Supplemental Digital Content is Available in the Text.
The China data of GBD 2016 found that 6.73 × 107 individuals had low back pain, and the prevalence was 4.2%. The years lived with disability were 7.7 million and years lived with disability rate was 481.9/100,000.
Keywords: Low back pain, Prevalence, Years live with disability, China, Global burden of disease study
Abstract
The aim of this work was to quantify the prevalence and years lived with disability (YLDs) caused by low back pain (LBP) in China from 1990 to 2016. Data from the GBD 2016 (Global Burden of Diseases, Injuries, and Risk Factors Study 2016) were used. We analyzed the age-sex-province-specific prevalence and YLDs for LBP of 33 provinces/regions in China. Comparisons were made with the data retrieved from the 1990 GBD study. We estimated that 5.45 × 107 individuals had LBP in 1990, which rose to 6.73 × 107 in 2016. The age-standardized prevalence of LBP decreased from 5.6% (95% uncertainty interval [95% UI]: 4.9%-6.3%) in 1990 to 4.2% (95% UI: 3.8%-4.8%) in 2016. The YLDs for LBP increased from 6.2 million (95% UI: 4.3-8.3 million) in 1990 to 7.7 million (95% UI: 5.4-10.2) in 2016. Age-standardized YLD rate (per 100,000 person) decreased from 637.5 (95% UI: 449.9-848.8) in 1990 to 481.9 (95% UI: 338.6-637.0) in 2016. A female preponderance was observed for prevalence and YLDs. The prevalence and YLDs rate for LBP slightly decreased from 1990 to 2016 in China; however, the total individuals and YLDs increased. Low back pain still ranks as the second leading cause of YLD burden disease in China. Considerable attention should be paid for LBP, especially in the female population.
1. Introduction
Low back pain (LBP) has the highest global burden of disease related to years lived with disability (YLDs) worldwide.12,22,29 Low back pain causes limitations in activity and work capacity, and induces considerable economic and medical burden to individuals, families, and governments, and therefore is a major public health issue.4,5,18,20 Unlike fatal diseases such as cancer or cardiovascular illnesses, LBP is nonfatal and will significantly impact YLDs rather than years of life lost.24
China's population is estimated at 1.396 billion (source: http://countrymeters.info/ct/China). The previous epidemiological studies for LBP were of small sample size, limited localities, and variations.23,44 The data of GBD (Global Burden of Disease Study) 2016 provide an updated and comprehensive assessment of the epidemiological characteristics of the major diseases and how they changed from 1990 to 2016,11–13 as well as the prevalence and YLDs caused by LBP in China.
The hypothesis of this study is that the prevalence and YLDs for LBP is diverse and may vary according to sex, age, and provinces/regions. The policy decision-makers require the information of the current status and trend of prevalence and YLDs for LBP to precisely allocate the scarce health care resources efficiently. Therefore, the aim of this study is to estimate the age-sex-province-specific point prevalence and YLDs characteristics of LBP in China.
2. Methods
All data and analyzes conducted were obtained from the China data in the GBD study 2016 (Global Burden of Diseases, Injuries, and Risk Factors Study 2016). Briefly, the GBD study provides a comprehensive assessment of age-sex-all-cause and cause-specific mortality, and disability for all major diseases and injuries for 195 countries from 1990 to 2016.11,12 This study focuses on the prevalence and YLDs of LBP in China. A total of 33 provinces/regions, including 31 mainland provinces, municipalities, autonomous regions, and the Hong Kong and Macao Special Administrative Regions (SAR), were analyzed.
The systematic reviews of published data, gray literature sources, and survey data were gathered. Bayesian meta-regression method DisMod-MR 2.1 was developed for the GBD 2016 study to address the challenges in estimating the point prevalence and YLDs outcomes. The detailed descriptions of the modeling strategy for point prevalence and YLDs estimation and validation had been previously published.12,22 The steps taken in estimating YLDs of LBP are summarized in supplementary Figure S1 (available at http://links.lww.com/PAIN/A662).
Low back pain is defined as back pain that lasts for at least 1 day (with/without one or both lower limbs), and the definition of the region of “low back” is the posterior area between lower margin of the 12th ribs and the lower gluteal folds.21,22
Disability weights (DWs) were used to represent the magnitude of health loss associated with LBP. Disability weights used in this study refers to the DWs used in the 2016 GBD study,16 measured on a scale from 0 to 1, where 0 equals a state of full health and 1 equals death.32
Eight sequelae were developed to describe the different levels of LBP severity and its associated functional loss as following22:
(1) Severe acute LBP without leg pain;
(2) Severe chronic LBP without leg pain;
(3) Mild acute LBP without leg pain;
(4) Mild chronic LBP without leg pain;
(5) Severe acute LBP with leg pain;
(6) Severe chronic LBP with leg pain;
(7) Mild acute LBP with leg pain; and
(8) Mild chronic LBP with leg pain.
