Abstract
Background:
Accumulating evidence has reported that physical activity (PA) is effective in reducing stroke and mortality. However, whether PA levels are associated with stroke in middle-aged and elderly people in Jiangxi Province of China remains unclear. In the present study, we evaluated the association between PA and the risk of stroke in Jiangxi Province of China.
Methods:
A cross-sectional survey was conducted in Jiangxi Province of China from November 2013 to August 2014, using standardized questionnaire forms and physical measurements. Self-reported PA was assessed using the international PA questionnaire. A history of stroke was self-reported by answering the questionnaire. Multivariate logistic regression analysis was performed to evaluate the association between PA levels and the risk of stroke after adjustment for sociodemographic characteristics, lifestyle factors, and disease-related risk factors.
Results:
A total of 10,398 participants (4240 men and 6158 women, aged 45 to 97 years) completed the International Physical Activity Questionnaire (IPAQ). Compared with low-intensity PA, vigorous PA was associated with graded reduction in the risk of stroke (odds ratio [OR] of 0.763, 95% confidence interval [CI] 0.717–0.812, P < .001 for trend). However, there were no significant differences between individuals in the low-intensity PA and moderate-intensity PA group (P > 0.05).
Conclusions:
Compared with low PA, vigorous PA, but not moderate PA, was associated with a lower risk of stroke in middle aged and elderly people in southern China, specifically among men. These findings suggested that increasing PA is beneficial.
Keywords: China, cross-sectional survey, physical activity, stroke
1. Introduction
Since the availability of new devices has continued to increase, physical inactivity is rising in many regions, both at work and at home. This phenomenon has caused new problems for human health—a decrease in the frequency of infectious diseases and an increase in non-communicable diseases.[1,2] In 2009, physical inactivity was reported to be the fourth leading risk factor for non-communicable diseases.[3] Among these diseases, stroke has developed to be a leading health problem worldwide for it is the second most common cause of mortality and the most common cause of long-term disability.[4–10] Despite recent reductions in stroke mortality in developed countries, the global stroke burden is increasing for a majority of the cases are from developing countries where stroke is one of the most common causes of death.[5,6,8,11–13]
Physical activity (PA) is defined by the World Health Organization (WHO) as any bodily movement produced by skeletal muscles that results in energy expenditure, including activities performed while working, playing, carrying out household chores, traveling, and engaging in recreational pursuits.[14] Increasing PA is associated with a decreased mortality rate and improved quality of life. The results from observational and cohort studies all have demonstrated an inverse association between PA and the risk of stroke and all-cause mortality.[12,15] A prospective urban rural epidemiology (PURE) study, including >130,000 participants from 17 countries, confirmed that higher PA was associated with a lower risk of stroke and mortality.[12] Mcdonnell M and colleagues observed that participation in regular moderate-to-vigorous PA (MVPA) reduced the risk of cardiovascular disease and stroke.[16]
To date, the information regarding the inverse associations of PA with people's health in China is increasing.[12,17,18] However, there were obvious differences between PA distributions and risks of diseases in different regions of China. The China Kadoorie Biobank Study whose participants were recruited from 10 diverse areas in China found that the percentage of stroke was 11.7% and each 4 MET-h/d higher PA (approximately1 hour of brisk walking per day) associated with a 6% lower risk of stroke.[18,19] A large prospective cohort containing 359,067 Taiwanese adults reported a low proportion of moderate-high PA and prevalence rate of cardiovascular disease or stroke upped to 3.0%.[20] The Dongfeng-Tongji (DFTJ) cohort of 24,606 middle-aged and older people from Shiyan city observed that there were 82.2% of subjects performing equal to or more than the WHO recommended minimum (7.5 MET-h/wk) and the percentage of circulatory system diseases was 0.36%.[21]
China is the most populous nation in the world and there are great differences in local economic development and health care in different regions of China. All these affected PA distributions and the prevalent tendency of disease. In addition, China is experiencing a rapid aging transition and an increasing in the risk of stroke.[12] Therefore, it is necessary to analyze the relationship between PA and stroke in various domains of daily living. In this study, we examined whether PA is associated with a lower risk of stroke in Jiangxi Province, China.
