Abstract
Background:
With the progress of surgical techniques and instruments, various minimally invasive surgical therapies were developed to treat benign prostatic hyperplasisa (BPH). However, the efficacy and safety of different transurethral procedures for the treatment of BPH are still undefined.
Method:
A systematic search was performed for all randomized controlled trials (RCTs), which compared the transurethral procedures for BPH from 1995 to 2016. The clinical baseline characteristics, International Prostate Symptom Score (IPSS), quality of life (QoL), postvoid residual (PVR), maximum flow rate (Qmax), short-term and long-term complications were analyzed using RevMan and ADDIS software.
Result:
Eighty-eight randomly controlled trials and fifteen procedures were included in the network meta-analysis. HoLEP greatly inproved PVR. TmLRP had the best efficacy in improving QoL score. Diode laser vaporization of prostate was superior in improving IPSS and Qmax. Diode laser through vaporization required the shortest time in catheterization, while Nd:YAG was the longest procedure. For the hospitalization time, TUR was the longest and HoLEP was the shortest. TmLRP was related to the lowest postoperative hemoglobin decrease. TmLEP had the least rates of occurrence of hematuria, reoperation and erectile dysfunction. HoLEP was the best choice to reduce the incidence of recatheterization, urinary retention, urinary tract infection, stress urinary incontinence and retrograde ejaculation. The complications such as blood transfusion, urethral stricture, bladder neck contracture were relatively rare in the patients who underwent diode laser vaporization of prostate.
Conclusion:
Compared with other transurethral procedures, thulium, holmium and diode lasers were associated with better efficacy and fewer complications.
Keywords: benign prostatic hyperplasisa (BPH), efficacy, transurethral procedures
1. Introduction
Benign prostate hyperplasia is a common disease among elderly men, which is the major cause of lower urinary tract symptoms (LUTS).[1] According to the statistics, 60% of men older than 60 years suffer from BPH and LUTS, which greatly decrease the quality of life.[2] Surgical treatment is often the most effective intervention.[3,4] For surgical procedures, monopolar TURP (M-TURP) was considered as “gold standard” for the treatment of BPH in the past decades, although it is associated with complications such as transurethral resection syndrome (TURS) and blood loss.[5]
With the progress of surgical techniques and development of instruments, multitudinous transurethral procedures have been invented to overcome the faultiness of M-TURP. These alternative transurethral procedures include bipolar plasmakinetic, electrovaporization, and various lasers.[6] The modalities of prostate tissue ablation include enucleation, resection, and vaporization.[7] All these available surgical treatments are widely used, and each surgical procedure has its own advantage or disadvantage. However, the efficacy and safety of different transurethral procedures for the treatment of BPH are still undefined.
Hundreds of randomized controlled trials compared these different types of transurethral procedures. However, most of them only compared 2 or 3 types of procedures. The efficacy and safety of different surgical procedures are difficult to estimate. In this study, we made a network meta-analysis to compare the efficacy and safety of different transurethral procedures for BPH.
2. Methods
2.1. Literature search strategy
A systematic search was performed for all randomized controlled trials (RCTs), which compared the transurethral procedures for BPH from 1995 to 2016. The literatures were based on the following databases: Embase, PubMed/Medline, Cochrane Library, and Scopus. The keywords included: randomized, benign prostatic hyperplasia, BPH, Thulium laser, Holmium laser, photoselective vaporization of prostate, Diode laser, Nd:YAG laser, “KTP: YAG laser, interstitial laser, monopolar transurethral resection, bipolar transurethral resection, plasmakinetic, and electrovaporization. There was no restriction on the language of the articles.
2.2. Inclusion and exclusion criteria
Inclusion criteria included: RCTs; patients diagnosed with BPH and needed surgical therapy; trials comparing different transurethral procedures for the treatment of BPH; at least one of the primary outcomes was clearly defined. Exclusion criteria included: patients with previous prostatic surgery, neurogenic bladder and urethral strictures; patients with prostatic carcinoma; open surgery, laparoscopic operation, transurethral microwave therapy, prostate stent and water induced thermotherapy; published only in abstracts; enrolled patients <40 in one trial; (6) animal experiment. This study was approved by The Ethics Committee of Cangzhou People Hospital. Participants have provided their written informed consent to participate in this study.
