Abstract
Unicompartmental knee arthroplasty (UKA) is one of the effective surgical methods for the treatment of unicompartmental knee arthritis. When UKA fails, a revised surgery to total knee arthroplasty (TKA) is often necessary. The purpose of this study was to compare the clinical outcomes of revision of failed UKAs to TKAs with primary TKAs. The hypothesis was that the TKAs revised from UKAs had inferior clinical outcomes compared with primary TKAs.
This meta-analysis was conducted in accordance with the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines. Newcastle-Ottawa Scale (NOS) proposed by the Cochrane Collaboration was used for evaluating the methodological quality of the studies. PubMed, Medline, Embase, Web of Science, and the Cochrane Library were searched to identify studies that compared the revision of UKA to TKA with primary TKA. Primary outcomes included Range of motion (ROM); Knee society score (KSS); (re-)revision rate and complications. Secondary outcomes were blood loss and length of hospital stay.
A total of 8 eligible retrospective comparative studies were identified from a keyword search. Results revealed that the primary TKAs group has a better ROM (MD = −7.29, 95% CI:−14.03–0.56, P < .05), higher Knee Society Knee scores (MD = −0.54, 95% CI:−1.12–0.04, P < .05), higher Knee Society function score (MD = −0.65,95% CI:−1.25–0.06, P < .05), lower (re-)revision rate (MD = 4.15, 95% CI:2.37–7.25, P < .05) than rUKAs. There was no significant difference in postoperative complications, blood loss and length of stay between the 2 groups.
Our meta-analysis revealed that compared with primary TKAs, TKAs revised from UKAs had inferior clinical outcomes.
Keywords: meta- analysis, total knee arthroplasty (TKA), unicompartmental knee arthroplasty (UKA)
1. Introduction
Unicompartmental knee arthroplasty (UKA) is an effective surgical method for the treatment of unicompartmental knee arthritis.[1–3] Compared with total knee arthroplasty (TKA), UKA is only used to perform osteotomy, replacement of the lesion compartment, and preserves the anterior cruciate ligament as well as its normal structure. Therefore, it is associated with smaller operative trauma, better postoperative joint function and higher patient satisfaction.[4–6] As the number of UKAs rises, revisions of UKAs are also increasing. When UKA fails, a revision procedure to TKA is often necessary. In recent years, there was an increasing number of studies on failed UKAs converted to TKAs. It is still a controversy whether revision of failed UKAs to TKAs can achieve comparable clinical outcomes with that of primary TKAs. Some studies have reported that the outcomes of revision of failed UKAs to TKAs were comparable with that of primary TKAs.[7–9] However, few reports have demonstrated contrast results.[10–12] Therefore, the purpose of this study was to compare the clinical outcome of revision of failed UKAs to TKAs with primary TKAs.
2. Materials and methods
2.1. Date sources and search strategy
This meta-analysis was conducted in accordance with the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Guidelines. Ethical approval was not required for this study as reviewing of existing literatures did not involve any individual patient data. PubMed, Medline, EmBase, Web of Science, and Cochrane library databases were searched till November 2017 for comparative studies involving clinical results of revision of UKA to TKA and primary TKA. Two authors (ZW and MJH) completed the article search with the help of the librarians. The search terms include: “revision of UKA” OR “revision of unicompartmental knee replacement” OR “revision of unicondylar knee arthroplasty” OR “revision of unicondylar knee replacement” AND “primary TKA” OR “primary total knee replacement”. Then, the articles were searched by abstract and title. Publication language was limited to English. Reference lists of all eligible studies and relevant reviews were manually searched for any additional trials.
2.2. Inclusion and exclusion criteria
Selection criteria.
The criteria used by 2 authors to select studies for the current meta-analysis are listed as below.
The inclusion criteria were studies including:
-
1.
Comparative study design
-
2.
Comparison clinical outcomes between revision of UKA to TKA and primary TKA
-
3.
At least 1 post-operative outcome of interest reported.
The exclusion criteria were those studies that were:
-
1.