2. Methods
2.1. Study design and participants
This cross-sectional survey was supported by the National Key R&D Program in the Twelfth Five-year Plan (No. 2011BAI11B01) from the Chinese Ministry of Science. Using a stratified multistage random sampling method, Jiangxi Province was divided into urban areas and rural areas based on administrative data. The details of the overall study design are described below. Eight different areas were selected using the probability-proportional-to-size method, in which 2 districts or 2 townships were selected. Next, 3 communities or villages were chosen within each district and township, respectively, using the simple random sampling (SRS) method.[22] Finally, a given number of participants from each of the 14 strata were chosen using the SRS method according to the national demographic composition; participants who stay locally for >6 months in Jiangxi Province, aged ≥15 years old, living in the administrative divisions directly under control of the central government throughout China measurements were chosen from communities or villages using the lists compiled from the local government registers of households.[22] The design effect was also considered while estimating the sample size. Assuming a design effect of 2.5 and a prevalence of stroke of 1.48% among the residents, aged 15 years and older, it was estimated that 15,269 participants were required for the analysis to ensure that the average lengths of the 95% confidence intervals for prevalence in the entire population and in the subpopulations, defined by age and sex, were <0.4% and 1.8%, respectively.[22] As a result, 15,364 residents aged 15 years and older who were intending to stay locally for >6 months were approached for this survey from November 2013 to August 2014. After excluding participants with missing data, the final sample size included in the analysis based on the outcome of interest was middle-aged and elderly people over 45 years. Only these populations were selected because the rate of stroke among people under 45 years of age was low. Therefore, 10,389 participants were included in the analysis.
2.2. Ethics statement
All participants who provided written informed consent were enrolled in the study. If the participants were unable to write, fingerprinting was used. This study was approved by the Medical Research Ethics Committee of the Second Affiliated Hospital of Nanchang University and the Fuwai Cardiovascular Hospital (Beijing, China).
2.3. Definitions
PA was assessed with the International Physical Activity Questionnaire (IPAQ) which was supported by the WHO and the Centers for Disease Control (CDC), suitable for assessing population levels of self-reported physical activity.[23–26] Participants in all groups were instructed to report the frequency and duration of walking or cycling and moderate-intensity and vigorous-intensity activity, including occupation or housework, transportation and leisure time, performed for at least 10 minutes per session. Both continuous and categoric indicators were obtained from the IPAQ. Weekly minutes of walking or cycling and moderate-intensity and vigorous-intensity activity were calculated separately by multiplying the number of d/wk by the duration on an average day. The reported minutes per week in each category were weighted by a metabolic equivalent of the task (MET; multiples of resting energy expenditure) resulting in a PA estimate independent of body weight, expressed in MET-min/wk and computed by multiplying METs by min/wk. The categoric analysis grouped each individual as performing low, moderate, or vigorous PA, according to the questionnaire scoring protocol previously described (standard scoring criteria http://www.ipaq.ki.se.). Participants were asked to report only episodes of activities of at least 10 minutes because it is the minimum time required to achieve health benefits. Values below 10 minutes were recorded as 0.
The detailed description of the categories is as follows:
-
(1)
Low: Meets neither “moderate” nor “vigorous” criteria.
-
(2)
Moderate: Meets any of the following 3 criteria: 3 days of vigorous activity of at least 20 min/d; 5 days of moderate-intensity activity or walking of >30 min/d for >10 minutes at a time; or 5 days of any combination of walking, moderate-intensity, or vigorous-intensity activities, achieving at least 600 MET-min/wk.
-
(3)
Vigorous: Meets either of 2 criteria: vigorous-intensity activity for >3 d/wk and accumulating at least 1500 MET-min/wk, or (b) >5days of any combination of walking, moderate-intensity, or vigorous-intensity activities, achieving at least 3000 MET min/wk.
History of stroke was included if the subjects self-answered “yes” to the question, “Have you ever been told by a doctor or other health professional that you had a stroke?” These patients were also asked for symptoms, initial dates, and diagnostic units to make a reasonable assessment of the original diagnosis. Stroke included subarachnoid hemorrhage, intracerebral hemorrhage, or cerebral ischemic necrosis but did not include secondary stroke caused by transient cerebral ischemia, brain tumor, brain metastasis tumor, or trauma.
Hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg, and if the individual was at least on one of antihypertensive drugs for 2 weeks.[27]
Body mass index (BMI) was calculated as the weight (kg)/height (m2). BMI ≥24 kg/m2 was defined as an elevated BMI. Abnormal WC was defined as above 0.85 for women and girls and above 0.9 for men and boys.
