Abstract
Inguinal canal-related groin pain is common in athletes and may involve numerous structures such as the conjoint tendon and the transversalis fascia. Ultrasound is the only dynamic tool that shows the passage of preperitoneal fat at the level of the Hesselbach triangle and allows excluding true inguinal hernias. Fascia transversalis bulging and inguinal ring dilatation may also be described. MRI assesses injuries of rectus abdominis and adductor longus enthesis and osteitis symphysis but its accuracy for the diagnosis of inguinal-related groin pain remains debated.
Introduction
Groin pain is one of the most frequent complain in athletes and is involved in up to 6% of all sports-related pathologies1 and 4% of injuries in professional soccer players.2 The terminology used for groin pain in athletes remains unclear and includes «athletic pubalgia», «sportsman’s hernia», «posterior wall weakness» and “inguinal related or groin pain”.3, 4 Moreover, «sportsman’s hernia» is a misleading term, since no hernia is present. The 2014 Doha consensus conference identified four anatomical structures that may be the cause of groin pain: the inguinal wall, the proximal insertion of the adductor muscles, the pubic symphysis, and the iliopsoas muscle.5 Nevertheless, other causes such as hip internal derangement, rectus abdominis strain, pelvic stress fracture have also been cited.2, 6 Because of the anatomical continuum between the aponeuroses of the different muscles that insert in the pubic bone, these structures are often all involved.2,7–10 In athletes with inguinal canal-related groin pain, surgical studies usually differentiate lesions of the posterior wall, including the conjoint tendon and the transversalis fascia from those of the anterior wall, including the rectus abdominis muscle, the inguinal ligament and the external oblique aponeurosis.3, 11,12 The term «Sportsman’s hernia» does not seem accurate because it may still be confused with true inguinoscrotal hernia or wall weakness in young athletes.9
The role of imaging has not been fully clarified:4 the definition and the diagnostic criteria for the 2012 Manchester conference and updated at the 2014 Doha conference do not include imaging.3 Although several studies on the diagnosis and management of athletes with inguinal canal-related groin pain have been recently published,6, 11,12 data on imaging features remain scarce. A recent study reported the excellent diagnostic value of dynamic ultrasound for the diagnosis,11 and, although MRI remains the reference technique for the investigation of groin pain in athletes,13–15 its role in the management of this pathology has not been fully defined.4 MRI is the gold-standard for the assessment of symphysis, adductor-related groin pain and the evaluation of rectus abdominis muscle.16 However, the role of MRI for the diagnosis of inguinal canal-related groin pain is less well-defined. Nevertheless, imaging plays a significant role in the diagnosis of this entity, and can help improve patient management by avoiding unnecessary surgery and limiting costs.
The aim of this article is to review the role of imaging in inguinal canal-related groin pain based on anatomical, pathogenic and clinical features.
Anatomy
The inguinal area corresponds to the inferior and anterolateral part of the abdominal wall. The anatomic arrangement of the bones and the muscular and fascial layers of this area make it a site of potential weakness, mainly because of the passage of the inguinal canal in males. Indeed, the inguinal canal has an oblique shape,17 which is lateral to the rectus abdominis muscle and medial to the inferior epigastric vessels. The inguinal canal can be described as a cylinder surrounded by four walls and two rings:
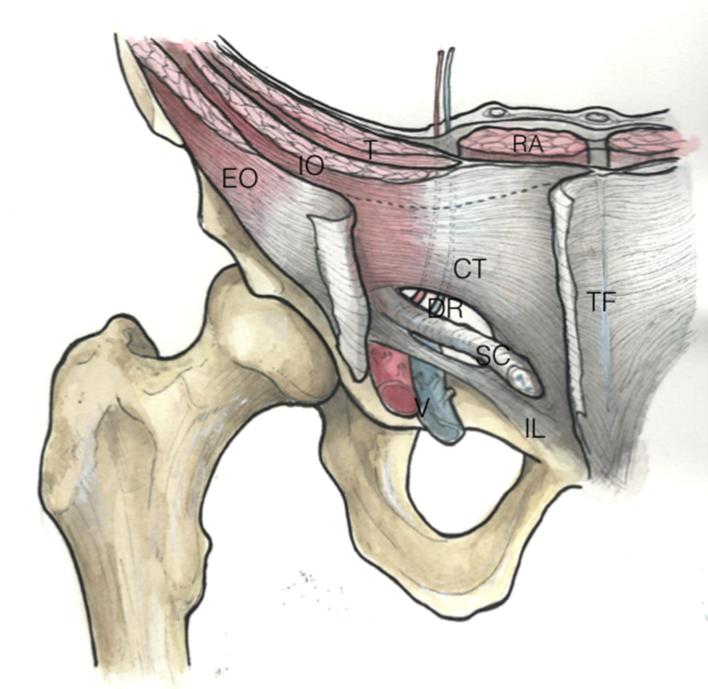
the superior wall, formed by the conjoint tendon (previously called the inguinal aponeurotic falx) of the internal oblique abdominal and the transverse abdominal muscles. Both muscles become aponeurotic before merging with the sheath of the rectus abdominis muscle18 (Figure 1).
he inferior wall (floor), including the cranial ramus of the pubic bone, and the inguinal ligament
the posterior wall, with the transversalis fascia and conjoint tendon;
the anterior wall, with the aponeurosis of external oblique and the fleshy part of the internal oblique muscle;
the superficial ring, subcutaneous and inferior, lateral and cranial to the pubic tubercle. This corresponds to a “window” between the lateral and medal pillars of the aponeurosis of the external oblique muscles.
