Abstract
Rationale:
Hepatic leiomyosarcoma is a rare malignant tumor, and in rare instances, its combination with fever may lead to misdiagnosis of liver abscess. In our case, the presence of the tumor was considered by the presence of blood vessels through the observation of hepatic tumor wall.
Patient concerns:
A 38-year-old woman who had been diagnosed with a liver abscess in a local hospital consulted our institution by complaining left upper quadrant pain and fever. The diagnosis was questioned in our workup, since no obvious inflammatory marker was found in the circulation, and contrast-enhanced computed tomography revealed a huge thick-walled mass in the right liver with multiple tortuous vessels within the wall.
Diagnosis:
Imaging revealed a neoplastic lesion rather than liver abscess. The enhancement of the solid tumor tissues was reduced during the portal phase and delayed phase, which was consistent with a wash-out enhancement. The histopathologic and immunohistochemical results confirmed the diagnosis was primary hepatic leiomyosarcoma. A pulmonary nodule during the postoperative follow-up was diagnosed as metastatic leiomyosarcoma tumor through surgery.
Interventions:
A right hepatectomy was performed to cure the hepatic mass. In the follow-up, a metastatic tumor in the lung was resected, followed by chemotherapy.
Outcomes:
Lung metastasis and liver recurrence occurred at 25 and 39 months after liver surgery, respectively. Then the patient was lost to follow-up.
Lessons:
Leiomyosarcoma is associated with a dismal prognosis, but outcomes for these patients may be improved by the combined surgical resection and chemotherapy.
Keywords: abscess, imaging, leiomyosarcoma, liver
1. Introduction
Leiomyosarcomas are the 2nd most common type of sarcoma in the abdomen. They frequently originate from veins, such as the inferior vena cava, but are rarely seen in the liver.[1] Moreover, hepatic sarcomas are also rare and account for <1% of malignant liver tumors.[2] Unlike the common hepatocellular carcinoma (HCC) that originate in hepatocytes, hepatic leiomyosarcomas derive from smooth muscle cells in hepatic vessels, bile ducts, or ligaments.[3]
Patients with fever, right upper abdominal pain, and cystic masses in the hepatic region are generally suspected of having liver abscesses during their initial clinical workup. Under rare conditions, fever is the major symptom of primary hepatic leiomyosarcoma. Here we report the case of a middle-aged woman with a primary hepatic leiomyosarcoma that presented as with fever and a thick-walled mass.
2. Case report
A 38-year-old female with a chief complaint of dull pain in the right upper abdomen and a fever of 37.9°C presented to a local hospital. An abdominal ultrasound examination showed a huge mass of the right lobe of the liver, which was interpreted as an abscess. The patient was transferred to our hospital for further evaluation and treatment. Routine blood tests after admission revealed a direct bilirubin level (5 mmol/L) at the upper limit of normal, with an unremarkable neutrophil count and remaining liver function tests. Tumor markers, including alpha-fetoprotein (AFP), carbohydrate antigen 19-9 (CA19-9), and carcinoembryonic antigen (CEA), were all within normal ranges. The physical examination suggested slight tenderness in the right upper quadrant and no rebound tenderness.
To further evaluate the lesion, both noncontrast and contrast-enhanced computed tomography (CT) scans were performed that revealed a cystic mass (10.4 × 13.6 cm2) in the right lobe of the liver, with a liquid density in the center. A contrast-enhanced CT scan showed enhancement of the wall of the lesion with multiple tortuous vessels revealed during the arterial phase, with a decreased degree of enhancement, presenting as a relative hypodensity during the portal and delayed phases. No enhancement was observed in the cystic area of the mass (Fig. 1). Considering the possibility of a liver tumor, we performed an expanded right hemi-hepatectomy. During the surgery, it was found that the liver was enlarged with good texture but had a huge mass protruding to the surface in the right lobe. No obvious abnormalities were found in any of the other abdominal organs. Intraoperative bleeding was estimated at 1500 mL. The patient's vital signs were stabilized using supplement fluid and transfusion of 6 U of red blood cells.
Figure 1.
