Abstract
The increasing use of personal listening devices (PLDs) has been accompanied by a rise in the prevalence of hearing loss (HL) in younger age groups. However, there have been few reports on the relationship between HL and leisure noise exposure (LNE) in adolescents. The purpose of our study was to investigate the prevalence of HL in students attending general middle and high schools and to identify factors affecting HL prevalence. A total of 2,879 nationally representative adolescents in the first years of middle and high school underwent audiometric testing and otological examinations, and completed questionnaires, from June to December 2016. A speech-frequency hearing loss (SFHL) was considered present when the pure tone averages (PTAs) at 0.5, 1, and 2 kHz were ≥ 15 dB and a high-frequency hearing loss (HFHL) was considered present when the PTAs at 3, 4, 6, and 8 kHz were ≥ 15 dB. About 17% of Korean adolescents exhibited at least slight HL. The prevalence rates of SFHL and HFHL in the poorer ear were 11.6% and 10.3%, respectively, among Korean adolescents. The use of local area network (LAN) gaming centers and an experience of being asked by others to lower earphone volume were associated with both SFHL and HFHL. It is important to avoid excessive LNE to prevent adolescent HL. Additionally, SFHL or HFHL in the poorer ear was associated with lower academic performance.
Introduction
Noise-induced hearing loss is a hearing impairment caused by exposure to loud sounds, and initially affects the high-frequency hearing threshold. Previously, noise-induced hearing loss that was attributable to occupational noise exposure was of major concern, and hearing loss (HL) caused by leisure noise exposure (LNE) was considered to be relatively unimportant [1, 2]. Although occupational HL is high in developing countries, the prevalence thereof is lower in developed countries because of governmental regulations, the use of personal protective equipment, and early HL detection via periodic screening [1, 3]. However, LNE is steadily increasing, attributable to major rises in smartphone use and participation in noisy leisure activities, such as listening to music through personal music systems and attending rock concerts or public nightclubs [3–6]. Noise exposure from repetitive leisure activities, which many young people are willing to accept, can increase the auditory threshold, particularly in this population [7–10].
A study from the USA reported that the prevalence of HL among US adolescents increased from 14.9% in 1988–1994 to 19.5% in 2005–2006. Although no significant relationship between noise exposure and HL was found, an influence of noise may be inferred by the reported increase in high-frequency hearing loss (HFHL) [11]. Another study did not find an increase in HL among US adolescents during these periods, but found an increase in the prevalence of noise-induced threshold shifts in female adolescents. Female participants used less hearing protection devices than males and the authors inferred that this may have some association with the increased prevalence of noise-induced threshold shifts [12]. Hong et al. also reported unilateral and bilateral HFHLs > 20 dB in 5.0% and 1.9%, respectively, of 1,658 adolescents aged 13–18 years in South Korea. They categorized the sources of noise as occupational, non- occupational, and momentary, and aimed to investigate how they affected HL. Although they did not detect a direct association between HL and any particular sort of noise, the use of earphones in noisy places was significantly associated with bilateral HFHL [13].
Thus, it has not yet been determined whether noise exposure affects adolescent HL. LNE is difficult to quantify and HL attributable to LNE varies from a temporary threshold shift to permanent HL. However, if noise exposure affects adolescent HL, early detection of HL and avoidance of additional noise exposure may be the most important factors to prevent further exacerbation.
In this study, we investigated the prevalence of HL and the associations between HL and noise-related factors, including specific types of LNE that adolescents are typically exposed to, as well as self-rated academic achievement in adolescents in South Korea.
Materials and methods
Study design and subjects
We performed a cross-sectional, complex sampling survey of first-year middle and high school students, except those attending special schools for disabled children. The sampling frame was the 2015 yearbook of educational statistics prepared by the Korean Educational Statistics Services [14].
We sought to enroll a total of 3,100 students from 124 middle schools and 124 high schools, based on the prevalence of HL in Korean adolescents, the estimated association between noise and HL, and an expected 80% response rate [15, 16]. The sample size required to analyze the association between LNE and HL was calculated using G*Power software, considering the sample size in a previous study, a statistical power of 0.80, and a two-tailed α-value of 0.05 [17]. We obtained a list of all Korean middle schools (n = 3,204), and another of all high schools (n = 2,383), and classified the schools for random sampling to ensure proportional representation of all regions of Korea (eight metropolitan and eight suburban or rural regions) and all types of schools (single-gender, coeducational, general, and vocational). Sample schools were systematically selected in each region from the lists of middle and high schools, in alphabetical order, followed by random selection of sample classes after ensuring that all classes were educationally similar. We targeted 248 of the 5,587 middle and high schools in Korea, expecting a 50% school response rate based on a pilot study, and that each class would have 25 students. Finally, sampling weight was calculated as the inverse selection probability for each stratum and each school. The final sampling weight was obtained after adjustment for non-response.
The survey was performed from June to November 2016. After distributing written information to students and parents, we evaluated only those who provided written informed consent of themselves and their parents. This study was approved by the Institutional Review Board of Seoul National University Hospital (No. 1604-086-755).
Data collection and measurements
Questionnaire
Students and parents were asked to complete separate questionnaires. Both questionnaires were based on Forms 1–2 and 1–3 of the Enforcement Rule for Health Screening at School of the School Health Act of South Korea, and those of the Korea Nutrition and Health Examination Survey (a nationally representative South Korean survey assessing the health and nutritional status of the entire population [18]).
The student questionnaire explored gender, age, any history of a disorder of the ear, nose, or throat, subjective hearing status, and any tinnitus. Participants answered “yes”, “no”, or “I don’t know” to the following question about tinnitus: “Have you ever experienced tinnitus, such as beeping, ringing, or buzzing, in the past year?” Questions pertaining to personal listening devices (PLDs) concerned usage of a PLD (“Do you use a personal listening device such as a smartphone, MP3 player, or personal media player?”), usage period (“How old were you when you started using a PLD?”), requests to turn down the volume (“Have you ever been asked to turn down the volume on your PLD?”), and the subjective volume intensity (10-point Likert scale), based on a previous study by Cone et al. [15]. In terms of LNE, we asked how often the subject visited local area network (LAN) gaming centers, karaoke rooms, and concert halls. We explored drinking and smoking histories. We asked the subject to self-rate his/her academic performance to allow us to explore the association between school performance and hearing. Academic performance was reported using a five-point Likert scale (Excellent, Good, Normal, Bad, or Poor). Participants who responded “Normal”, “Bad”, or “Poor” were considered to exhibit lower academic performance. The parental questionnaires explored the student’s perinatal history, any visit to an intensive care unit, any family history of HL, and the residential noise level.
Audiological evaluation
Pure tone audiometry was conducted using an AD229b diagnostic audiometer (Interacoustics, Assen, Denmark) in soundproof booths inside a mobile vehicle by four experienced audiologists. Prior to audiometry, otological examinations were performed by trained, experienced otolaryngology residents using otoscopes. Factors affecting hearing, such as external ear anomalies, ear wax, retraction of the tympanic membrane, cholesteatoma, and middle ear effusion were recorded; modifiable factors (cerumen or foreign bodies in the external auditory canal) were managed prior to the hearing tests.