2.3. Data extraction
We collected the following data from these literatures: the quality of trials; clinical basic characteristics; effectiveness index, including IPSS, Qmax, PVR, and QoL scores; operating time, hospitalization and catheterization time; short-term complications-related outcomes, and long-term complications.
2.4. Quality analysis
The data abstraction and quality evaluation were performed independently by 2 reviewers (FS and JL) according to Cochrane guidelines 5.1.0 and quality-control standards set by Jada.[8] A third member (YZ) participated in the discussion when divergence appeared. The Cochrane Handbook evaluation elements include randomization, allocation concealment, blinding, incomplete outcome data, and selective reporting.[9] But blinding is impractical in clinical work. So “blinding” was cancelled in this study. The judgments were categorized as “low risk of bias,” “high risk of bias” or “unclear risk of bias.” The risk of bias of all included studies was analyzed by RevMan 5.3.0 software. In addition, there were many trials related to bipolar TURP. In fact, it represents different techniques. International Electrotechnical Commission (http://www.iec.ch), designed the bipolar as mirrored dual-loop distal consisting of active and passive electrode and both electrodes must be attached in a single-port system. The plasmakinetic system reaches the specification for bipolar TURP. Though bipolar transurethral resection in saline (TURis) is another main transurethral procedure for BPH, it does not conform to the definition of International Electrotechnical Commission. So articles related to plasmakinetic system or TURis were distinguished in our research.
2.5. Statistical analysis
We relied on PRISMA criteria and PICO methodology was used to analyze the outcomes of interest and population.[10] ADDIS 1.16.6 software was used to conduct this network meta-analysis. ADDIS is a nonprogramming software adhered to Bayesian approach, which helps us to predict the comparable estimates between indirect comparisons. By means of this software, the relative effect estimates were calculated and the procedures could be sorted from the best to the worst. We created a consistency model to combine the effect of indirect comparisons and P < . 05 was set as significant inconsistency. The results are expressed as rank probability.
3. Results
3.1. Characteristics of eligible studies
Around 1850 records were found through initial searching. Due to duplicate or nonrandomized, 1620 articles were excluded. About 88 randomly controlled trials (RCTs) in 97 articles[11–106] (11187 enrolled patients) were finally included in the network meta-analysis. Figure 1 showed the flow diagram of the search. Table 1 showed the basic characteristics of included RCTs, such as types of prostate tissue ablation, the number of patients, age, prostate size, Qmax, PVR, IPSS, QoL, and the max follow-up time. The basic characteristics of enrolled patients were substantially equal in general. Fifteen procedures were studied in this systematic review and the numbers beside the lines were the quantities of comparative trials (Fig. 2). The risk of bias was shown in Figure 3. “Blinding” was ignored in this study because it is impractical in clinical work. Overall, the quality of these studies was relatively high through the other 5 items introduced by Cochrane criterion.
Figure 1.
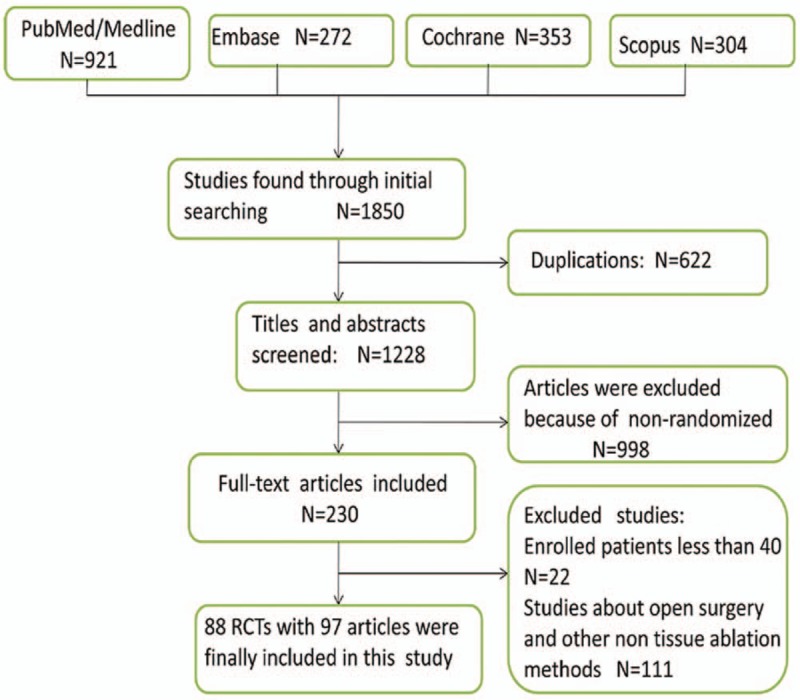
Flowchart for this network meta-analysis.