Case reports
-
2.
Non-comparative studies or non-human studies
-
3.
Lacking in scientific design
2.3. Study quality assessment
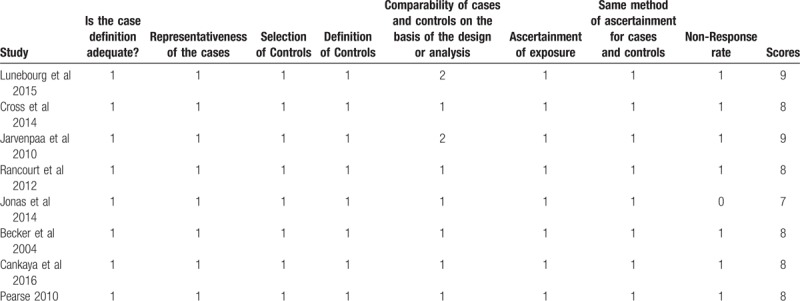
Newcastle-Ottawa scale (NOS)[13,14] proposed by the Cochrane Collaboration was used for evaluating the methodological quality of the studies by 2 authors (W.Z. and J.H.M.), and disagreement was resolved by discussion. Three domains were assessed, (selection, comparability, and outcome), with 4 categories in the selection domain, 1 category in the comparability domain, and 3 categories in the outcome domain. The total possible score was 9 points. Disagreements between the 2 authors were resolved by consensus (Table 2).
Table 2.
Newcastle-Ottawa scale.
2.4. Data extraction
All potentially eligible studies identified by searches were independently reviewed by 2 authors (W.Z. and J.H.M.). The disagreement was resolved by discussion. Data from articles that met the inclusion were abstracted independently by 2 authors (W.Z. and J.H.M.), including patient characteristics (age, sex, and other baseline characteristics), trial design, total participants and allocation, trial outcomes (Table 1). Primary outcomes included ROM, KSS score, (re-)revision rate and complications. Secondary outcomes were loss of blood and length of hospital stay.
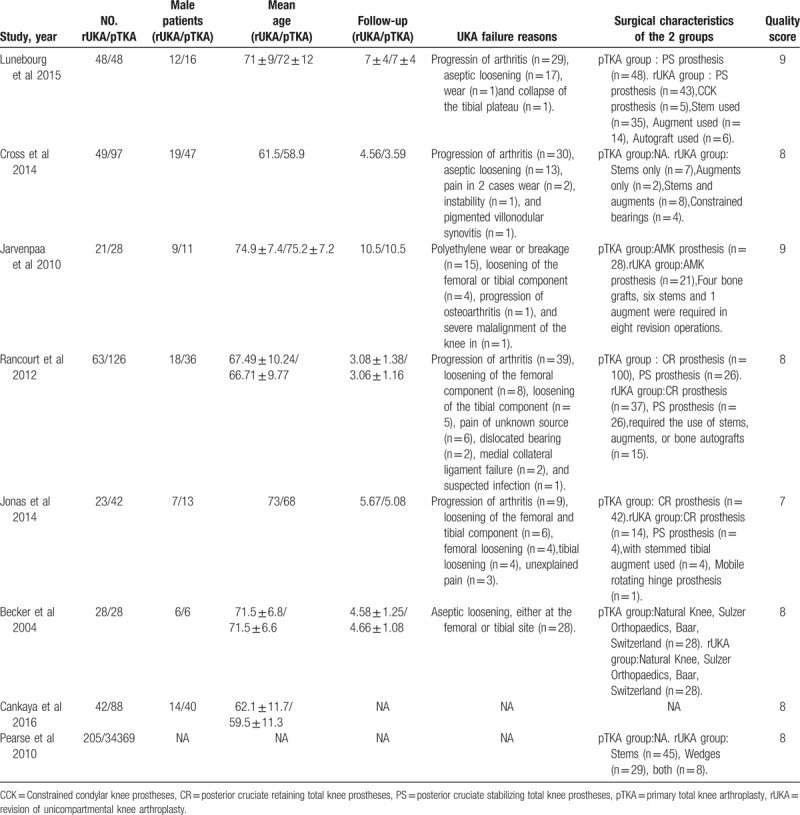
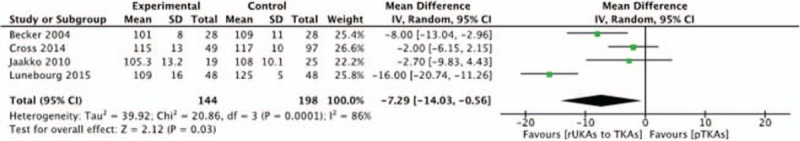
Table 1.