The tested frequencies ranged from 0.5 to 8 kHz, i.e., 0.5, 1, 2, 3, 4, 6, and 8 kHz. Testing began at 1 kHz, followed by 2, 4, 8, 1, 0.5, and 0.25 kHz. The participants started the test by listening to a 30 dB tone; the test tone was reduced by 10 dB or increased by 5 dB according to the presence or absence of a response. The hearing threshold was defined as the lowest intensity level (in dB) at which the participant responded to 50% of the stimuli. When the hearing threshold was ≥ 25 dB at any frequency (0.5–8 kHz), the bone conduction threshold to distinguish between sensorineural and conductive HL was determined. The severity of HL was based on the poorer threshold for unilateral HL and the better threshold for bilateral HL, as described previously [11]. We defined “slight HL” as a hearing threshold ≥ 15 dB and “worse HL” as a hearing threshold ≥ 25 dB, thus, including mild HL. The speech-frequency hearing loss (SFHL) was the average of the HLs at 0.5, 1, and 2 kHz, while the HFHL was the average of the HLs at 3, 4, 6, and 8 kHz.
Statistical analyses
First, we calculated the unweighted frequencies and weighted prevalence rates of SFHL and HFHL; this was deemed appropriate given the multi-stage, complex sampling design. Second, we used a multivariate logistic regression model to calculate odds ratios (ORs) for the associations between HL and various factors. The model included demographic characteristics (educational level, gender, and monthly household income); known risk factors (cigarette smoking, alcohol consumption, a history of sinusitis, the use of sinusitis medication, a history of otitis media, and the use of otitis media medication); tinnitus status (“yes”, “no”, or “I don’t know”); and associations between HL and noise sources (PLD use, duration of such use, PLD volume, requests from others to turn down the volume, exposure to leisure noise over the past year). To estimate the association between leisure time noise exposure and HL with consideration of known risk factors, noise sources were not included as model covariates. We adjusted for potential confounders (known risk factors for HL) including age, gender, household income, smoking status, alcohol consumption, any history of ear infection or rhinosinusitis, and any family history of HL [11]. Third, we analyzed the dose-response associations between HL and use of LAN gaming centers, a major source of LNE in Korea. We multiplied visits per month by hours per visit by years since first visit; this was the cumulative LNE imparted by the gaming centers. We divided all subjects into three groups in terms of LAN gaming center use: never-user, light user (lower 50%), and heavy user (upper 50%). We employed multivariate logistic regression to explore the association between LAN gaming center exposure and HL, adjusted for age, gender, household income, smoking status, alcohol use, any history of ear infection or rhinosinusitis, and any family history of HL. Finally, we performed a multivariate logistic regression to investigate the associations between lower academic performance and hearing status after adjusting for education level, gender, and household income. All statistical analyses were performed with the aid of SAS SURVEYMEANS, SAS SURVEYFREQ, or SAS SURVEYLOGISTIC (ver. 9.3; SAS Institute, Cary, NC) to allow for the complex survey design and to consider the sampling weights. Statistical significance was defined as a two-sided p-value < 0.05.
Results
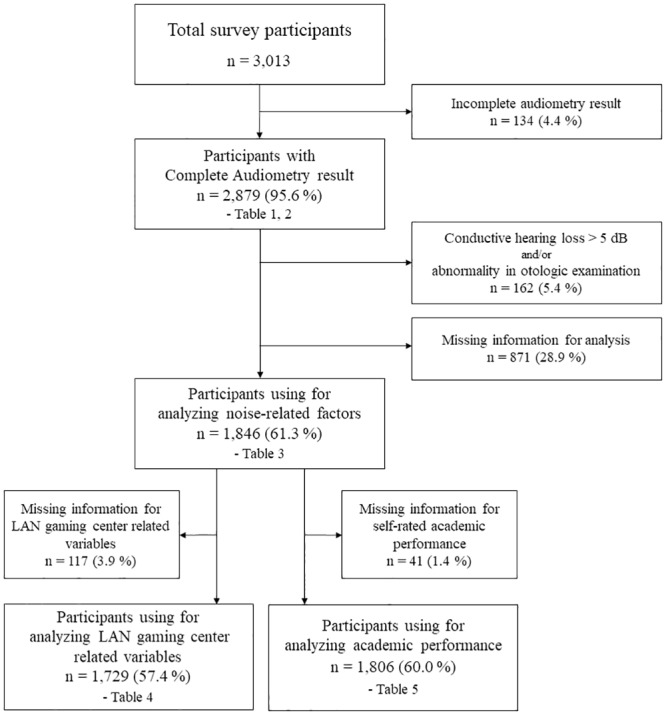
Overall, 109 of the 248 schools contacted agreed to participate in the survey, with 3,013 students agreeing to complete the questionnaires. Of the 3,013 participants, 134 were excluded because of incomplete data. A total of 2,879 students underwent audiological and otological examinations (95.6%). The demographic characteristics of these 2,879 participants are summarized in Table 1. We excluded those with conductive HL > 5 dB and/or any otological abnormality (middle ear effusion, cholesteatoma, and/or excessive cerumen). Age, gender, smoking habits, alcohol intake, socioeconomic status, and noise-related behaviors did not differ significantly between participants who were included and excluded. After excluding those for whom essential data were missing, 1,846 students were assessed for factors related to HL; 1,803 students were included to analyze factors related to tinnitus; 1,729 students were subjected to analysis regarding LAN gaming center-related variables; and 1,806 students were subjected to an academic performance analysis (Fig 1).
Table 1. Demographic characteristics of study participants by school level.