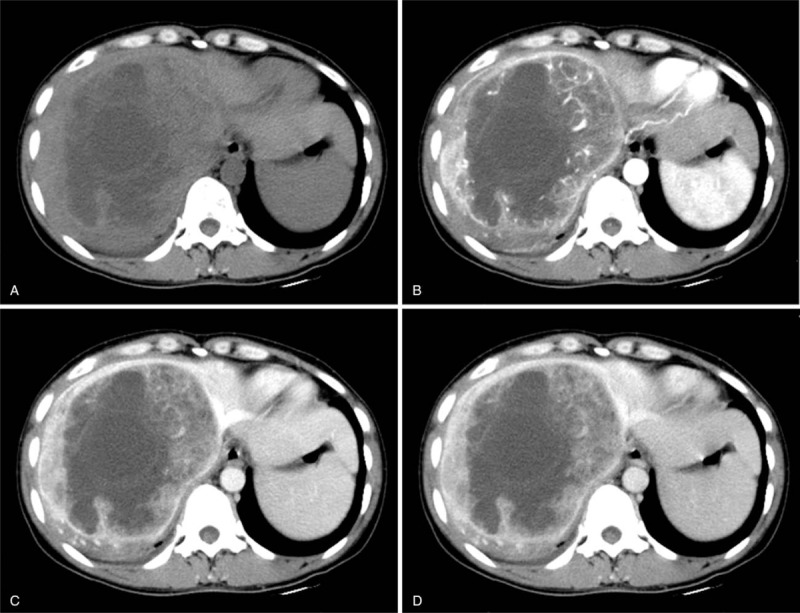
(A) Nonenhanced computed tomography (CT) scan showing a large heterogeneous tumor of the right liver with ill-defined edges. A contrast-enhanced CT scan indicated significant heterogeneous enhancement of the mass, with multiple wrapped vessels within the wall during the arterial phase (B). The enhancement of solid components decreased during the portal venous phase (C) and delayed phase (D). The unenhanced region of the tumor was confirmed to be necrosis.
A large amount of necrosis and hematoma was found in the liver mass. Microscopic examination of the resected tumor indicated that uniform sized spindle-shaped tumor cells were present in nest-like patterns with patchy infiltration, regional hemorrhage and necrosis. Immunohistochemical results revealed VM(+), SMA(+), CD99 (small amounts +), CK(−), AFP(−), HEP(−), CD117(−), and EMA(−) findings (Fig. 2). The pathology diagnosis was primary hepatic leiomyosarcoma. At 25 months after the initial surgery, the patient underwent a left lower wedge resection of the lung for enlargement of a left lower pulmonary nodule, which was highly suspicious for tumor. The surgical pathology evaluation indicated that the pulmonary nodule was a metastatic leiomyosarcoma. Subsequently, the patient underwent four courses of GD (gemcitabine and docetaxel) chemotherapy. At the 39th postoperative month, the patient developed hepatic tumor recurrence. Unfortunately, the patient was then lost to follow-up and no further outcome information is available.
Figure 2.
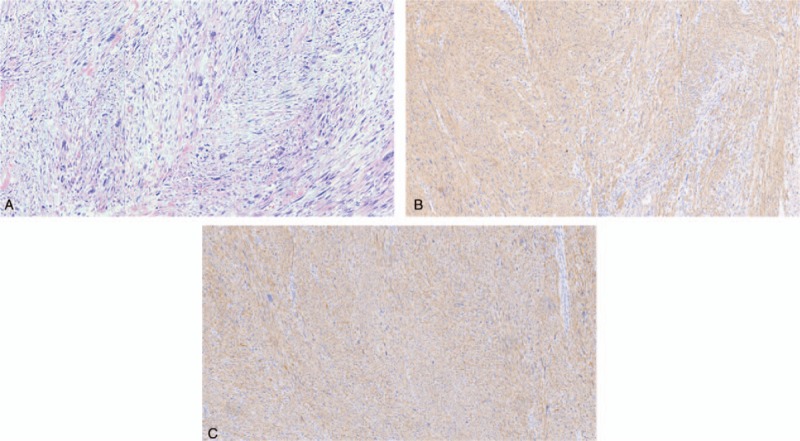
(A) The tumor consisted of uniformly sized spindle-shaped neoplastic cells. Heterogeneous nuclei and multinucleated giant cells were found (hematoxylin and eosin, ×100). Immunohistochemistry-indicated leiomyosarcoma cells were VM+ (B) and SMA+ (C) (×100).
