study is to assess the contribution of peri-articular soft tissues to hip joint kinematics and their influence on hip stability.
Methods
Four hemi-corpse specimens (3 males, average age 72 years) were studied using a custom navigation system. Hip kinematics (femoral head motion relative to the acetabulum and joint range of motion) were evaluated with the hip manually positioned in 36 different positions with (I) soft tissues intact, (II) after removal of the skin and muscles and (III) after partial capsulectomy. Each position was repeated 3 times in each state.
Results
Excellent interclass correlation for each test was determined (ICC range, 0.84–0.96). Femoral head anatomical centre displacement relative to the acetabulum occurred in all 3 planes, even with all the soft tissue intact (average, 3.3 ± 2.8 mm lateral translation; 1.4 ± 1.8 mm posterior translation and 0.3 ± 1.5 mm distally). These translations increased as more soft tissue was removed, except medial–lateral displacement, with an average 4.6 ± 2.9 mm lateral translation, 0.7 ± 1.3 mm posterior translation and 1.5 ± 1.9 mm distal translation when partial capsulectomy was performed. Range of motion increased in all 3 planes with increasing removal of the soft tissues.
Conclusions
This study showed that femoral head anatomical centre displacement within the acetabulum occurs and increases with increasing removal of peri-articular soft tissues, confirming their influence on hip stability. Hip kinematics was also influenced by peri-articular soft tissues; specifically range of motion increases with increasing removal of those tissues. From clinicians’ point of view, they have therefore to consider the influence of their surgeries on peri-articular soft tissues, since excessive translations may promote hip arthritis.
Keywords: Hip kinematics, Hip stability, Peri-articular soft tissues, Hip biomechanics, Hip navigation
Introduction
There is an increasing interest in the non-arthritic hip joint as improvement in the diagnosis of hip pathologies has been made easier with the advancement of imaging techniques, including magnetic resonance imaging (MRI) [33], and as a result of the improvements in hip arthroscopy [2, 19] with better and more hip-specific instrumentation both allowing treatment of a wider array of hip problems [2, 17].
However, despite research on hip chondral [6] and soft tissue structures (i.e. labrum [3, 18] and joint capsule [15, 16, 27, 28]), our basic understanding of hip joint kinematics and its influence on hip pathologies and, alternatively, the influence of hip defects on joint movements, is lacking. In fact, of all the major joints in the body, the hip has been least studied with regard to its kinematics and kinetics, particularly in the non-diseased or non-prosthetic arthroplasty hip joint [7]. This lack of biomechanical and clinical research needs to be addressed to improve our understanding of the pathomechanics of hip injuries, including labral lesions, the role of femoro-acetabular impingement and the effects on hip function, as well as the treatment of these hip problems.
The hypothesis of this work is that hip joint does not act as a pure ball-and-socket joint and that the peri-articular soft tissues perform an important contribution to passive hip stability, constraining the movement of the femoral head inside the acetabulum during movements. The main objectives of this study are therefore to (1) assess hip kinematics with all the soft tissues intact, (2) assess the relative contributions of the soft tissues to hip stability (as determined by femoral head anatomical centre displacement) and (3) assess the relative contributions of periarticular soft tissues to hip range of motion (ROM) after serial sectioning of the soft tissue structures about the hip. This initial work is to study the kinematics of the passive hip joint, without load bearing or joint reaction forces due to muscular contraction. This will allow a better understanding of the true contribution of the non-contractile periarticular soft tissues to hip joint stability and femoral head motion within the acetabulum.
Materials and methods
Eight hips from four fresh-frozen normal cadaveric hemicorpse specimens (3 males and 1 female, aged 72 ± 21 years) were included in this study. Before testing, a board-certified musculoskeletal radiologist examined all hips by means of magnetic resonance imaging (GE 1.5T Signa MRI System) to exclude any specimens with arthritis, significant soft tissue pathology or previous surgery. All specimens were thawed 24 h prior to testing. After thawing, each specimen was fixed to a wooden support with threaded Steinmann pins. This wooden support was then fixed to the end of a sturdy table using heavy duty “C” clamps to stabilize the pelvis while allowing unrestricted complete motion of the hip and femur. The lower limbs were sectioned at the level of the knee joint, thus having complete specimens from the upper iliac crest (entire pelvis) to the distal part of the femur (femoral condyles). A threaded Steinmann pin was drilled into the femoral condyles, through transepicondylar line, to control femoral rotation during kinematic acquisition.