| Total§ | Middle school, Grade 7 | High school, Grade 7 | |||
|---|---|---|---|---|---|
| Male§ | Female§ | Male§ | Female§ | ||
| Total | 2,879 (100.0) | 852 (100.0) | 720 (100.0) | 659 (100.0) | 648 (100.0) |
| Household income per month, $US | |||||
| < 2,000 | 77 (2.3) | 22 (2.7) | 17 (2.8) | 22 (1.4) | 16 (2.1) |
| 2,000–3,000 | 323 (9.8) | 77 (7.4) | 79 (10.1) | 80 (10.1) | 87 (12.2) |
| 3,000–4,000 | 1,133 (39.2) | 338 (35.9) | 293 (40.9) | 236 (39.9) | 266 (40.6) |
| ≥ 4,000 | 962 (35.9) | 309 (38.9) | 259 (36.9) | 195 (33.7) | 199 (33.8) |
| Missing | 384 (12.8) | 106 (15.1) | 72 (9.4) | 126 (15.0) | 80 (11.3) |
| Cigarette smoking status | |||||
| Never | 2,534 (89.0) | 754 (91.5) | 677 (95.1) | 493 (76.0) | 610 (94.1) |
| Ever | 323 (10.8) | 82 (7.9) | 37 (4.6) | 166 (24.0) | 38 (5.9) |
| Missing | 22 (0.2) | 16 (0.6) | 6 (0.2) | 0 (0) | 0 (0) |
| Alcohol use | |||||
| Never | 2,310 (81.0) | 756 (89.3) | 665 (93.6) | 420 (64.6) | 469 (75.4) |
| Ever | 543 (18.8) | 77 (10.0) | 48 (6.1) | 239 (35.4) | 179 (24.6) |
| Missing | 26 (0.3) | 19 (0.7) | 7 (0.3) | 0 (0) | 0 (0) |
| History of sinusitis | |||||
| Yes | 265 (9.3) | 63 (9.1) | 49 (5.9) | 85 (12.2) | 68 (10.3) |
| No | 2,358 (81.5) | 687 (78.5) | 616 (87.8) | 518 (78.5) | 537 (81.2) |
| Missing | 256 (9.2) | 102 (12.4) | 55 (6.4) | 56 (9.3) | 43 (8.4) |
| Took medication for sinusitis in past 2 weeks | |||||
| Yes | 41 (1.5) | 13 (2.0) | 9 (0.9) | 11 (2.4) | 8 (0.8) |
| No | 2,299 (80.2) | 667 (78.0) | 593 (84.9) | 525 (80.7) | 514 (76.7) |
| Missing | 539 (18.3) | 172 (20.0) | 118 (14.2) | 123 (16.9) | 126 (22.5) |
| History of ear infection | |||||
| Yes | 295 (9.8) | 69 (7.5) | 78 (10.3) | 67 (8.8) | 81 (13.4) |
| No | 2,317 (80.4) | 677 (79.0) | 590 (83.9) | 535 (81.5) | 515 (76.7) |
| Missing | 267 (9.8) | 106 (13.5) | 52 (5.8) | 57 (9.7) | 52 (9.9) |
| Took medication for otitis media in past 2 weeks | |||||
| Yes | 21 (0.6) | 9 (0.7) | 7 (1.0) | 2 (0.1) | 3 (0.5) |
| No | 2,307 (80.4) | 667 (77.6) | 597 (85.1) | 531 (82.7) | 512 (75.8) |
| Missing | 551 (19.0) | 176 (21.7) | 116 (13.9) | 126 (17.1) | 133 (23.8) |
| Subjective hearing discomfort | |||||
| None | 2,279 (79.5) | 689 (81.3) | 568 (80.8) | 522 (77.9) | 500 (77.7) |
| Mild-to-moderate | 427 (15.2) | 94 (11.8) | 105 (13.8) | 108 (18.0) | 120 (17.5) |
| Severe | 11 (0.4) | 1 (0.1) | 1 (0.1) | 5 (0.6) | 4 (0.7) |
| Profound | |||||
| Missing | 162 (4.9) | 68 (6.7) | 46 (5.2) | 24 (3.4) | 24 (4.1) |
| Has hearing aid | |||||
| Yes | 14 (0.2) | 9 (0.6) | 3 (0.2) | 1 (0.02) | 1 (0.1) |
| Yes, but do not use | 4 (0.02) | 1 (0.04) | 1 (0.04) | 1 (0.002) | 1 (0) |
| No | 885 (30.3) | 233 (26.1) | 196 (25.3) | 230 (36.8) | 226 (33.8) |
| Missing | 1,976 (69.4) | 609 (73.3) | 520 (74.5) | 427 (63.2) | 420 (66) |
| Tinnitus | |||||
| Yes | 1,298 (43.9) | 247 (27.0) | 319 (45.0) | 310 (45.0) | 422 (62.6) |
| No | 1,035 (37.5) | 430 (53.8) | 240 (33.9) | 232 (37.3) | 133 (21.5) |
| I don’t know | 416 (14.6) | 116 (13.8) | 126 (17.7) | 90 (13.1) | 84 (13.8) |
| Missing | 130 (4.0) | 59 (5.4) | 35 (3.3) | 27 (4.7) | 9 (2.2) |
| Personal stereo usage | |||||
| Yes | 2,518 (87.1) | 666 (76.8) | 638 (89.2) | 596 (89.7) | 618 (94.3) |
| No | 345 (12.8) | 175 (22.8) | 77 (10.6) | 63 (10.3) | 30 (5.7) |
| Missing | 16 (0.2) | 11 (0.4) | 5 (0.2) | 0 (0) | 0 (0) |
| Type of personal stereo | |||||
| With earphones | 2,330 (80.8) | 575 (67.6) | 596 (83.0) | 553 (83.0) | 606 (92.3) |
| Any other device With headphones |
152 (5.2) | 77 (8.0) | 30 (4.7) | 36 (5.8) | 9 (1.8) |
| Not applicable | 361 (12.9) | 186 (23.2) | 82 (10.8) | 63 (10.3) | 30 (5.7) |
| Missing | 36 (1.0) | 14 (1.2) | 12 (1.5) | 7 (1.0) | 3 (0.2) |
| Usage period | |||||
| Not applicable | 345 (12.8) | 175 (22.8) | 77 (10.6) | 63 (10.3) | 30 (5.7) |
| 0–4 years | 1,379 (48.3) | 499 (57.7) | 421 (58.7) | 269 (41.9) | 190 (31.8) |
| ≥ 4 years | 1,139 (38.8) | 167 (19.1) | 217 (30.5) | 327 (47.8) | 428 (62.5) |
| Missing | 16 (0.2) | 11 (0.4) | 5 (0.2) | 0 (0) | 0 (0) |
| Volume level | |||||
| Not applicable | 345 (12.8) | 175 (22.8) | 77 (10.6) | 63 (10.3) | 30 (5.7) |
| 0–4 | 1,446 (52.2) | 375 (42.3) | 384 (56.3) | 336 (55.9) | 351 (55.5) |
| 5–9 | 1,072 (34.8) | 291 (34.5) | 254 (32.9) | 260 (33.7) | 267 (38.8) |
| Missing | 16 (0.2) | 11 (0.4) | 5 (0.2) | 0 (0) | 0 (0) |
| Request to turn down the volume | |||||
| Ever experienced | 401 (14.0) | 76 (9.4) | 121 (18.3) | 88 (12.5) | 116 (16.8) |
| Never experienced | 2,062 (71.4) | 572 (65.7) | 497 (69.2) | 500 (75.9) | 493 (75.7) |
| Missing | 416 (14.6) | 204 (24.9) | 102 (12.6) | 71 (11.6) | 39 (7.5) |
| Usage of noisy facility in the past year | |||||
| LAN gaming center | 1,701 (59.8) | 568 (66.1) | 224 (31.8) | 576 (88.6) | 333 (50.4) |
| Karaoke room | 2072 (74.7) | 392 (48.5) | 624 (87.7) | 482 (76.9) | 574 (89.7) |
| Concert auditorium | 370 (12.3) | 50 (6.2) | 114 (14.8) | 60 (7.3) | 146 (23.2) |
| Dance club | 8 (0.3) | 1 (0.02) | 1 (0.04) | 4 (1.0) | 2 (0.3) |
§ Unweighted frequencies with weighted percentages.
Fig 1. Flow chart of the selection process.
The prevalence rates of SFHL and HFHL were 11.6% and 10.3%, respectively, in Korean adolescents. In total, 17.2% exhibited either SFHL or HFHL. The prevalence of any HL (PTA of either ear better at high frequencies [3, 4, 6, and 8 kHz] or speech frequencies [0.5, 1, and 2 kHz] ≥ 15 dB) were 17.9% and 16.5% among middle and high school students, respectively. The prevalence rates of any HL at high frequencies were 10.5% among middle school students and 10.2% among high school students. The prevalence rates of any HL at speech frequencies were 12.7% and 10.4% among middle and high school students, respectively. The prevalence of slight HL was 16.0% and that of serious HL was 1.2%. The detailed data are shown in Table 2.
