Abstract
Objectives:
To compare the effect of toric versus spherical soft contact lenses on objective measures of visual performance using visual acuity and electromyography of the orbicularis oculi muscle.
Methods:
Current soft contact lens wearers with −0.75 to −1.75 D astigmatism in each eye were binocularly fitted with toric (1-Day ACUVUE MOIST for astigmatism) and spherical (1-Day ACUVUE MOIST) contact lenses in random order. After each fitting and at 1-week follow-up, high- and low-contrast visual acuities were measured. Electromyography was used to objectively evaluate eyestrain. Linear mixed models were used to assess differences between toric and spherical contact lenses.
Results:
The mean age (±SD) of the 60 participants was 27.5±5.0 years, spherical refractive error was −3.68±2.01 D, and cylinder was −1.28±0.36 D. High- and low-contrast visual acuities with toric lenses were better than with spherical lenses at both fitting (toric high-contrast: −0.065±0.078 and low-contrast: 0.133±0.103 vs. spherical high-contrast: 0.001±0.104 and low-contrast: 0.224±0.107) and follow-up (toric high-contrast: −0.083±0.087 and low-contrast: 0.108±0.107 vs. spherical high-contrast: −0.015±0.095 and low-contrast: 0.211±0.104) (all P<0.0001). Electromyography-measured eyestrain was less with toric versus spherical contact lenses at fitting (least-square ratio of toric over spherical=0.72; P=0.0019) but not at follow-up (ratio=0.86; P=0.11).
Conclusion:
These results suggest that toric contact lenses provided improved objective measures of vision in a low-to-moderate astigmatic population.
Key Words: Eyestrain, Toric contact lens, Electromyography, Astigmatism, Visual acuity
For many contact lens wearers, astigmatism is left uncorrected despite the availability of toric contact lenses. Approximately 47% of patients have 0.75 D of astigmatism or more in at least one eye,1 but astigmatism-correcting lenses, toric contact lenses, are only fitted on approximately 25% of patients.2 A review by Read et al.3 provides an excellent summary of vision-related compromises associated with uncorrected astigmatism. In studies investigating the use of contact lenses to correct astigmatism, high- and low-contrast visual acuity measures have been shown to improve with toric contact lenses compared with spherical contact lenses4,5 and aspheric lenses.6 Subjects also report improvement in vision with toric contact lenses compared with spherical contact lenses.5 Studies evaluating the effect of induced astigmatism on outcome measures beyond visual acuity have reported reduced reading speeds and subjective rating of clarity while using a computer and mobile phone, which were related to the amount of induced uncorrected astigmatism.7 Contact lens wearers also reported improved subjective comfort during visual display terminal use when their astigmatism was corrected versus when left uncorrected.8 Objective assessments of vision with toric contact lenses versus spherical contact lenses could help us better understand the benefits of toric contact lenses.
Eyestrain is the most common complaint among computer users9; therefore, establishing a method to assess it objectively is of specific relevance when astigmatism is left uncorrected. As both the use and variety of digital media platforms continue to grow, the impact of eyestrain in contact lens wearers is of interest. The use of electromyography as an objective measure of orbicularis oculi activity under glare conditions has been validated previously.10 Subsequent research reported increased electromyography responses in a variety of asthenopia-inducing conditions, including refractive error with astigmatism. This increased response due to refractive error was also associated with an eyelid squinting response in subjects.11 Electromyography responses have also been found to increase linearly with increasing amounts of astigmatism, which is also associated with a decrease in subjectively reported comfort while reading.12 These results demonstrate the utility of electromyography to achieve the purpose of this study, which is to compare eyestrain between toric contact lenses versus spherical contact lenses, with the prediction that toric contact lens wearers have reduced eyestrain with corresponding improvements in visual performance.
METHODS
This subject-masked, randomized, 2×2 cross-over study was approved by the University of Houston Committee for the Protection of Human Subjects and complied with the tenets of the Declaration of Helsinki. After providing informed consent for participation, subjects provided a medical and contact lens history. Subjects were required to be 18 to 45 years of age without the need for presbyopic correction. Their spherical refraction at the corneal plane had to be between +4.00 and +0.25D or −0.50 and −9.00D, inclusive. In addition, their cylinder power at the corneal plane had to be between −0.75 and −1.75 DC, inclusive. Subjects were also required to be habitual soft contact lens wearers (either spherical or toric) with a reported average wear frequency of at least 5 days a week and at least 8 hrs a day in the month before the initial visit. Subjects with eye abnormalities beyond refractive correction (e.g., previous ocular surgeries, slit-lamp examination findings that would contraindicate contact lens wear, active ocular infection, and strabismus) were excluded from the study.