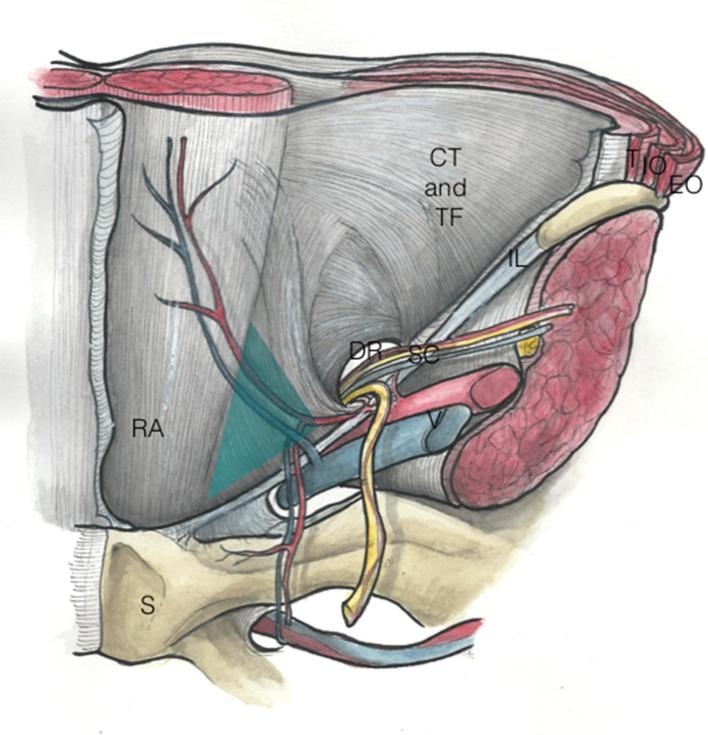
he deep ring, superior, and located at the middle of the inguinal ligament. It is inferior to the conjoint tendon, and lateral to the inferior epigastric vessels. Medial to this deep ring, the Hesselbach triangle is medial to the inferior epigastric vessels, lateral to the rectus abdominis muscles and cranial to the inguinal ligament. The deep ring and the Hesselbach triangle are the weak spots of the posterior wall, where sportsman’s hernia and true hernias may occur (Figure 2). Finally, this area is covered by preperitoneal fat and by the peritoneum.17
Figure 1.
Schematic drawing from an anterior view of the inguinal canal. The internal deep ring is superior, and located at the middle of the inguinal ligament. It is inferior and mediolateral to the conjoint tendon, and lateral to the inferior epigastric vessels. The external superficial ring is a triangular opening in the external oblique aponeurosis. The inferior epigastric artery (a) and vein (v) originate from the external iliac artery and vein and lie medial to the internal inguinal ring. CT, conjoint tendon; EO, external oblique muscle; EOA, external oblique aponeurosis; IL, inguinal ligament; IO, interne oblique muscle; RA, rectus abdominis; SC, spermatic cord; T, transverse muscle; TF, transversalis fascia; DR, deep ring.
Figure 2.
Schematic drawing from a posterior view of the Hesselbach triangle. Medial to this deep ring, the Hesselbach triangle is medial to the inferior epigastric vessels, lateral to the rectus abdominis muscles and cranial to the inguinal ligament. CT, conjoint tendon; TF, transversalis fascia; IL, inguinal ligament; RA, rectus abdominis; DR, deep ring; S, symphysis; SC, spermatic cord; T, transverse muscle; O, interne oblique muscle; E, external oblique muscle.
The inguinal canal contains:
in male: the spermatic cord, and its coverings and the ilioinguinal nerve. The spermatic cord normally contains three arteries (the artery to the vas deferens, the testicular artery and the cremasteric artery), three fascial layers (the external spermatic, cremasteric, and internal spermatic fascia); the pampiniform plexus, the vas deferens (ductus deferens), testicular lymphatics, and three nerves (genital branch of the genitofemoral nerve, sympathetic and visceral afferent fibres, ilioinguinal nerve)
in female: the round ligament of the uterus, the ilioinguinal nerve and the genital branch of the genitofemoral nerve.19
Pathophysiology
The origin of inguinal canal-related groin pain is functional.20 Physiologically, during muscular contraction of the abdominal wall, the conjoint tendon lowers and closes the deep inguinal ring like “a curtain” decreasing its diameter. Thus, the inguinal canal becomes more oblique and longer, and the deep ring of the inguinal canal moves upwards and outwards. Functionally, the “sealing” of the inguinal canal depends upon the contraction of the flat muscles, mainly the internal oblique muscle as well as the morphology of the conjoint tendon.19
Thus, in the presence of the conjoint tendon, the internal oblique muscle compresses by contracting the inguinal canal, acting as a “sphincter” and preventing the development of a hernia.17, 21 According to our experience, conjoint tendon abnormalities play a role in the defective covering of the deep ring during muscle contraction, weakening the posterior wall. When this is combined with repetitive microtraumatic muscular lesions, parietal weakness can develop.
The lowering of the conjoint tendon towards the inguinal ligament, the upwards and outwards movement of the deep inguinal ring, the closing of the pillars of the external oblique muscle resulting in narrowing of the superficial inguinal ring, the retraction of the cremaster and the ascent of the cord are all anatomic factors that limit the opening of the canal. Inguinal wall weakness may involve one or more of the parietal components of the anterior or posterior walls.7
Posterior wall deficiency is due to degeneration of the transversis abdominis and internal oblique muscles resulting in weakness of the posterior inguinal wall, which become lax and can protrude into the inguinal canal causing a mass effect during straining. With ongoing injury, this can potentially in turn lead to complete disruption of the posterior wall resulting in a direct inguinal hernia. The conjoint tendon and/or the fascia transversalis are most frequently involved according to recent surgical descriptions3, 11 (Figure 3) . At the posterior wall, protrusion of the pre-peritoneal fat in the spermatic cord contributes to the progressive widening of the deep inguinal ring helping maintain the degeneration of the posterior wall, resulting in:
Figure 3.