The YLDs were calculated by following formats: (1) YLDtotal = YLDsequela1 + YLDsequela2 + YLDsequela3 + … + YLDsequela8; (2) YLDsequela = Prevsequela eqDWhealth state. Sequelae refers to the above 8 sequelae, Prev is the prevalence number of LBP in each sequela, and DWhealth state refers to the health state reported in the 2016 GBD study.16
The point prevalence was standardized by the constituent ratio of age in China. The uncertainty interval (UI) was calculated from the standard errors generated from the input data, and the uncertainty was calculated from all steps of data manipulations. The 95% UI ranged from 2.5 to 97.5 centile values.16
3. Results
3.1. Prevalence
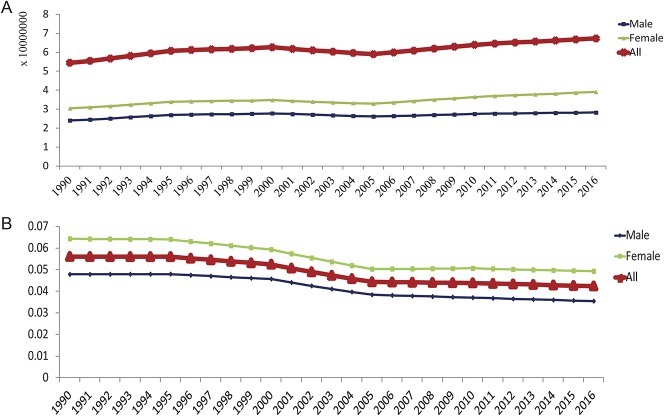
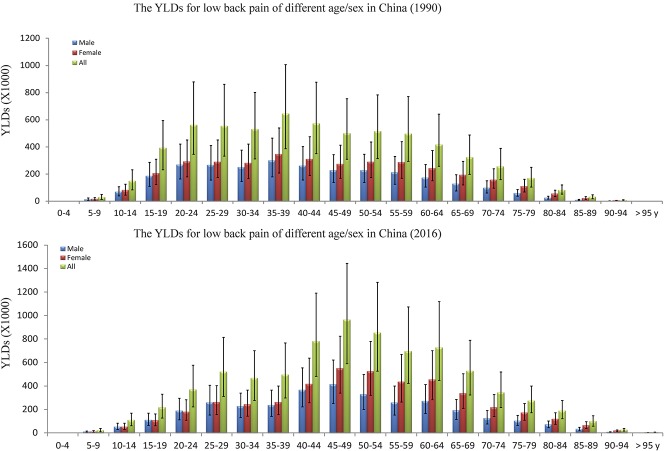
We estimated that 5.45 × 107 individuals had LBP in 1990, rising to 6.73 × 107 in 2016, with an increase of 23.5% (Fig. 1A). The age-standardized point prevalence rate of LBP decreased from 5.6% (95% UI: 4.9%-6.3%) in 1990 to 4.2% (95% UI: 3.8%-4.8%) in 2016. Sex-specific analysis found that the age-standardized point prevalence in females was higher than males. In 1990, the point prevalence was 6.4% (95% UI: 5.6%-7.3%) for females and 4.8% (95% UI: 4.2%-5.4%) for males, which decreased to 4.9% (95% UI: 4.4%-5.6%) for females and 3.5% (95% UI: 3.1%-4.0%) for males in 2016 (Fig. 1B).
Figure 1.
The trends of low back pain in China from 1990 to 2016. (A) 5.45 × 107 individuals had low back pain in 1990, and rising to 6.73 × 107 in 2016. (B) The age-standardized point prevalence of low back pain decreased from 5.6% (95% UI: 4.9%-6.3%) in 1990 to 4.2% (95% UI: 3.8%-4.8%) in 2016. UI, uncertainty interval.