Characteristics of the included studies.
2.5. Statistical analysis and synthesis of results
Review Manager Software (Revman v5.3) was used to calculate experimental data from the included studies. Odds ratios with 95% confidence intervals (CI) and the mean difference (MD) with 95% CI were adopted for dichotomous and continuous outcomes respectively. Publication bias may exist due to the limited number of included studies. Thus, the random effect model was used for meta-analysis as it includes the heterogeneity of data, and can also provide a relatively conservative overall evaluation. In the Cochrane guide, the asymmetry expression of funnel plot suggests the existence of publication bias. However, due to the limited number of the included studies, it is impracticable to use the funnel plot in our study. In addition, owing to the insufficient number of extracted data, subgroup analysis cannot be implemented, either. Sensitivity analysis was carried out to explore the impact of an individual study by deleting 1 study each time.
2.6. Investigation of heterogeneity
Heterogeneity among the trials was estimated by Q statistics and I2. The value of I2 statistic represents that the extent of variation is due to heterogeneity instead of chance. If I2 > 50%, it means that substantial heterogeneity exists. Therefore, a random effect model was used to assess the outcome. If the substantial heterogeneity still exist, the subgroup analysis was used to interpret the potential source of heterogeneity. Considering the importance of inconsistency depends on several factors, therefore, interpreting the threshold of I2 may be misleading. I2 < 50% and P value > .1 represent that the heterogeneity may not be important and a fixed effect model was used to evaluate the outcome (Figs. 1–8).
Figure 1.
Forest plot analysis of range of motion (ROM).
Figure 8.
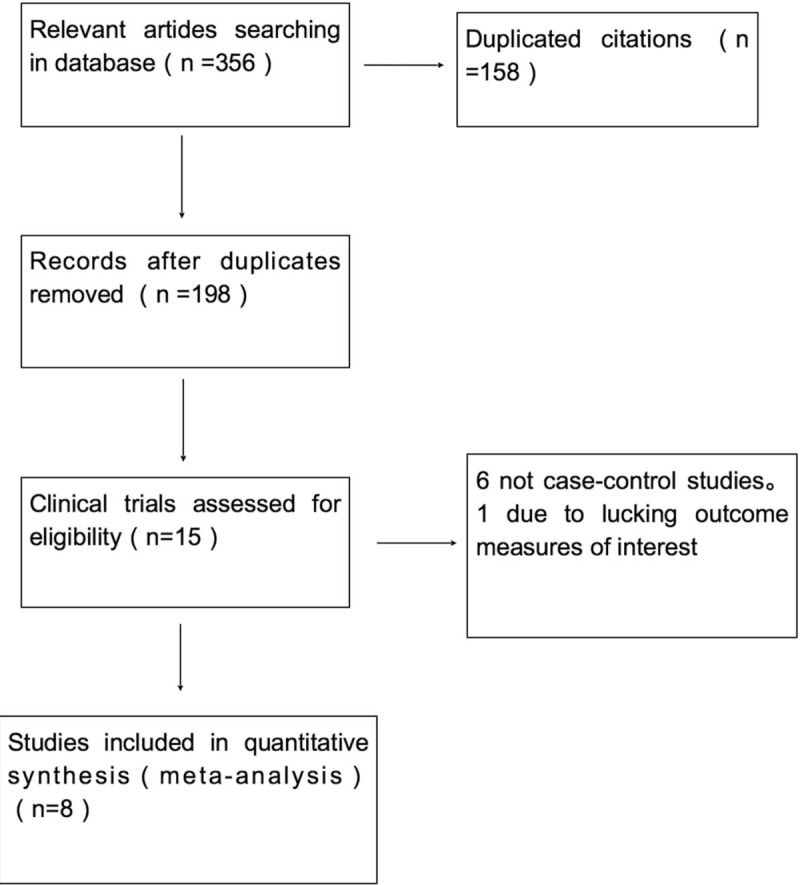
Flow chart of the literature search.