A commercially available optical-based system for intraoperative kinematic assessment (BluIGS/KLEE, Orthokey Ltd, Delaware, DE, USA) was used to acquire the kinematic and anatomic data. Repeatability of the system for kinematic test was reported by Martelli et al. [21] and Zaffagnini et al. [32] and was about 1 mm and 1 in kinematic test repetition. The optical localizer ensured indeed a 3D accuracy of 0.35 mm in the identification of singular passive optical marker. In order to track the relative motion between the femur and the pelvis, a tracker equipped with these passive optical markers was mounted on iliac crest (on the same side of the evaluated hip), and a corresponding tracker was fixed on the femoral diaphysis, about 100 mm distal to the lesser trochanter towards the anterolateral femur.
The anatomical references, necessary to correctly evaluate the anatomical motions, were identified through the palpation of anatomical bony landmarks (right and left anterior superior iliac spines, right and left pubic tubercles, and medial and lateral femoral epicondyles) using a probe equipped with passive optical markers. The functional hip joint centre (HJC) was identified through a pivoting motion [26] and used to define the anatomical femoral reference only during real-time acquisitions; for the complete performed analysis, we used the described anatomical femoral head and acetabulum centres.
Kinematic movements (articular ranges of motion) were decomposed using these defined anatomical references, allowing the continuous assessment of hip ROM with 6 degrees of freedom [23, 31].
A fellowship-trained orthopaedic surgeon experienced with this navigation system performed the landmark identification and then a set of passive kinematic manoeuvres—for a total of 36 positions—to assess ROM while applying a manual load (Table 1). Each set of kinematic tests was performed with the limb in three different conditions:
State I: Intact limb: only the trackers were fixed to the bones;
State II: no-skin and no-muscle: skin and muscular layers were removed; the labrum and capsuloligamentous complex remain intact;
State III: partial circumferential capsulectomy with the acetabular labrum left intact.
Table 1.
Sets of movements acquired during experimental sessions
| Flexion/extension | Abduction/adduction | Internal/external rotation |
|---|---|---|
| Full flexion | Neutral | Max internal |
| Neutral | ||
| Max external | ||
| Full abduction | Max internal | |
| Neutral | ||
| Max external | ||
| Full adduction | Max internal | |
| Neutral | ||
| Max external | ||
| 90° of Flexion | Neutral | Max internal |
| Neutral | ||
| Max external | ||
| Full abduction | Max internal | |
| Neutral | ||
| Max external | ||
| Full adduction | Max internal | |
| Neutral | ||
| Max external | ||
| 0° of Flexion | Neutral | Max internal |
| Neutral | ||
| Max external | ||
| Full abduction | Max internal | |
| Neutral | ||
| Max external | ||
| Full adduction | Max internal | |
| Neutral | ||
| Max external | ||
| Full Extension | Neutral | Max internal |
| Neutral | ||
| Max external | ||
| Full abduction | Max internal | |
| Neutral | ||
| Max external | ||
| Full adduction | Max internal | |
| Neutral | ||
| Max external |
While passively moving the hip, the surgeon kept attention to avoid forceful displacement of the femoral head relative to the acetabulum, controlling on the navigation system the limb rotation and degree of flexion, in order to achieve the defined positions. Further, care was taken to consider the limit of motion and head translation; at the instant, there was any indication of hip subluxation, in the situation of partial circumferential capsulectomy.
Each test was repeated 3 times to allow for confirmation of the intra-observer reliability of this methodology; item standard deviation (STD) and intra-class correlation coefficient (ICC) were used to estimate the reliability of the angular values and displacement, obtained during test repetitions [1].
Following data acquisition in the 3 different soft tissue conditions, the specimens were dissected and disarticulated, allowing the acquisition of the anatomical surfaces of hip joint acetabulum and femoral head using the navigation probe, to define the corresponding anatomical centres. Specifically, a sphere was fitted on the point cloud acquired on the femoral head by means of a sphere fitting method—using a standard least-square approach and solving the overdetermined matrix system with the SVD numerical technique—thus identifying the centre of the sphere and the corresponding spherical radius [13]. Similarly, the corresponding acetabular centre and corresponding radius were estimated. The root mean square error (RMSE) associated with the sphere deviation was used to assess the reliability of the performed fittings. The previously defined femoral and pelvic anatomical reference systems were successively centred in the femoral head anatomical centre and acetabulum anatomical centre, respectively, thus to evaluate the corresponding relative anatomical displacements for each performed movements and conditions.
The relative displacements at standing position (i.e. maintaining the limb at 0° of flexion no ABD/ADD stress and normally IR/ER) for each condition were analysed in order to verify any changes also in the static starting point.
Statistical analysis
Wilcoxon’s signed ranks test was performed to statistically compare ranges of motion and translations of the femoral head anatomical centre, between each limb condition. Statistical significance was set at p = 0.05. All the data were analysed using unique MATLAB (Mathworks, Inc, Natick, MA, USA) functions designed and implemented specifically for this study.