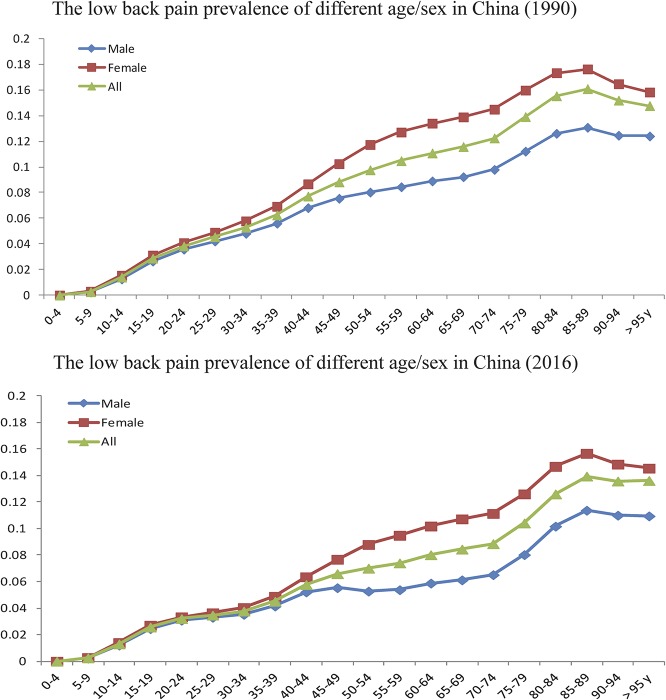
From the age category 0 to 4 years to 85 to 89 years, the point prevalence of LBP increased and peaked in the age category of 85 to 89 years, and then decreased slightly from the age category 85 to 89 years to >95 years (both 1990 and 2016 data) (Fig. 2). The point prevalence in females increased faster than that in males. The sex disparity in point prevalence occurred in the 15 to 19 age category in 1990 and in the 25 to 29 age category in 2016. The disparity in point prevalence between females and males was stable from the age category of 55 to 59 years and up (Fig. 2).
Figure 2.
Age-specific analysis indicates that the point prevalence increased with age in both 1990 and 2016, with a faster rise in females than in males. The point prevalence of both sexes peaked at 85 to 89 years, followed by a slight decrease. The sex disparity in point prevalence appears at 15 to 19 years in 1990, whereas appears at 25 to 29 years in 2016.
In the 33 provinces/regions in China, Beijing had the highest age-standardized point prevalence of LBP, with 6.6% (95% UI: 6.0%-7.2%) in 1990 and 6.2% (95% UI: 5.8%-6.7%) in 2016. Macao had lowest point prevalence of LBP, with 4.8% (95% UI: 4.3%-5.4%) in 1990 and Guangdong with 3.5% (95% UI: 3.1%-4.0%) in 2016. The age-standardized point prevalence in most provinces/regions (29/33) were >5.0% of the point prevalence in 1990 (Fig. 3A), with only slight disparity among different provinces/regions, whereas most of them (32/33) were less than 5.0% in 2016 (Fig. 3B).
Figure 3.
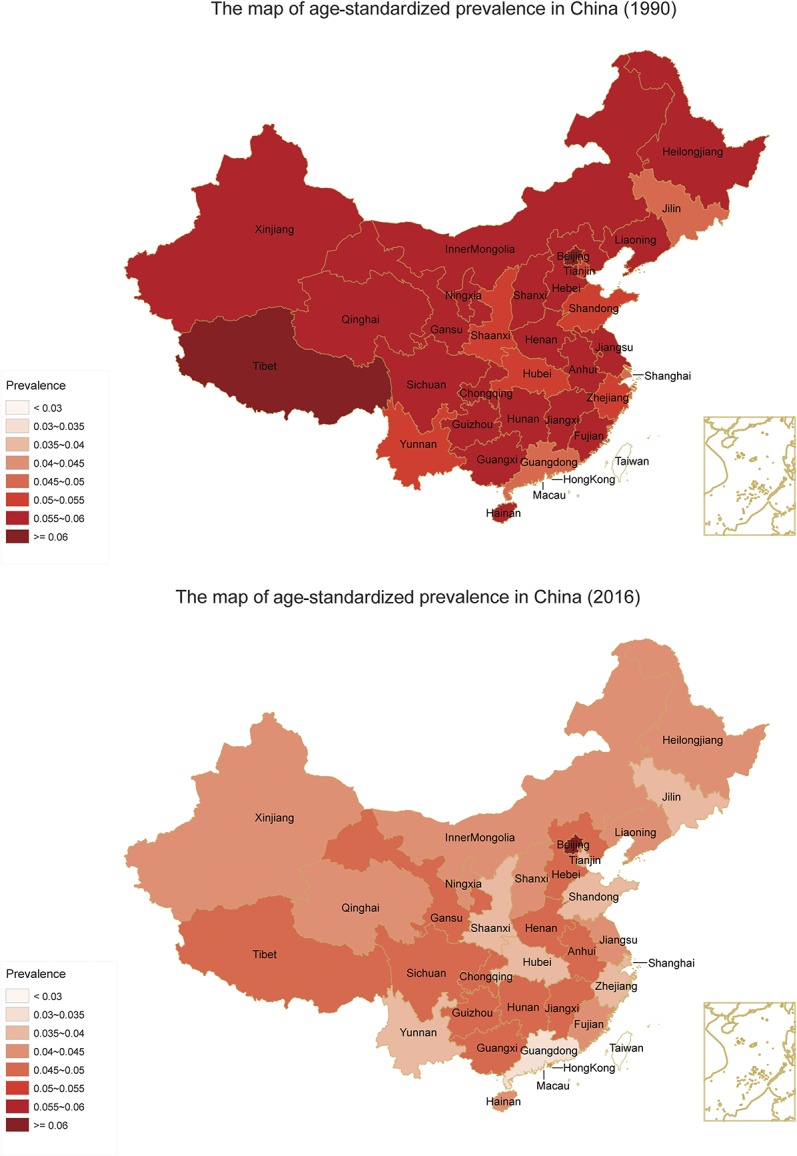
The age-standardized point prevalence of low back pain in 33 provinces/regions in China (without the data of Taiwan). The age-standardized point prevalence in most provinces/regions (29/33) was more than 5.0% in 1990, with only slight disparity, whereas most of them (32/33) were less than 5.0% in 2016.
