Abstract
Rationale:
Adult recurrent neuroblastoma is extremely rare, especially in the posterior mediastinum and retroperitoneal cavity. The surgical treatment of this special part of the tumor is also a clinical difficulty.
Patient concerns:
This study reports a case of a 24-year-old man with a history of treated posterior mediastinal neuroblastoma. Enhanced computed tomography found a heterogeneously enhancing mass occupying the retroperitoneal and posterior mediastinum, and the initial impression was recurrent neuroblastoma.
Diagnoses:
The patient was diagnosed with recurrent neuroblastoma based on his medical history and histopathological results.
Interventions:
The young adult underwent radical resection of recurrent neuroblastoma in posterior mediastinum and retroperitoneum through thoracoabdominal incision.
Outcomes:
The young patient recovered to normal within 10 days after surgery and had no relapse for following-up 12 months.
Lessons:
Despite the difficulty of surgery, it is feasible to remove the tumor in the posterior mediastinum and retroperitoneal cavity safely.
Keywords: adult neuroblastoma, case report, computed tomography, surgery
1. Introduction
Neuroblastoma is a rare type of tumor that evolves from immature nerve cells. It not only develops in the adrenal glands but also occurs in the abdomen, chest, or nerve tissue adjacent to the spine. It is common in children aged younger than 5 years.[1,2] According to the statistics of the National Cancer Institute of the United States, the incidence of neuroblastoma in children is 1/100,000, which is relatively common in boys. There are approximately 650 newly diagnosed neuroblastoma patients each year in the United States.[3]
Nearly 20% to 50% of high-risk cases are progressive or refractory, resulting from insufficient response to induction high-dose chemotherapy.[4] In addition, recurrence after the 1st line of treatment is also common.[5]
Adult neuroblastoma is very rare; adult recurrent neuroblastoma in the posterior mediastinum and retroperitoneal cavity is extremely rare.[6] As a matter of fact, according to related literature studies, this is the 1st case around the world that has been reported. The treatment of recurrent neuroblastoma located in the posterior mediastinum and retroperitoneum remains to be further assessed. To better understand the tumor of this special part, we describe a case of a 24-year-old man diagnosed with recurrent neuroblastoma in the chest and abdomen.
2. Case presentation
A 24-year-old male patient whose medical history included neuroblastoma gets readmitted to the First Affiliated Hospital Bengbu Medical College with chief complaint of discomfort in his chest for 12 months. He was diagnosed with posterior mediastinal tumor in the Department of Thoracic Surgery, the First Affiliated Hospital of Bengbu Medical College 4 years ago. On December 28, 2013, the thoracotomy was performed, and the tumor was completely removed. Postoperative pathology proved to be a posterior mediastinal neuroblastoma. He did not receive postoperative radiotherapy and chemotherapy, and he did not take examination regularly for 4 years after surgery. The chest-enhanced CT scan during this hospital stay demonstrated that a 7-cm, moderately enhanced space-occupying lesions arised from the right posterior mediastinum and retroperitoneum, which was at the rear of the inferior vena cava (Fig. 1). Based on his medical history, the provisional diagnosis was adult recurrent neuroblastoma.
Figure 1.
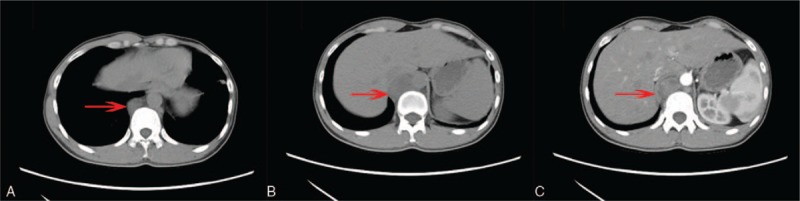
Abdominal enhanced computed CT images. (A) Nonenhanced image reveals the mass (red arrow) in the posterior mediastinum. (B) Nonenhanced image reveals the mass in the posterior mediastinum. (C) Axial enhanced image reveals the mass with heterogeneous enhancement. CT = computed tomography.