Table 2. Prevalence of hearing loss in Korean adolescents.
| Slight or serious (≥ 15 dB) | Slight (15–24 dB) | Serious (≥ 25 dB) | ||||
|---|---|---|---|---|---|---|
| No. | Prevalence, % (95% CI) | No. | Prevalence, % (95% CI) | No. | Prevalence, % (95% CI) | |
| All participants (n = 2,879) | ||||||
| Any* HL§ | 570 | 17.2 (15.0–19.4) | 527 | 16.0 (14–18) | 43 | 1.2 (0.8–1.6) |
| Any HFHL | 330 | 10.3 (8.8–11.9) | 295 | 9.4 (7.9–10.9) | 35 | 1.0 (0.7–1.2) |
| Any SFHL | 391 | 11.6 (9.5–13.6) | 369 | 10.9 (9.0–12.8) | 22 | 0.7 (0.3–1.0) |
| Bilateral HL§ | 181 | 6.6 (5.4–7.7) | 164 | 5.9 (4.7–7.1) | 17 | 0.7 (0.5–0.9) |
| Bilateral HFHL | 102 | 3.6 (2.8–4.4) | 85 | 2.9 (2.1–3.7) | 17 | 0.7 (0.5–0.9) |
| Bilateral SFHL | 118 | 4.3 (3.1–5.5) | 111 | 4.0 (2.8–5.2) | 7 | 0.3 (0.1–0.5) |
| Middle school, Grade 7 (n = 1,572) | ||||||
| Any* HL§ | 329 | 17.9 (14.4–21.4) | 307 | 16.7 (13.5–19.9) | 22 | 1.2 (0.6–1.7) |
| Any HFHL | 183 | 10.5 (8.6–12.4) | 168 | 9.7 (7.8–11.6) | 15 | 0.8 (0.5–1.2) |
| Any SFHL | 243 | 12.7 (9.5–15.8) | 226 | 11.7 (8.8–14.5) | 17 | 1.0 (0.4–1.5) |
| Bilateral HL§ | 108 | 6.5 (5.3–7.7) | 101 | 6.0 (4.8–7.3) | 7 | 0.4 (0.2–0.7) |
| Bilateral HFHL | 57 | 3.8 (3.1–4.5) | 50 | 3.3 (2.6–4.1) | 7 | 0.4 (0.2–0.7) |
| Bilateral SFHL | 76 | 4.4 (3.2–5.6) | 72 | 4.0 (2.8–5.2) | 4 | 0.3 (0.1–0.6) |
| High school, Grade 10 (n = 1,307) | ||||||
| Any* HL§ | 241 | 16.5 (13.8–19.1) | 15.2 (12.7–17.7) | 21 | 1.3 (0.7–1.9) | |
| Any HFHL | 147 | 10.2 (7.7–12.7) | 127 | 9.0 (6.5–11.6) | 20 | 1.2 (0.7–1.6) |
| Any SFHL | 148 | 10.4 (7.6–13.1) | 143 | 10.0 (7.5–12.5) | 5 | 0.4 (0–0.8) |
| Bilateral HL§ | 73 | 6.7 (4.5–8.8) | 63 | 5.8 (3.5–8.0) | 10 | 0.9 (0.5–1.3) |
| Bilateral HFHL | 45 | 3.4 (1.8–4.9) | 35 | 2.5 (0.9–4.0) | 10 | 0.9 (0.5–1.3) |
| Bilateral SFHL | 42 | 4.2 (2.0–6.5) | 39 | 4.0 (1.8–6.2) | 3 | 0.2 (0–0.6) |
* The PTA in the most affected ear was used to define any HL, and the PTA in the less affected ear used to define bilateral HL. Any HL was considered present if bilateral HL was evident at either high or speech frequencies.
§ Participants exhibiting HL either at high frequencies (3, 4, 6, and 8 kHz) or speech frequencies (0.5, 1, and 2 kHz) were classified into these categories.
HL: hearing loss; CI: confidence interval; PTA: pure tone average; HFHL: high-frequency hearing loss; SFHL: speech-frequency hearing loss.
We constructed multivariate logistic regression models to analyze the associations between HL and related factors (Table 3). All analyses were performed after adjusting for education level, gender, household income, cigarette smoking status, alcohol consumption, a history of sinusitis or otitis media (n = 1,846). Education level was not associated with bilateral HL, bilateral HFHL, or bilateral SFHL. Gender was not associated with any HL or HFHL, but female gender was negatively associated with SFHL (OR, 0.49; 95% CI, 0.29–0.82). Subjects who had ever drunk alcohol were at risk of HFHL (OR, 1.90; 95% CI, 1.10–3.28). A history of rhinosinusitis was associated with SFHL and a history of ear infection was associated with HFHL. A low household income was associated with HL. Those living in households with incomes of < $2,000 per month were 8.5-fold more likely to exhibit HFHL (OR, 8.50; 95% CI, 4.84–14.93). We found no significant difference in the prevalence of HL based on the extent or duration of PLD usage. However, among respondents who had ever been asked to lower their earphone volume, the risk of HFHL was 3.32-fold higher (95% CI, 2.09–5.25). Subjective volume was not associated with HL. Recent use of LAN gaming centers increased HFHL 2.21-fold (95% CI, 1.15–4.23). Those who attended concerts exhibited a lower prevalence of HFHL than those who did not attend concerts (OR, 0.35; 95% CI, 0.16–0.77). Visiting karaoke rooms was not associated with HFHL prevalence.
Table 3. Multivariate logistic regression of potential risk factors for HL in Korean adolescents (n = 1,846).
| No. | Bilateral HL* | Bilateral HFHL* | Bilateral SFHL* | ||||
|---|---|---|---|---|---|---|---|
| n (%) § | OR (95% CI) † | n (%) § | OR (95% CI) | n (%) § | OR (95% CI) | ||
| School level | |||||||
| Middle school, Grade 7 | 1,034 | 66 (5.7) | 1 (Reference) | 31 (3.0) | 1 (Reference) | 46 (3.9) | 1 (Reference) |
| High school, Grade 10 | 812 | 42 (5.0) | 0.83 (0.58–1.20) | 23 (2.4) | 0.74 (0.41–1.33) | 26 (3.5) | 0.80 (0.53–1.22) |
| Gender | |||||||
| Male | 937 | 59 (6.2) | 1 (Reference) | 23 (2.8) | 1 (Reference) | 45 (4.7) | 1 (Reference) |
| Female | 909 | 49 (4.5) | 0.63 (0.42–0.95) | 31 (2.6) | 0.84 (0.51–1.40) | 27 (2.7) | 0.49 (0.29–0.82) |
| Household income per month, $US | |||||||
| < 2,000 | 47 | 5 (15.7) | 5.17 (3.29–8.11) | 3 (14.3) | 8.50 (4.84–14.93) | 3 (12.3) | 7.98 (4.71–13.54) |
| 2,000–3,000 | 241 | 12 (3.6) | 1.05 (0.55–2.01) | 5 (1.3) | 0.58 (0.30–1.10) | 10 (3.3) | 2.22 (1.05–4.68) |
| 3,000–4,000 | 840 | 58 (6.9) | 2.03 (1.24–3.33) | 27 (2.9) | 1.29 (0.68–2.43) | 41 (5.1) | 3.39 (1.84–6.23) |
| ≥ 4,000 | 718 | 33 (3.6) | 1 (Reference) | 19 (2.2) | 1 (Reference) | 18 (1.7) | 1 (Reference) |
| Cigarette smoking | |||||||
| Never | 1,689 | 97 (5.5) | 1 (Reference) | 49 (2.8) | 1 (Reference) | 64 (3.7) | 1 (Reference) |