3.2. Years lived with disability
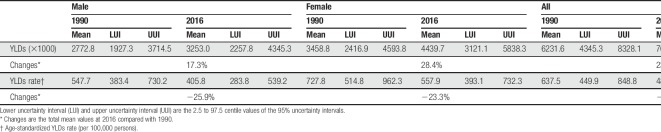
The YLDs for LBP were increased 23.4%, from 6.2 million (95% UI: 4.3-8.3 million) in 1990 to 7.7 million (95% UI: 5.4-10.2) in 2016 (Table 1). Sex-specific analysis also found the YLDs for LBP to be higher in females compared with males (supplementary Table 1, available at http://links.lww.com/PAIN/A662). With increased age, the YLDs increased first, and then decreased; the age category of peaked YLDs was changed from 35 to 39 years in 1990 to 45 to 49 years in 2016 (Fig. 4).
Table 1.
Years lived with disability (YLDs) (×1000) and age-standardized YLDs rate (per 100,000 persons) for low back pain by sex in China (1990 and 2016).
Figure 4.
Age-specific analysis indicates that as the age increases, the years lived with disability (YLDs) is increased first, and then decreased. The peak age category is 35 to 39 years in 1990 and 45 to 49 years in 2016.
Age-standardized YLDs rate (per 100,000 persons) decreased by 24.4%, from 637.5 (95% UI: 449.9-848.8) in 1990 to 481.9 (95% UI: 338.6-637.0) in 2016 (Table 1). Beijing, Hong Kong, and Henan were the 3 highest regions of age-standardized YLDs (rates of 705.2, 540.7, and 535.6/100,000, respectively) in 2016 (supplementary Table 2, available at http://links.lww.com/PAIN/A662).
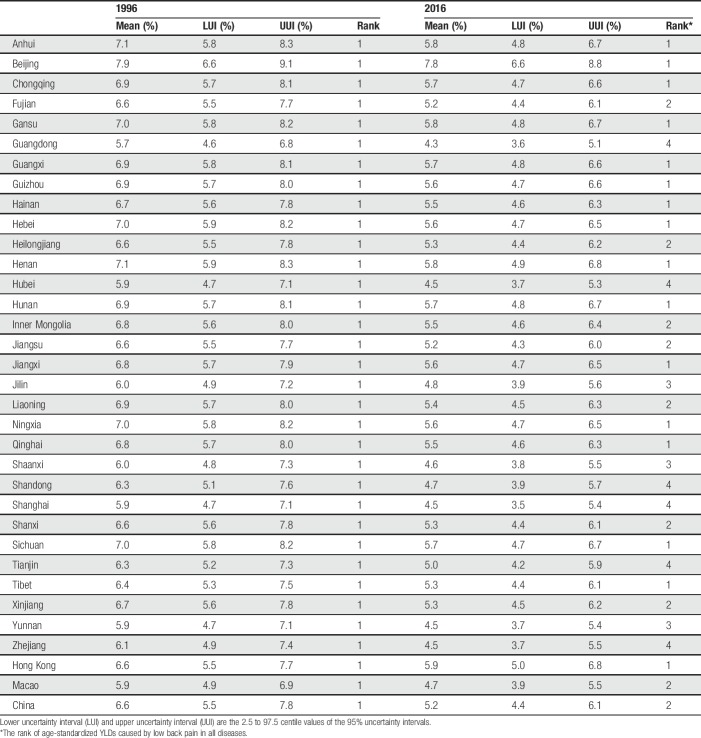
In 1990, the percent of age-standardized YLDs for LBP ranged from 5.7% to 7.9% in different provinces/regions in China, and the LBP ranked as the leading cause of YLDs in all 33 provinces/regions and in the total Chinese population at that time. However, the percent of age-standardized YLDs caused by LBP ranged from 4.3% to 7.8% in different provinces/regions and LBP ranked as the leading cause of YLDs in 16/33 provinces/regions in 2016, as the second leading cause in 8/33, as the third leading cause in 3/33, and as the fourth leading cause in 6/33 (Table 2). Therefore, LBP was the second leading cause of YLDs in the total Chinese population in 2016 (Table 2).