Eligible subjects completed a total of four study visits at The Ocular Surface Institute at the University of Houston, College of Optometry. At study visit 1, subjects were randomly fit with either toric contact lenses (1-Day ACUVUE MOIST for astigmatism; Johnson & Johnson Vision Care, Inc., Jacksonville, FL) or spherical contact lenses (1-Day ACUVUE MOIST). Subjects who qualified for randomization were assigned a lens-type order by a trained examiner sequentially based on their first study visit using a printed computer-generated randomization scheme that specified into which lens the subject would be fit first. The randomization scheme was generated before subject enrollment. Subjects were masked to the lens type, and all lens packaging was masked by overlabelling. The initial contact lens power for each lens type was determined after referencing a standardized most plus/least minus manifest refraction to the corneal plane. For spherical contact lenses, the spherical equivalent power was selected. For toric contact lenses, the toric contact lens cylinder amount chosen was the closest value available without exceeding the amount of astigmatism at the corneal plane. Movement, coverage, centration, and rotation were assessed to ensure a proper fit. In the case of lens rotation, modification of the toric contact lens axis was determined using the clinical “LARS” procedure (left add, right subtract) as deemed necessary to optimize the contact lens prescription for the subject. The contact lens power was considered final when a spherical over-refraction of less than or equal to ±0.25DS was obtained that yielded best visual acuity. High-contrast distance visual acuity, low-contrast distance visual acuity, and electromyography with a distance target were performed after determining the final contact lens powers to be dispensed. Subjects were instructed to wear the study lenses on a full-time basis (a minimum of 5 days) before returning for visit 2, which was scheduled for 5 to 10 days after visit 1.
Subjects were required to have been wearing their assigned study contact lenses for at least 2 hrs before returning to the clinic for visit 2. After assessing for appropriate contact lens fit, high- and low-contrast visual acuity and electromyography were assessed with the study lenses as noted previously. At the conclusion of visit 2, subjects departed wearing their habitual contact lenses or spectacles and entered a washout period of 5 to 10 days before returning for visit 3. At study visit 3, subjects were fit with the lens type not previously assigned at study visit 1, and distance high- and low-contrast visual acuities and electromyography were assessed. Subjects wore the second pair of study contact lenses for 5 to 10 days before returning for visit 4 (the final visit). Like at visit 2, subjects had to have been wearing their assigned study lens for at least 2 hrs before the study visit, and assessments again included distance high- and low-contrast visual acuities and electromyography.
Outcome Procedures
This article highlights the secondary outcomes of this study: electromyography measures and high- and low-contrast visual acuity. Sample size was determined based on the primary outcome, which was a difference in the National Eye Institute Refractive Error Quality of Life questionnaire responses between spherical and toric contact lenses. A full description of the sample size calculation can be found in the article outlining these results.13 The study was closed upon reaching our sample size goal of having 60 subjects complete all study visits, per protocol.
Electromyography was used to record the electrical activity produced by the contraction of the orbicularis oculi muscle to objectively assess eyestrain. The electrical activity was assessed using two electrodes attached to the skin overlying the inferior portion of the orbicularis oculi muscle of the right eye in a horizontal orientation to each other. Both electrodes were approximately 1.5 cm below the lower right eyelid margin and separated by 1 cm. A ground electrode was attached to the left earlobe. This placement is based on the methods described previously that used skin electrode recordings to assess asthenopia and squint.12,14,15 Figure 1 shows the electromyography setup. The measurements were acquired using a GrassLink 15LT Physio acquisition system with LabVIEW PolyVIEW16 software at a rate of 1,000 samples per second for 40 sec. During the recording, subjects continuously read randomized sets of five 20/30 letters at 6% contrast from a Nidek-computerized distance visual acuity chart; the 20/30 letter size and 6% contrast were chosen to provide a visually demanding task.
FIG. 1.