| Ever | 157 | 11 (4.3) | 0.74 (0.41–1.33) | 5 (1.8) | 0.58 (0.27–1.28) | 8 (3.3) | 0.79 (0.41–1.54) |
| Alcohol consumption | |||||||
| Never | 1,552 | 88 (5.4) | 1 (Reference) | 40 (2.5) | 1 (Reference) | 60 (3.8) | 1 (Reference) |
| Ever | 324 | 20 (5.2) | 0.98 (0.65–1.48) | 14 (3.8) | 1.90 (1.10–3.28) | 12 (3.4) | 0.82 (0.56–1.20) |
| History of sinusitis | |||||||
| Yes | 173 | 11 (6.3) | 0.99 (0.68–1.46) | 5 (4) | 0.98 (0.62–1.56) | 10 (6.2) | 1.68 (1.16–2.44) |
| No | 1,673 | 97 (5.3) | 1 (Reference) | 49 (2.6) | 1 (Reference) | 62 (3.4) | 1 (Reference) |
| Took medication for sinusitis in the past 2 weeks | |||||||
| Yes | 19 | 1 (4.1) | 0.77 (0.47–1.26) | 1 (4.1) | 2.10 (1.09–4.03) | 1 (4.1) | 0.66 (0.39–1.11) |
| No | 1,827 | 107 (5.4) | 1 (Reference) | 53 (2.7) | 1 (Reference) | 71 (3.7) | 1 (Reference) |
| History of ear infection | |||||||
| Yes | 195 | 13 (8.2) | 1.92 (1.14–3.22) | 7 (5.7) | 2.98 (1.53–5.81) | 9 (5.7) | 1.73 (0.99–3.02) |
| No | 1,651 | 95 (5.1) | 1 (Reference) | 47 (2.4) | 1 (Reference) | 63 (3.5) | 1 (Reference) |
| Took medication for otitis media in the past 2 weeks | |||||||
| Yes | 8 | 0 (0) | 0 (0) | 0 (0) | |||
| No | 1838 | 108 (5.4) | 1 (Reference) | 54 (2.7) | 1 (Reference) | 72 (3.7) | 1 (Reference) |
| Tinnitus# | |||||||
| Yes | 968 | 51 (5.4) | 1 (Reference) | 24 (2.8) | 1 (Reference) | 33 (3.4) | 1 (Reference) |
| No | 835 | 53 (5.4) | 1.01 (0.74–1.39) | 29 (2.7) | 0.86 (0.54–1.36) | 36 (4.0) | 1.24 (0.89–1.74) |
| Personal stereo use | |||||||
| No | 190 | 19 (8.0) | 1 (Reference) | 8 (3.6) | 1 (Reference) | 11 (4.4) | 1 (Reference) |
| Yes | 1,656 | 89 (5.1) | 0.67 (0.35–1.26) | 46 (2.6) | 0.68 (0.20–2.38) | 61 (3.6) | 0.96 (0.49–1.91) |
| Usage period | |||||||
| < 4 years | 895 | 47 (4.8) | 1 (Reference) | 23 (2.7) | 1 (Reference) | 34 (3.6) | 1 (Reference) |
| ≥ 4 years | 761 | 42 (5.4) | 1.28 (0.84–1.94) | 23 (2.4) | 0.94 (0.53–1.66) | 27 (3.6) | 1.16 (0.79–1.71) |
| Not applicable | 190 | 19 (8) | 1.65 (0.89–3.05) | 8 (3.6) | 1.43 (0.44–4.64) | 11 (4.4) | 1.10 (0.56–2.15) |
| Volume level | |||||||
| 0–4 | 941 | 42 (4.7) | 1 (Reference) | 20 (2.3) | 1 (Reference) | 30 (3.8) | 1 (Reference) |
| 5–9 | 715 | 47 (5.7) | 1.34 (0.91–1.96) | 26 (3.1) | 1.46 (0.94–2.26) | 31 (3.4) | 0.99 (0.61–1.59) |
| Not applicable | 190 | 19 (8.0) | 1.70 (0.88–3.28) | 8 (3.6) | 1.72 (0.51–5.80) | 11 (4.4) | 1.04 (0.51–2.12) |
| Request to turn down the volume†† | |||||||
| Ever experienced | 270 | 24 (6.7) | 1.67 (1.12–2.48) | 17 (5.3) | 3.32 (2.09–5.25) | 14 (3.2) | 1.04 (0.58–1.84) |
| Never experienced | 1,360 | 64 (4.8) | 1 (Reference) | 28 (2.0) | 1 (Reference) | 46 (3.7) | 1 (Reference) |
| Usage of LAN gaming center in the past year | |||||||
| Yes | 1,084 | 68 (5.7) | 0.95 (0.60–1.52) | 37 (3.4) | 2.21 (1.15–4.23) | 45 (3.7) | 0.67 (0.40–1.12) |
| No | 762 | 40 (5) | 1 (Reference) | 17 (1.7) | 1 (Reference) | 27 (3.7) | 1 (Reference) |
| Use of karaoke room in the past year | |||||||
| Yes | 1,364 | 81 (5.4) | 1.35 (0.91–2.02) | 41 (2.9) | 1.59 (0.96–2.64) | 53 (3.5) | 1.11 (0.79–1.56) |
| No | 482 | 27 (5.3) | 1 (Reference) | 13 (2.3) | 1 (Reference) | 19 (4.4) | 1 (Reference) |
| Attended a concert in the past year | |||||||
| Yes | 257 | 12 (3.2) | 0.65 (0.36–1.16) | 5 (1.0) | 0.35 (0.16–0.77) | 9 (2.4) | 0.85 (0.42–1.72) |
| No | 1,589 | 96 (5.7) | 1 (Reference) | 49 (3.0) | 1 (Reference) | 63 (3.9) | 1 (Reference) |
| Attended a dance club in the past year | |||||||
| Yes | 3 | ||||||
| No | 1,843 | 108 (5.4) | 1 (Reference) | 54 (2.7) | 1 (Reference) | 72 (3.7) | 1 (Reference) |
* The PTA in the least-affected ear was used to categorize HL. HFHL was defined as PTAs at 0.5, 1, and 2 kHz ≥ 15 dB. SFHL was defined as PTAs at 3, 4, 6, and 8 kHz ≥ 15 dB. HL was considered present if bilateral HL was evident at either high or speech frequencies.
§ Unweighted frequencies with weighted percentages.
† The ORs for HL were calculated using multivariate logistic regression after adjusting for school level (= age), gender, household income, cigarette smoking and alcohol consumption status, a history of sinusitis, a history of otitis media, and a history of HL in the family.
†† Missing data (n = 216) was not included in this analysis.
# Missing data (n = 43) was no included in this analysis.
HL: hearing loss; HFHL: high-frequency hearing loss; SFHL: speech-frequency hearing loss; CI: confidence interval; PTA: pure tone average; OR: Odds Ratio.
Analysis of LAN gaming center use and HFHL prevalence showed a positive correlation between cumulative hours spent in gaming centers and HFHL prevalence (Table 4). Compared with never-users, the ORs for light users (bottom 50% of users) and heavy users (top 50%) were 1.57-fold (95% CI, 0.85–2.90) and 3.21-fold (95% CI, 1.60–6.88), respectively. The test for trends in cumulative use time was statistically significant (p = 0.003). However, no significant association was found between LAN use time and SFHL. The prevalence of HFHL was affected by the average use frequency (heavy users [7.7 ± 5.2 times]: OR, 2.43; 95% CI, 1.17–5.03) and time spent per visit (heavy users [2.6 ± 1.0 h]: OR, 2.14; 95% CI, 1.05–4.33).