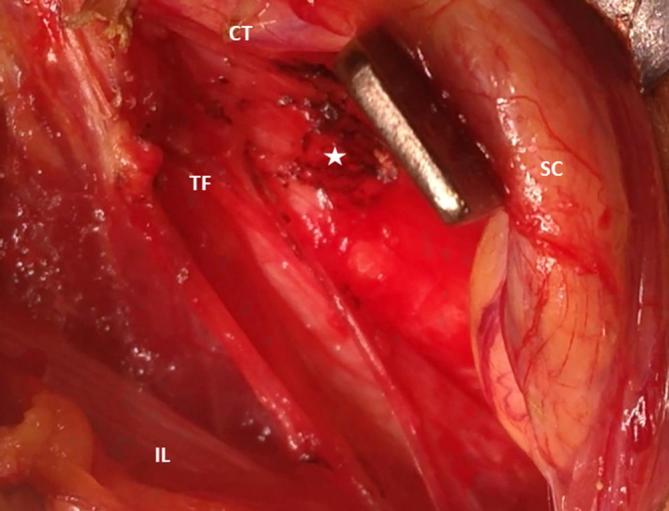
Anterior laparoscopic view of the inguinal canal during Shouldice procedure shows dehiscence of the TF and protrusion of pre-peritoneal fat (star). CT, conjoint tendon; IL, inguinal ligament; SC, Spermatic cord; TF, transversalis fascia.
Compression of the genital branch of the genitofemoral nerve or the ilioinguinal nerve, leading to the development of a neuroma called the “hockey groin syndrome” in the literature;13
Functional imbalance between the abdominal wall and adductor muscles due to the anatomic relationships of those structures and the deficiency of the conjoint tendon and fascia transversalis.1, 7
Anterior wall deficiency arises as a consequence of degeneration and tear of the external oblique muscle and aponeurosis resulting in a dehiscence between the inguinal ligament and leading to dilatation of the superficial inguinal ring. Positive imaging findings are rarely seen in this group and therefore this is primarily a clinical diagnosis.
Clinical presentation
Inguinal-related groin pain is relatively frequent and represents up to 18% of consultations in sports medical departments, with a ratio of 9 males/1 female.8, 9 It is associated with sports with increased intra-abdominal pressure involving kicks, rapid changes in direction and rapid twist starts, which are found in sports such as football, rugby, hockey or running.1, 9 The pain is inguinal near the pubic tubercle. It usually occurs gradually and is frequently unilateral, ranging from simple discomfort to severe pain sometimes extending to the pelvis, perineum, thigh root and lumbar region. It is generally worsened by stress and relieved by rest. The pain is worsened by contraction contraresistance of the abdominal muscles during Valsalva maneuvers, coughing or sneezing. Initially, the pain disappears when sports are no longer practiced, then may gradually become permanent and may prevent the practice of sports altogether.3 The 2014 Doha Consensus Conference clearly redefined the clinical diagnosis of inguinal-related groin pain as the presence of least three of the following five signs:5
pain with palpation of the pubic tubercle at the insertion of the conjoint tendon;
pain with palpation of the deep inguinal ring;
pain or dilatation of the superficial inguinal ring without hernia;
pain at the origin of the tendon of the long adductor; and/or
diffuse inguinal pain radiating to the perineum, thigh or contralateral level.
However, recent studies22, 23 suggested sportsman’s hernia is often associated with other causes of groin pain in the athlete (Table 1).
Table 1.
Differential diagnosis of inguinal-related groin pain in the athlete
| Structures | Types of lesions |
| Symphysis pubis | Osteitis pubis |
| Adductor longus tendon | Enthesitis/tendinitis/tear |
| Rectus abdominis muscle | Muscle strain/fatty infiltration |
| Iliopsoas muscle | Muscle strain |
| Snapping | |
| Hip joint | Osteoarthritis |
| Femoroacetabular impingement | |
| Labral tears | |
| Pelvic bones | Stress fractures |
| Nerves | Lumbar nerves referred pain |
Imaging
Conventional radiographs
Conventional radiographs are essential to evaluate the pubic symphysis, and to eliminate congenital abnormalities such as femoroacetabular impingement, developmental dysplasia of the hip as well as degenerative conditions of hip and sacroiliac joints. Furthermore, they may also indicate erosions, sclerosis and symphysis widening in cases of osteitis pubis.24 In adolescent athletes, signs of pubic apophysitis can be seen at secondary ossification centers.25 Indeed, Sailly et al26 identified another cause of groin pain due to a pubic apophysitis at the secondary ossification centre located along the anteromedial corner of pubis beneath the insertions of symphysial joint capsule and adductor longus tendon.
Ultrasound
Technique
An ultrasound examination should be performed with the patient resting in the supine position and should include Valsalva maneuvers in the supine and standing position. A bilateral and comparative examination should be performed8, 27,28 with a high-frequency probe (linear 12- to 18 MHz transducer). First, in the axial position, the Hesselbach triangle is located between the ostium of the lower epigastric arteries on the external iliac artery and the lateral edge of the rectus abdominis muscle. The deep inguinal ring is located lateral to the lower epigastric artery. Then, the posterior wall of the inguinal canal is assessed for bulging at rest and with Valsava maneuvers. Still in axial position, the transducer is moved down to the level of the medial attachment of the inguinal ligament crossing the superficial inguinal ring, by following the spermatic cord to the pubic tubercle. Once the spermatic cord is visualized, anterior motion of the pre-peritoneal fat is observed while repeating the Valsava maneuver. The sagittal assessment is performed from the ostium of the lower epigastric artery sliding the transducer medially and laterally. At this level, the inguinal ligament may be identified in its short axis at the lower edge of the deep inguinal ring.