Smoking habit was defined as never, current (daily smoking, >6 months), and former (cessation of smoking, >6 months). Alcohol drinking was defined as drinking alcohol at least one time per week during the previous year.[28–31]
Educational level was divided into 3 domains according to the number of years of education, including 0 to 6, 7 to 9, and ≥10 years.
The inclusion criteria referred to the reference norm of BP, BMI, and WC for the screening of hypertension, overweight, and abnormal WC in Chinese people from Chinese guidelines.[27,32,33]
2.4. Data collection procedures
Participants were required to complete a questionnaire developed by the coordinating center, Fuwai Hospital which was administered through face-to-face interviews by trained staff to obtain information on demographic characteristics and socioeconomic factors.[22] There are 11 questions included in the questionnaire in this study, including demographic data (such as age, sex, marital status, residence, education, and employment status), behavioral characteristics (such as smoking habits, drinking, and physical activity), and medical history (hypertension and stroke, which was collected and verified with medical or hospital records). The details of anthropometric data and clinical variables will be detailed below.
Physical measurements, including body height, weight, waist circumference (WC), heart rate (HR), and blood pressure (BP), were collected by standardized methods for anthropometrics. All investigators were medical professionals who were systematically trained, and standard protocols and instruments were used. Body weight without heavy clothing and shoes to the nearest 0.1 kg was measured indoors using an Omron body fat and weight measurement device (V-BODY HBF-371, Omron, Kyoto, Japan). Height was measured without shoes and hats using a standard right-angle device and a fixed measurement tape to the nearest 0.5 cm. In addition, participants whose hair fluffy should be compacted and the hair knot should be unraveled. When measuring waist circumference, participants were asked to take off their coat and waist circumference was obtained to the nearest 0.5 cm by putting the measuring tape at the midpoint between the lower margin of the last rib and the top of the hip bone (at the level of umbilicus directly on the skin) at the end of the expiration. All measurements were taken twice, and the average of the 2 values was used. Blood pressure and heart rate were measured with the OMRON HBP-1300 professional portable blood pressure monitor (OMRON) 3 times on the right arm positioned at heart level after the participant was sitting at rest for 5 minutes without talking, with 30 seconds between each measurement with an observer present, the average of the 3 readings was used for analysis.[22,34] Participants were asked to avoid vigorous exercise, smoking, drinking, and consumption of coffee and tea for at least 30 minutes before the measurements.
To ensure standardization and data quality, comprehensive operations manuals, reinforced by periodic training workshops and regular communication, were used at all sites. Data were entered locally at each site into a customized database programmed with range and consistency checks and transmitted electronically to the coordinating center, where further quality control measures were implemented.
2.5. Statistical analysis
All data were established using the EpiData version 3.02 software (Odense, Denmark). After alignment correction, both Empower (R) (www.empowerstats.com; X&Y Solutions, Inc., Boston, MA) and Microsoft Excel 2007 were used for statistical analysis. Multiple imputation, based on 5 replications and a chained equation approach method in the R MI procedure was used to account for missing data. Continuous variables are presented as the mean ± standard deviation and are compared using the t test. Categorical variables are expressed as percentages and analyzed using the chi-square test or Fisher exact test, as appropriate. Because of significant differences in various baseline characteristics between stroke and non-stroke patients, a propensity score weighting method was applied. Inverse probability of treatment weight (IPTW) was then calculated as the inverse of the propensity score for stroke patients and as the inverse of (1 – propensity score) for the non-stroke patients. Therefore, IPTW multivariate logistic regression analysis was used to assess the association between PA and stroke.[35] Statistical significance was based on P < .05.
3. Results
As shown in Fig. 1, a total of 15,296 participants from 15,364 eligible participants were included in the statistical analysis and 10,389 participants were finally included in this study. Sixty-eight participants were excluded because of missing data including sex, age, and so on. The majority of non-responders were young people because of their busy work. Then 200 participants were excluded because of missing data for PA (n = 72) and stoke (n = 128). Based on the outcome of our interest that middle-aged and elderly people over 45 years had higher risk of stroke, the next 4698 individuals who were <45 years old were excluded.
Figure 1.