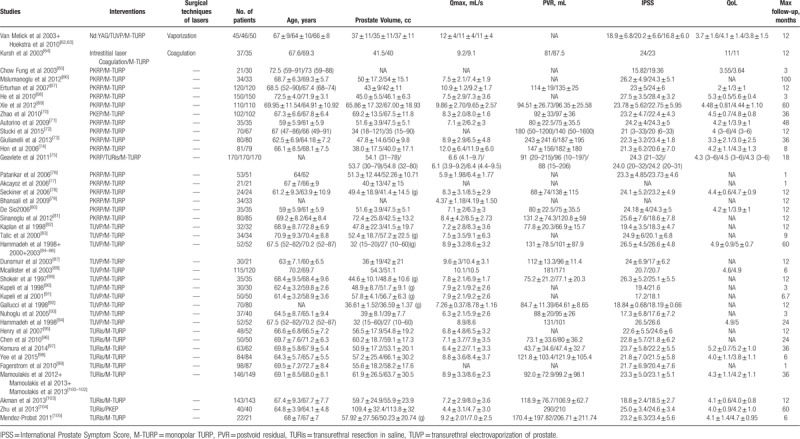
Table 1.
The basic characteristics of included randomly controlled trials.
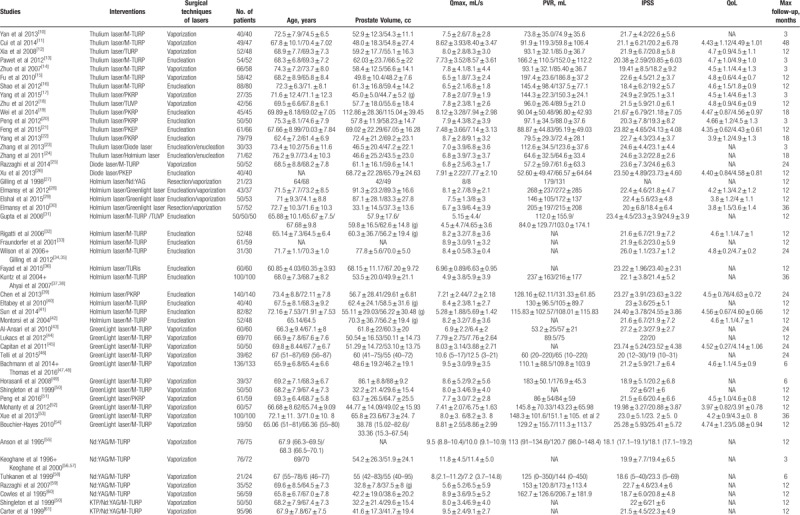
Figure 2.
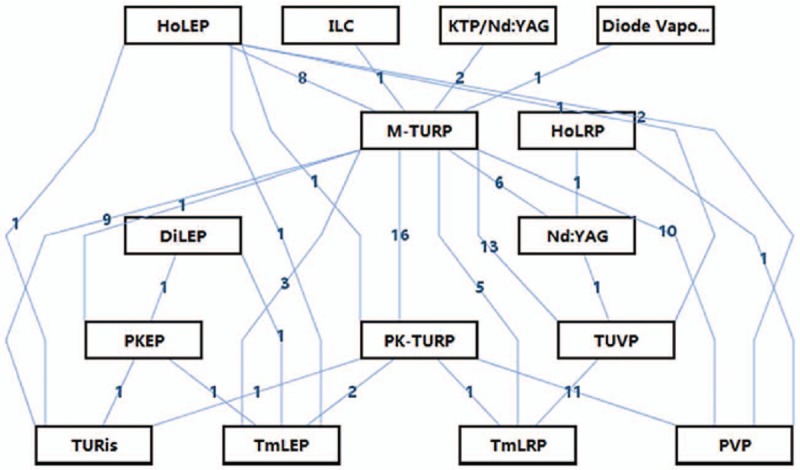
Comparison network of included trials. DiLEP = diode laser enucleation of prostate, HoLEP = holmium laser enucleation of prostate, HoLRP = holmium laser resection of prostate, ILC = Intrestitial laser coagulation, M-TURP = monopolar transurethral resection of prostate, PKEP = plasmakinetic enucleation of prostate, PKRP = plasmakinetic resection of prostate, PVP = photoselective vaporization of prostate, TmLRP = thulium laser resection of prostate, TmLEP = thulium laser enucleation of prostate, TURis = bipolar transurethral resection in saline, TUVP = transurethral electrovaporization of prostate.