Figure 2.
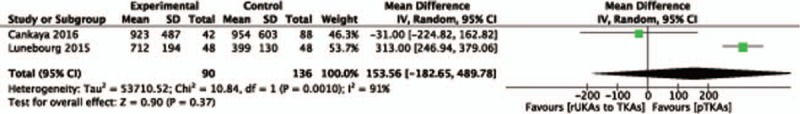
Forest plot analysis of blood loss.
Figure 3.
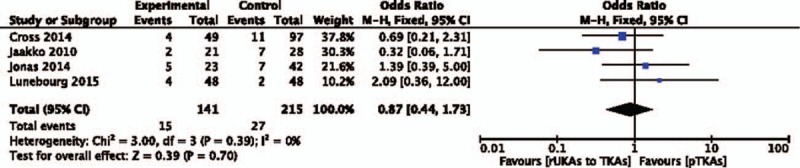
Forest plot analysis of complications.
Figure 4.
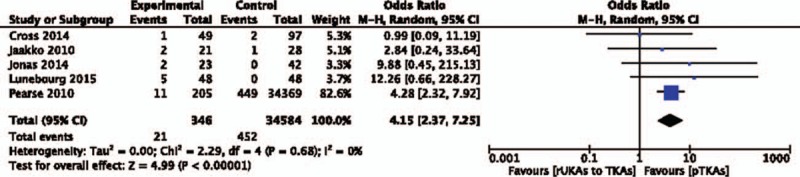
Forest plot analysis of (Re-)Revision rate.
Figure 5.
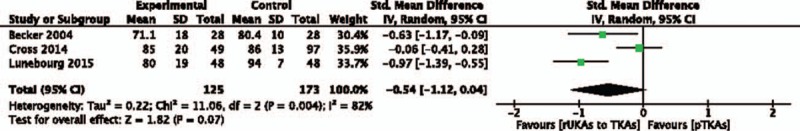
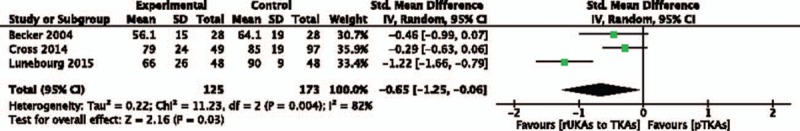
Forest plot analysis of Knee Society Knee score.
Figure 6.
Forest plot analysis of Knee Society function score.
Figure 7.
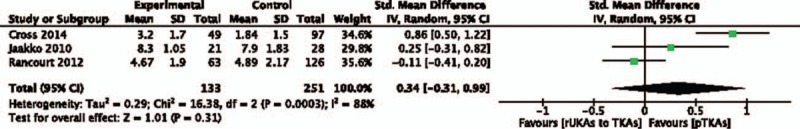
Forest plot analysis of Length of stay.
2.7. Dealing with missing data
When the data of included studies were incomplete, we contacted the authors to acquire the integrated information. The extracted data were presented as the form of mean ± standard deviation (SD) in this meta-analysis. According to the Cochrane Handbook for Systematic Reviews, when the extracted data were presented as median and interquartile range (IQR), we assumed that the median was equivalent to the mean and that the width of the IQR was equivalent to 1.35 times the SD. If the data were presented in a figure, Get Data software was used to estimated means ± SD.
3. Results
-
1.