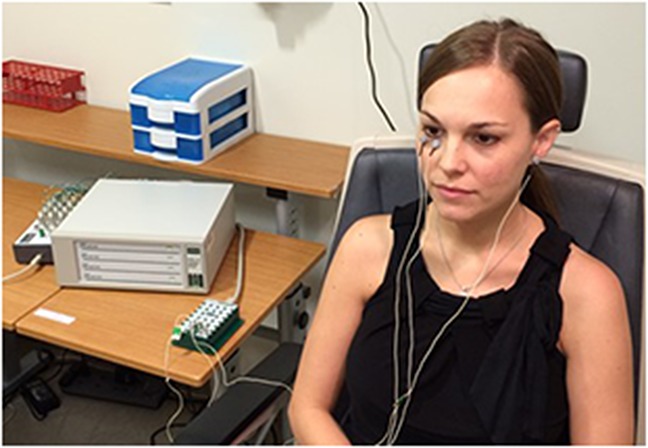
The experimental setup for the electromyography showing the placement of electrodes.
Distance visual acuity was assessed under photopic conditions using lightbox-mounted Precision Vision Early Treatment Diabetic Retinopathy Study (ETDRS) charts 4 m from the subject. For each measure, the chart luminance was confirmed to be at least 85 cd/m2. At each visit, high-contrast (100%) and low-contrast (10%) distance visual acuities were assessed monocularly with a different chart for each eye. Subjects started reading letters at the top of the chart and stopped after missing three or more letters on a single line. The number of letters correct and logMAR equivalent were recorded.
Statistical Analysis
Electromyography data were modeled based on a total of eight data points calculated from each electromyography recording. The 40-sec recording was broken into windows of 100 ms, and each window overlapped with the previous window by 50 ms (e.g., 1–100 ms, 51–151 ms, 101–201 ms, etc.). The root mean squared value of the electromyography data (in volts) was found for each window using the formula root mean squared 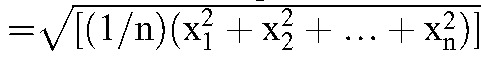 .16 Approximately 100 windowed root mean squared values were grouped to make 5-second blocks, and the median of each of the 5-second blocks was calculated to give a median root mean squared value. A log transformation was performed on the median root mean squared values before the linear mixed model analysis to achieve normality of the data.
.16 Approximately 100 windowed root mean squared values were grouped to make 5-second blocks, and the median of each of the 5-second blocks was calculated to give a median root mean squared value. A log transformation was performed on the median root mean squared values before the linear mixed model analysis to achieve normality of the data.
Linear mixed models were used to compare high-contrast visual acuity, low-contrast visual acuity, and electromyography data between the toric contact lenses and spherical contact lenses. The high-contrast visual acuity and low-contrast visual acuity models controlled for the order of lenses (toric contact lenses first vs. spherical contact lenses first), lens wear period, lens, event (fitting visit versus follow-up visit), and the lens by event interaction. The electromyography model controlled for order of lenses, lens wear period, lens, event, time interval (the eight data points per electromyography recording described above) as well as all two- and three-way interactions for lens, event, and time interval.
RESULTS
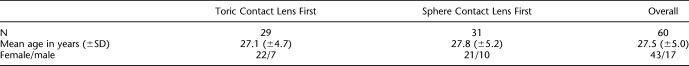
Sixty subjects completed the study per protocol between September 2013 and June 2014 and were included in the analysis. Thirty-nine subjects were assigned to be fitted in toric contact lenses first; however, eight were discontinued after being randomized or were excluded from analyses due to failure to follow the study protocol. Thirty-nine subjects were assigned to be fitted in spherical contact lenses first, but 10 were discontinued or excluded from the analyses because of failure to follow the study protocol. The reasons for discontinuation/exclusion include failure to meet inclusion criteria for the length of enrollment (2), unsatisfactory lens fit or discomfort (5), subjects being lost to follow-up or not adhering to the protocol (10), or the electromyography device not working properly to allow for data acquisition at time of visit (1). Three subjects discontinued because of lens discomfort and/or blurred vision, and one subject was found to not be eligible on secondary chart review. Table 1 provides the demographic information for each group and for the entire sample that was used in all analyses. Based on manifest refraction, the mean (±SD) spherical refractive error was −3.68±2.01 D and mean (±SD) cylindrical refractive error was −1.28±0.36 DC. The manifest refraction axis was distributed as follows: 180°±20°=79.2%; 90°±30°=12.5%; and other =8.3%. Sixty-five percent of the subjects habitually wore toric contact lenses bilaterally, and 31.7% wore spherical contact lenses bilaterally. Two subjects wore a toric contact lens in one eye and spherical contact lens in the other.