Figure 3.
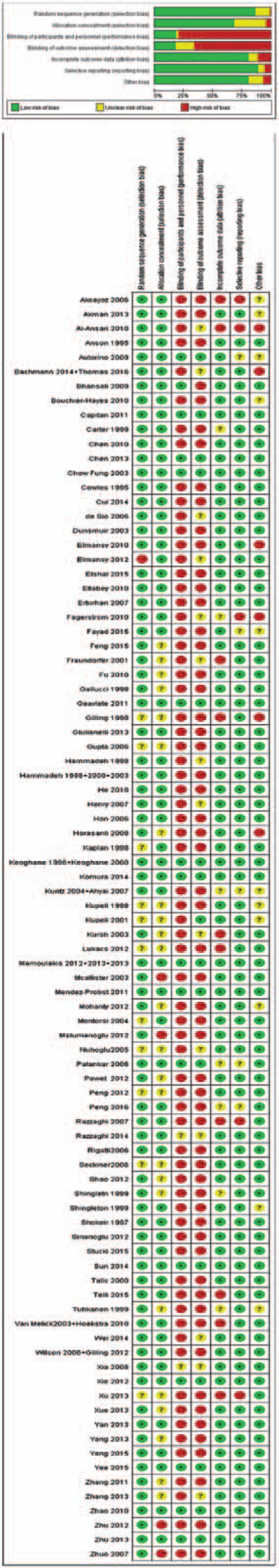
Risk of bias for selected trials.
Table 1 (Continued).
The basic characteristics of included randomly controlled trials.
Among reported trials, standard TURP (M-TURP) was the most commonly used technology, which was shown in 69 studies. The frequency of surgical energy platform from high to low was: M-TURP (69) > bipolar plasmakinetic (36) > electrovaporization (16) > thulium laser (15) = holmium laser (15) > greenlight laser (14) > TURis (12) > Nd:YAG (8) > diode laser (3) > KTP/Nd:YAG (2) > Intrestitial laser (1). The main modalities of tissue ablation include enucleation, resection, and vaporization.
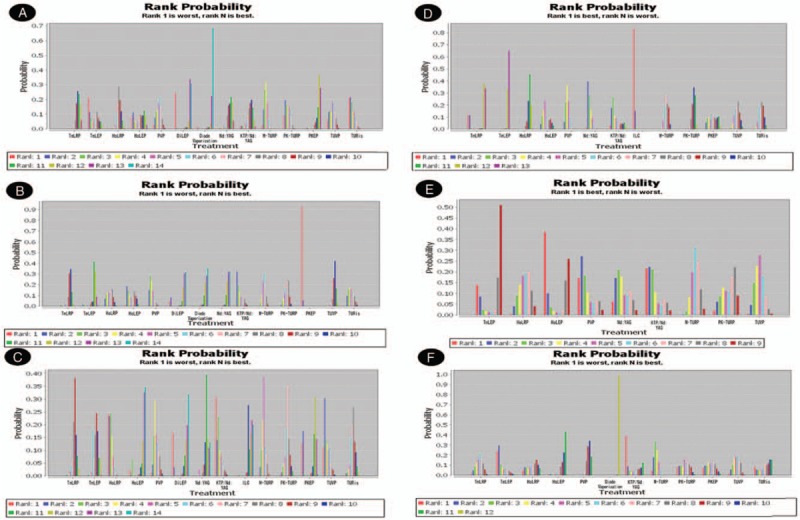
3.2. Effectiveness index evaluation after operation
Effectiveness index included IPSS, Qmax, PVR, and QoL scores; operating time, hospitalization, and catheterization time. For IPSS diode laser vaporization of prostate was significantly superior to other procedures, and TUVP was the worst one. The relative effect estimate of diode laser vaporization versus TUVP was −4.02 (−8.05, −0.06). Rank probability of IPSS from the best to the worst was diode laser vaporization > Nd:YAG > PVP > KTP/Nd:YAG > ILC > TURis > TmLRP > TmLEP > HoLEP > M-TURP > HoLRP > DiLEP > transurethral plasmakinetic resection of prostate (PKRP) > PKEP > TUVP. (Figure 4A) Diode laser vaporization of prostate also had the best efficiency in improving Qmax,. Rank probability of Qmax from the best to the worst was diode laser vaporization > PVP > Nd:YAG > KTP/Nd:YAG > ILC > HoLRP > TmLRP > TURis > TmLEP > M-TURP > PKRP > HoLEP > DiLEP > PKEP > TUVP (Fig. 4B). The relative effect estimate of the best one versus the worst (TUVP) was −5.40 (−10.14, −0.67). Pooled data revealed that HoLEP was the best choice for improving PVR, and KTP/Nd:YAG was the worst one. The relative effect estimate was 28.26 (−21.05, 77.36). Rank