Results
The analysis of repeatability was performed defining the item standard deviation (STD) and intra-class correlation coefficient (ICC) for each angular value and displacement obtained during the elaboration of the repeated tests. The results demonstrate an excellent correlation for each test (ICC range, 0.84–0.96), giving reliability to the performed data analysis and obtained results (Table 2).
Table 2.
ICC and item STD (standard deviation) detailed for each performed test: flexion/extension (FLEX/EXT), abduction/adduction (ABD/ADD) and internal/external rotation (IR/ER) angles (in degrees) and medial/lateral (MED/LAT), anterior/posterior (ANT/POST) and proximal/distal (PROX/DIST) displacements (in mm)
| EXT |
FLEX |
ADD |
ABD |
ER |
IR |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICC | STD | ICC | STD | ICC | STD | ICC | STD | ICC | STD | ICC | STD |
| 0.91 | 2.4 | 0.84 | 1.7 | 0.88 | 1.9 | 0.87 | 2.1 | 0.93 | 3.0 | 0.95 | 2.4 |
| MED |
LAT |
ANT |
POST |
PROX |
DIST |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICC | STD | ICC | STD | ICC | STD | ICC | STD | ICC | STD | ICC | STD |
| 0.94 | 0.6 | 0.96 | 0.6 | 0.93 | 0.4 | 0.94 | 0.3 | 0.96 | 0.4 | 0.94 | 0.5 |
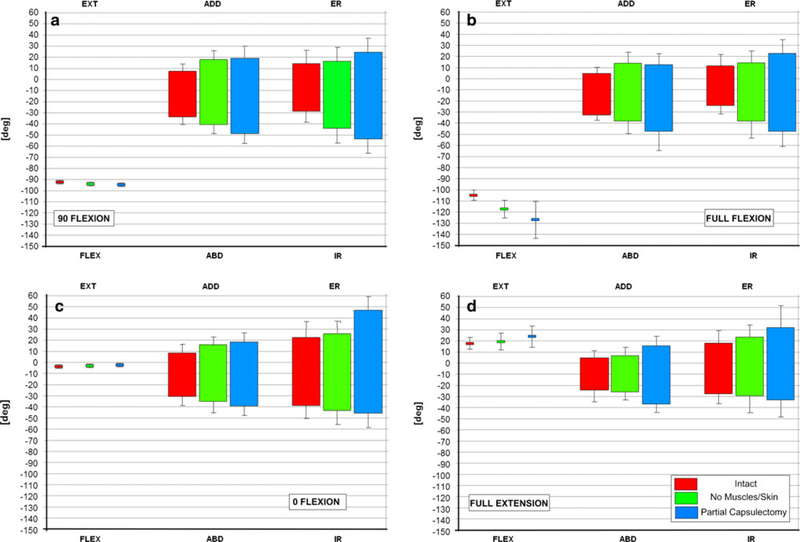
The specific kinematic analysis of the changes in passive ROM is summarized (Fig. 1). Specifically, concerning FLEX/EXT, ABD/ADD and IR/ER ranges, there were statistically significantly differences in all soft tissue conditions from each other (p< 0.05).
Fig. 1.
Ranges of motion for flexion/extension, (FLEX/EXT) abduction/adduction (ABD/ADD) and internal/external (IR/ER) rotation for each performed test and hip position with each graph representing the testing in different hip flexion–extension positions, and each different colour bar representing the different soft tissue states (I intact, II after removal of skin and muscles, while leaving the capsuloligamentous structures intact, and III after partial circumferential capsulectomy). Figure 1 represents the ROM in each plane with the hip in a 90 degrees of flexion, b in full flexion, c in neutral flexion–extension and d in hyperextension of the hip
The mean acetabulum radius was assessed to be 25.7 ± 2.1 mm with a RMSE of 1.9 ± 0.3 mm, whereas the mean femoral head radius 25.7 ± 1.6 mm but with a lower RMSE of 1.0 ± 0.3 mm. The mean difference in the radius estimation between left and right side of each specimen was less than 0.3 ± 1.1 mm for the femoral head and 0.3 ± 0.2 mm for the acetabulum. The RMSE was comparable with the error introduced during the acquisitions and related to the optical system. The acetabulum and femoral head radii resulted comparable.
Translation of the femoral head occurs with passive motion, even in the normal hip with intact surrounding soft tissues. The starting positions (i.e. the position of the femoral head anatomical centre with respect to acetabulum anatomical centre in the anatomical pelvic reference) for each condition are reported in Table 3.
Table 3.