Search results: The literature search identified 356 studies in total and 158 of them were excluded due to duplication. After reading the titles and abstracts, 15 studies were screened out. Having read the abstracts and full text articles, we further excluded 6 studies due to ineligibility and 1 study lacked the outcome measures of interest.[11,15–21] Finally, there were 8 eligible studies with a total of 731 patients from case control studies and 34,574 patients from the New Zealand Joint Registry for data extraction and meta-analysis.
-
2.
Range of motion (ROM): Four studies (N = 342) provided the postoperative ROM data. Results revealed that pTKA group had a better ROM than rUKA to TKA group (MD = −7.29, 95% CI:−14.03–0.56, P < .05).
-
3.
(Re-)Revision rate: Five studies (N = 34,930) provided the (re-)revision rate data. Meta-analysis results revealed that rUKA group had a higher (re-)revision rate than that of pTKA group (MD = 4.15, 95% CI:2.37–7.25, P < .05).
-
4.
Knee Society Knee score: Three studies (N = 298) provided Knee Society Knee score data. Results revealed that rUKA group had a lower Knee Society Knee score than that of pTKA group (MD = −0.54,95% CI:−1.12–0.04, P < .05).
-
5.
Knee Society function score: Three studies (N = 298) provided Knee Society function score data. Results revealed that rUKA group had a lower Knee Society Knee score than that of pTKA group (MD = −0.65, 95% CI:−1.25–0.06, P < .05).
-
6.
Blood loss: Two studies (N = 226) provided blood loss data. The results of this meta-analysis revealed there is no significant difference between revision of UKAs to TKAs group and pTKA group (MD = 153.36, 95% CI:−182.65–489.78, P = .37).
-
7.
Length of stay and complications: There was no significant difference in the postoperative complications (MD = 0.87, 95% CI:0.44–1.73, P = .7) and length of stay (MD = 0.34, 95% CI:−0.31–0.99, P = .31) between the 2 groups.
4. Discussion
Our meta-analysis revealed that compared with revision of UKAs to TKAs, primary TKAs had a better postoperative ROM, lower (re-)revision rate and better KSS score. There was no significant difference in postoperative complications, blood loss and length of stay between the 2 groups.
For the postoperative (re-)revision rate, results of this meta-analysis revealed that the revision rate of failed UKAs to TKAs was significantly higher than that of the primary TKAs. Data from the New Zealand National Joint Registry revealed that UKAs converted to TKAs had a revision rate of 4 times higher than that of primary TKAs.[15] Data from the Swedish National Joint Registry revealed that the rate of revision of UKAs converted to TKAs in 5 years was 7%, which was 2 times higher than that of primary TKAs.[22] Data from the Australian joint registration center revealed that the rate of revision of UKAs converted to TKAs in 3 years was 10%, which was >2 times higher than that of the primary TKAs. The main reason for the revision was aseptic loosening, with an estimated rate of 46% after UKAs converted to TKAs.[23,24] Lunebourg study revealed that the revision rate of revised UKA group at 5 and 10 years was 7% and 15%, respectively. The results were significantly higher than that of the primary TKA group and close to that of the revision of TKA group.[16] To summarize, the revision rate of revised UKAs to TKAs was significantly higher than that of pTKA.