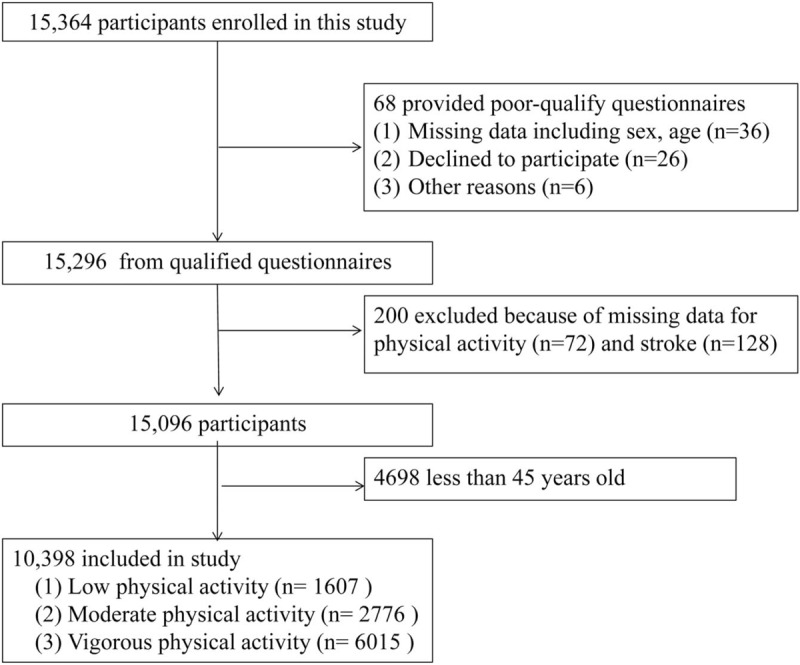
Participant selection for the study.
3.1. Characteristics of the subjects
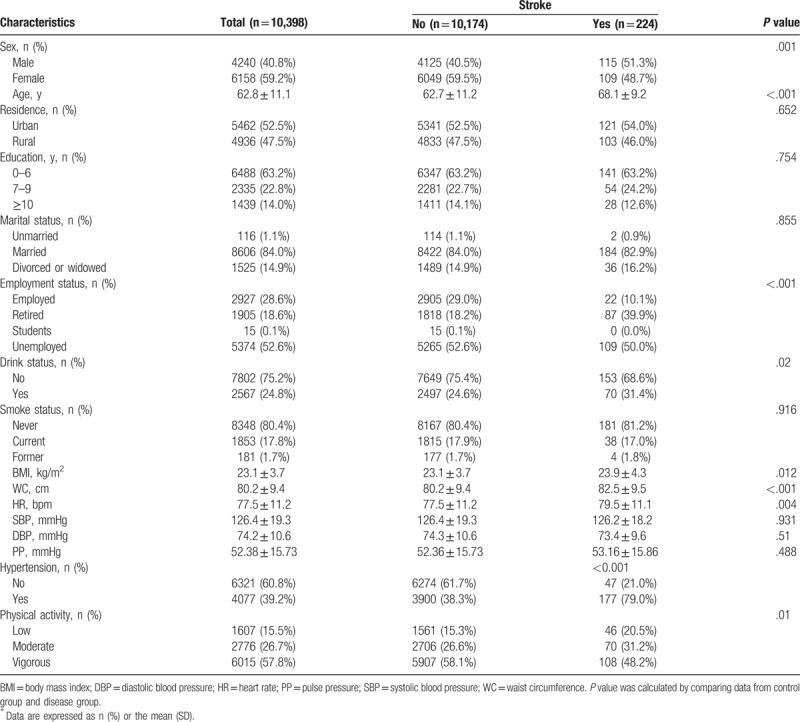
A total of 10,398 participants out of 15,364 eligible participants (4240 men and 6158 women, aged 45–97 years) were included in this analysis and the average age was 62.8 ± 11.1 years in Table 1. Of these participants, 5462 (52.5%) came from urban areas, and 4936 (47.5%) came from rural areas. The prevalence of stroke was 215.0 per 10,000 people (224 cases). Of the 10,398 participants, the percentage of PA levels from low-intensity, moderate-intensity, and vigorous-intensity were 15.5%, 26.7%, and 57.8%, respectively. Compared with the control group, those who had stroke were more likely to have men, a higher mean age, BMI, WC, and HR, history of hypertension, drinkers, and those retired or unemployed. In addition, there was significant difference in the distribution of PA being observed between disease group and the control group.
Table 1.
Characteristics of participants∗.