The suitable pathway for the tumor adhering to inferior vena cava in the right posterior mediastinum and posterior mediastinum is thoracoabdominal incision. He was placed at lithotomy position, and upper abdominal median incision combined with right thoracic fifth intercostal incision was made under general anesthesia (Fig. 2A). Subsequently, the abdominal and thoracic cavity was entered layer by layer with right arcus costarum being cut off. The liver round ligament, the falciform ligament, the left and right coronary ligaments and the left and right triangular ligaments were cut to fully dissociate the liver. At the same time, the right diaphragm was disconnected to completely expose the mass measuring approximately 7cm × 3cm × 2 cm, which originated from the right posterior mediastinum and extended into the retroperitoneum (Fig. 2B). The tumor was located behind the inferior vena cava, from the right posterior mediastinum to the right renal vein, which was hard, and slightly sticky with surrounding tissues. Along the edge of the tumor, the tumor was completely resected with the amount of bleeding about 200 mL. Furthermore, the chest drainage tube was routinely applied, while the abdominal drainage tube was not placed. The removal time of the thoracic drainage tube was 4 days after this operation. The incision was healed without any swelling, pyorrhea, or fissuration. No complications were encountered during the postoperative period, and the patient was discharged 6 days later. The patient refused chemotherapy or radiotherapy and had no relapse for following-up 12 months. Moreover, immunohistochemical stains for NSE, CgA, Syn, CD56, and S-100 showed positivity. The final pathological diagnosis was neuroblastoma (Fig. 3). In addition, the case report was approved by the Ethical Committee of the First Affiliated Hospital of Bengbu Medical College, and a written consent form was obtained from the patient before the publication of this study.
Figure 2.
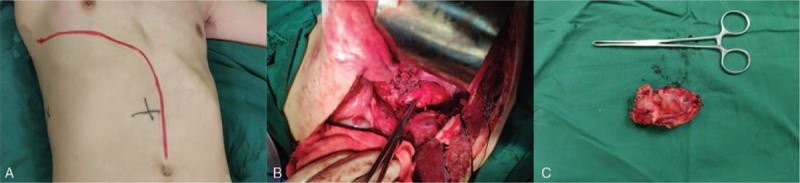
The presentation of surgical procedure. (A) Incision selection. (B) Complete tumor exposure. (C) Complete tumor resection.
Figure 3.
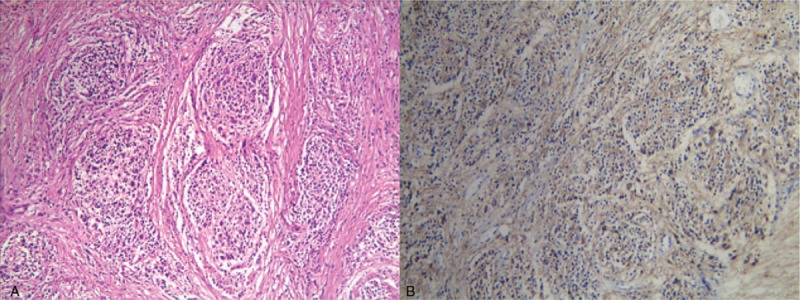
Microscopic images of the surgical specimen. (A) The tumor showed a nested organoid growth pattern (HE, ×100). (B) Immunohistochemical examinations revealed that the tumor cells were positive for Syn (×100). HE = hematoxylin and eosin.
3. Discussion
Neuroblastoma is composed of undifferentiated neuroblasts, which most frequently starts from one of the adrenal glands, but can also develop in the neck, chest, or abdomen. As far as we know, this is the 1st case of neuroblastoma occupying the posterior mediastinum and retroperitoneum. The symptoms of neuroblastoma are often vague, resulting in diagnostic difficulty. Neuroblastoma often spreads to other parts of the body before any symptoms are apparent, and 50% to 60% of all neuroblastoma cases present with metastases.[2,7]
The incidence of neuroblastoma varies by age, and most of the cases are detected in the perinatal period, followed by the steady decline in the first 10 years. Neuroblastoma rarely occurs in adolescents and young adults; however, it proves to be more fatal for them.[8–10] Although young adult neuroblastoma is rare, clinicians should not ignore neuroblastoma because the tumor is highly malignant.