The controversy about the complexity of UKA conversion to TKA still persists. According to the reported studies, the utilization rate of stem was 2% to 72% and the utilization rate of augment was 3% to 31% in the revision of failed UKAs to TKAs.[5,13,25–30] According to Berend et al,[14] the difficulty of revision of UKAs to TKAs and the use of revision prosthesis are related to UKA failure. When revision occurred due to the progression of arthritis, there was no requirement for stems and augments. In this view, Johnathan et al[31] and Rancourt et al[17] have put forwarded a different opinion. A retrospective matched study of Rancourt et al[17] revealed that 61.9% of the UKAs underwent revision for progression of arthritis, and more than half of them required stems, augments, and/or grafts. Furthermore, the bone defects during the revision of failed UKAs are important factors that affect the difficulty of the operation and clinical effect of the patients postoperatively. Two recent studies pointed out that the tibial bone defects were the common problems during the revision of failed UKAs to TKAs, and stems, augments, bone grafts and thicker polyethylene were often required to solve this problem. This in turn significantly increases the difficulty of the operation, with inferior clinical outcomes compared to primary TKAs.[32,33] Sarraf et al[34] predicted that bone defects during the revision of failed UKAs to TKAs might be due to polyethylene thickness. The authors mentioned that the use of polyethylene thickness as a surrogate for tibial bone loss without considering the preservation of joint line, ligamentous stability and use of augments leading to inaccuracy. However, authors believed that large sample data from the UK National Joint Registry can help to reduce the errors caused by these factors. Their statistical results revealed that the average thickness of polyethylene during revision of failed UKAs to TKAs group and primary TKAs group were 12.79 mm and 10.43 mm, respectively, reflecting the degree of tibial bone defects. In addition, the case control study of Becker[18] revealed that the average polyethylene thickness of the revision of failed UKAs to TKAs group and primary TKAs group were 12.4 + 3 mm and 10.3 + 3 mm, which was close to the data of the registry. In summary, the use of stems, augments, grafts and bone defects are important factors affecting the complexity of revision of a failed UKA to TKA.
Results of this meta-analysis revealed that the KSS scores of primary TKA group were better than that of the revision of UKAs to TKAs group. This may be due to the complexity of operation, greater trauma of operation, more bleeding volume and use of revision prosthesis. This meta-analysis revealed that there was no statistical difference in postoperative complications between the 2 groups. Postoperative complications were the common complications observed after joint arthroplasty, such as wound infection, delayed wound healing, venous thrombosis of the lower limbs, etc. For the amount of bleeding, results revealed no significant difference between the 2 groups. But due to insufficient data, a high-quality and large-scale clinical trials are needed to confirm these findings in future. There was no significant difference in the length of stay between the 2 groups. ROM is an important clinical index for joint function recovery after joint replacement. This meta-analysis revealed that the primary TKA group had better ROM than that of the revised UKAs to TKAs group.
5. Limitations
Firstly, the studies included were only in English in our study, but few studies written in other languages have been missed out. Secondly, the results of the included studies are scattered, limiting the amount of data that can be extracted. Finally, some effective indicators, such as imaging follow-up results, average cost, operation time, polyethylene thickness and other data cannot be extracted, which limited the comprehensiveness of the results. The advantages of this study are clinically instructive and provide a reference for the treatment of clinical cases.
6. Conclusion
Our meta-analysis revealed that compared with primary TKAs, TKAs revised from UKAs had inferior clinical effects in terms of worse postoperative ROM, higher (re-)revision rate, and worse KSS scores. As for the postoperative complications, blood loss and length of stay, there was no more significant difference between the 2 groups.
In summary, the outcome of failed UKAs revision is not as optimistic as expected. The key factors influencing the operation complexity and postoperative clinical effect are the type of UKA prosthesis, mode of failure, bone defect as well as surgical technique. Therefore, it is suggested that before undergoing the revision surgery, each patient should be fully evaluated and prepared on a case by case basis.
Author contributions
Conceptualization: Zhaohui Liu and Weiguo Wang.
Data curation: Wei Zuo and Jinhui Ma.
Formal analysis: Wei Zuo.
Investigation: Wei Zuo.
Methodology: Wei Zuo and Qidong Zhang.
Software: Wei Zuo.
Writing – original draft: Wei Zuo.
Writing – review & editing: WanShou Guo.
Footnotes
Abbreviations: CI = confidence intervals, KSS = knee society score, MD = mean difference, MOOSE = Meta-analysis Of Observational Studies in Epidemiology, NOS = Newcastle-Ottawa Scale, ROM = range of motion, TKA = total knee arthroplasty, UKA = unicompartmental knee arthroplasty.
Zuo Wei and Jinhui Ma Joint first authors.
This article was supported by the National Natural Science Foundation of China (grant number 81673776), and the fund receiver is the corresponding author of this article.