TABLE 1.
Demographic Information by Randomization Group
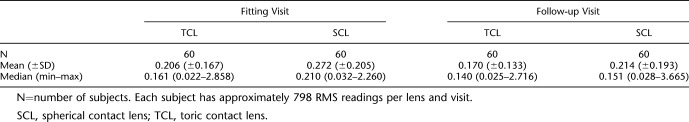
Table 2 shows the mean and median electromyography root mean squared values for subjects while wearing toric contact lenses and spherical contact lenses at both the fitting and follow-up visits. Electromyography recordings showed less orbicularis muscle activity with toric contact lenses compared with spherical contact lenses at the fitting visit. As shown in Figure 2, which illustrates the least-square mean ratio at each visit (toric contact lenses/spherical contact lenses) of the log-transformed median root mean squared values, orbicularis muscle activity with toric contact lens wear was significantly less than with spherical contact lens wear at the fitting visit (P=0.0019) but was not different between lens types at follow-up (P=0.11).
TABLE 2.
Electromyography (EMG) root mean squared (RMS) Data in Volts (Before Log Transformation)
FIG. 2.
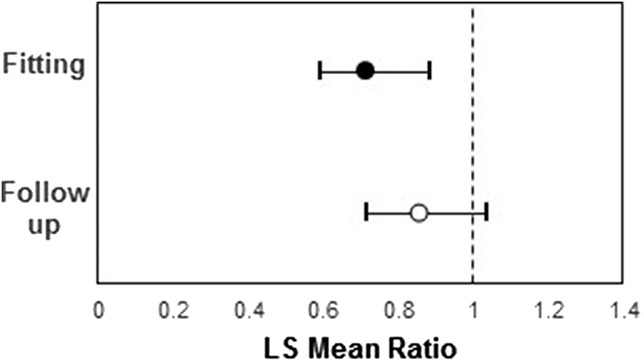
Least-square (LS) mean ratio of the log-transformed electromyography median root mean squared (RMS) values at the fitting visit and follow-up visit. The dashed line represents no difference. Area to the left of the dashed line indicates less eyestrain with toric contact lenses, and area to the right of the dashed line indicates less eyestrain with spherical contact lenses.
Toric contact lenses provided better high- and low-contrast visual acuities at both the fitting visits (study visits 1 and 3) and follow-up visits (study visits 2 and 4) as shown in Figure 3. At the fitting visit, the least-square mean difference (toric contact lenses – spherical contact lenses) in logMAR was −0.07 (3.5 letter improvement; 95% confidence interval: −0.09 to −0.04) for high-contrast visual acuity and −0.09 (4.5 letter improvement; 95% confidence interval: −0.12 to −0.06) for low-contrast visual acuity. At the follow-up visit, the least-square mean difference in logMAR was −0.07 (3.5 letter improvement; 95% confidence interval: −0.09 to −0.05) for high-contrast visual acuity and −0.10 (5 letter improvement; 95% confidence interval: −0.13 to −0.08) for low-contrast visual acuity. The improvement with toric contact lenses was statistically significant for distance high- and low-contrast visual acuities at both the fitting and follow-up visits (all P<0.0001).
FIG. 3.
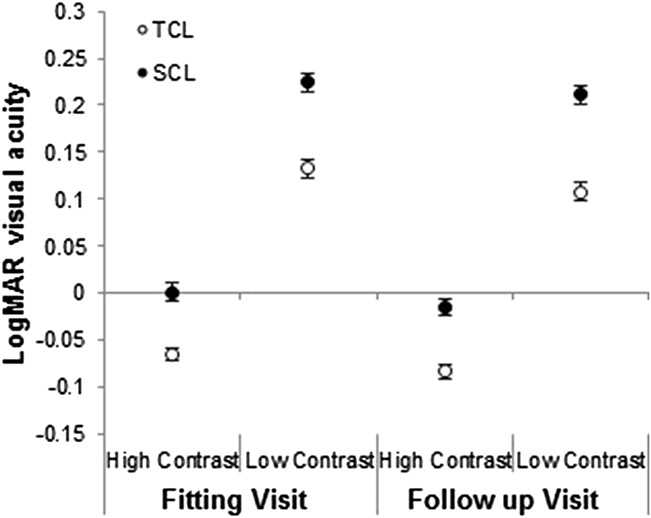
Mean (±SE) high- and low-contrast logMAR distance visual acuity measured at the fitting and follow-up visits with toric contact lenses (TCLs) and spherical contact lenses (SCLs).