Table 2.
The percent of age-standardized years lived with disability (YLDs) caused by low back pain in all diseases by provinces/regions (1990 and 2016).
4. Discussion
4.1. Characteristics of point prevalence
Many countries reported the prevalence and burden of LBP,2,6,34,37 to provide information for policy-making with regards to prevention and treatment.9 In China, only some provinces and regions reported their regional prevalence or burden of LBP.23,44 Our present study is the first systematic analysis of the point prevalence and YLDs for LBP in China from 1990 to 2016.
In 2016, the age-standardized point prevalence of LBP in China was 4.2% (95% UI: 3.8%-4.8%), which is lower than the global point prevalence of 7.0% (95% UI: 6.5%-8.1%)12,15 and similar to the China 2015 prevalence of 4.3% (95% UI: 3.8%-4.8%.10 Although the number of LBP individuals increased from 1990 to 2016, the overall point prevalence has decreased; this may contribute by the parallel with an increased total population size in China, and lifestyle changes in past decades. From the Fig. 2B, we can find that the point prevalence had significantly decreased from 2000 to 2010, Chinese population had increased income and take more care about health at that time, and the young people prefer some light labor occupations.
Beijing had the highest age-standardized point prevalence of LBP, 6.6% in 1990 and 6.2% in 2016. Tian et al.35 reported that sleeping less than 7 hours per day and “hardworking” may be the risk factors for lumbar disk disease, which may contribute to lower back pain. Beijing is a city with lights turned on all night, and with great work pressure; all these factors may keep Beijing to be the highest age-standardized point prevalence of LBP in China.
The age-standardized point prevalence of LBP in females was higher than that in males in 2016, which is consistent with many previous studies.1,27,41,42 The exact contributors for this phenomenon remain poorly understand.1 Generally, females are affected by more painful conditions of musculoskeletal system than males.25 The potential explanations of sex differences include psychological, biological, and sociocultural factors.36,41 Psychological factors of the higher sensitivity to pain among women and perceived greater willingness to report the painful symptoms may partly explain it.31,43 Biological factors of menstrual cycle fluctuations and hormonal mechanisms may also help us to explain the sex differences.30 In addition, hormonal differences and weight changes due to menopause38 and pregnancy14may also affect the musculoskeletal and neurological systems and result in LBP.
Moreover, we found the sex disparity in point prevalence to appear in the 15 to 19 age category in 1990, but delayed to the 25 to 29 age category in 2016. Previous studies reported that LBP was the most common cause of work-related disability in younger populations;1,7 therefore, may be most female participants work after primary high school in 1990, but work after college in 2016 with the improved education level, thereby delaying the onset of back pain.
For the age group more than 55 to 59 years, the sex disparity of LBP is stable, and menopause may contribute to the higher point prevalence of LBP in females42 after 50 to 55 years. It was reported that the menopause occurs at a median age of 51.3 years among the population;17 therefore, we conducted an additional stratified prevalence analysis of age group of “15 to 49” and “50 to 69” years for female population, and we found that point prevalence of “50 to 69” age group was 12.8% in 1990 and 9.7% in 2016, significantly higher than that of the “15 to 49” age group of 5.5% in 1990 and 4.8% in 2016. Lou et al.26 reported that estrogen decrease after menopause was associated with the lumbar disk degeneration, which was considered to cause the LBP; consistent results of severe intervertebral disk degeneration among postmenopausal females were found by Wang et al.39,40
4.2. Characteristics of years lived with disability
We use the YLDs to quantify the burden of LBP in this study, because there is no mortality from LBP, and years of life lost = 0. Therefore, YLDs is the same indicator to the DALYs (disability-adjusted life years), which was used by Hoy et al.22
Although the age-standardized point prevalence rate of LBP decreased from 5.6% in 1990 to 4.2% in 2016, from 1990 to 2016, the increased population size and longer life expectancy in China (the longer life expectancy in China is 69.2 years for females and 65.0 years for males, improved to 79.9 years for females and 73.4 years for males)11 contributed to the growth of YLDs. In result of above 3 mainly factors of population growth, ageing and LBP prevalence trends, the YLDs for LBP were increased 23.4%, from 6.2 million (95% UI: 4.3-8.3 million) in 1990 to 7.7 million (95% UI: 5.4-10.2) in 2016.