The authors of this work have nothing to disclose.
References
- [1].Jr ER, Higgins LL. Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am Vol 2008;90:118–22. [DOI] [PubMed] [Google Scholar]
- [2].Berger RA, Meneghini RM, Jacobs JJ, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am Vol 2005;87:999–1006. [DOI] [PubMed] [Google Scholar]
- [3].Argenson JN, Chevrol-Benkeddache Y, Berger JMAT Modern unicompartmental knee arthroplasty with cement. J Bone Joint Surg - Series A 2013;95:905–9. [Google Scholar]
- [4].Newman JH, Pydisetty RV, Ackroyd CE. Unicompartmental or totak knee replacement. The 15-year results of a prospective randomised controlled trial. Bone Joint J 2009;91:52–7. [DOI] [PubMed] [Google Scholar]
- [5].Saldanha KAN, Keys GW, Svard UCG, et al. Revision of Oxford medial unicompartmental knee arthroplasty to total knee arthroplasty — results of a multicentre study. Knee 2007;14:275–9. [DOI] [PubMed] [Google Scholar]
- [6].Lombardi AV, Berend KR, Walter CA, et al. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 2009;467:1450–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Engh GA. Orthopaedic crossfire –can we justify unicondylar arthroplasty as a temporizing procedure? In the affirmative. J Arthroplasty 2002;17:54–5. [DOI] [PubMed] [Google Scholar]
- [8].Miller M, Benjamin JB, Marson B, et al. The effect of implant constraint on results of conversion of unicompartmental knee arthroplasty to total knee arthroplasty. Orthopedics 2002;25:1353. [DOI] [PubMed] [Google Scholar]
- [9].Levine WN, Ozuna RM, Scott RD, et al. Conversion of failed modern unicompartmental arthroplasty to total knee arthroplasty. J Arthroplasty 1996;11:797–801. [DOI] [PubMed] [Google Scholar]
- [10].Oduwole KO, Sayana MK, Onayemi F, et al. Analysis of revision procedures for failed unicondylar knee replacement. Ir J Med Sci 2010;179:361–4. [DOI] [PubMed] [Google Scholar]
- [11].Järvenpää J, Kettunen J, Miettinen H, et al. The clinical outcome of revision knee replacement after unicompartmental knee arthroplasty versus primary total knee arthroplasty: 8-17 years follow-up study of 49 patients. Int Orthop 2010;34:649–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Manson TT, Kelly NH, Lipman JD, et al. Unicondylar knee retrieval analysis. J Arthroplasty 2010;25:108–11. [DOI] [PubMed] [Google Scholar]
- [13].Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am Vol 1991;73:186–90. [PubMed] [Google Scholar]
- [14].Berend KR, George J, Jr, L.A. Unicompartmental knee arthroplasty to total knee arthroplasty conversion: assuring a primary outcome. Orthopedics 2009;32:684–1684. [DOI] [PubMed] [Google Scholar]
- [15].Pearse AJ, Hooper GJ, Rothwell A, et al. Survival and functional outcome after revision of a unicompartmental to a total knee replacement: the New Zealand National Joint Registry. J Bone Joint Surg Br 2010;92:508–12. [DOI] [PubMed] [Google Scholar]
- [16].Lunebourg A, Parratte S, Ollivier M, et al. Are revisions of unicompartmental knee arthroplasties more like a primary or revision TKA? J Arthroplasty 2015;30:1985–9. [DOI] [PubMed] [Google Scholar]
- [17].Rancourt MF, Kemp KA, Plamondon SM, et al. Unicompartmental knee arthroplasties revised to total knee arthroplasties compared with primary total knee arthroplasties. J Arthroplasty 2012;27:106–10. [DOI] [PubMed] [Google Scholar]
- [18].Becker R, John M, Neumann WH. Clinical outcomes in the revision of unicondylar arthoplasties to bicondylar arthroplasties. A matched-pair study. Arch Orthop Trauma Surg 2004;124:702–7. [DOI] [PubMed] [Google Scholar]