Contrast-enhanced CT is an indispensable method to diagnose this disease, and it can clearly show the extent, morphology, and internal conditions of the tumor. Uneven enhancement is an obvious feature of neuroblastoma, because of its high degree of malignancy and rich blood supply. Moreover, calcification in the tumor is another characteristic of neuroblastoma. The presence of stippled calcification is seen in 85% of abdominal neuroblastoma.[11,12] In addition, CT examination can clearly show the relationship between the tumor and surrounding tissues and organs, and provide necessary imaging data for the treatment of neuroblastoma.
For adult neuroblastoma, uniform staging criteria have not been established, and the stages can only refer to the stages of neuroblastoma in children. International Neuroblastoma Risk Group Staging System stratifies neuroblastoma according to its anatomical presence at diagnosis. Our case was diagnosed with having stage 1 neuroblastoma, which was resectable. For many types of tumor, treatment depends on stages. However, it is risk groups that determine the treatment of neuroblastoma. The risk stratification is based on a child's age, cancer stage, tumor histology, and tumor biology and then the patients are divided into low-, intermediate-, and high-risk groups.[13]
Currently, there are no standard treatment guidelines for adult patients with neuroblastoma. As a result, treatment programs adapted to children have been tried for adult cases.[14] The therapies for these different risk categories are very different. Low-risk disease typically has a good outcome with surgery or simply observation. Intermediate-risk disease is treated with surgery and chemotherapy.[15] In high-risk disease, the prognosis is poor despite aggressive multimodal therapy including intensive chemotherapy, surgery, radiation therapy, stem cell transplant, differentiation agent isotretinoin (also called 13-cis-retinoic acid), and frequently immunotherapy with anti-GD2 monoclonal antibody therapy.[16]
Despite the application of 1st-line treatment, recurrence of neuroblastoma is also common.[17] According to the preoperative imaging findings, the recurrent tumor occurs only in the area where the cancer first formed (Fig. 1). Complete resection of the tumor is feasible. Postoperative chemotherapy is recommended for the patient with recurrent neuroblastoma.
Although laparoscopic technology has many advantages for patients, open surgical treatment with a curative intention is selected for this patient considering the difficulty of reoperation and the special anatomical location of the tumor.[18] Alternative surgical approaches are similar to esophagectomy performed using several methods.[19] With regard to the point of entry, we should firstly consider a transhiatial procedure, a transthoracic procedure and a thoracoabdominal precedure. There are a number of surgical options, the choice of the surgical approach depends on the characteristics and location of the tumor, and the preference of the surgeon. The best choices for particular location of the tumor remain the subject of research and discussion.
Based on the degree of neuroblast differentiation, neuroblastoma is divided into three subtypes, namely undifferentiated neuroblastoma, poorly differentiated neuroblastoma, and differentiated neuroblastoma.[14] In neuroblastoma, the amount of Schwannian stroma is associated with prognosis.[20] Our case was identified with differentiated neuroblastoma according to the histopathological and immunohistochemical results.
4. Conclusion
Although adult neuroblastoma is rare but highly malignant, clinicians should not ignore the disease. There is no uniform treatment guideline for adult neuroblastoma, and the therapeutic methods for adult need refer to a treatment plan for children with neuroblastoma. Surgery is the main treatment in the early stage, and comprehensive treatment can be performed in the late stage. Multimodal oncological treatment for adult recurrent neuroblastoma should be taken into account, followed by surgical treatment, if this is feasible. To better treat adult recurrent neuroblastoma, a large number of basic researches and clinical experiments are needed.
Acknowledgments
The authors acknowledge the support of the Department of Thoracic Surgery, the First Affiliated Hospital of Bengbu Medical College.
Author contributions
Investigation: Xiang Ma, Yunchuan Yang, Zhaoying Wang, Wanliang Sun, Dengyong Zhang.
Supervision: Binquan Wu, Hua Wu, Peiyuan Cui, Zheng Lu.
Writing – original draft: Xiang Ma, Yunchuan Yang.
Writing – review & editing: Peiyuan Cui.
Footnotes
Abbreviation: CT = computed tomography.
XM and YY contributed equally to this study.