We also found the age category of peaked YLDs was 35 to 39 years in 1990, to delay to 45 to 49 years in 2016. One reason may be due to the longer life expectancy in 2016 than that in 1990 too (improved 10.5 years for females and 8.4 years for males).11 Another reason may be the increased number of aged population due to the baby boomers in 1960s to 1970s.19
The age-standardized YLDs rate (per 100,000 persons) was 481.9 (95% UI: 338.6-637.0) in 2016, which was lower than 788.9 (95% UI: 558.7-1034.6) as reported worldwide.12,15 Similarly, the point prevalence and age-standardized YLDs rates in 2016 decreased compared with the data from 1990 because of the larger proportional population increase than total YLDs.
The highest age-standardized YLDs rate of Beijing, Hong Kong, and Henan are 705.2, 540.7, and 535.6/100,000, respectively, in 2016, decreased from 747.9, 606.8, and 681.9/100,000, respectively, in 1990, and had decreased 5.7%, 10.9%, and 21.5%, respectively (supplementary Table 2, available at http://links.lww.com/PAIN/A662), whereas the mean decreased age-standardized YLDs rate of total China population is 24.4%. Therefore, the less decreased Beijing and Hong Kong ranked as the first and second. Henan had high basic age-standardized YLDs rate of 681.9/100,000 in 1990 and decreased 21.5%; although still ranked as the third, the value of 535.6/100,000 is very close to the top 10 provinces/regions in China (supplementary Table 2, available at http://links.lww.com/PAIN/A662).
In 1990, LBP was the first leading cause of YLDs in China, which dropped to being the second leading cause in 2016. Before this study, most hypothesized that the point prevalence and YLDs rate should continue to increase,3,22 and hence stay as the first leading cause of YLDs. However, with a greater decline in the point prevalence and YLDs, LBP became the second leading cause of YLDs in 2016. In some provinces/regions (such as Guangdong, Hubei, Shandong, Shanghai, Tianjin, and Zhejiang), LBP was even ranked as the fourth leading cause of YLDs, whereas the neck pain–caused YLDs ranked as the No.1 in above provinces/regions in 2016. Furthermore, to analyze the reasons of decreased rank of LBP-caused YLDs, we found that the prevalence of LBP in the above-mentioned provinces/regions was significantly decreased, but the point prevalence of neck pain was stable from 1990 to 2016; therefore, our data suggest that the reason of the decreased rank of LBP-caused YLDs in above-mentioned provinces/regions is the decreased prevalence of LBP, but not the increased prevalence of other diseases. Although, the reason of the decreased YLDs caused by LBP is unclear, the improvement of primary medical care and increased outdoor physical exercises in China may partly explain it.
4.3. Relevant to preventive policy
Although the point prevalence of LBP slightly decreased from 1990 to 2016, the 2016 Chinese data from the global burden study also shows that LBP is ranked as the second leading cause of YLDs burden. Therefore, governments and health care service providers should still pay considerable attention to LBP.3
Beijing reports the highest YLDs for LBP. Perhaps the experience of Guangdong, Hubei, Shandong, Shanghai, Tianjin, and Zhejiang may be helpful for Beijing to use for decreasing the point prevalence and YLDs of LBP. Having adequate rest time, less work pressure, exercises, and reducing occupational sitting time may prevent LBP.8,28,33 These are all primary care interventions that can be initiated through policy-makers. Moreover, the scarce health care resources may be allocated to the 40 to 50 age group, which reported higher YLDs for LBP, and the elderly and female population who had higher prevalence of LBP.
4.4. Strengths and limitations
In the 2016 GBD study, there were many variations in recalling period, anatomical location, and minimum duration of episodes. Such as multiple pain sites may overstated the YLDs. To ensure that the quantified LBP is more accurate than previous GBD studies, the LBP with or without activity limitations is adjusted in the 2016 GBD study (For all the data from 1990 to 2016); YLDs in this study was focused mainly caused by LBP, and use 8 sequelae to calculate the YLDs to minimize the deviation. Disability weight is another uncertainty for YLDs estimates as it is based on the selected survey, and without new data conducted since the 2013 GBD study;12,22 however, 8 DWs of health state were used in our study to minimize the deviation. Therefore, the uncertainty of DW is acceptable.