Table 4. Multivariate logistic regression of the association between LAN gaming center-related variables and HL in Korean adolescents (n = 1,729).
| Classification | n | Mean ± SD | HFHL* | SFHL* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | %§ | OR | 95% CI | n | %§ | OR | 95% CI | |||
| Years from first use | ||||||||||
| Never-user | 762 | 17 | 1.7 | 27 | 3.7 | |||||
| Lower 50% | 526 | 1.9 ± 0.9 | 17 | 3.5 | 2.01 | (1.05–3.85) | 24 | 3.56 | 0.612 | (0.34–1.12) |
| Higher 50% | 441 | 5.8 ± 1.9 | 16 | 3.3 | 2.39 | (1.15–4.95) | 17 | 3.82 | 0.692 | (0.41–1.18) |
| p-value | 0.014 | 0.153 | ||||||||
| Number of visits per month - Usage number per month | ||||||||||
| Never-user | 762 | 17 | 1.7 | 27 | 3.7 | |||||
| Lower 50% | 475 | 1.3 ± 0.6 | 14 | 3.1 | 1.95 | (0.98–3.90) | 14 | 3.2 | 0.67 | (0.36–1.25) |
| Higher 50% | 492 | 7.7 ± 5.2 | 19 | 3.7 | 2.43 | (1.17–5.03) | 27 | 4.2 | 0.61 | (0.35–1.07) |
| p-value | 0.017 | 0.090 | ||||||||
| Hours spent at any one visit - Usage hours at one time | ||||||||||
| Never-user | 762 | 17 | 1.7 | 27 | 3.7 | |||||
| Lower 50% | 318 | 1.0 ± 0.2 | 4 | 3.4 | 2.12 | (1.14–3.92) | 7 | 3.9 | 0.72 | (0.43–1.22) |
| Higher 50% | 649 | 2.6 ± 1.0 | 29 | 3.4 | 2.14 | (1.05–4.33) | 34 | 3.6 | 0.60 | (0.33–1.09) |
| p-value | 0.035 | 0.095 | ||||||||
| Cumulative usage time | ||||||||||
| Never-user | 762 | 17 | 1.7 | 27 | 3.7 | |||||
| Light user (lower 50%) | 475 | 62.8 ± 49.4 | 12 | 2.5 | 1.57 | (0.85–2.90) | 14 | 4.0 | 0.80 | (0.45–1.41) |
| Heavy user (higher 50%) | 492 | 982.2 ± 1,158.0 | 21 | 4.2 | 3.21 | (1.60–6.88) | 27 | 3.4 | 0.49 | (0.27–0.87) |
| p-value | 0.003 | |
0.019 | |||||||
* The PTA in the better ear was used to categorize HL. HFHL was defined as PTAs at 0.5, 1, and 2 kHz ≥ 15 dB. SFHL was defined as PTAs of 3, 4, 6, and 8 kHz ≥ 15 dB.
§ Unweighted frequencies with weighted percentages.
HL: hearing loss; HFHL: high-frequency hearing loss; SFHL: speech-frequency hearing loss; CI: confidence interval; PTA: pure tone average; OR: odds ratio.
HL affected school performance. In children with ≥ 15 dB of HFHL or SFHL, the odds of lower academic performance were 1.33-fold (95% CI, 1.02–1.74) and 1.47-fold (95% CI, 1.21–1.79), respectively, higher than those of other children (Table 5).
Table 5. Adjusted ORs for self-rated lower academic performance by the extent of HL. (n = 1,806).
| Type of HL | No. | Self-rated poor academic performance | |
|---|---|---|---|
| n (%) § | OR (95% CI) † | ||
| Any HL* | |||
| Normal | 1,483 | 798 (46.8) | 1 (Reference) |
| Abnormal | 323 | 199 (62.6) | 1.46 (1.12–1.77) |
| Any HFHL* | |||
| Normal | 1,631 | 887 (54.0) | 1 (Reference) |
| Abnormal | 175 | 110 (61.1) | 1.33 (1.02–1.74) |
| Any SFHL* | |||
| Normal | 1,579 | 856 (53.6) | 1 (Reference) |
| Abnormal | 227 | 141 (63.1) | 1.47 (1.21–1.79) |
| Bilateral HL** | |||
| Normal | 1,701 | 925 (53.9) | 1 (Reference) |
| Abnormal | 105 | 72 (66.8) | 1.65 (1.10–2.47) |
| Bilateral HFHL** | |||
| Normal | 1,753 | 959 (54.3) | 1 (Reference) |
| Abnormal | 53 | 38 (65.1) | 1.60 (0.94–2.72) |
| Bilateral SFHL | |||
| Normal | 1,736 | 951 (54.2) | 1 (Reference) |
| Abnormal | 70 | 46 (66.0) | 1.44 (0.95–2.17) |
* The PTA in the poorer ear was used to categorize HL. HFHL was defined as PTAs at 0.5, 1, and 2 kHz ≥ 15 dB. SFHL was defined as PTAs at 3, 4, 6, and 8 kHz ≥ 15 dB.
** The PTA in the better ear was used to categorize HL. HFHL was defined as PTAs at 0.5, 1, and 2 kHz ≥ 15 dB. SFHL was defined as PTAs at 3, 4, 6, and 8 kHz ≥ 15 dB.
§ Unweighted frequencies with weighted percentages.
† ORs for HL were calculated by multivariate logistic regression after adjusting for school level, gender, and household income.
HL: hearing loss; HFHL: high-frequency hearing loss; SFHL: speech-frequency hearing loss; CI: confidence interval; PTA: pure tone average; OR: odds ratio.
Discussion
We found that the prevalence of HL was 17.2% overall, and 17.9% and 16.5% in middle and high schools, respectively. The extent of HFHL was 10.3%. LNE in noisy LAN gaming centers and setting earphone volume to levels causing others to ask that the volume be reduced affected HFHL. Both SFHL and HFHL were inversely associated with self-rated academic performance.
Currently, many adolescents use smartphones, which are the most common PLDs. In 2011, adolescent Korean smartphone users constituted 12.8% and 21.7% of all middle and high school students, respectively, but those figures rose to 86.6% and 90.2% in 2015 [19, 20]. The dramatic increase in accessibility to PLDs, and the resulting increase in LNE, can also be expected to affect the prevalence of noise-induced HL. We found no significant relationship between PLD use and HL. This seems to be due to variation in the interpretation of the question of whether or not a participant used a PLD. To determine whether the respondents used a PLD, the authors asked the following question.
“Do you use portable music and video playback devices, such as smart phones, MP3 players, or PMPs?”
Participants who had a smartphone for a purpose other than listening to music were also likely to answer “yes” and be misclassified as PLD users, which obscured the relationship between PLD use and HL. However, the following questions that concerned the precise pattern of PLD use showed that the requests to lower the volume seemed to be associated with greater HL. Therefore, the volume of LNE may be closely related to HL. This volume ranges from 50–100 dB. Use of PLDs at volumes > 80 dB LAeq increased hearing thresholds and affected syllable identification in a noisy environment [5]. We did not measure volume objectively. Rather, we recorded subjective volume intensities but found no relationship between self-reported volume and HL, which may indicate that self-reported volume data are inaccurate. However, we found a significant correlation between requests to lower the volume and HFHL, suggesting that the reactions of others to volume may be a simple and relatively accurate measure of volume control, and may be more reliable than self-reported volume.