probability of Qmax from the best to the worst was HoLEP > Nd:YAG > PVP > ILC > diode laser vaporization > PKRP > TURis > M-TURP > HoLRP > TmLRP > TmLEP > DiLEP > PKEP > TUVP > KTP/Nd:YAG (Fig. 4C). For QoL, TmLRP was the best technique and TUR was the worst one. The relative effect estimate was 0.18 (−0.29, 0.64). Rank probability from the best to the worst: TmLRP > TmLEP > HoLEP > HoLRP > PVP > DiLEP > M-TURP > PKRP > PKEP > TUVP > TURis (Fig. 4D).
Figure 4.
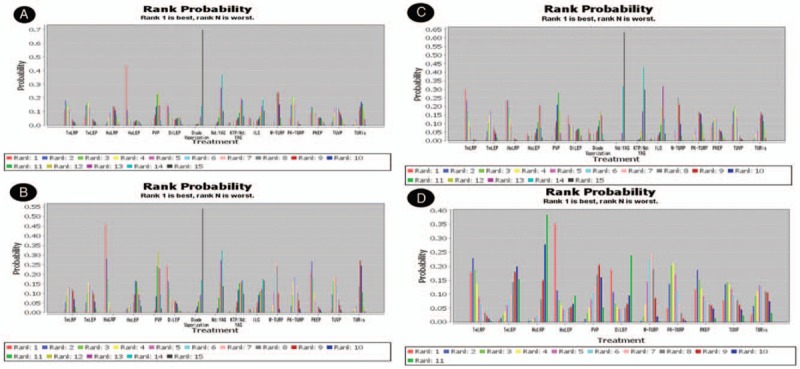
Rank probability of functional outcomes. (A) Rank probability of IPSS; (B) rank probability of Qmax; (C) rank probability of PVR; (D) rank probability of QoL. IPSS = International Prostate Symptom Score.
Perioperative outcomes included operation time, catheterization, and hospitalization time. PKRP needed the fewest time in operation compared with other transurethral procedures and HoLRP was the slowest one. The relative effect estimate of PKRP versus HoLRP was 21.63 (6.65, 36.36). Rank probability from the fastest to the slowest: PKRP > DiLEP > M-TURP > Nd:YAG > KTP/Nd:YAG > TUVP > TURis > TmLRP > diode laser vaporization > PVP > PKEP > HoLEP > TmLEP > HoLRP (Fig. 5A). Diode laser through vaporization required the shortest time in catheterization, while Nd:YAG was the longest one. The relative effect estimate of Diode laser versus Nd:YAG laser was −11.82 (−16.59, −7.10). Rank probability from the shortest to the longest: diode laser vaporization > HoLRP > TmLRP > PVP > DiLEP > TmLEP > HoLEP > PKRP > PKEP > TURis > TUVP > M-TURP > ILC > Nd:YAG (Fig. 5B). For hospitalization time, TUR is required the longest and HoLEP was the shortest. The relative effect estimate of HoLEP versus TUR was −4.98 (−14.57, 4.68). Rank probability from the shortest to the longest: HoLEP > PVP > TmLRP > TmLEP > HoLRP > DiLEP > diode laser vaporization > Nd:YAG > PKRP > M-TURP > PKEP > TUVP > TURis (Fig. 5C).