DISCUSSION
This study showed improved visual function with toric contact lenses compared with spherical contact lenses in low-to-moderate astigmatic subjects. As far as we are aware, this study was the first to use electromyography in contact lens wearers to assess the contribution of astigmatism to eyestrain. This study was not designed to assess the correlation between eyestrain and amount of astigmatism; however, a previous study showed increased eyestrain with larger amounts of uncorrected astigmatism.12 It is interesting that the present results showed a statistically significant reduction in objective eyestrain at the fitting visit but not at the follow-up visit. This inconsistency in the electromyography results could potentially be explained by adaptation to the mild blur caused by uncorrected astigmatism resulting in less squinting or strain after a week of adaptation to spherical contact lenses. A hypothesis of adaptation was also proposed in a study that showed reduced orbicularis oculi activity assessed using electromyography in the 2nd hr of computer work compared with the 1st hr.17
These electromyography results should also be considered in context with the high- and low-contrast visual acuity data and subjective questionnaire data that we previously reported.13 Although the improvements in both high- and low-contrast visual acuities with toric contact lenses versus spherical contact lenses were consistent at both the fitting visit and the follow-up visit, the electromyography root mean squared data only showed significantly reduced eyestrain at the fitting visit. The National Eye Institute Refractive Error Quality of Life questionnaire global score, the clarity of vision subscale score and satisfaction with correction subscale score all showed subjective improvements with toric (74.9±10.5, 75.7±46.0, 79.7±15.5, respectively) versus spherical contact lenses (67.6±14.4, 50.1±31.7, 62.0±28.9, respectively) at the follow-up visit. These improved subjective scores demonstrate that the subjects within this study preferred toric contact lenses to spherical contact lenses at follow-up.13 Although improvement with toric contact lenses is not reflected in the electromyography recordings at the follow-up visit, this lack of sustained electromyography improvement at follow-up is consistent with the hypothesis that subjects adapted to the reduced image quality caused by uncorrected astigmatism resulting in less eyestrain/squinting when wearing spherical contact lenses despite still noting a difference between lens types. Both subjective refractive quality of life and objective visual acuity favored toric over spherical contact lenses at follow-up, demonstrating that astigmatic patients benefitted from toric contact lenses even if no difference in eyestrain was detected at the follow-up visit. Further work is needed to confirm this finding.
Studies finding proposed neural adaptation to the eye's habitual astigmatism support this hypothesis.18 Previous work has found that after just 4 hrs of deprivation in a specific orientation, such as occurs with uncorrected astigmatism, there is increased sensitivity in that particular orientation.19 Although this increased sensitivity did not result in meaningful improvements in visual acuity from the fitting to follow-up visit in our study, this adaptation perhaps was adequate to reduce squinting and eyestrain with spherical contact lenses after wearing them for a week, resulting in no difference in electromyography values when wearing the toric contact lenses and spherical contact lenses at the follow-up visit. An alternative hypothesis is that the initial exposure to the electromyography procedures experienced by the subjects at the fitting visit may have been associated with some stress and may have impacted the measures collected. The subjects may have been more comfortable with the measurement at the follow-up visit. The impact of stress associated with this initial exposure to the electromyography system was minimized by randomizing the order of toric contact lenses and spherical contact lenses for each subject. Further studies are needed to better understand the influence of neural adaptation on eyestrain and the impact of initial exposure to testing.
