Abstract
Rationale:
Takotsubo syndrome (TTS) most commonly occurs in postmenopausal women who have been exposed to a triggering event such as acute physical or emotional distress. Sepsis-induced TTS in young premenopausal women were rarely reported. In particular, the relationship between sepsis-induced TTS and sepsis-induced cardiomyopathy (SIC) remains to be illuminated.
Patient concerns:
Two young premenopausal women were admitted to the hospital with sepsis and myocardial involvement.
Diagnosis:
Both patients fully met the Mayo Clinic criteria for TTS.
Interventions:
Both patients received anti-infection and fluid infusion treatment.
Outcomes:
Both patients were discharged without complications and the follow-up ultrasonic echocardiography showed normal results.
Lessons:
In this report, we describe 2 young premenopausal women with sepsis-induced TTS. There is an overlap between sepsis-induced TTS and SIC, and SIC could be a special type of TTS, which occurs under the stress of sepsis.
Keywords: premenopausal woman, sepsis-induced cardiomyopathy, sepsis-induced Takotsubo syndrome
1. Introduction
Takotsubo syndrome (TTS) is characterized by transient left ventricular dysfunction under severe emotional or physiological stress, also known as "apical ballooning syndrome”, "broken-heart syndrome", and ”stress cardiomyopathy”.[1,2] The syndrome was initially recognized and reported in Japan in 1990. Sato et al[3] named it after a narrow-necked, round-bottomed Japanese fishing pot used for trapping octopus, which is morphologically similar to the echocardiographic appearance of the heart. TTS most commonly occurs in postmenopausal women who have been exposed to a triggering event such as acute physical or emotional distress.[4,5] A previous analysis reported that sepsis was the most frequent cause of TTS, and TTS was prevalent in patients with sepsis, with an average age of 62.8 years.[6,7] Here we present 2 cases of sepsis-induced TTS occurring in young premenopausal women which were rarely reported, and further discuss the difference with sepsis-induced cardiomyopathy (SIC).
2. Case report
2.1. Case 1
A 28-year-old female first visited a local clinic with a sore throat. The patient was treated with intravenous antibiotic. She experienced sudden onset of fever and chills during antibiotic infusion, with decreased blood pressure of 70/40 mmHg. She was then transferred to our emergency department. Upon examination, her temperature was 37.5 °C, the heart rate was 110 beats per minute, the blood pressure was 65/37 mmHg, the respiratory rate was 23 breaths per minute, and the oxygen saturation was 94% while the patient was breathing 2 L of oxygen per minute. The remainder of the examination was normal. The results of her laboratory tests were listed in Table 1. Computer tomography scans of her chest, abdomen and pelvic cavity did not reveal any site of infection. The electrocardiogram (ECG) showed normal rhythm with T-wave inversion (Fig. 1), and transient accelerated idioventricular rhythm (Fig. 2). She was initially diagnosed as septic shock with multiple organ dysfunction. Ultrasonic echocardiography (UCG) on the 3rd day after admission showed decreased left ventricular apical impulse movement and a low left ventricular ejection fraction (LVEF) of 40%, which was diagnosed as TTS. Coronary arteriography on the 7th day after admission revealed no lesion. The final diagnosis was sepsis-induced TTS. The patient recovered after antibiotic and intravenous fluids resuscitation therapy, and finally, she was discharged from the hospital. The follow-up UCG was completely normal with LVEF of 77%.
Table 1.
Results of laboratory investigations in case 1.