The authors have no conflicts of interest to disclose.
References
- [1].Iehara T, Hamazaki M, Tajiri T, et al. Successful treatment of infants with localized neuroblastoma based on their MYCN status. Int J Clin Oncol 2013;18:389–95. [DOI] [PubMed] [Google Scholar]
- [2].Tolbert VP, Matthay KK. Neuroblastoma: clinical and biological approach to risk stratification and treatment. Cell Tissue Res 2018;372:195–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Eleveld TF, Oldridge DA, Bernard V, et al. Relapsed neuroblastomas show frequent RAS-MAPK pathway mutations. Nat Genet 2015;47:864–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kushner B, Kramer K, LaQuaglia M, et al. Reduction from seven to five cycles of intensive induction chemotherapy in children with high-risk neuroblastoma. J Clin Oncol 2004;22:4888–92. [DOI] [PubMed] [Google Scholar]
- [5].Ceschel S, Casotto V, Valsecchi M, et al. Survival after relapse in children with solid tumors: a follow-up study from the Italian off-therapy registry. Pediatr Blood Cancer 2006;47:560–6. [DOI] [PubMed] [Google Scholar]
- [6].Yanik F, Karamustafaoglu YA, Yoruk Y. A rare mediastinal occurrence of neuroblastoma in an adult: case report. Sao Paulo Med J 2018;0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Johnsen JI, Dyberg C, Fransson S, et al. Molecular mechanisms and therapeutic targets in neuroblastoma. Pharmacol Res 2018;131:164–76. [DOI] [PubMed] [Google Scholar]
- [8].Nakagawara A, Li YY, Izumi H, et al. Neuroblastoma. Jpn J Clin Oncol 2018;48:214–41. [DOI] [PubMed] [Google Scholar]
- [9].Esiashvili N, Goodman M, Ward K, et al. Neuroblastoma in adults: incidence and survival analysis based on SEER data. Pediatr Blood Cancer 2007;49:41–6. [DOI] [PubMed] [Google Scholar]
- [10].Franks LM, Bollen A, Seeger RC, et al. Neuroblastoma in adults and adolescents: an indolent course with poor survival. Cancer 1997;79:2028–35. [DOI] [PubMed] [Google Scholar]
- [11].Lonergan GJ, Schwab CM, Suarez ES, et al. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics 2002;22:911–34. [DOI] [PubMed] [Google Scholar]
- [12].Kembhavi SA, Shah S, Rangarajan V, et al. Imaging in neuroblastoma: An update. The Indian journal of radiology & imaging 2015;25:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Brodeur G. Neuroblastoma: biological insights into a clinical enigma. Nat Rev Cancer 2003;3:203–16. [DOI] [PubMed] [Google Scholar]
- [14].Brodeur GM, Pritchard J, Berthold F, et al. Revisions of the international criteria for neuroblastoma diagnosis, staging and response to treatment. Prog Clin Biol Res 1994;385:363–9. [PubMed] [Google Scholar]
- [15].Haase G, Perez C, Atkinson J. Current aspects of biology, risk assessment, and treatment of neuroblastoma. Semin Surg Oncol 1999;16:91–104. [DOI] [PubMed] [Google Scholar]
- [16].Fish J, Grupp S. Stem cell transplantation for neuroblastoma. Bone Marrow Transplant 2008;41:159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Pinto N, DuBois S, Marachelian A, et al. Phase I study of vorinostat in combination with isotretinoin in patients with refractory/recurrent neuroblastoma: a new approaches to Neuroblastoma Therapy (NANT) trial. Pediatr Blood Cancer 2018;65:e27023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kasai M, Cipriani F, Gayet B, et al. Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery 2018. [DOI] [PubMed] [Google Scholar]
- [19].Miyazaki T, Sakai M, Sohda M, et al. [Thoracoscopic esophagectomy]. Kyobu Geka 2014;67:773–7. [PubMed] [Google Scholar]
- [20].Zeine R, Salwen H, Peddinti R, et al. Presence of cancer-associated fibroblasts inversely correlates with Schwannian stroma in neuroblastoma tumors. Mod Pathol 2009;22:950–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