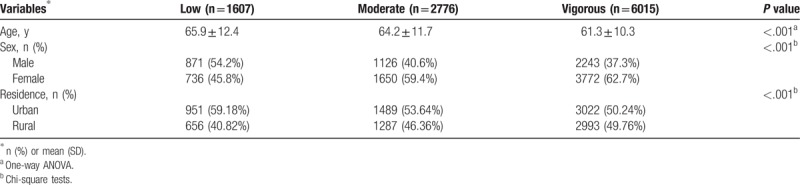
3.2. Distribution of PA
Table 2 presents the distribution of physical activity by sex and age. People were younger with PA changes from low to high (P < .001). Compared with men, women had lower rate of low-intensity PA and higher rate of moderate- and vigorous-intensity PA. The same trend was occurred in urban and rural.
Table 2.
Distribution of physical activity levels.
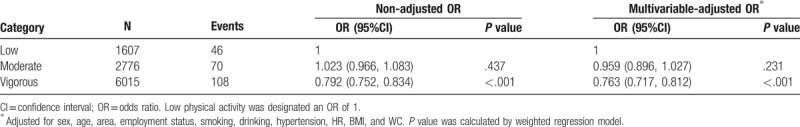
3.3. Association between PA and stroke
Table 3 shows the weighted association between PA and stroke. There were 224 individuals with incident of stroke. When stratified by PA, there was a downward trend in the risk of stroke from low to moderate-vigorous PA. Participants in the vigorous-intensity PA group were significantly associated with lower rates of stroke compared with the low group (P < .001). After adjustment for sex, age, area, smoking, drinking, employment, BMI, WC, HR, and hypertension, the trend still existed and participants with vigorous-intensity PA had an OR of 0.763 (95% confidence interval [CI] 0.717–0.812) for stroke (P < .001). However, there was no difference between individuals in the low-intensity PA and the moderate group (P > .05).
Table 3.
Association between physical activity and lower risk of stroke.
4. Discussion
Increased PA in daily life may contribute to various health benefits and decreased risk of diseases, such as stroke. In our study, we observed that participants with vigorous PA, but not moderate PA, had a lower risk of stroke in Jiangxi Province, China. The assessment of PA levels referenced the International Physical Activity Questionnaire (IPAQ) whose activities come from different sources activities, including occupation or housework, transportation, and leisure time. It is different from previous research which analyzed the benefits of leisure related physical activity. Furthermore, the benefit of vigorous PA was independent of a range of socioeconomic and stroke risk factors.
Although it is accepted that PA reduces the risk for stroke events, agreement about the levels of different types of PA, including frequency, intensity, and duration, has not been established because study results for the effects of PA on stroke have been inconsistent. For example, the study conducted by the Reasons for Geographic and Racial Differences in Stroke (REGARDS) reported that participation in regular moderate-to-vigorous physical activity (MVPA) reduces the risk of cardiovascular disease and stroke, which was in agreement with the results reported by Lear et al.[12] A prospective study from the Japan Public Health Center, which contained 74,913 people, confirmed that moderate-intensity PA may prevent stroke, but vigorous-intensity activity may not be beneficial or even disadvantageous for the prevention of hemorrhagic stroke.[36] However, in our study, we observed a graded effect, such that participants with vigorous-intensity PA had a lower stroke risk than participants engaging in low PA after adjusting for confounding factors. Although there was a tendency toward a lower risk of stroke in participants with moderate PA compared with that in participants with low activity, the benefit was not significantly different. This inconsistent association of stroke with PA from previous studies may be due to racial differences and differences in population and sample sizes, measurement methods, classifications of physical activity, and diagnosis of stroke. In our study, physical activity was self-reported and its assessment was based on the IPAQ which included information not only leisure time but also occupation, housework, and transportation. All these may overestimate the levels of PA compared with other research.[37] Therefore, to some extent, it might explain why there was no statistical difference in low PA group and moderate PA group. Moreover, the population distribution among the 3 different strengths of PA was uneven, wherein 15.5% participants showed low-intensity PA, 26.7% showed moderate-intensity PA, and 57.8% showed vigorous-intensity PA. Differences in population distribution in different groups might have certain of limitation for analysis of results in our study. Future studies with respect to the relationship between PA and stroke need larger sample sizes and should consider the consistency in measurement and classification methods for PA, in greater detail, to increase the reliability and accuracy of the conclusions.