Visual improvements were illustrated with measures of distance high- and low-contrast visual acuities. Subjects, on average, experienced over half of a line improvement (3.5 letters) in high-contrast acuity and a full-line (5 letters) improvement in low-contrast acuity when fitted with toric contact lenses versus spherical contact lenses. The improvements in high- and low-contrast visual acuities observed in this study were in agreement with previous studies.4–6,20 Morgan et al. evaluated toric contact lenses compared with aspheric soft contact lenses in subjects with −0.75 to −1.00 D of astigmatism and found a 2- to 5-letter improvement in high-contrast visual acuity with toric contact lenses only, depending on the pupil size. The same study also found a 1-line improvement in low-contrast visual acuity, similar to our study with toric contact lenses versus spherical contact lenses.6 The current results are also similar to a study by Richdale et al.4 that found between a 3- and 5.5-letter improvement in high-contrast visual acuity with toric contact lenses versus spherical contact lenses in subjects with −0.75 to −1.00 D of astigmatism depending on room illumination, and a 11-letter improvement with toric contact lenses in subjects with −1.25 D to −2.00 D of astigmatism. This same study also reported a 3.5-letter improvement in low-contrast visual acuity with toric contact lenses in subjects with −0.75 to −1.00 D of astigmatism, and an 8.5- to 12.5-letter improvement in subjects with −1.25 to −2.00 D of astigmatism, depending on room illumination. Also consistent with these studies, Cho et al.5 found a 5.5-letter (1-line) improvement in low-contrast visual acuity with toric contact lenses versus spherical contact lenses in subjects with −0.75 to −1.25 D of astigmatism; subjects also rated their vision as better with toric contact lenses. Although a recent study by Gaib and Vasudevan20 did not find meaningful improvements in vision with custom toric contact lenses compared with spherical contact lenses, their study included cylinder amounts of −0.50 to −1.00 DC with 60% of subjects only having −0.50 of astigmatism. By contrast, this study excluded subjects with only −0.50 D of astigmatism, and the subjects had a mean cylindrical refractive error of −1.28±0.36 DC. The inclusion of a significant number of subjects with only −0.50 D of astigmatism, a level of astigmatism below the amount that most toric contact lenses correct and below which most practitioners correct with contact lenses, likely explains the minimal visual acuity improvements in their study.
A limitation of this study was that only one toric contact lens design was evaluated. Differences in toric contact lens design and stabilization method can influence the rotational stability of the lens and the higher-order aberrations caused by the lens design.21 Clinicians should keep in mind that our results apply to the two lenses tested in this study. With the potential influence of these lens design and fit characteristics, it is possible that our results could vary with different designs. Another limitation was that eyestrain was only assessed using electromyography for a single low-contrast target at distance. A patient's visual experience throughout the day includes a range of contrast levels, working distances, and lighting conditions. Additional distance and near targets under various illuminations may better capture the overall influence of eyestrain on a patient's visual function. Finally, although we made every effort to mask subjects to the type of contact lens they were wearing in each phase of the study (sphere vs. toric), an astute observer might have noticed differences in the lens characteristics, such as toric lens markings. Although this potential exists, we feel that it is unlikely that these observations had a significant influence on the study outcomes, given that differences in visual acuity between lens types at the fitting visits (where only examiners handled the lenses before testing) were consistent with visual acuity differences at the follow-up visits.
With the rise in computer use around the world and the variety of electronic devices available to consumers, objective measures, such as electromyography, should be further developed to ensure that eyestrain is minimized for patients. Although this study assessed eyestrain at distance with a low-contrast target, future studies should consider the utilization of electromyography to assess eyestrain at a computer as well as while reading in contact lens wearers. Although the goal of this study was to examine the benefits of toric contact lenses in subjects with low-to-moderate levels of astigmatism, a future study should evaluate whether subjects with more astigmatism show the hypothesized adaptation between the fitting and follow-up. In addition, studies should consider the impact of astigmatism correction in relation to other factors commonly associated with computer vision syndrome, such as tear film instability and binocular vision disorders.
Overall, these results confirmed that toric contact lenses, in low-to-moderate astigmats, improved visual acuity by roughly 1 line compared with spherical contact lenses. Objective reductions in eyestrain were measured by electromyography with toric contact lenses versus spherical contact lenses at the time of lens fitting. These results support the use of toric contact lenses even in patients with low-to-moderate astigmatism.
Footnotes
B. K. Little and K. O. Lorenz are employed by Johnson & Johnson Vision Care, Inc. While the other authors have no conflicts of interest related to the content of this manuscript, they have all been funded by Johnson & Johnson Vision Care, Inc.
Supported by Johnson & Johnson Vision Care, Inc.
A portion of this work was presented at the October 2015 American Academy of Optometry Annual Meeting, New Orleans, LA; the January 2016 Global Specialty Lens Symposium, Las Vegas, NV; and the March 2016 British Contact Lens Association and Netherlands Contact Lens Congress, Veldhoven, The Netherlands.