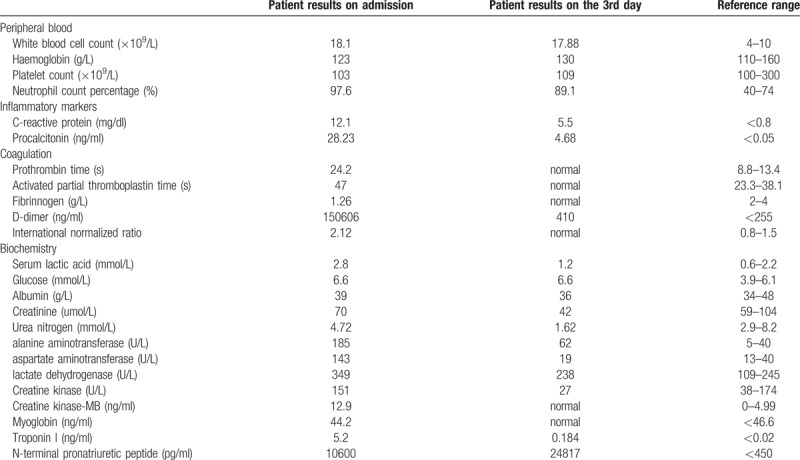
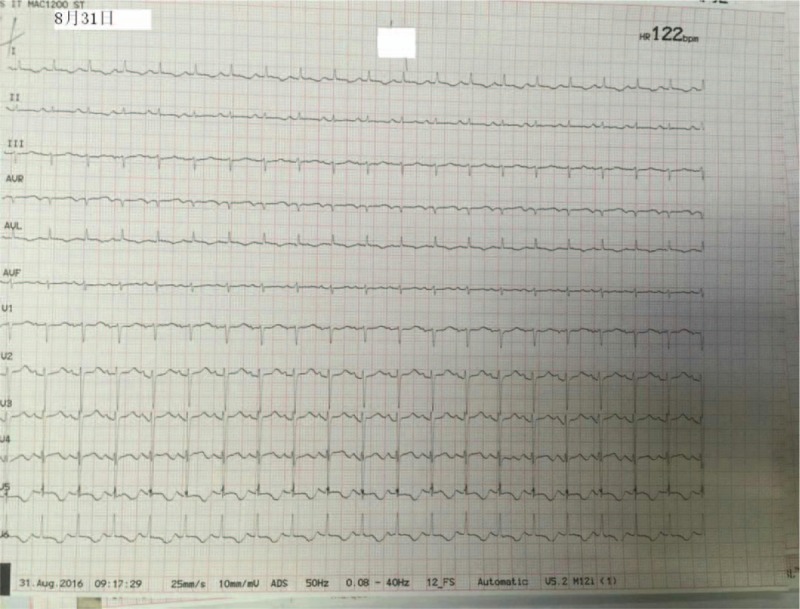
Figure 1.
The electrocardiogram on the 3rd day after admission in case 1. It showed T wave inversion in leads I, AVL, and V2-V6.
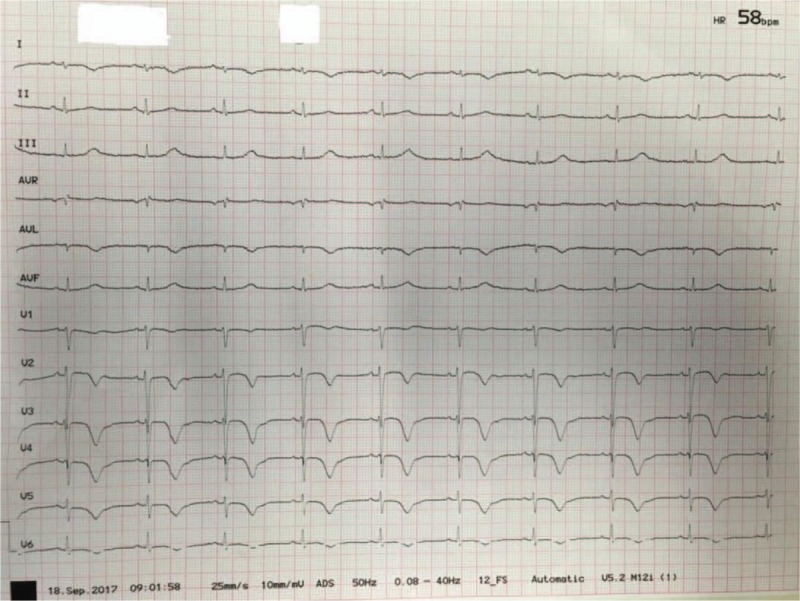
Figure 2.
The electrocardiogram on the 2nd day after admission in case 1. It showed accelerated idioventricular rhythm.