3. Discussion
Hepatic leiomyosarcoma patients show common symptoms of abdominal pain, weight loss, appetite loss, and weakness,[3–8] and uncommon symptoms of fever, abdominal distension, back pain, and jaundice.[4,5,9,10] Hepatic leiomyosarcoma originating from the hepatic vein may lead to the Budd–Chiari syndrome owing to the obvious space-occupying effect of large tumors.[6] Nonetheless, for small tumors, hepatic leiomyosarcomas may be asymptomatic in clinic.[5,11] A swollen liver or hepatic mass can frequently be palpable in hepatic leiomyosarcoma patients during physical examination.[5] Meanwhile, the ages upon tumor detection broadly range from 5 months to 86 years old, with the average about 58 years.[5,10,12–17] No obvious gender difference is observed in tumor incidence, despite the slightly higher male morbidity.[5] In our case, the middle-aged hepatic leiomyosarcoma woman presented abdominal pain with fever, which was different from 2 previous fever cases (1 infant and 1 elderly woman). Ultrasound showed our case had a cystic thick-walled mass, which resulted in the misdiagnosis of liver abscess in the local hospital. Laboratory examinations, including liver function and plasma indexes, showed no obvious abnormality. The levels of plasma tumor markers were also within normal ranges,[3–10] except for 1 case with elevated CEA as a result of the combined colorectal cancer.[11]
The etiology of hepatic leiomyosarcoma remains unclear and reportedly can involve viral hepatitis (B and C), advanced HIV/AIDS, Hodgkin lymphoma, autosomal dominant polycystic kidney disease, kidney transplantation, or other combined tumors.[7,9,12] Moreover, hepatitis C was once hypothesized to exert the oncogenic effect, but no evidence supported the presence of the hepatitis C virus genome in these tumors.[15] Interestingly, more than half (55.4%) of the hepatic leiomyosarcoma cases were reported from America and especially Japan.[5] These regional differences in the incidence of hepatic leiomyosarcoma may be of importance for the identification of potential etiologic factors. In the case of our patient, as a previously healthy middle-aged woman she had none of the known risk factors reported above. Therefore, the pathogenesis of hepatic leiomyosarcoma requires further elucidation.
Hepatic leiomyosarcoma frequently occurs in the right lobe and is usually large in volume, with average diameters up to 14.5 cm.[5] These sizes generally lead to significant space-occupying effects. On ultrasonography, hepatic leiomyosarcomas typically are visualized as heterogeneous hypoechoic masses.[9,12] And routine CT scans of hepatic leiomyosarcomas can display either well- or ill-defined hypodense masses, that generally are necrotic and occasionally show bleeding or heterogeneous enhancement.[3,6–11,13,15,16] In rare instances, hepatic leiomyosarcomas present as cystic masses with internal or marginal solid enhancement.[12,14,16,17] Magnetic resonance imaging of the tumor may reveal lobulated masses with hypo-intensity on T1-weighted imaging, heterogeneous hyperintensities on T2-weighted imaging, high signal on diffusion-weighted imaging, heterogeneous enhancement, and occasional capsules.[5,7,9] Hepatic leiomyosarcomas have characteristically high metabolism on positron emission tomography.[5,7] Typically, these tumors do not have associated lymph node metastases or distant metastases.[5,7] Hepatic leiomyosarcoma is distinguished from HCC, in that HCC is frequently associated with cirrhosis and elevated AFP, which distinguish the 2 tumors. But hepatic leiomyosarcoma, like HCC, can also present with a wash-out enhancement pattern. However, HCC also has been associated with intrahepatic metastases, portal vein emboli, and pseudo capsules. In the case of our patient, the tumor was found to be a cystic solid mass, with associated fever, which was distinguished from liver abscesses in 2 ways. First, most hepatic leiomyosarcomas lack the typical features of liver abscesses, such as intra-lesional gas and peri-lesional edema. Second, hepatic leiomyosarcomas contain obvious tortuous blood vessels that do not occur in liver abscesses. Our patient was clinically diagnosed with a liver abscess after the initial workup, but during our evaluation the abundant vessels in the tumor walls led to consideration of a neoplastic lesion. Therefore, the finding of cystic lesions with thick walls containing vascular channels may be a valuable clue to help distinguish a hepatic leiomyosarcoma from a liver abscess.
Needle biopsies can be used to obtain tissue samples for making definitive diagnoses of hepatic leiomyosarcomas, but the actions involved in taking the biopsy are linked with the risk of tumor cell implantation.[3,5,7,10,11] Hepatic leiomyosarcomas are known for having poor prognoses and short survival times because of easy recurrence and metastases.
Radical tumor resection combined with chemotherapy may improve the prognosis of hepatic leiomyosarcomas.[5,9,12] Neoadjuvant chemotherapy is occasionally utilized in individual cases and can bring a favorable prognosis.[10] Radiochemotherapy can also be applied to unresectable leiomyosarcomas, but its efficacy is uncertain.[5] Portal venous embolization is occasionally employed in unresectable tumors, so as to reduce the tumor size and spare the chance of resection for patients with hepatic leiomyosarcoma.[6] A few patients with hepatic leiomyosarcomas have been treated with liver transplantation, but without satisfactory effect.[5] In the case of our patient, the primary lesion and metastatic tumor were aggressively resected, and chemotherapy was also provided to prolong the survival time.