- [19].Cross MB, Yi PY, Moric M, et al. Revising an HTO or UKA to TKA: is it more like a primary TKA or a revision TKA? J Arthroplasty 2014;29:229–31. [DOI] [PubMed] [Google Scholar]
- [20].Jonas SC, Shah R, Mitra A, et al. 5-year cost/benefit analysis of revision of failed unicompartmental knee replacements (UKRs); not “just” a primary total knee replacement (TKR). Knee 2014;21:840–2. [DOI] [PubMed] [Google Scholar]
- [21].Cankaya D, Della Valle CJ. blood loss and transfusion rates in the revision of unicompartmental knee arthroplasty to total knee arthroplasty are similar to those of primary total knee arthroplasty but are lower compared with the revision total knee arthroplasty. J Arthroplasty 2016;31:339. [DOI] [PubMed] [Google Scholar]
- [22].Lewold S, Robertsson O, Knutson K, et al. Revision of unicompartmental knee arthroplasty: outcome in 1135 cases from the Swedish knee arthroplasty study. Acta Orthop Scand 1998;69:469. [DOI] [PubMed] [Google Scholar]
- [23].Hang JR, Stanford TE, Graves SE, et al. Outcome of revision of unicompartmental knee replacement. Acta Orthop 2010;81:95–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Leta TH, Lygre SHL, Skredderstuen A, et al. Outcomes of unicompartmental knee arthroplasty after aseptic revision to total knee arthroplasty. J Bone Joint Surg Am Vol 2016;98:431–40. [DOI] [PubMed] [Google Scholar]
- [25].Johnson S, Jones P, Newman JH. The survivorship and results of total knee replacements converted from unicompartmental knee replacements. Knee 2007;14:154–7. [DOI] [PubMed] [Google Scholar]
- [26].Mcauley JP, Engh GA, Ammeen DJ. Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res 2001;19:279–82. [DOI] [PubMed] [Google Scholar]
- [27].Barrett WP, Scott RD. Revision of failed unicondylar unicompartmental knee arthroplasty. J Bone Joint Surg Am Vol 1987;69:1328–35. [PubMed] [Google Scholar]
- [28].Springer BD, Scott RD, Thornhill TS. Conversion of failed unicompartmental knee arthroplasty to TKA. Clin Orthop Relat Res 2006;446:214–20. [DOI] [PubMed] [Google Scholar]
- [29].Châtain F, Richard A, Deschamps G, et al. [Revision total knee arthroplasty after unicompartmental femorotibial prosthesis: 54 cases]. Rev Chir Orthop Reparatrice Appar Mot 2004;90:49–57. [DOI] [PubMed] [Google Scholar]
- [30].Sierra Rafael J, Kassel Cale A, Wetters Nathan G, et al. Revision of unicompartmental arthroplasty to total knee arthroplasty: not always a slam dunk!. J Arthroplasty 2013;28:128–32. [DOI] [PubMed] [Google Scholar]
- [31].Craik JD, El Shafie SA, Singh VK, et al. Revision of unicompartmental knee arthroplasty versus primary total knee arthroplasty. J Arthroplasty 2015;30:592–4. [DOI] [PubMed] [Google Scholar]
- [32].Chou DT, Swamy GN, Lewis JR, et al. Revision of failed unicompartmental knee replacement to total knee replacement. Knee 2012;19:356–9. [DOI] [PubMed] [Google Scholar]
- [33].Jones HW, Chan W, Harrison T, et al. Revision of medial Oxford unicompartmental knee replacement to a total knee replacement: similar to a primary? Knee 2012;19:339–43. [DOI] [PubMed] [Google Scholar]
- [34].Sarraf KM, Sujith K, Pastides PS, et al. Bone loss during revision of unicompartmental to total knee arthroplasty: an analysis of implanted polyethylene thickness from the national joint registry data. J Arthroplasty 2013;28:1571–4. [DOI] [PubMed] [Google Scholar]