Figure 5.
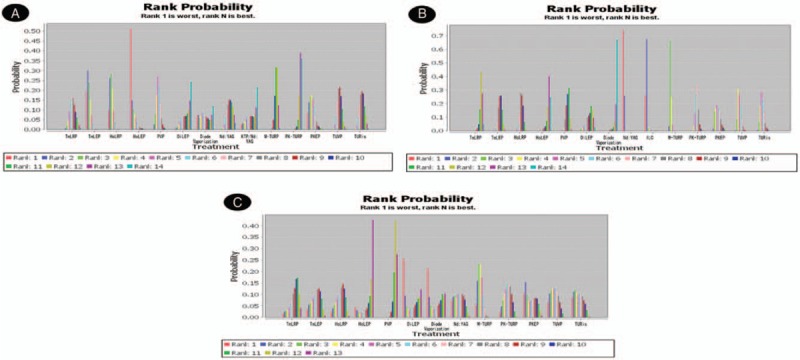
Rank probability of perioperation-related outcomes. (A) Rank probability of operation time; (B) rank probability of catheterization time; (C) rank probability of hospitalization time.
3.3. Complication evaluation after operation
Short-term complications included TURS, hematuria, postoperative hemoglobin decrease, blood transfusion, clot retention, recatheterization, urinary retention, dysuria, and urinary tract infection. Fifty articles reported TURS and the network analysis showed that M-TURP was related to the highest incidence rate of TURS and PKRP was related to the lowest occurrence rate. The relative effect estimate of PKRP versus M-TURP was 16.24 (4.02, 22.53) (Fig. 6A). Hematuria was rarely observed in TmLEP and mostly happened in M-TURP. TmLRP led the lowest postoperative hemoglobin decrease and TUR was the worst one. M-TURP was the most common technique associated with blood transfusion and Diode laser vaporization was the safest choice; Clot retention was mostly observed in M-TURP but rarely in PVP (Fig. 6B–E).
Figure 6.
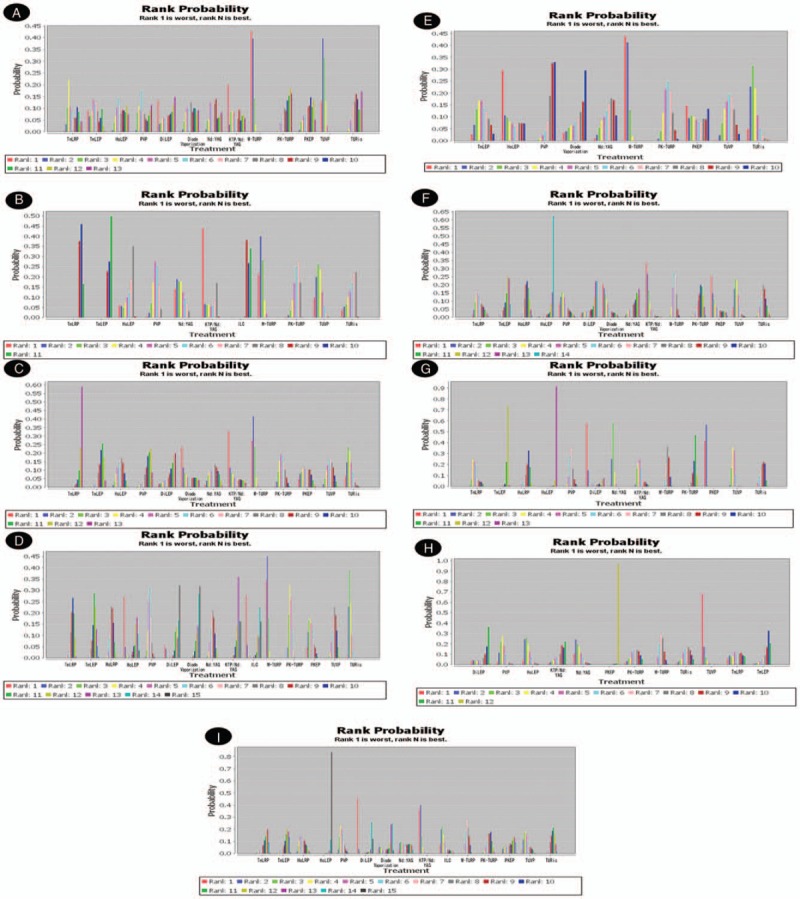
Rank probability of short-term complications. (A) Rank probability of TURS; (B) rank probability of hematuria; (C) rank probability of postoperative hemoglobin decrease; (D) rank probability of blood transfusion; (E) rank probability of clot retention; (F) rank probability of recatheterization; (G) rank probability of urinary retention; (H) rank probability of dysuria; (I) rank probability of urinary tract infection. TURS = transurethral resection syndrome.