2.2. Case 2
A 48-year-old premenopausal female with past medical history of mixed connective tissue disease came to our emergency room with complaints of fever and dyspnea. Upon examination, her temperature was 38.8 °C, the heart rate was 125 beats per minute, the blood pressure was 134/67 mmHg, the respiratory rate was 24 breaths per minute, and the oxygen saturation was 96% while the patient was breathing 2 L of oxygen per minute. Both lungs could be heard moist rales. The remainder of the examination was normal. Results of her laboratory tests were listed in Table 2. Chest X-ray revealed left lung infection and a left pleural effusion. The ECG showed sinus tachycardia and T-wave inversion (Fig. 3). She was initially diagnosed as sepsis-associated multiple organ dysfunction caused by pneumonia and empyema. Her UCG on the 2nd day after admission showed no movement of the left ventricular mid to apical segments with LVEF of 30%, which was diagnosed as TTS. The patient was diagnosed with sepsis-induced TTS and discharged. The follow-up UCG was restored to normal with LVEF of 50% 2 months after her discharge.
Table 2.
Results of laboratory investigations in case 2.
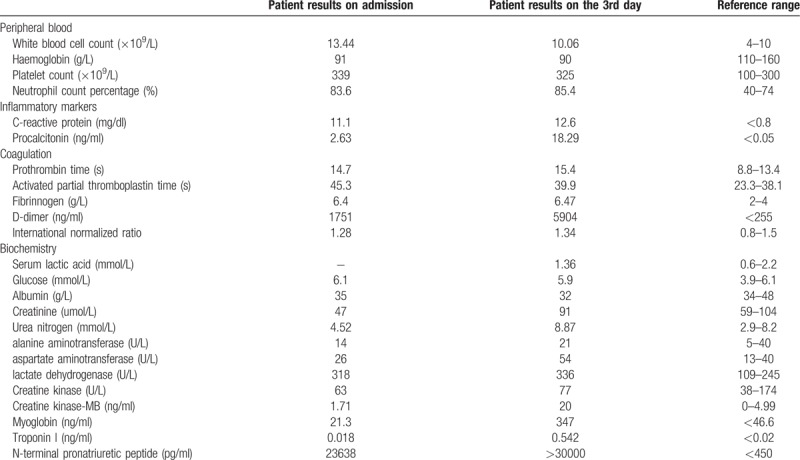
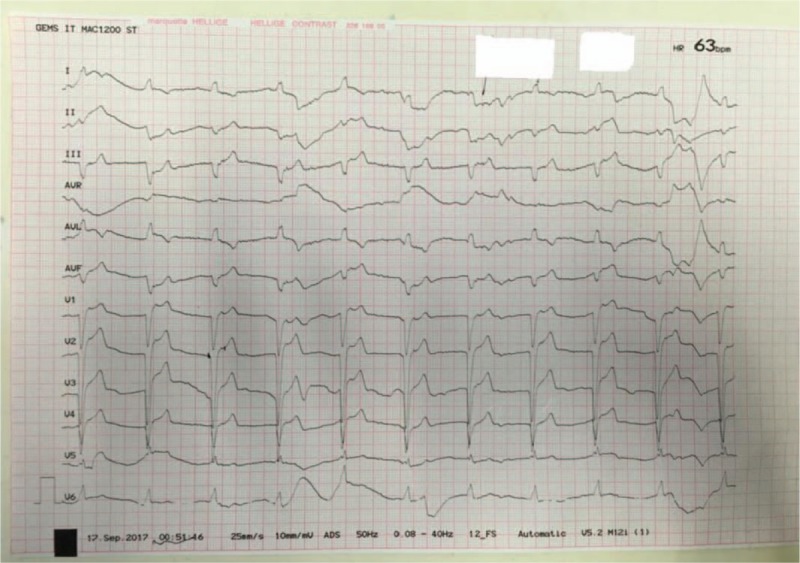
Figure 3.
The electrocardiogram on the 3rd day after admission in case 2. It showed sinus tachycardia with T wave inversion in leads I, AVL, and V5-V6.