To our knowledge, there were different lifestyles in different regions, these may also makes a difference in the prevalence of stroke and the distribution of PA.[38,39] PA may increase physical fitness and retain strength and muscle mass, which may reduce disease risk and benefit people.[40,41] But, differences in race, sex, age, habits, and personal health status all affect the benefit of PA in decreasing risk of stroke. Moreover, population characteristics, such as sex ratio, age, personal health status, and the percentage of smoking and drinking, were different in almost all studies. These may explain the disparities of the effects of PA on the risk of stroke observed in our study and others. There was a negative relationship between vigorous PA and the risk of stroke in our analysis, but it is weak. It might because the prevalence of stroke in Jiangxi, China was lower compared with other regions.[42,43] This is, people in south of China may need relatively high levels of physical activity to achieve the goal of reduced risk of stroke. Altogether, increased PA has benefit in reduced risk of stroke but with differing effects.[44,45]
This study has several limitations. First, it is a cross-sectional study that cannot provide causal relationships. Prospective longitudinal data are needed for future research. Second, the study participants were from Jiangxi Province, China, and hence, the generalizability of the results to other populations remains to be verified. Furthermore, only individuals aged over 45 years were selected, and although stroke is common among the elderly, it is unclear whether our results are also applicable to younger populations. Third, PA was assessed from the self-reported IPAQ responses. Imprecise reporting of the variables, at least in part, may have occurred, and an overall tendency to overestimate PA, compared with objective measurements, was inevitable, which may have masked the potential benefits occurring at lower physical activity levels than those reported here.[37] However, the reliability and validity of the IPAQ has been demonstrated by several studies from different countries.[37,46] In addition, objective measurement methods, such as accelerometers, are not cost-effective in such large sample sizes. The use of self-reported measures for assessing PA using the IPAQ is considered acceptable in large studies. Fourth, stroke was also assessed according to the self-reported questionnaire responses. The type and extent of stroke was not evaluated accurately; hence, our results are more prone to bias. Finally, although we considered demography, smoking and drinking habits, and several risk factors, such as BMI, WC, and hypertension, the influence of the potential confounding effects cannot be excluded entirely.
Despite these limitations, our study has several strengths. An important merit is the cross-sectional study design and inclusion of a large sample from the south of China, based on city-sex-age distribution, whereby the validity is better than that of studies based on hospital data; moreover, the data in our study were obtained from face-to-face interviews, which are more reliable than telephone interviews. Another strength of this study is the method used to assess PA levels. Since there are various methods to evaluate PA data, to date, there is no consensus on a criterion standard for defining levels of PA. Herein, we used a questionnaire (IPAQ version) that has been validated in several studies and for several populations and requires responses for the intensity, frequency, and duration of activity to investigate the association between PA and stroke, thus reducing the risk of misclassification or over- and under-estimation.
5. Conclusion
In conclusion, our findings demonstrated that vigorous PA, but not moderate PA, was associated with a lower risk of stroke in south of China, and this association was independent of demography and other risk factors. These findings suggest that people may get benefit from increased PA in daily life. Still, further longitudinal epidemiologic studies are needed to assess the effects between PA and stroke.
Acknowledgments
The authors acknowledge the contributions of the staff members who participated in this study as well as the study participants who shared their time with us.
Author contributions
Huihui Bao and Xiaoshu Cheng conceived the study and revised the manuscript. Xiaoshu Cheng participated in its design and coordination and helped to draft the manuscript. Juxiang Li, Ping Li, Yanqing Wu, Qinghua Wu, Zengwu Wang, Runlin Gao, Huihui Bao, Xiaoshu Cheng participated in its design, performed the statistical analysis and wrote the manuscript. Lingling Yu, Qian Liang, Lihua Hu and Wei Zhou designed and carried out the questionnaires. Lingling Yu, Qian Liang, Lihua Hu, Wei Zhou, Xiao Huang, Chunjiao You collected the samples and did the data clearance. All authors read and approved the final manuscript.
Conceptualization: Lingling Yu.
Data curation: Lingling Yu, Qian Liang, Wei Zhou, Lihua Hu, Huihui Bao.
Formal analysis: Lingling Yu, Wei Zhou, Lihua Hu.
Funding acquisition: Huihui Bao, Xiaoshu Cheng.
Investigation: Lingling Yu, Qian Liang, Xiao Huang.
Project administration: Xiao Huang.
Software: Lingling Yu, Qian Liang, Wei Zhou.
Supervision: Chunjiao You, Juxiang Li, Yanqing Wu, Ping Li, Qinghua Wu, Huihui Bao, Xiaoshu Cheng, Zengwu Wang, Runlin Gao.