Anterior/posterior (ANT/POST), medial/lateral (MED/LAT) and proximal/distal (PROX/DIST) displacements at standing position with the corresponding p statistical values of the comparisons
| Intact (I) | No muscles/skin (II) | Partial capsulectomy (III) | pI–II | pI–III | pII–III | |
|---|---|---|---|---|---|---|
| MED(+)/LAT(-) | −3.3 ± 2.8 | −3.4 ± 2.4 | −4.6 ± 2.9 | n.s. | n.s. | n.s. |
| ANT(+)/POST(-) | −1.4 ± 1.8 | −1.1 ± 0.8 | −0.7 ± 1.3 | n.s. | n.s. | n.s. |
| PROX(+)/DIST(-) | −0.3 ± 1.5 | −0.3 ± 1.8 | −1.5 ± 1.9 | n.s. | 0.016 | 0.023 |
n.s. no significance
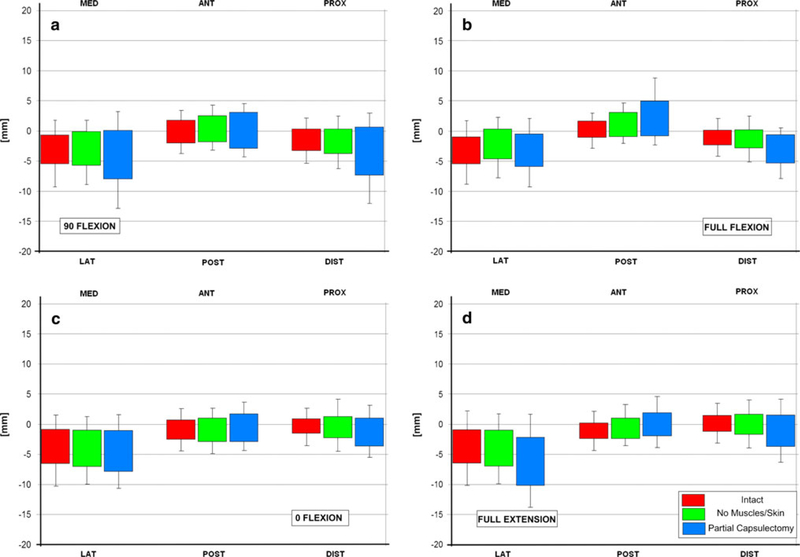
We averaged the maximal translations through all of the repeated acquisitions and evaluating the displacements of anatomical femoral head centre relatively to acetabulum anatomical centre in anatomical pelvic reference. The motion of the femoral head within the acetabulum revealed to occur with lateral translation, distal translation and anterior translation predominating (Fig. 2). Specifically, the differences in MED/LAT range were statistically significant for the comparison between ‘intact’ condition and partial capsulectomy (p< 0.05) and between state II and state III (p<0.05) conditions, whereas there was no statistically significant difference between states I and II (n.s.). All the ranges in ANT/POST and PROX/DIST direction were statistically different by each condition (p< 0.05).
Fig. 2.
Displacements of the femoral head relative to the acetabulum in medial/lateral (MED/LAT), anterior/posterior (ANT/POST) and proximal/distal (PROX/DIST) during each test and hip position with each histogram representing the testing in different hip flexion– extension positions, and each different colour bar representing the different soft tissue states (I intact, II after removal of skin and muscles, while leaving the capsuloligamentous structures intact, and III after partial circumferential capsulectomy). a Femoral head motion in the 3 planes while the hip was in 90 degrees of flexion and the hip rotated and abducted–adducted. b is for the same measurements while the hip was in full flexion, c in neutral flexion– extension and d with the hip in hyperextension
The maximal ANT/POST, MED/LAT and PROX/DIST displacements and the maximal FLEX/EXT, ABD/ADD and IR/ER angles are listed in Table 4.
Table 4.