3. Discussion
About 90% of TTS patients are women with a mean age of 67 to 70 years and around 80% are older than 50 years based on the published literatures.[8] Women older than 55 years have a 5-fold greater risk of developing TTS than women younger than 55 years and a 10-fold greater risk than men.[5] A hallmark of TTS is its association with a preceding stressful event, such as emotional stressors or physical stressors. Initially, most reported triggers involved an emotional trauma.[3] As TTS became better known, physical triggers are more commonly observed than emotional stress triggers.[8] A previous analysis reported that sepsis was the most frequent cause of TTS, and TTS was prevalent in patients with sepsis, with an average age of 62.8 years.[6,7] Both patients in this report with sepsis-induced TTS were young premenopausal women, which was rarely reported. On the other hand, about one-third of patients present without evidence of an identifiable preceding stressful event.[9]
Currently, the precise pathophysiological mechanism of TTS remains unclear, but there is considerable evidence that sympathetic stimulation is central to its pathogenesis. The most widely accepted hypothesis is an excess of catecholamines causing calcium overload in cardiac myocytes, leading to myocardial stunning.[10] The hypothesis was also confirmed by histopathology. The pathological changes of myocardial specimens, which came from patients who died of TTS, were consistent with the hearts of animals injected with large amounts of catecholamine.[11] Several other hypotheses have been proposed such as plaque rupture, multi-vessel epicardial spasm, microcirculatory dysfunction and activation of myocardial survival pathways.[12]
The 2 cases in our report meet the most widely cited TTS diagnostic criteria first introduced by Mayo Clinic in 2004 and modified in 2008.[13] Currently, there are new international criteria for the diagnosis of TTS that may help improve identification and stratification of TTS.[12] The 2 cases in this report both diagnosed as sepsis or septic shock initially. Both cases had elevated troponin levels with ECG changes. Both had UCGs that showed TTS without coronary lesion or history of coronary heart disease. The 2 patients both recovered and finally discharged with normal UCG results. All of these were in line with the new international diagnostic criteria.
Guidelines regarding TTS management are lacking as no prospective randomized clinical trials have been performed in this patient population. Therapeutic strategies are therefore based on clinical experience and expert consensus.[14] Recently, it has been suggested that the Ca2+-sensitizer Levosimendan could be used safely and effectively in TTS as an alternative inotrope to catecholamine agents.[15] As catecholamine levels are elevated in TTS, beta-blockers seem to be reasonable until full recovery of LVEF, but trials supporting this hypothesis are lacking. Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers may potentially facilitate left ventricular recovery.[14] The 2 cases mentioned in this report, 1 diagnosed with septic shock, another with hypotension, unable to use beta-blockers or angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers. We could try to use the Ca2+-sensitizer Levosimendan in such patients in the future.
Data on long-term survival of TTS is scarce. Both patients in this report survived and recovered after sepsis was cured, which seemly showed good prognosis of TTS. In the largest TTS registry to date, death rate is estimated to be 5.6% and rate of major adverse cardiac and cerebrovascular event is 9.9% per patient per year, suggesting that TTS is not a benign disease.[8] The predictive factors of TTS in 1-year mortality include atrial fibrillation, LVEF on admission <45%, and neurologic disorders, rather than TTS type.[16]
The intensive care unit patients were often under stress caused by physical factors, especially sepsis, resulting in sepsis-induced TTS or SIC. The relationship between the 2 diseases remains to be illuminated, which make it difficult to differentiate between them.
SIC is a complication of severe sepsis and septic shock first described by Parker et al in 1984 as a reversible myocardial depression that occurs in patients with septic shock.[17,18] SIC has 3 characteristics: reversible left ventricular dilatation, reversible depressed ejection fraction, and recovery in 7 to 10 days.[19] The pathogenesis of SIC is complicated that inotropic catecholamines may have adverse effect in patients with septic shock, and the decrease in β-adrenergic response in patients with SIC may be a protective mechanism to these effects.[19]
In summary, SIC has something in common with TTS:
-
(1)
Neither of their pathogenesis is related to blood supply obstacles in coronary artery, which extend beyond a single epicardial vascular distribution.
-
(2)
Catecholamine plays an important role in the pathogenesis of both.
-
(3)
Both are self-limiting disease. After the disease is cured, heart function could resume as usual.
Thus, there is an overlap between sepsis-induced TTS and SIC. In the opinion of the authors, SIC could be a special type of TTS, which occurs under the stress of sepsis.
The 2 cases mentioned in this report were both young premenopausal women diagnosed as sepsis-induced TTS, which was rarely reported. In future, we should strengthen the monitoring of young septic patients with myocardial involvement, which might be TTS.