We investigated the relationships between HL and several types of LNE: LAN gaming centers, karaoke rooms, and concert auditoria. The prevalence of HFHL was higher in adolescents using LAN gaming centers, in contrast to the findings of a recent report indicating that no significant relationship was evident between HL and the maximum equivalent LNE, such as time spent in nightclubs or music venues, at concerts or festivals, and listening through headphones [8]. Shin et al. explored noise exposure in Korean LAN gaming centers by installing noise dosimeters in the headsets of middle- and high-school students visiting such centers [21]. The average noise level was 80–85 dBA, and 6.7% of subjects were exposed to an average noise level >100 dBA, suggesting that the noise levels in gaming centers are high. Additionally, the LNEs of LAN gaming centers are repetitive and long. A total of 43.7% of our subjects reported that they visited such centers more than once a week; of these, >95% stated that they remained for >1 h on each visit. Frequent users (the top 50%) reported 7.7±5.2 visits/month and heavy users (the top 50%) remained for 2.6±1.0 h per visit. Of all students who used gaming centers, the number of visits per month, the length (in h) of any one visit, and cumulative visit time, were positively associated with HFHL. Therefore, LAN gaming centers may induce HFHL.
In contrast, subjects who attended concerts had a lower prevalence of HFHL than those who did not. Of 257 subjects who attended concerts in the past year, 154 (65.3%) went to a single concert, in marked contrast to the number of visits to LAN gaming centers. Occasional exposure to concert noise is less likely to affect hearing than repetitive noise. Also, the concert noise level would vary by the featured music genre. Last, those who attended concerts had higher family incomes than others; the negative association between concert attendance and HFHL is explained by the difference in income level.
Both HFHL and SFHL were negatively related to household income, consistent with the findings of previous studies. The National Health and Nutrition Examination Survey of 2005–2006 reported that school-aged children living in poverty had a higher prevalence of HL than other groups [11]. A Korean population-based study also reported an association between low family income and adolescent HL [13]. How household income affects hearing remains controversial. Some authors have suggested that any direct relationship between socioeconomic status and HL remains unproven, rather being attributable to other factors such as prematurity, low birth weight, or poor familial income attributable to parental hearing impairment [22, 23]. Other authors have found that adolescents of high socioeconomic status were more concerned about noisy activities and used more hearing-protection devices [24]. In our data, there was no association between household income and PLD use or volume. However, household income was negatively associated with LAN gaming center usage and was positively associated with Karaoke room usage and attending a concert. Comparing to the lowest income group, the highest income group had OR for LAN gaming center usage of 0.55 (95% CI: 0.30–0.99), OR for Karaoke room usage of 1.85 (95% CI: 1.004–3.41), and OR for attending a concert of 4.21 (95% CI: 2.28–7.79). The different pattern of LNE according to the household income may affect the different prevalence of HL.
We found that even slight HL among school-aged children is significantly associated with self-rated academic performance after adjusting for gender, grade, and household income. Previous studies found that educational performance was (negatively) associated with mild bilateral or unilateral HL [25–28]. Bess et al. reported that the grade retention rate (repeating one or more grades) of children with minimal sensorineural HL was significantly higher than the school-district norms, and that the educational performance of such children was significantly poorer than that of other children [29]. A recent, prospective cohort study showed that children with unilateral HL could catch up in terms of language and verbal intelligence skills over time but not in terms of academic performance [30]. School-aged children with minimal sensorineural HL exhibit poorer speech-recognition ability than those without HL [31]. Although some authors found no differences in terms of the effort devoted to hearing and the associated fatigue between children with minimal HL and others [32], the former children found listening demanding and experienced more listening-related fatigue, as did children with profound HL [33]. Furthermore, a population-based study in Australia showed that children with mild HL exhibited worse phonological short-term memory and phonological discrimination than others [34]. Therefore, differences in speech-recognition ability, short-term memory and listening-related fatigue may explain why children with slight HL exhibit poorer academic performance.
Hearing screening tests have been conducted in preschool and/or school-aged children in many countries [35, 36]. Pure tone audiometry at multiple frequencies, including 1, 2, and 4 kHz, is the usual method to screen school-age children, and the criteria for pass, refer, re-screen vary from 20 to 35 dB [36]. Currently, South Korea conducts simple hearing screening tests annually to all elementary school students in grades 1 and 4, and middle and high school students in grade 1. However, the screening test only records the presence or absence of a reaction in each ear when 40 dB of sound is delivered at a single frequency of 1 kHz. Therefore, it is difficult to detect a mild HL < 40 dB and/or HL limited to a specific frequency such as the ski-slope type of HL. The latest school hearing test report stated that the prevalence of “ear disease”, including HL, otitis media, and otitis externa is only 0.2% [37]. Thus, the current hearing test does not detect the slight HL affecting > 15% of all adolescents. Consequently, neither risk-factor control nor relevant education are yet possible. Given the fact that even slight HL can affect academic performance, and thus the self-esteem, of adolescents, we strongly recommend that careful hearing tests at several frequencies should be offered to middle and high school students [38].
Our study had certain limitations. Some questions required long-term memory recall (perinatal history of the child and residence history) and students often do not know their exact medical history. Thus, more complicated questions were answered by the parents, while students were asked about their major medical history in the past year. In addition, causal inferences cannot be drawn due to the cross-sectional nature of the study design. The school participation rate was low because of the complexity of the methods, which required active involvement of students, parents, and teachers. The audiological tests were conducted at the mobile soundproof booth in schools for convenience; this may have caused an increased prevalence of slight HL at the speech frequencies, due to uncontrolled environmental vibrations and excessive noises from the nearby playground or school buildings.
Despite these drawbacks, this study is noteworthy in that it assessed, through detailed audiometry, the actual prevalence of HL and HFHL in adolescents who were regarded as normal by conventional hearing screening testing. In addition, the authors analyzed the association between various types of LNE and HL. As LNE in adolescents is increasing, and is expected to increase further in the years to come, the results of our study constitute useful information for preventing HL in adolescents.
Conclusions
About 17% (one-sixth) of Korean adolescents exhibit at least slight HL. Frequent exposure to loud, high-intensity leisure noise can affect the hearing threshold. HL may be associated with poor school performance. It is important to avoid excessive exposure to leisure noise when seeking to prevent HL in adolescents.