Maximal medial/lateral (MED/LAT), anterior/posterior (ANT/POST) and proximal/distal (PROX/DIST) displacements and the extreme angular ranges of motion (i.e.FLEX/EXT, ADD/ABD, INT/EXT rotation), with the corresponding statistical p values of the comparisons
| Intact (I) | No muscles/skin (II) | Partial capsulectomy (III) | pI–II | pI–III | pII–III | |
|---|---|---|---|---|---|---|
| MED(+) | 0.1 ± 2.8 | 0.8 ± 1.8 | 0.3 ± 2.9 | n.s. | n.s. | n.s. |
| LAT(-) | −6.2 ± 3.8 | −6.6 ± 3.1 | −12.7 ± 2.1 | n.s. | 0.023 | 0.016 |
| ANT(+) | 2.1 ± 1.8 | 3.3 ± 1.6 | 6.0 ± 3.1 | n.s. | 0.008 | 0.039 |
| POST(-) | −2.9 ± 1.8 | −3.2 ± 1.8 | −3.8 ± 1.5 | n.s. | n.s. | n.s. |
| PROX(+) | 1.6 ± 2.1 | 2.0 ± 2.8 | 2.1 ± 2.3 | n.s. | n.s. | n.s. |
| DIST(-) | −3.6 ± 1.9 | −4.5 ± 2.0 | −10.6 ± 5.9 | 0.008 | 0.008 | 0.008 |
| FLEX(+) | 19.0 ± 5.4 | 22.2 ± 6.8 | 33.9 ± 6.5 | 0.008 | 0.008 | 0.008 |
| EXT(-) | −104.8 ± 7.3 | −117.9 ± 5.8 | −123.8 ± 7.4 | 0.008 | n.s. | n.s. |
| ADD(+) | 11.9 ± 13.6 | 20.3 ± 12.2 | 22.7 ± 14.6 | 0.008 | 0.008 | 0.016 |
| ABD(-) | −36.6 ± 5.1 | −43.7 ± 8.2 | −53.5 ± 18.5 | 0.008 | 0.008 | n.s. |
| INT R(+) | 24.3 ± 6.7 | 28.8 ± 9.3 | 49.8 ± 13.0 | 0.008 | 0.016 | 0.016 |
| EXT R(-) | −39.8 ± 11.4 | −47.3 ± 14.2 | −55.8 ± 12.2 | 0.008 | 0.008 | 0.016 |
n.s. no significance
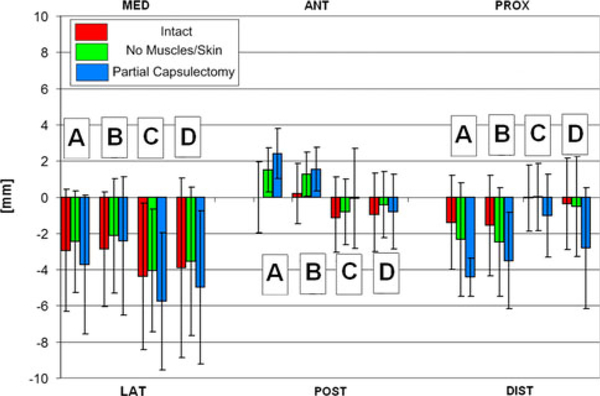
Additionally, angular positions (i.e. flex/ext, abd/add and IR/ER) and femoral head displacement relative to the acetabulum centre were assessed in a few clinically important hip positions, which were defined as:
Full Flexion—Adduction—Internal Rotation (some use as impingement test of the hip) (A in Fig. 3);
90° Flexion—Adduction—Internal Rotation (true impingement test of the hip) (B in Fig. 3);
Full Extension—External Rotation (used to assess posterior hip impingement) (C in Fig. 3);
Full Extension—Adduction—External Rotation (used to assess anterior hip instability and/or posterior hip impingement) (D in Fig. 3).
Fig. 3.
Medial/lateral (MED/LAT), anterior/posterior (ANT/POST) and proximal/distal (PROX/DIST) displacement corresponding to: full flexion—adduction—internal rotation (A); 90° flexion—adduction—internal rotation (B); full extension—external rotation (C); full extension—adduction—external rotation (D)
Changes in femoral head displacement in these defined hip positions are shown in Fig. 3. Similarly, the mean angular values corresponding to the mean maximal femoral head displacements are shown in Fig. 4, with particular emphasis on the position that results in:
maximal anterior femoral head displacement (A in Fig. 4);
maximal posterior femoral head anatomical centre displacement (B in Fig. 4);
maximal lateral femoral head displacement (C in Fig. 4).
Fig. 4.
Ranges of flexion/extension (FLEX/EXT) abduction/adduction (ABD/ADD) and internal/external (INT/EXT) rotation corresponding to: maximal anterior displacement (A); maximal posterior displacement (B); max lateral displacement (C)
Discussion
The most important finding of the present study was to highlight the effective importance of peri-articular soft tissues to hip joint kinematics and passive stability, underlining the behaviour of the hip that does not act as a perfect ball-and-socket joint.
Much of the previous work on hip biomechanics and kinematics related to joint arthroplasty. In the non-arthroplasty hip, soft tissue kinematic and biomechanical research have evaluated the check-rein role of the different hip capsuloligamentous structures for stability and limitation of motion [4, 5, 12, 15, 16, 20, 27, 30] as well as recent work on the function of the acetabular labrum[3,8–11,29].However, the role of these and other peri-articular structures on the ball-and-socket biomechanics of the non-arthritic hip joint has not been studied extensively [22, 24, 25]. Rydell summarized that the hip joint looks like a ball-and-socket joint but does not act completely like one [25]. Rydell noted that the femoral head pivots against the acetabulum, and thus is more of a gimbal constructed joint, not a ball-and-socket joint [25]. Morris defined the hip as a ball-and-socket joint that is polyaxial, but again, specific kinematics was lacking [22].