Normal features
In young athletic subjects, there should be no prominence of the pre-peritoneal fat through the deep inguinal ring or the Hesselbach triangle when the examination at rest is compared to that with abdominal pressure (Figure 4).28 On the axial plane, the distance between the lateral edge of the rectus abdominis and the ostium of the lower epigastric artery is usually less than 2 cm.13
Figure 4.
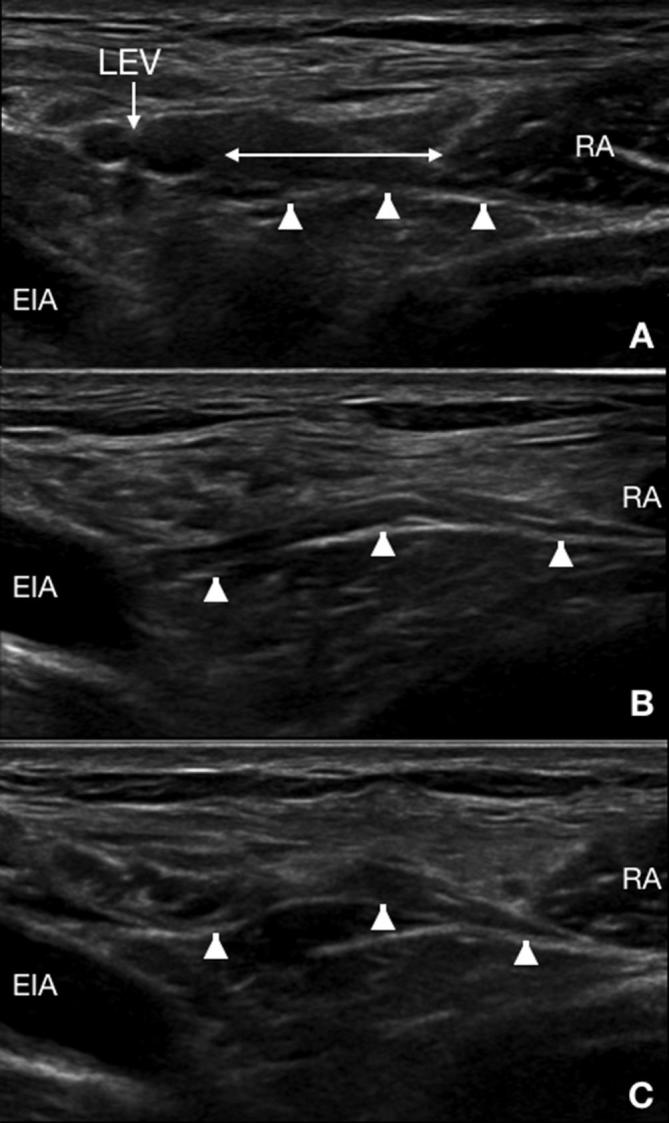
Ultrasound of an asymptomatic male athlete. Dynamic ultrasound in the axial plane at rest (A) and at the beginning (B) and end (C) of Valsalva’s maneuvers shows the location of the Hesselbach triangle (double arrows) at the level of the LEV. Additionally, there is a slight convexity of the fascia transversalis (arrowheads) without protrusion of pre-peritoneal fat. LEV, lower epigastric vessels; RA, rectus abdominis.
Pathological features
Several studies8, 11,29 have described a posterior wall bulge or protrusion of pre-peritoneal fat through the Hesselbach triangle or the deep ring during abdominal thrusts11 (Figure 5). In a study of 573 patients who underwent surgery, Santilli et al11 showed that ultrasound had a sensitivity of 95% and a specificity of 100% compared with the findings of laparoscopy with positive and negative predictive values close to 100%. Others features have been described such as a convex and painful bulge of the transversalis fascia30 or inguinal dilatation of more than 2 cm on dynamic ultrasound.31
Figure 5.