Clinicaltrials.gov Registration: NCT01857102.
REFERENCES
- 1.Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens 2011;37:20–25. [DOI] [PubMed] [Google Scholar]
- 2.Morgan PB, Efron N, Woods CA. An international survey of toric contact lens prescribing. Eye Contact Lens 2013;39:132–137. [DOI] [PubMed] [Google Scholar]
- 3.Read SA, Vincent SJ, Collins MJ. The visual and functional impacts of astigmatism and its clinical management. Ophthalmic Physiol Opt 2014;34:267–294. [DOI] [PubMed] [Google Scholar]
- 4.Richdale K, Berntsen DA, Mack CJ, et al. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci 2007;84:969–975. [DOI] [PubMed] [Google Scholar]
- 5.Cho P, Cheung SW, Charm J. Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for astigmatism in subjects with low astigmatism. Clin Exp Optom 2012;95:43–47. [DOI] [PubMed] [Google Scholar]
- 6.Morgan PB, Efron SE, Efron N, et al. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optom Vis Sci 2005;82:823–828. [DOI] [PubMed] [Google Scholar]
- 7.Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. J Cataract Refractive Surg 2011;37:454–460. [DOI] [PubMed] [Google Scholar]
- 8.Wiggins N, Daum K, Snyder C. Effects of residual astigmatism in contact lens wear on visual discomfort in VDT use. J Am Optometric Assoc 1992;63:177–181. [PubMed] [Google Scholar]
- 9.Agarwal S, Goel D, Sharma A. Evaluation of the factors which contribute to the ocular complaints in computer users. J Clin Diagn Res 2013;7:331–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berman S, Bullimore M, Jacobs R, et al. An objective measure of discomfort glare. J Illuminating Eng Soc 1994;23:40–49. [Google Scholar]
- 11.Gowrisankaran S, Sheedy JE, Hayes JR. Eyelid squint response to asthenopia-inducing conditions. Optom Vis Sci 2007;84:611–619. [DOI] [PubMed] [Google Scholar]
- 12.Nahar NK, Sheedy JE, Hayes J, et al. Objective measurements of lower-level visual stress. Optom Vis Sci 2007;84:620–629. [DOI] [PubMed] [Google Scholar]
- 13.Cox SM, Berntsen DA, Bickle K, et al. Efficacy of toric contact lenses in fitting and patient-reported outcomes in contact lens wearers. Eye Contact Lens 2017. Epub ahead of print. [DOI] [PubMed]
- 14.Nahar NK, Gowrisankaran S, Hayes JR, et al. Interactions of visual and cognitive stress. Optometry 2011;82:689–696. [DOI] [PubMed] [Google Scholar]
- 15.Gowrisankaran S, Nahar NK, Hayes JR, et al. Asthenopia and blink rate under visual and cognitive loads. Optom Vis Sci 2012;89:97–104. [DOI] [PubMed] [Google Scholar]
- 16.Clancy EA, Morin EL, Merletti R. Sampling, noise-reduction and amplitude estimation issues in Surface electromyography. J Electromyogr Kinesiol 2002;12:1–16. [DOI] [PubMed] [Google Scholar]
- 17.Thorud HM, Helland M, Aaras A, et al. Eye-related pain induced by visually demanding computer work. Optom Vis Sci 2012;89:E452–E464. [DOI] [PubMed] [Google Scholar]
- 18.Marcos S, Velasco-Ocana M, Dorronsoro C, et al. Impact of astigmatism and high-order aberrations on subjective best focus. J Vis 2015;15:4. [DOI] [PubMed] [Google Scholar]
- 19.Zhang P, Bao M, Kwon M, et al. Effects of orientation-specific visual deprivation induced with altered reality. Curr Biol 2009;19:1956–1960. [DOI] [PubMed] [Google Scholar]
- 20.Gaib SN, Vasudevan B. Low toric soft contact lens acceptance study. Cont Lens Anterior Eye 2015;38:194–198. [DOI] [PubMed] [Google Scholar]
- 21.Berntsen DA, Merchea MM, Richdale K, et al. Higher-order aberrations when wearing sphere and toric soft contact lenses. Optom Vis Sci 2009;86:115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]