This study helps shed light on the relative contributions of the peri-articular soft tissues to passive hip joint kinematics. Specifically, this study highlights the role of the various soft tissue structures on hip joint kinematics. First, contrary to expectations with a ball-and-socket joint, passive ROM increases with serially soft tissue excision. However, perhaps more importantly, this study clearly shows the hip does not function as a true ball-and-socket joint, in that the femoral head translates multidirectionally with passive hip motion with all the soft tissues intact and that gradual removal of soft tissue constraints increases the translations of the femoral head within the acetabulum, despite maintaining an intact labrum. This may be important when considering the risk of labral injury, as well as for the protection of labral repairs. Additionally, ligamentous injury associated with hip subluxation and dislocation, or with surgery, may have potential deleterious effects by allowing greater femoral head translations. This may lead to articular cartilage or labral injury as a result of shear stresses or edge loading.
Using our navigation system to study hip joint kinematics, removal of skin and muscle did increase hip ROM, nearly equally in all planes (rotation and abduction/adduction) to a small degree with the hip extended fully or at 0° flexion/extension. At 90° flexion, the hip motions are increased relatively symmetrically, but greater magnitude as compared with neutral flexion–extension or hip extension, and this may be the result of the contribution of the hip ligaments that are anterior to the hip and are taut in extension and lax in flexion. In full hip flexion, removal of the skin and muscle increased the rotations and abduction arc the most, but particularly in adduction and internal rotation. Femoral head anatomical centre translations increased only minimally when the skin and muscles were removed, regardless of hip flexion/extension. The directions of these translations are predominantly distally and laterally. With the hip in the fully flexed position, however, there was also anterior translation of the femoral head when the muscles and skin were removed.
With the capsule circumferentially cut, passive hip ROM expectantly increased globally. However, the increase in abduction/adduction was minimal, while internal rotation increased most in all degrees of hip flexion. This would be expected, as the hip ligaments appear to anatomically provide rotational control. Taking into account that this study did not evaluate the role of joint reactional forces, this study confirms that the ligaments play a greater role in the passive stability of the joint, as compared with the other soft tissues, such as the periarticular muscles.
Additional function of the hip capsuloligamentous structures in joint constraint was evident. Femoral head translation was significantly increased, predominantly laterally, but also anteriorly in hip extension and neutral flexion–extension and 90° hip flexion. There was even greater lateral and anterior head translation at full flexion. At both 90° hip flexion, and even more so in full flexion, there was significant distal translation of the femoral head when the capsuloligamentous structures were partially excised, confirming the importance of these structures in higher degrees of flexion.
It should be noted that the displacements appear to be quite large. This could be the result of several factors. First, manual stresses were applied directly to the joint, thus achieving the limits of constrained movement of the joint prior to subluxation. Another potential reason for this apparent large amount of displacement may be the lack of joint reactional forces or weight-bearing loads, compressing the joint that may reduce the translations. Even considering these limitations, our findings are consistent with the maximum displacements obtained with the MRI-based in vivo analysis performed by Gilles et al. [14].
This study does present some other limitations. First, this study was performed in a passive fashion, without the benefit of muscular load replicating joint reactional forces or weight-bearing loads. However, this is the first study to actually determine the contributions of the non-contractile peri-articular structures on hip joint stability, regardless of the fact that it is in a passive, not loaded state. This provides an initial understanding to the contribution of these structures. Further studies will allow the addition of the muscular contribution and load bearing in this constrained joint to joint stability and femoral head motion relative to the acetabulum. Hip examination hip under anaesthesia may be similar to what was studied here, and thus may help in the evaluation of the surgical patient. Second, this study used fresh-frozen cadaver specimens with an average age of 72 years. While this may not be the average age population that one would be clinically evaluating with nonarthritic hip problems, we feel the kinematics should be similar. If anything, the soft tissues may be more “stiff” and less compliant in these older specimens, suggesting our results may underestimate femoral head motion relative to the acetabulum, as well as gains in ROM by the removal of soft tissues. Another limitation is the fact we did not apply a controlled, measured load to the femur as we moved the hip. However, being that the positions were either set degrees (0 or 90) that could be obtained from the optoelectric navigation system or the end ROM, we felt that a load control was not necessary, especially since one surgeon performed all the tests, and repeated the tests 3 times for reliability testing. Based on our results, particularly the high ICC with our repeat testing, the need for an objective force measurement tool was unnecessary.
From the clinical point of view and day-by-day practice, this information may allow for better understanding of the significance of physical examination manoeuvres in assessing joint stability and the importance of the implication of peri-articular soft tissues on hip kinematics, as well.