5. Conclusion
The point prevalence and YLDs rate for LBP slightly decreased from 1990 to 2016 in China. However, the total number of sufferers and YLDs remains increased. Low back pain still ranks as the second leading cause of YLDs burden in China. Considerable attention to LBP is needed, especially for the female population.
Conflict of interest statement
The authors have no conflict of interest to declare.
Supplementary Material
Acknowledgments
Author contributions: Conception and design: A. Wu, W. Dong, M. Zhou, and J. Zhao. Analysis and interpretation of data: A. Wu, W. Dong, S. Liu, X. Zeng, K. Zhang, Z. Sun, and X. Wang. Drafting the article: A. Wu, W. Dong, J.P.Y. Cheung, and K.Y.H. Kwan. Revising article critically for important intellectual content: All authors. Final approval of the version to be published: All authors.
This work was supported by the China Postdoctoral Science Foundation (2018M630450) and National Natural Science Foundation of China (81501933).
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/A662.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
A. Wu and W. Dong contributed equally to this study and are the co-first authors. J. Zhao and M. Zhou contributed equally to this study and are the co-correspondence authors.
References
- [1].Bailey A. Risk factors for low back pain in women: still more questions to be answered. Menopause 2009;16:3–4. [DOI] [PubMed] [Google Scholar]
- [2].Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287. [DOI] [PubMed] [Google Scholar]
- [3].Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, Croft P, Lancet Low Back Pain Series Working Group. Low back pain: a call for action. Lancet 2018;391:2384–8. [DOI] [PubMed] [Google Scholar]
- [4].Chen Y, Campbell P, Strauss VY, Foster NE, Jordan KP, Dunn KM. Trajectories and predictors of the long-term course of low back pain: cohort study with 5-year follow-up. PAIN 2017;159:252–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Deyo RA, Cherkin D, Conrad D, Volinn E. Cost, controversy, crisis: low back pain and the health of the public. Annu Rev Public Health 1991;12:141–56. [DOI] [PubMed] [Google Scholar]
- [6].Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from US national surveys, 2002. Spine (Phila Pa 1976) 2006;31:2724–7. [DOI] [PubMed] [Google Scholar]
- [7].Driscoll T, Jacklyn G, Orchard J, Passmore E, Vos T, Freedman G, Lim S, Punnett L. The global burden of occupationally related low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:975–81. [DOI] [PubMed] [Google Scholar]
- [8].Evans R, Haas M, Schulz C, Leininger B, Hanson L, Bronfort G. Spinal manipulation and exercise for low back pain in adolescents: a randomized trial. PAIN 2018;159:1297–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018;391:2368–83. [DOI] [PubMed] [Google Scholar]
- [10].GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1545–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1260–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1345–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gibson L. Pregnancy related low back pain. Int J Childbirth Education 2017;32:27–9. [Google Scholar]
- [15].Global Burden of Disease Collaborative Network. GBD Results tool: Use the following to cite data included in this download: Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Seattle: Institute for Health Metrics and Evaluation (IHME), 2017. Available at: http://ghdx.healthdata.org/gbd-results-tool. Accessed March 20, 2018. [Google Scholar]
- [16].Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Population Estimates 1950–2016. Seattle: Institute for Health Metrics and Evaluation (IHME), 2017. [Google Scholar]
- [17].Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, Epling JW, Jr, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phipps MG, Silverstein M, Simon MA, Tseng CW. Hormone therapy for the primary prevention of chronic conditions in postmenopausal women: US preventive services task force recommendation statement. JAMA 2017;318:2224–33. [DOI] [PubMed] [Google Scholar]
- [18].Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J. What low back pain is and why we need to pay attention. Lancet 2018;391:2356–67. [DOI] [PubMed] [Google Scholar]
- [19].Heise L. China's baby boomers. World Watch 1988;1:10–11. [PubMed] [Google Scholar]
- [20].Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol 2010;24:769–81. [DOI] [PubMed] [Google Scholar]
- [21].Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, Buchbinder R. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol 2010;24:155–65. [DOI] [PubMed] [Google Scholar]