Validation: Huihui Bao, Xiaoshu Cheng.
Writing – original draft: Lingling Yu.
Writing – review & editing: Lingling Yu, Huihui Bao, Xiaoshu Cheng.
Footnotes
Abbreviations: BMI = body mass index, BP = blood pressure, DBP = diastolic blood pressure, HR = heart rate, PA = physical activity, PP = pulse pressure, SBP = systolic blood pressure, WC = waist circumference.
LY is the first author.
This research was supported by the National Key R&D Program in the Twelfth Five-year Plan (No. 2011BAI11B01 and 2014ZX09303305) from the Chinese Ministry of Science and Technology, the National Natural Science Foundation of China (No. 81560051, 81460045 and 81460010), the Significant New Drug Creation (No. 2014ZX09303305) from the Project of National Science and Technology Major Project, the China Postdoctoral Science Foundation Funded Project (No. 2017M622107).
The authors report no conflicts of interest in this work.
References
- [1].Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997;349:1269–76. [DOI] [PubMed] [Google Scholar]
- [2].Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA 2011;305:2448–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247–57. [DOI] [PubMed] [Google Scholar]
- [4].Donnan GA, Fisher M, Macleod M, et al. Stroke. Lancet 2008;371:1612–23. [DOI] [PubMed] [Google Scholar]
- [5].Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the Global Burden of Ischemic and Hemorrhagic Stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology 2015;45:161–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Listed NA. Correction to: heart disease and stroke statistics-2017 update: a report From the American Heart Association. Circulation 2017;135:e646. [DOI] [PubMed] [Google Scholar]
- [7].Loprinzi PD, Addoh O. Accelerometer-determined physical activity and all-cause mortality in a National Prospective Cohort Study of Adults Post-Acute Stroke. Am J Health Promot 2018;32:24–7. [DOI] [PubMed] [Google Scholar]
- [8].Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: a report From the American Heart Association. Circulation 2016;133:e38–60. [DOI] [PubMed] [Google Scholar]
- [9].Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [DOI] [PubMed] [Google Scholar]
- [10].Chen J, Liu M, Sun D, et al. Effectiveness and neural mechanisms of home-based telerehabilitation in patients with stroke based on fMRI and DTI: A study protocol for a randomized controlled trial. Medicine (Baltimore) 2018;97:e9605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Choi JU, Kang SH. The effects of patient-centered task-oriented training on balance activities of daily living and self-efficacy following stroke. J Phys Ther Sci 2015;27:2985–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet 2017;390:2643–54. [DOI] [PubMed] [Google Scholar]
- [13].Kavouras SA, Panagiotakos DB, Pitsavos C, et al. Physical activity, obesity status, and glycemic control: The ATTICA study. Med Sci Sports Exerc 2007;39:606–11. [DOI] [PubMed] [Google Scholar]
- [14].Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 1985;100:126–31. [PMC free article] [PubMed] [Google Scholar]
- [15].Kim KJ. KHCI correlations between the sequelae of stroke and physical activity in Korean adult stroke patients. J Phys Ther Sci 2016;28:1916–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].McDonnell MN, Hillier SL, Hooker SP, et al. Physical activity frequency and risk of incident stroke in a national US study of blacks and whites. Stroke 2013;44:2519–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zhou P, Hughes AK, Grady SC, et al. Physical activity and chronic diseases among older people in a mid-size city in China: a longitudinal investigation of bipolar effects. BMC Public Health 2018;18:486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bennett DA, Du H, Clarke R, et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol 2017;2:1349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tian X, Du H, Li L, et al. Fruit consumption and physical activity in relation to all-cause and cardiovascular mortality among 70,000 Chinese adults with pre-existing vascular disease. PLos One 2017;12:e173054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Zhang Z, Hoek G, Chang LY, et al. Particulate matter air pollution, physical activity and systemic inflammation in Taiwanese adults. Int J Hyg Environ Health 2018;221:41–7. [DOI] [PubMed] [Google Scholar]
- [21].Zhou Y, Zhang R, Liu Y, et al. Association of regular physical activity with total and cause-specific mortality among middle-aged and older Chinese: a prospective cohort study. Sci Rep 2017;7:39939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wang Z, Zhang L, Chen Z, et al. Survey on prevalence of hypertension in China: background, aim, method and design. Int J Cardiol 2014;174:721–3. [DOI] [PubMed] [Google Scholar]