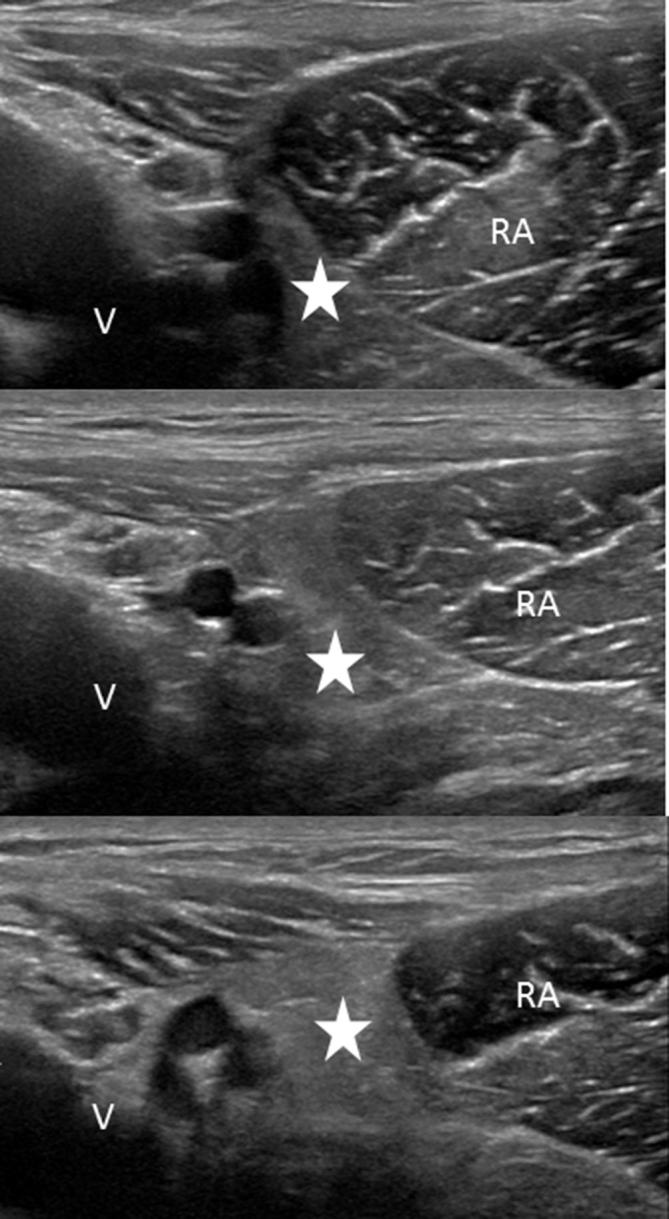
Ultrasound of a 27-year-old male soccer player with bilateral groin pain. Dynamic ultrasound at the level of Hesselbach’s triangle of the right deep inguinal ring in the transverse planes shows progressive bulging of the preperitoneal fat during Valsalva’s maneuvers (white arrow). V, vessels; RA, rectus abdominis.
Ultrasound helps to exclude the main differential diagnosis of inguinal hernia, which corresponds to the passage of peritoneal fat and the peritoneum with or without digestive contents, medial to the inferior epigastric vessels in the Hesselbach triangle (direct inguinal hernia) or lateral to the inferior epigastric vessels through the deep inguinal ring (indirect inguinal hernia).32 In these cases, the presence of hyperechoic fat tissue in the Hesselbach triangle between the ostium of the lower epigastric artery and the rectus abdominis is abnormal both at rest and during effort.28 Parietal weakness may be asymptomatic and is more frequent in elderly patients.28 Anatomical variants of the conjoint tendon or abnormalities of the transversalis fascia are not directly visible on ultrasound.11 Very few ultrasound features have been described for the superficial inguinal ring. The presence of a neuroma of the genitofemoral nerve is an interesting indirect sign of anterior wall weakness.33 In our experience, the ultrasound features of lesions of the aponeurosis of the external oblique muscle remain unknown.
MRI
A few recent studies have assessed the role of MRI in inguinal related groin pain.4, 6,13,15,16,34,35
Imaging protocols
Several authors6, 15,35 described a MRI protocol tailored to clinical athletic pubalgia including coronal short tau inversion-recovery (STIR) and T1 weighted spin echo sequences with a large field of view (ranging from 28 to 36 cm) to exclude remote pathologies. Then, sequences should be acquired with a surface coil, placed over the anterior pelvis centered at the pubic symphysis. Our protocol includes sagittal and axial T2 weighted fat spin echo (FSE) fat-suppressed sequences as well as proton density FSE-weighted and T2 weighted FSE fat-suppressed axial oblique sequence angled with the anterior border of the ileum.15, 35 Although the goal of T1 weighted images is to identify the anatomical structures, fat-saturated T2 weighted images allow visualizing signal abnormalities in tendinous and bony structures. Three-dimensional T1 weighted acquisitions may be helpful when using reformatted images in the plane of the conjoint tendon, the inguinal ligament or the aponeurosis of the external oblique muscle19, 34 (Table 2). Valsalva maneuver can improve the performance of the MRI but is not performed in a routine protocol.35 In a recent study, Omar et al36 performed dynamic T1 weighted sequence in order to assess anterior motion of the posterior wall to detect lipoma within the inguinal canal. Gadolinium-chelate is mainly used in patients with a previous history of surgery.19, 34
Table 2.
MRI protocol
| Plan | Sequence | TE (ms) | TR (ms) | Thickness (mm)/gap | FOV (cm) | Matrix |
| Coronal | T1 | Min | 572 | 3,5/0,4 | 36 | 448 × 320 |
| Oblique axial | T1 | Min | 572 | 3,5/0,4 | 24 | 512 × 320 |
| Oblique axiale | PD/FS | 45 | 3241 | 3.5/0.4 | 24 | 512 × 320 |
| Axial | STIR | 42 | 4968 | 4/1 | 38 | 352 × 256 |
| Sagittal | DP/FS | 45 | 3241 | 3/0,4 | 24 | 512 × 320 |
FOV, field of view; FS, fat saturation; PD, proton density; STIR, short tau inversion-recovery; TE, echo time; TR, repetition time.
Posterior wall
Some articles13, 14,16 have described the MRI features of posterior wall weakness as a bulging or convex appearance of the deep inguinal ring and/or the Hesselbach triangle13 (Figure 6). The limits of the Hesselbach triangle are difficult to visualize on MRI. In our experience, axial T1 weighted images can help identify the aponeurosis of the external oblique muscle and the transversalis fascia on the axial plane, and the conjoint tendon on coronal plane (Figure 7). Read et al34 described the conjoint tendon on oblique coronal T1 and T2 weighted images as a hypointense structure stretching from the underside of the oblique internal and transverse muscles to the inguinal ligament. Cherian et al37 identified the conjoint tendon in a coronal plane CT scan. If the conjoint tendon and the inguinal ligament are far apart, this may be a risk factor for inguinal related groin pain.34 However, this feature is difficult to assess because there is no accepted reference distance. The presence of pre-peritoneal fat without a hernial sac can be visualized in the spermatic cord and has been previously described in the literature as a lipoma38 (Figure 8). Another indirect feature of posterior wall weakness is the anterior displacement of the vas deferens.13, 34 A German study13 described signal abnormalities of the deep ring with significant dilatation of more than 2 cm. Inguinal ligament abnormalities such as abnormal insertion, thickening or thinning, traumatic lesions and/or tearing have also been reported.12 Maquirriain et al39 have also described associated insertions as well as morphological and signal abnormalities of the rectus abdominis and flat muscles.