Supporting information
(PDF)
(PDF)
(XLSX)
Acknowledgments
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see:
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
Funded by Korean society of otolaryngology-head and neck surgery. Grant number: 2016KORL0645. URL: http://www.korl.or.kr/. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Korean otology society Grant number: N/A. URL: http://www.otologicalsociety.or.kr/. Role: The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lie A, Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby KC, et al. Occupational noise exposure and hearing: a systematic review. Int Arch Occup Environ Health. 2016;89(3):351–72. 10.1007/s00420-015-1083-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ivory R, Kane R, Diaz RC. Noise-induced hearing loss: a recreational noise perspective. Curr Opin Otolaryngol Head Neck Surg. 2014;22(5):394–8. 10.1097/MOO.0000000000000085 . [DOI] [PubMed] [Google Scholar]
- 3.Sliwinska-Kowalska M, Davis A. Noise-induced hearing loss. Noise Health. 2012;14(61):274–80. 10.4103/1463-1741.104893 . [DOI] [PubMed] [Google Scholar]
- 4.Dehnert K, Raab U, Perez-Alvarez C, Steffens T, Bolte G, Fromme H, et al. Total leisure noise exposure and its association with hearing loss among adolescents. Int J Audiol. 2015;54(10):665–73. 10.3109/14992027.2015.1030510 . [DOI] [PubMed] [Google Scholar]
- 5.Kumar UA, Deepashree SR. Personal music systems and hearing. J Laryngol Otol. 2016;130(8):717–29. 10.1017/S0022215116001031 . [DOI] [PubMed] [Google Scholar]
- 6.Smith PA, Davis A, Ferguson M, Lutman ME. The prevalence and type of social noise exposure in young adults in England. Noise Health. 2000;2(6):41–56. . [PubMed] [Google Scholar]
- 7.Davis JM, Elfenbein J, Schum R, Bentler RA. Effects of mild and moderate hearing impairments on language, educational, and psychosocial behavior of children. J Speech Hear Disord. 1986;51(1):53–62. . [DOI] [PubMed] [Google Scholar]
- 8.Degeest S, Clays E, Corthals P, Keppler H. Epidemiology and Risk Factors for Leisure Noise-Induced Hearing Damage in Flemish Young Adults. Noise and Health. 2017;19(86):10 10.4103/1463-1741.199241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar A, Mathew K, Alexander SA, Kiran C. Output sound pressure levels of personal music systems and their effect on hearing. Noise Health. 2009;11(44):132–40. 10.4103/1463-1741.53357 . [DOI] [PubMed] [Google Scholar]
- 10.Vogel I, Verschuure H, van der Ploeg CP, Brug J, Raat H. Estimating adolescent risk for hearing loss based on data from a large school-based survey. Am J Public Health. 2010;100(6):1095–100. 10.2105/AJPH.2009.168690 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in prevalence of hearing loss in US adolescents. JAMA. 2010;304(7):772–8. 10.1001/jama.2010.1124 . [DOI] [PubMed] [Google Scholar]
- 12.Henderson E, Testa MA, Hartnick CJP. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. 2010:peds. 2010–0926. [DOI] [PubMed]
- 13.Hong SM, Park I-S, Kim YB, Hong SJ, Lee B. Analysis of the Prevalence of and Factors Associated with Hearing Loss in Korean Adolescents. PloS one. 2016;11(8):e0159981 10.1371/journal.pone.0159981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Center for Educational Statistics. List of educational institutions in 2015: Korean Educational Statistics Service; 2015 [cited 2017 March 21]. http://kess.kedi.re.kr/post/6650378?itemCode=04&menuId=m_02_04_02.
- 15.Cone BK, Wake M, Tobin S, Poulakis Z, Rickards FW. Slight-mild sensorineural hearing loss in children: audiometric, clinical, and risk factor profiles. Ear and hearing. 2010;31(2):202–12. 10.1097/AUD.0b013e3181c62263 [DOI] [PubMed] [Google Scholar]
- 16.Jun HJ, Hwang SY, Lee SH, Lee JE, Song JJ, Chae S. The prevalence of hearing loss in South Korea: data from a population-based study. Laryngoscope. 2015;125(3):690–4. 10.1002/lary.24913 . [DOI] [PubMed] [Google Scholar]
- 17.Faul F, Erdfelder E, Lang A-G, Buchner AJBrm. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. 2007;39(2):175–91. [DOI] [PubMed] [Google Scholar]
- 18.Kweon S, Kim Y, Jang M-j, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). 2014;43(1):69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.KISDI. Behavioral change in possession and use of media in 2015. KISDI Stat report. 2015;15(17):1–11. [Google Scholar]
- 20.Shin J, Ha J. Behavioral change in possession and use of media in 2011–2014. KISDI Stat report. 2014;12(1):1–10. [Google Scholar]
- 21.Shin JW, Kim HW. Noise Exposure Levels for the Middle and the High School Students using Headsets in the PC Rooms. Korean Industrial Hygiene Association Journal. 2005;15(2):135–43. [Google Scholar]
- 22.Kubba H, Macandie C, Ritchie K, MacFarlane M. Is deafness a disease of poverty? The association between socio-economic deprivation and congenital hearing impairment. International journal of audiology. 2004;43(3):123–5. [DOI] [PubMed] [Google Scholar]
- 23.Sutton GJ, Rowe SJ. Risk factors for childhood sensorineural hearing loss in the Oxford region. British journal of audiology. 1997;31(1):39–54. [DOI] [PubMed] [Google Scholar]
- 24.Widén SO, Erlandsson S. The influence of socio-economic status on adolescent attitude to social noise and hearing protection. Noise and health. 2004;7(25):59 [PubMed] [Google Scholar]
- 25.Blair JC. The effects of mild sensorineural hearing loss on academic performance of young school-age children. Volta Review. 1985;87(2):87–93. [Google Scholar]
- 26.Lieu JEC. Speech-language and educational consequences of unilateral hearing loss in children. Archives of Otolaryngology–Head & Neck Surgery. 2004;130(5):524–30. [DOI] [PubMed] [Google Scholar]
- 27.Quigley SP, Thomure FE. Some Effects of Hearing Impairment upon School Performance. 1969.
- 28.Tharpe AM. Unilateral and mild bilateral hearing loss in children: past and current perspectives. Trends in Amplification. 2008;12(1):7–15. 10.1177/1084713807304668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bess FH, Dodd-Murphy J, Parker RA. Children with minimal sensorineural hearing loss: prevalence, educational performance, and functional status. Ear and hearing. 1998;19(5):339–54. [DOI] [PubMed] [Google Scholar]
- 30.Lieu JE, Tye‐Murray N, Fu Q. Longitudinal study of children with unilateral hearing loss. The Laryngoscope. 2012;122(9):2088–95. 10.1002/lary.23454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crandell CC. Speech recognition in noise by children with minimal degrees of sensorineural hearing loss. Ear and hearing. 1993;14(3):210–6. [DOI] [PubMed] [Google Scholar]
- 32.Hicks CB, Tharpe AM. Listening effort and fatigue in school-age children with and without hearing loss. Journal of Speech, Language, and Hearing Research. 2002;45(3):573–84. [DOI] [PubMed] [Google Scholar]
- 33.Alhanbali S, Dawes P, Lloyd S, Munro KJ. Self-Reported Listening-Related Effort and Fatigue in Hearing-Impaired Adults. Ear and Hearing. 2017;38(1):e39–e48. 10.1097/AUD.0000000000000361 [DOI] [PubMed] [Google Scholar]
- 34.Wake M, Tobin S, Cone-Wesson B, Dahl H-H, Gillam L, McCormick L, et al. Slight/mild sensorineural hearing loss in children. Pediatrics. 2006;118(5):1842–51. 10.1542/peds.2005-3168 [DOI] [PubMed] [Google Scholar]
- 35.Lee J, Rhee J, Park SK, Chang J, Kim JS, Park KH, et al. Development of a More Effective Hearing Screening Questionnaire for Infants and Children during Medical Check-Ups. Korean Journal of Otorhinolaryngology-Head and Neck Surgery. 2016;59(4):273–80. [Google Scholar]
- 36.Sekhar DL, Zalewski TR, Paul IM. Variability of state school-based hearing screening protocols in the United States. J Community Health. 2013;38(3):569–74. 10.1007/s10900-013-9652-6 . [DOI] [PubMed] [Google Scholar]
- 37.Park S-W, Hwang JH. Analysis of results of health examination of elementary, middle and high school students in Korea. Korean Educational Development Institute, 2015. [Google Scholar]
- 38.Huang C. Self-concept and academic achievement: a meta-analysis of longitudinal relations. J Sch Psychol. 2011;49(5):505–28. 10.1016/j.jsp.2011.07.001 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.