4. Consent for publication
Informed written consent was obtained from the patients for publication of the case report and accompanying images.
Acknowledgments
We thanked for the patients’ cooperation during the treatment process.
Author contributions
Conceptualization: Fan Wang and Wei Wen.
Investigation: Fan Wang.
Methodology: Fan Wang.
Resources: Fan Wang.
Supervision: Wei Wen.
Writing – original draft: Fan Wang.
Writing – review and editing: Fan Wang and Wei Wen.
Footnotes
Abbreviations: ECG = electrocardiogram, LVEF = left ventricular ejection fraction, SIC = sepsis-induced cardiomyopathy, TTS = Takotsubo syndrome, UCG = ultrasonic echocardiography.
The authors report no conflicts of interest.
References
- [1].Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: a systematic review. Int J Cardiol 2008;124:283–92. [DOI] [PubMed] [Google Scholar]
- [2].Sharkey SW, Lesser JR, Maron MS, et al. Why not just call it tako-tsubo cardiomyopathy: a discussion of nomenclature. J Am Coll Cardiol 2011;57:1496–7. [DOI] [PubMed] [Google Scholar]
- [3].Sato H, Tateishi H, Uchida T, Dote K, Ishihara M. Takotsubo type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, eds. Clinical Aspect of Myocardial Injury from Ischemia to Heart Failure. Kagaku Hyoronsha, Tokyo, 1990:56-64 [in Japanese]. [Google Scholar]
- [4].Bybee K, Prasad A. Stress-related cardiomyopathy syndromes. Circulation 2008;118:397–409. [DOI] [PubMed] [Google Scholar]
- [5].Deshmukh A, Kumar G, Pant S, et al. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J 2012;164:66–71. e61. [DOI] [PubMed] [Google Scholar]
- [6].Han SJ, Lee TH, Bang CH, et al. Risk factors and outcomes of sepsis-induced myocardial dysfunction and stress-induced cardiomyopathy in sepsis or septic shock. Medicine 2018;97:e0263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cappelletti S, Ciallella C, Aromatario M, et al. Takotsubo cardiomyopathy and sepsis. Angiology 2017;68:288. [DOI] [PubMed] [Google Scholar]
- [8].Templin C, Ghadri JR, Diekmann J, et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015;373:929–38. [DOI] [PubMed] [Google Scholar]
- [9].Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006;27:1523–9. [DOI] [PubMed] [Google Scholar]
- [10].Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–48. [DOI] [PubMed] [Google Scholar]
- [11].Samuels MA. The brain-heart connection. Circulation 2007;116:77–84. [DOI] [PubMed] [Google Scholar]
- [12].Ghadri JR, Wittstein IS, Prasad A, et al. International expert consensus document on Takotsubo syndrome (part I): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J 2018;39:2032–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155:408–17. [DOI] [PubMed] [Google Scholar]
- [14].Ghadri JR, Wittstein IS, Prasad A, et al. International expert consensus document on Takotsubo syndrome (part II): diagnostic workup, outcome, and management. Eur Heart J 2018;39:2047–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Santoro F, Ieva R, Ferraretti A, et al. Safety and feasibility of levosimendan administration in takotsubo cardiomyopathy: a case series. Cardiovasc Ther 2013;31:e133–137. [DOI] [PubMed] [Google Scholar]
- [16].Ghadri JR, Cammann VL, Napp LC, et al. Differences in the clinical profile and outcomes of typical and atypical Takotsubo syndrome: data from the International Takotsubo Registry. JAMA Cardiol 2016;1:335–40. [DOI] [PubMed] [Google Scholar]
- [17].Tsuchihashi K, Ueshima K, Uchida T, et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 2001;38:11–8. [DOI] [PubMed] [Google Scholar]
- [18].Hoesel LM, Niederbichler AD, Ward PA. Complement-related molecular events in sepsis leading to heart failure. Mol Immunol 2007;44:95–102. [DOI] [PubMed] [Google Scholar]
- [19].Sato R, Nasu M. A review of sepsis-induced cardiomyopathy. J Intensive Care 2015;3:48. [DOI] [PMC free article] [PubMed] [Google Scholar]