Moreover, the study also suggests that further investigations are necessary to understand the implications of femoral head anatomical centre displacement within the acetabulum in the context of a possible prevention of degenerative osteoarthritis. Moreover, the influence of different surgical labral repairs on hip stability has to be analysed. Furthermore, the effects of the individual capsuloligamentous structures on hip stability and anatomical centre displacement are also in need of further study.
Conclusion
This study shows the femoral head moves relative to the acetabulum in the intact state, and soft tissue damage may result in increased femoral head translations. The clinical significance of this is unclear, though there is concern that excessive translations may result in hip arthritis. Further, peri-articular soft tissues affect passive hip range of motion.
The findings of this study are a preliminary contribution in the understanding of the contribution of the passive structures of muscles, joint capsule and ligaments to hip joint kinematics.
Contributor Information
Marc R. Safran, Department of Orthopaedic Surgery, Stanford University, Medical Center, Stanford, CA, USA
Nicola Lopomo, Laboratorio di Nano Biotecnologie, NaBi, Istituto Ortopedico Rizzoli, Bologna, Italy, Laboratorio di Biomeccanica e Innovazione Tecnologica, Istituto, Ortopedico Rizzoli, via Di Barbiano, 1/10, Bologna, Italy, n.lopomo@biomec.ior.it.
Stefano Zaffagnini, Laboratorio di Biomeccanica e Innovazione Tecnologica, Istituto, Ortopedico Rizzoli, via Di Barbiano, 1/10, Bologna, Italy.
Cecilia Signorelli, Dipartimento di Bioingegneria, Politecnico di Milano, Milan, Italy, Laboratorio di Biomeccanica e Innovazione Tecnologica, Istituto, Ortopedico Rizzoli, via Di Barbiano, 1/10, Bologna, Italy.
Zackary D. Vaughn, Department of Orthopaedic Surgery, Stanford University, Medical Center, Stanford, CA, USA
Derek P. Lindsey, Bone and Joint Center, VA Palo Alto Health Care System, Stanford University, Stanford, CA, USA
Garry Gold, Department of Orthopaedic Surgery, Stanford University, Medical Center, Stanford, CA, USA.
Giovanni Giordano, Ospedale “Morgagni-Pierantoni”, U.O. Ortopedia e Traumatologia, Forlì, Italy.
Maurilio Marcacci, Laboratorio di Biomeccanica e Innovazione Tecnologica, Istituto, Ortopedico Rizzoli, via Di Barbiano, 1/10, Bologna, Italy.
References
- 1.Bland JM, Altman DG (1996) Measurement error and correlation coefficients. BMJ 313:41–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Byrd JWT, Jones KS (2009) Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res 467:739–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, Patel RV, Miller AR, McCarthy JC, Lowe WR, Noble PC (2007) The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res 465:16–22 [DOI] [PubMed] [Google Scholar]
- 4.Crowninshield RD, Johnston RC, Brand RA, Pedersen DR (1983) Pathologic ligamentous constraint of the hip. Clin Orthop Relat Res 181:291–297 [PubMed] [Google Scholar]
- 5.Crowninshield RD, Johnston RC, Andrews JG, Brand RA (1978) A biomechanical investigation of the human hip. J Biomech 11: 75–85 [DOI] [PubMed] [Google Scholar]
- 6.Daniel M, Iglic A, Kralj-Iglic V (2005) The shape of acetabular cartilage optimizes hip contact stress distribution. J Anat 207: 85–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis KE, Ritter MA, Berend ME, Meding JB (2007) The importance of range of motion after total hip arthroplasty. Clin Orthop Relat Res 465:180–184 [DOI] [PubMed] [Google Scholar]
- 8.Dy CJ, Thompson MT, Crawford MJ, Alexander JW, McCarthy JC, Noble PC (2008) Tensile strain in the anterior part of the acetabular labrum during provocative maneuvering of the normal hip. J Bone Joint Surg Am 90(A):1464–1472 [DOI] [PubMed] [Google Scholar]
- 9.Ferguson SJ, Bryant JT, Ganz R, Ito K (2003) An in vitro in vestigation of the acetabular labral seal in hip joint mechanics. J Biomech 36:171–178 [DOI] [PubMed] [Google Scholar]
- 10.Ferguson SJ, Bryant JT, Ito K (2001) The material properties of the bovine acetabular labrum. J Orthop Res 19:887–896 [DOI] [PubMed] [Google Scholar]