Figure 6.
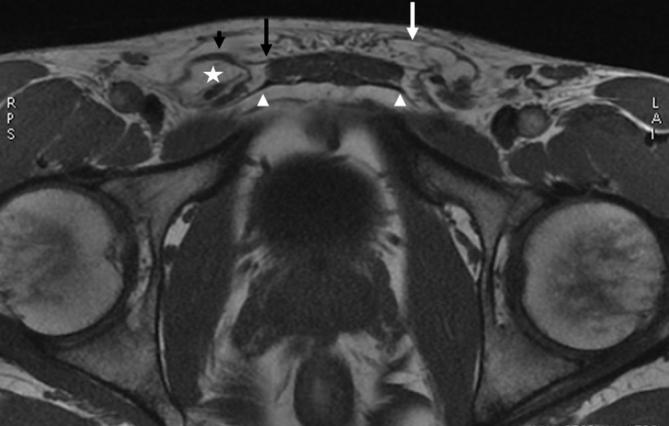
MRI of a 25-year-old male rugby player with bilateral groin pain. 3D-GE T1 weighted sequence in the axial plane shows fat within the right spermatic cord (white star), anterior wall bulging and thickening of the right external oblique aponeurosis (black arrowhead), normal distal insertion of the CT (white arrowheads) and tear of the left external oblique (white arrow). 3D, threedimensional.
Figure 7.
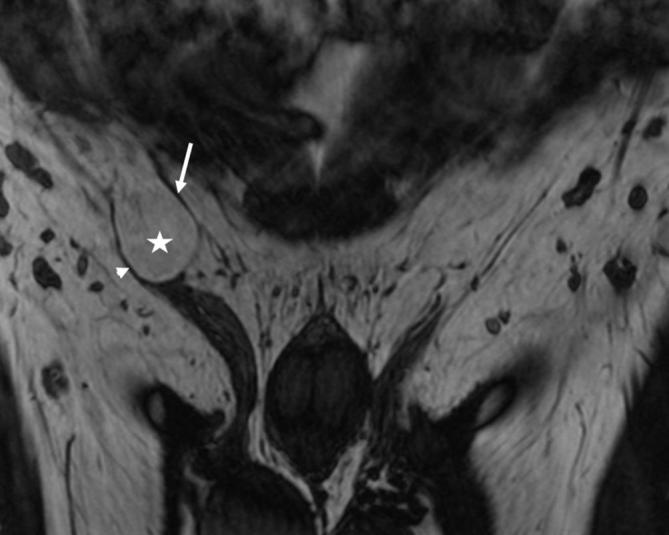
MRI of a 27-year-old male soccer player with right groin pain. 3D-GE T1 weighted sequence in the coronal plane shows thinning thickening of the inguinal ligament (arrowhead) and conjoint tendon (arrow). 3D, three-dimensional.
Figure 8.
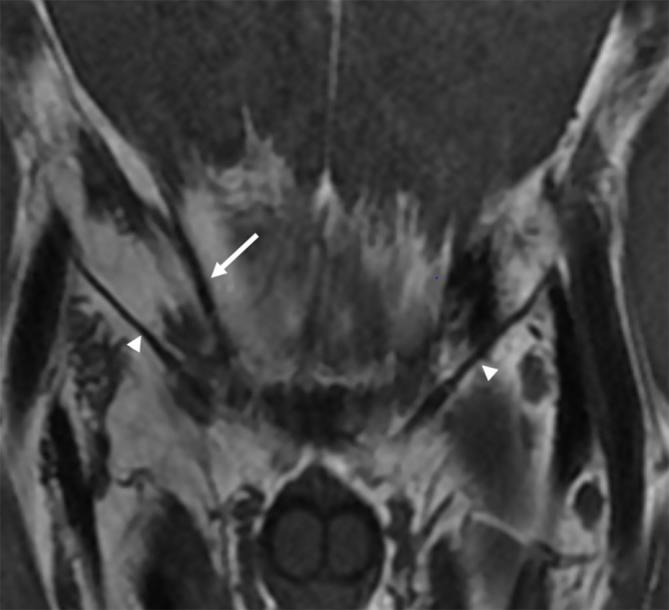
MRI of a 23-year-old male soccer player with right groin pain. 3D-GE T1 weighted sequence in the coronal plane shows fat within the right spermatic cord (white star), thinning and stretching of the inguinal ligament (arrowhead) and thinned conjoint tendon (white arrow).