- [22].Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968–74. [DOI] [PubMed] [Google Scholar]
- [23].Lau E, Egger P, Coggon D, Cooper C, Valenti L, O'Connell D. Low back pain in Hong Kong: prevalence and characteristics compared with Britain. J Epidemiol Community Health 1995;49:492–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Lee H, Hubscher M, Moseley GL, Kamper SJ, Traeger AC, Mansell G, McAuley JH. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. PAIN 2015;156:988–97. [DOI] [PubMed] [Google Scholar]
- [25].Leveille SG, Zhang Y, McMullen W, Kelly-Hayes M, Felson DT. Sex differences in musculoskeletal pain in older adults. PAIN 2005;116:332–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lou C, Chen HL, Feng XZ, Xiang GH, Zhu SP, Tian NF, Jin YL, Fang MQ, Wang C, Xu HZ. Menopause is associated with lumbar disc degeneration: a review of 4230 intervertebral discs. Climacteric 2014;17:700–4. [DOI] [PubMed] [Google Scholar]
- [27].Nagi SZ, Riley LE, Newby LG. A social epidemiology of back pain in a general population. J Chronic Dis 1973;26:769–79. [Google Scholar]
- [28].Pronk NP, Katz AS, Lowry M, Payfer JR. Peer reviewed: reducing occupational sitting time and improving worker health: the take-a-stand project, 2011. Prev Chronic Dis 2012;9:E154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Rice AS, Smith BH, Blyth FM. Pain and the global burden of disease. PAIN 2016;157:791–6. [DOI] [PubMed] [Google Scholar]
- [30].Riley JL, III, Robinson ME, Wise EA, Price DD. A meta-analytic review of pain perception across the menstrual cycle. PAIN 1999;81:225–35. [DOI] [PubMed] [Google Scholar]
- [31].Rollman GB, Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain 2001;17:20–4. [DOI] [PubMed] [Google Scholar]
- [32].Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar M, Speybroeck N. Disability weights for the global burden of disease 2013 study. Lancet Glob Health 2015;3:e712–e723. [DOI] [PubMed] [Google Scholar]
- [33].Steffens D, Maher CG, Pereira LS, Stevens ML, Oliveira VC, Chapple M, Teixeira-Salmela LF, Hancock MJ. Prevention of low back pain: a systematic review and meta-analysis. JAMA Intern Med 2016;176:199–208. [DOI] [PubMed] [Google Scholar]
- [34].Taimela S, Kujala UM, Salminen JJ, Viljanen T. The prevalence of low back pain among children and adolescents: a nationwide, cohort‐based questionnaire survey in Finland. Spine (Phila Pa 1976) 1997;22:1132–6. [DOI] [PubMed] [Google Scholar]
- [35].Tian W, Lv Y, Liu Y, Xiao B, Han X. The high prevalence of symptomatic degenerative lumbar osteoarthritis in Chinese adults: a population-based study. Spine (Phila Pa 1976) 2014;39:1301–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol 2002;70:678–90. [DOI] [PubMed] [Google Scholar]
- [37].Walker BF, Muller R, Grant WD. Low back pain in Australian adults. Prevalence and associated disability. J Manipulative Physiol Ther 2004;27:238–44. [DOI] [PubMed] [Google Scholar]
- [38].Wang YXJ, Griffith JF. Effect of menopause on lumbar disk degeneration: potential etiology. Radiology 2010;257:318–20. [DOI] [PubMed] [Google Scholar]
- [39].Wang YX, Griffith J, Ma H, Kwok A, Leung J, Yeung D, Ahuja A, Leung P. Relationship between gender, bone mineral density, and disc degeneration in the lumbar spine: a study in elderly subjects using an eight-level MRI-based disc degeneration grading system. Osteoporos Int 2011;22:91–6. [DOI] [PubMed] [Google Scholar]
- [40].Wang YXJ, Griffith JF, Zeng XJ, Deng M, Kwok AW, Leung J, Ahuja AT, Kwok T, Leung PC. Prevalence and sex difference of lumbar disc space narrowing in elderly Chinese men and women: osteoporotic fractures in men (Hong Kong) and osteoporotic fractures in women (Hong Kong) studies. Arthritis Rheumatol 2013;65:1004–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Wáng YXJ, Wáng JQ, Káplár Z. Increased low back pain prevalence in females than in males after menopause age: evidences based on synthetic literature review. Quant Imaging Med Surg 2016;6:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Wang YXJ. Menopause as a potential cause for higher prevalence of low back pain in women than in age-matched men. J Orthop Translat 2017;8:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Wolfe F, Ross K, Anderson J, Russell I. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol 1995;22:151–6. [PubMed] [Google Scholar]
- [44].Zeng QY, Chen R, Xiao ZY, Huang S-B, Liu Y, Xu JC, Le Chen S, Darmawan J, Couchman KG, Wigley RD. Low prevalence of knee and back pain in southeast China; the Shantou COPCORD study. J Rheumatol 2004;31:2439–43. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.