- 11.Ferguson SJ, Bryant JT, Ganz R, Ito K (2000) The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech 33:953–960 [DOI] [PubMed] [Google Scholar]
- 12.Fuss FK, Bacher A (1991) New aspects of the morphology and function of the human hip joint ligaments. Am J Anat 192:1–13 [DOI] [PubMed] [Google Scholar]
- 13.Gamage SSHU, Lasenby J (2002) New least squares solutions for estimating the average centre of rotation and the axis of rotation. J Biomech 35:87–93 [DOI] [PubMed] [Google Scholar]
- 14.Gilles B, Christophe FK, Magnenat-Thalmann N, Becker CD, Duc SR, Menetrey J, Hoffmeyer P (2009) MRI-based assessment of hip joint translations. J Biomech 42(9):1201–1205 [DOI] [PubMed] [Google Scholar]
- 15.Hewitt JD, Glisson RR, Guilak F, Vail TP (2002) The mechanical properties of the human hip capsule ligaments. J Arthroplasty 17:82–89 [DOI] [PubMed] [Google Scholar]
- 16.Hewitt J, Guilak F, Glisson R, Vail TP (2001) Regional material properties of the human hip joint capsule ligaments. J Orthop Res 19:359–364 [DOI] [PubMed] [Google Scholar]
- 17.Kelly BT, Weiland DE, Schenker ML, Philippon MJ (2005) Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy 21:1496–1504 [DOI] [PubMed] [Google Scholar]
- 18.Konrath GA, Hamel AJ, Olson SA, Bay B, Sharkey NA (1998) The role of the acetabular labrum and the transverse acetabular ligament in load transmission in the hip. J Bone Joint Surg Am 80:1781–1788 [DOI] [PubMed] [Google Scholar]
- 19.Larson CM, Guanche CA, Kelly BT, Clohisy JC, Ranawat AS(2009) Advanced techniques in hip arthroscopy. Instr Course Lect 58:423–436 [PubMed] [Google Scholar]
- 20.Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B(2008) The function of the hip capsular ligaments: a quantitative report. Arthroscopy 24:188–195 [DOI] [PubMed] [Google Scholar]
- 21.Martelli S, Lopomo N, Bignozzi S, Zaffagnini S, Visani A (2007) Validation of a new protocol for navigated intraoperative assessment of knee kinematics. Comput Biol Med 37:872–878 [DOI] [PubMed] [Google Scholar]
- 22.Morris JM (1971) Biomechanical aspects of the hip joint. Orthop Clin North Am 2(1):33–54 (review) [PubMed] [Google Scholar]
- 23.Murray DW (1993) The definition and measurement of acetabular orientation. J Bone Joint Surg Br 75:228–232 [DOI] [PubMed] [Google Scholar]
- 24.Nordin M, Frankel VH (1980) Biomechanics of the Hip In: Frankel VH (ed) Basic biomechanics of the skeletal system. Lea & Febiger, Philadelphia, pp 149–177 [Google Scholar]
- 25.Rydell N (1972) Biomechanics of the hip joint. Clin Orthop RelRes 92:5–15 [DOI] [PubMed] [Google Scholar]
- 26.Siston RA, Delp SL (2006) Evaluation of a new algorithm to determine the hip joint center. J Biomech 39:125–130 [DOI] [PubMed] [Google Scholar]
- 27.Stewart KJ, Edmonds-Wilson RH, Brand RA, Brown TD (2002) Spatial distribution of hip capsule structural and material properties. J Biomech 35:1491–1498 [DOI] [PubMed] [Google Scholar]
- 28.Stewart KJ, Pedersen DR, Callaghan JJ, Brown TD (2004) Implementing capsule representation in a total hip dislocation finite element model. Iowa Orthop J 24:1–8 [PMC free article] [PubMed] [Google Scholar]
- 29.Takechi H, Nagashima H, Ito S (1982) Intra-articular pressure of the hip joint outside and inside the limbus. Nippon Seikeigeka Gakkai Zasshi 56:529–536 [PubMed] [Google Scholar]
- 30.Vrahas MS, Brand RA, Brown TD, Andrews JG (1990) Contribution of passive tissues to the intersegmental moments at the hip. J Biomech 23:357–362 [DOI] [PubMed] [Google Scholar]
- 31.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech 35:543–548 [DOI] [PubMed] [Google Scholar]
- 32.Zaffagnini S, Bignozzi S, Martelli S, Imakiire N, Lopomo N,Marcacci M (2006) New intraoperative protocol for kinematic evaluation of ACL reconstruction: preliminary results. Knee Surg Sports Traumatol Arthrosc 14:811–816 [DOI] [PubMed] [Google Scholar]
- 33.Ziegert AJ, Blankenbaker DG, De Smet AA, Keene JS, Shinki K,Fine JP (2009) Comparison of standard hip MR arthrographic imaging planes and sequences for detection of arthroscopically proven labral tear. AJR Am J Roentgenol 192:1397–1400 [DOI] [PubMed] [Google Scholar]