Anterior wall
Because the aponeurosis of the external oblique muscle is so thin, there are very few reports of the MRI features of anterior wall lesions. Hyperintense signal of the superficial ring has been described on T2 weighted images and may be a sign of injury.13 Iliohypogastric and ilioinguinal neuroma or impingement is difficult to visualize due to the limited spatial resolution of MRI.33
Conclusion
Inguinal-related groin pain was redefined by the Doha conference in 2014 and was chosen as the preferred term to describe weakness of the posterior wall of the inguinal canal with projection of pre-peritoneal fat through the weakness area (Hesselbach triangle or deep inguinal ring) without true hernia. Ultrasound examination shows the fat protrusion medial to the lower epigastric vessels during Valsalva maneuvers. MRI may confirm bulging of the anterior and posterior walls, and/or the presence of fat within the cord. The conjoint tendon may also be visualized. Thus, thorough knowledge of imaging techniques and the features of this entity can help confirm the diagnosis and optimize patient management.
Contributor Information
Myriame Bou Antoun, Email: myriame.bouantoun@gmail.com.
Gilles Reboul, Email: gilles.reboul@orange.fr.
Maxime Ronot, Email: maxime.ronot@aphp.fr.
Amandine Crombe, Email: amandine.crombe2@gmail.com.
Nicolas Poussange, Email: nicolaspoussange@me.com.
Lionel Pesquer, Email: Lionelpesquer@gmail.com.
REFERENCES
- 1.Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med 2001; 29: 521–33. doi: 10.1177/03635465010290042501 [DOI] [PubMed] [Google Scholar]
- 2.Agten CA, Sutter R, Buck FM, Pfirrmann CW. Hip imaging in athletes: sports imaging series. Radiology 2016; 280: 351–69. doi: 10.1148/radiol.2016151348 [DOI] [PubMed] [Google Scholar]
- 3.Dimitrakopoulou A, Schilders E. Sportsman's hernia? An ambiguous term. J Hip Preserv Surg 2016; 3: 16–22. doi: 10.1093/jhps/hnv083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weir A, Robinson P, Hogan B, Franklyn-Miller A. MRI investigation for groin pain in athletes: is radiological terminology clarifying or confusing? Br J Sports Med 2017; 51: 1185–6. doi: 10.1136/bjsports-2016-096973 [DOI] [PubMed] [Google Scholar]
- 5.Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015; 49: 768–74. doi: 10.1136/bjsports-2015-094869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hegazi TM, Belair JA, McCarthy EJ, Roedl JB, Morrison WB. Sports Injuries about the Hip: What the Radiologist Should Know. Radiographics 2016; 36: 1717–45. doi: 10.1148/rg.2016160012 [DOI] [PubMed] [Google Scholar]
- 7.Robertson BA, Barker PJ, Fahrer M, Schache AG. The anatomy of the pubic region revisited. Sports Med 2009; 39: 225–34. doi: 10.2165/00007256-200939030-00004 [DOI] [PubMed] [Google Scholar]
- 8.Balconi G. US in pubalgia. J Ultrasound 2011; 14: 157–66. doi: 10.1016/j.jus.2011.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Minnich JM, Hanks JB, Muschaweck U, Brunt LM, Diduch DR. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 2011; 39: 1341–9. doi: 10.1177/0363546511402807 [DOI] [PubMed] [Google Scholar]
- 10.Munegato D, Bigoni M, Gridavilla G, Olmi S, Cesana G, Zatti G. Sports hernia and femoroacetabular impingement in athletes: a systematic review. World J Clin Cases 2015; 3: 823. doi: 10.12998/wjcc.v3.i9.823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santilli OL, Nardelli N, Santilli HA, Tripoloni DE. Sports hernias: experience in a sports medicine center. Hernia 2016; 20: 77–84. doi: 10.1007/s10029-015-1367-4 [DOI] [PubMed] [Google Scholar]
- 12.Sheen AJ, Iqbal Z. Contemporary management of 'Inguinal disruption' in the sportsman's groin. BMC Sports Sci Med Rehabil 2014; 6: 39. doi: 10.1186/2052-1847-6-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koulouris G. Imaging review of groin pain in elite athletes: an anatomic approach to imaging findings. AJR Am J Roentgenol 2008; 191: 962–72. doi: 10.2214/AJR.07.3410 [DOI] [PubMed] [Google Scholar]
- 14.Chopra A, Robinson P. Imaging athletic groin pain. Radiol Clin North Am 2016; 54: 865–73. doi: 10.1016/j.rcl.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 15.Branci S, Thorborg K, Bech BH, Boesen M, Magnussen E, Court-Payen M, et al. The Copenhagen Standardised MRI protocol to assess the pubic symphysis and adductor regions of athletes: outline and intratester and intertester reliability. Br J Sports Med 2015; 49: 692–9. doi: 10.1136/bjsports-2014-094239 [DOI] [PubMed] [Google Scholar]
- 16.Zoga AC, Kavanagh EC, Omar IM, Morrison WB, Koulouris G, Lopez H, et al. Athletic pubalgia and the "sports hernia": MR imaging findings. Radiology 2008; 247: 797–807. doi: 10.1148/radiol.2473070049 [DOI] [PubMed] [Google Scholar]
- 17.Kingsnorth AN, Skandalakis PN, Colborn GL, Weidman TA, Skandalakis LJ, Skandalakis JE. Embryology, anatomy, and surgical applications of the preperitoneal space. Surg Clin North Am 2000; 80: 1–24. doi: 10.1016/S0039-6109(05)70394-7 [DOI] [PubMed] [Google Scholar]