- [23].Bauman A, Bull F, Chey T, et al. The International Prevalence Study on Physical Activity: results from 20 countries. Int J Behav Nutr Phys Act 2009;6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Pitsavos C, Kavouras SA, Panagiotakos DB, et al. Physical activity status and acute coronary syndromes survival. J Am Coll Cardiol 2008;51:2034–9. [DOI] [PubMed] [Google Scholar]
- [25].Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. [DOI] [PubMed] [Google Scholar]
- [26].Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1081–93. [DOI] [PubMed] [Google Scholar]
- [27].Lenfant C, Chobanian AV, Jones DW, et al. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension 2003;41:1178–9. [DOI] [PubMed] [Google Scholar]
- [28].Sacco RL, Elkind M, Boden-Albala B, et al. The protective effect of moderate alcohol consumption on ischemic stroke. JAMA 1999;281:53–60. [DOI] [PubMed] [Google Scholar]
- [29].Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Je Y, De Vivo I, Giovannucci E. Long-term alcohol intake and risk of endometrial cancer in the Nurses’ Health Study, 1980-2010. Br J Cancer 2014;111:186–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wang C, Li W, Yin L, et al. Comparison of healthy lifestyle behaviors among individuals with and without cardiovascular diseases from urban and rural areas in China: A cross-sectional study. PLoS One 2017;12:e181981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hou X, Lu J, Weng J, et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: a national diabetes and metabolic disorders survey. PLoS One 2013;8:e57319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Liu LS. [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011;39:579–615. [PubMed] [Google Scholar]
- [34].Li LM, Rao KQ, Kong LZ, et al. A description on the Chinese national nutrition and health survey in 2002. Zhonghua Liu Xing Bing Xue Za Zhi 2005;26:478–84. [PubMed] [Google Scholar]
- [35].Puri R, Nissen SE, Shao M, et al. Antiatherosclerotic effects of long-term maximally intensive statin therapy after acute coronary syndrome: insights from Study of Coronary Atheroma by Intravascular Ultrasound: effect of rosuvastatin versus atorvastatin. Arterioscler Thromb Vasc Biol 2014;34:2465–72. [DOI] [PubMed] [Google Scholar]
- [36].Kubota Y, Iso H, Yamagishi K, et al. Daily total physical activity and incident stroke: The Japan Public Health Center-Based Prospective Study. Stroke 2017;48:1730–6. [DOI] [PubMed] [Google Scholar]
- [37].Lee PH, Macfarlane DJ, Lam TH, et al. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act 2011;8:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Chiuve SE, Rexrode KM, Spiegelman D, et al. Primary prevention of stroke by healthy lifestyle. Circulation 2008;118:947–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Tikk K, Sookthai D, Monni S, et al. Primary preventive potential for stroke by avoidance of major lifestyle risk factors: the European Prospective Investigation into Cancer and Nutrition-Heidelberg cohort. Stroke 2014;45:2041–6. [DOI] [PubMed] [Google Scholar]
- [40].Meijer EP, Westerterp KR, Verstappen F. The effect of exercise training on total daily physical activity in the elderly. Eur J Appl Physiol Occup Physiol 1999;80:16–21. [DOI] [PubMed] [Google Scholar]
- [41].Westerterp KR, Meijer GA, Janssen EM, et al. Long-term effect of physical activity on energy balance and body composition. Br J Nutr 1992;68:21–30. [DOI] [PubMed] [Google Scholar]
- [42].Yan R, Li W, Yin L, et al. Cardiovascular diseases and risk-factor burden in Urban and Rural Communities in high-, middle-, and low-income regions of China: a large community-based epidemiological study. J Am Heart Assoc 2017;6:pii: e004445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016;388:761–75. [DOI] [PubMed] [Google Scholar]
- [44].Jeong HG, Kim DY, Kang DW, et al. Physical activity frequency and the risk of stroke: A Nationwide Cohort Study in Korea. J Am Heart Assoc 2017;6:e5671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Lee Y, Kim WS, Paik NJ. Gender differences in physical activity and health-related behaviors among stroke survivors: data from the 5th Korea National Health and Nutrition Examination Survey. Top Stroke Rehabil 2017;24:381–7. [DOI] [PubMed] [Google Scholar]
- [46].Ekelund U, Sepp H, Brage S, et al. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutr 2006;9:258–65. [DOI] [PubMed] [Google Scholar]