In conclusion, we reported a case of hepatic leiomyosarcoma with rare manifestations, similar to a liver abscess. Imaging showed tortuous vessels in the thick wall of the tumor that contributed to identifying it as a hepatic leiomyosarcoma instead of a liver abscess. Efforts should be made to maximize opportunities for radical resection of hepatic leiomyosarcomas, while the application of chemotherapy and radiotherapy also deserves further exploration.
Author contributions
Conceptualization: Wenjie Liang.
Data curation: Weihai Liu, Wenjie Liang.
Writing – original draft: Weihai Liu, Wenjie Liang.
Writing – review & editing: Weihai Liu, Wenjie Liang.
Footnotes
Abbreviations: AFP = alpha-fetoprotein, CA19-9 = carbohydrate antigen 19-9, CEA = carcinoembryonic antigen, CT = computed tomography, HCC = hepatocellular carcinoma, MRI = magnetic resonance imaging.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Levy AD, Manning MA, Miettinen MM. Soft-tissue sarcomas of the abdomen and pelvis: radiologic-pathologic features, part 2-uncommon sarcomas. Radiographics 2017;37:797–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Weitz J, Klimstra DS, Cymes K, et al. Management of primary liver sarcomas. Cancer 2007;109:1391–6. [DOI] [PubMed] [Google Scholar]
- [3].Gohrbandt AE, Hansen T, Ell C, et al. Portal vein leiomyosarcoma: a case report and review of the literature. BMC Surg 2016;16:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Shamseddine A, Faraj W, Mukherji D, et al. Unusually young age distribution of primary hepatic leiomyosarcoma: case series and review of the adult literature. World J Surg Oncol 2010;8:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chi M, Dudek AZ, Wind KP. Primary hepatic leiomyosarcoma in adults: analysis of prognostic factors. Onkologie 2012;35:210–4. [DOI] [PubMed] [Google Scholar]
- [6].Giakoustidis D, Giakoustidis A, Goulopoulos T, et al. Primary gigantic leiomyosarcoma of the liver treated with portal vein embolization and liver resection. Ann Hepatobiliary Pancreat Surg 2017;21:228–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Iida T, Maeda T, Amari Y, et al. Primary hepatic leiomyosarcoma in a patient with autosomal dominant polycystic kidney disease. CEN Case Rep 2017;6:74–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Majumder S, Dedania B, Rezaizadeh H, et al. Tumor rupture as the initial manifestation of primary hepatic leiomyosarcoma. Gastrointest Cancer Res 2014;7:33–4. [PMC free article] [PubMed] [Google Scholar]
- [9].Metta H, Corti M, Trione N, et al. Primary hepatic leiomyosarcoma - a rare neoplasm in an adult patient with AIDS: second case report and literature review. J Gastrointest Cancer 2014;45:36–9. [DOI] [PubMed] [Google Scholar]
- [10].Tsai PS, Yeh TC, Shih SL. Primary hepatic leiomyosarcoma in a 5-month-old female infant. Acta Radiol Short Rep 2013;2: 2047981613498722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Takehara K, Aoki H, Takehara Y, et al. Primary hepatic leiomyosarcoma with liver metastasis of rectal cancer. World J Gastroenterol 2012;18:5479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Shivathirthan N, Kita J, Iso Y, et al. Primary hepatic leiomyosarcoma: case report and literature review. World J Gastrointest Oncol 2011;3:148–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Giuliante F, Sarno G, Ardito F, et al. Primary hepatic leiomyosarcoma in a young man after Hodgkin's disease: diagnostic pitfalls and therapeutic challenge. Tumori 2009;95:374–7. [DOI] [PubMed] [Google Scholar]
- [14].Lee HJ, Lee JL, Choi WH. A case of primary myxoid leiomyosarcoma of the liver. Korean J Intern Med 2002;17:278–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tsuji M, Takenaka R, Kashihara T, et al. Primary hepatic leiomyosarcoma in a patient with hepatitis C virus-related liver cirrhosis. Pathol Int 2000;50:41–7. [DOI] [PubMed] [Google Scholar]
- [16].Ferrozzi F, Bova D, Zangrandi A, et al. Primary liver leiomyosarcoma: CT appearance. Abdom Imaging 1996;21:157–60. [DOI] [PubMed] [Google Scholar]
- [17].Maki HS, Hubert BC, Sajjad SM, et al. Primary hepatic leiomyosarcoma. Arch Surg 1987;122:1193–6. [DOI] [PubMed] [Google Scholar]