- 18.Bhosale PR, Patnana M, Viswanathan C, Szklaruk J. The inguinal canal: anatomy and imaging features of common and uncommon masses. Radiographics 2008; 28: 819–35. doi: 10.1148/rg.283075110 [DOI] [PubMed] [Google Scholar]
- 19.Revzin MV, Ersahin D, Israel GM, Kirsch JD, Mathur M, Bokhari J, et al. US of the inguinal canal: comprehensive review of pathologic processes with CT and MR imaging correlation. Radiographics 2016; 36: 2028–48. doi: 10.1148/rg.2016150181 [DOI] [PubMed] [Google Scholar]
- 20.Thomeé R, Jónasson P, Thorborg K, Sansone M, Ahldén M, Thomeé C, et al. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc 2014; 22: 835–42. doi: 10.1007/s00167-013-2721-7 [DOI] [PubMed] [Google Scholar]
- 21.Peiper C, Junge K, Prescher A, Stumpf M, Schumpelick V. Abdominal musculature and the transversalis fascia: an anatomical viewpoint. Hernia 2004; 8: 376–80. doi: 10.1007/s10029-004-0254-1 [DOI] [PubMed] [Google Scholar]
- 22.Naal FD, Dalla Riva F, Wuerz TH, Dubs B, Leunig M. Sonographic prevalence of groin hernias and adductor tendinopathy in patients with femoroacetabular impingement. Am J Sports Med 2015; 43: 2146–51. doi: 10.1177/0363546515591259 [DOI] [PubMed] [Google Scholar]
- 23.Strosberg DS, Ellis TJ, Renton DB. The role of femoroacetabular impingement in core muscle injury/athletic pubalgia: diagnosis and management. Front Surg 2016; 3: 6. doi: 10.3389/fsurg.2016.00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paksoy M, Sekmen U. Sportsman hernia; the review of current diagnosis and treatment modalities. Turk J Surg 2016; 32: 122–9. doi: 10.5152/UCD.2015.3132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O'Dell MC, Jaramillo D, Bancroft L, Varich L, Logsdon G, Servaes S. Imaging of sports-related injuries of the lower extremity in pediatric patients. Radiographics 2016; 36: 1807–27. doi: 10.1148/rg.2016160009 [DOI] [PubMed] [Google Scholar]
- 26.Sailly M, Whiteley R, Read JW, Giuffre B, Johnson A, Hölmich P. Pubic apophysitis: a previously undescribed clinical entity of groin pain in athletes. Br J Sports Med 2015; 49: 828–34. doi: 10.1136/bjsports-2014-094436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Balius R, Pedret C, Galilea P, Idoate F, Ruiz-Cotorro A. Ultrasound assessment of asymmetric hypertrophy of the rectus abdominis muscle and prevalence of associated injury in professional tennis players. Skeletal Radiol 2012; 41: 1575–81. doi: 10.1007/s00256-012-1429-y [DOI] [PubMed] [Google Scholar]
- 28.Morley N, Grant T, Blount K, Omar I. Sonographic evaluation of athletic pubalgia. Skeletal Radiol 2016; 45: 689–99. doi: 10.1007/s00256-016-2340-8 [DOI] [PubMed] [Google Scholar]
- 29.Jamadar DA, Jacobson JA, Morag Y, Girish G, Ebrahim F, Gest T, et al. Sonography of inguinal region hernias. AJR Am J Roentgenol 2006; 187: 185–90. doi: 10.2214/AJR.05.1813 [DOI] [PubMed] [Google Scholar]
- 30.Orchard JW, Read JW, Anderson IJ. The use of diagnostic imaging in sports medicine. Med J Aust 2005; 183: 482. [PubMed] [Google Scholar]
- 31.Muschaweck U, Berger LM. Sportsmen's groin-diagnostic approach and treatment with the minimal repair technique: a single-center uncontrolled clinical review. Sports Health 2010; 2: 216–21. doi: 10.1177/1941738110367623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vasileff WK, Nekhline M, Kolowich PA, Talpos GB, Eyler WR, van Holsbeeck M. Inguinal hernia in athletes: role of dynamic ultrasound. Sports Health 2017; 9: 414–21. doi: 10.1177/1941738117717009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tagliafico A, Bignotti B, Cadoni A, Perez MM, Martinoli C. Anatomical study of the iliohypogastric, ilioinguinal, and genitofemoral nerves using high-resolution ultrasound. Muscle Nerve 2015; 51: 42–8. doi: 10.1002/mus.24277 [DOI] [PubMed] [Google Scholar]
- 34.Garvey JFW, Read JW, Turner A. Sportsman hernia: what can we do? Hernia 2010; 14: 17–25. doi: 10.1007/s10029-009-0611-1 [DOI] [PubMed] [Google Scholar]
- 35.Zajick DC, Zoga AC, Omar IM, Meyers WC. Spectrum of MRI findings in clinical athletic pubalgia. Semin Musculoskelet Radiol 2008; 12: 003–12. doi: 10.1055/s-2008-1067933 [DOI] [PubMed] [Google Scholar]
- 36.Omar IM, Zoga AC, Kavanagh EC, Koulouris G, Bergin D, Gopez AG, et al. Athletic pubalgia and "sports hernia": optimal MR imaging technique and findings. Radiographics 2008; 28: 1415–38. doi: 10.1148/rg.285075217 [DOI] [PubMed] [Google Scholar]
- 37.Cherian PT, Parnell AP. Radiologic anatomy of the inguinofemoral region: insights from MDCT. AJR Am J Roentgenol 2007; 189: W177–W183. doi: 10.2214/AJR.07.2489 [DOI] [PubMed] [Google Scholar]
- 38.Lilly MC, Arregui ME. Lipomas of the cord and round ligament. Ann Surg 2002; 235: 586–590. doi: 10.1097/00000658-200204000-00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maquirriain J, Ghisi JP, Kokalj AM. Rectus abdominis muscle strains in tennis players. Br J Sports Med 2007; 41: 842–8. doi: 10.1136/bjsm.2007.036129 [DOI] [PMC free article] [PubMed] [Google Scholar]