Recatheterization occurred rarely in HoLEP and commonly in KTP/Nd:YAG. Urinary retention always happened to the patients, who underwent Nd:YAG laser resection and it was barely occurred in HoLEP. TUVP had the highest rate of dysuria and PKEP was the best one; In addition, urinary tract infection was rare in patients treated with HoLEP (Fig. 6F–I).
Long-term complications included urethral stricture, bladder neck contracture, stress urinary incontinence, reoperation, retrograde ejaculation, and erectile dysfunction. There were 69 articles reported urethral stricture. Diode laser vaporization showed the best security due to the network analysis and TUR was the most dangerous one. The relative effect estimate of diode laser vaporization versus TUR was 0.77 (0.32, 1.72) (Fig. 7A). Around 46 studies were related to bladder neck contracture. Diode laser vaporization leaded to the lowest occurrence rate and KTP/Nd:YAG laser leaded to the highest incidence rate (Fig. 7B). Stress urinary incontinence was frequently occurred in KTP/Nd:YAG laser and HoLEP was on the contrary (Fig. 7C).
Figure 7.
Rank probability of long-term complications. (A) Rank probability of urethral stricture; (B) rank probability of bladder neck contracture; (C) rank probability of stress urinary incontinence; (D) rank probability of reoperation; (E) rank probability of erectile dysfunction; (F) rank probability of retrograde ejaculation.
Reoperation was reported in 37 studies. The reasons included bleeding, clot retention, urethral stricture, bladder neck contracture recurrence of hyperplasia, and so on. The particular reasons were too disperse to make subgroup analysis. We analyzed the overall reoperation rate. ILC was the most common technique inducing reoperation, while TmLEP was the safest choice (Fig. 7D). For the male sexual function, our attention was fixed on the occurrence of retrograde ejaculation and erectile dysfunction. TmLEP had the least rates of occurrence of erectile dysfunction, while KTP/Nd:YAG laser leaded to the highest incidence rate. Retrograde ejaculation was rare in patients treated with HoLEP and was common in M-TURP (Fig. 7E and F).
4. Discussion
Lower urinary tract symptoms (LUTS) are significantly associated with bladder outlet obstruction.89% of patients with bladder outlet obstruction was due to benign prostatic obstruction.[107] Monopolar TURP is an effective method for the treatment of BPH and has been regarded as gold standard for decades. However, M-TURP is always accompanied by various complications, such as transurethral resection syndrome, bleeding, clot retention and retrograde ejaculation. To improve the efficiency and reduce these complications, various transurethral procedures have been developed, such as transurethral electrovaporization of prostate (TUVP), bipolar TURP and various lasers. Each procedure has its own advantage and disadvantage. Nørby et al[108] also investigated the cost-effectiveness of different treatments for benign prostatic hyperplasia through a short-term follow-up. In this study, we made a network meta-analysis and compare the efficacy and safety of different transurethral procedures for the treatment of BPH.
Nd:YAG laser, KTP/Nd:YAG laser and interstitial laser coagulation were popular procedures in the last century and rarely used today.[50,55,60,64] No matter in direct analysis or in our network meta-analysis, they have no advantages compared with other techniques.[27] We also found that M-TURP, TUVP,[82–94] and TURis were ordinary in effectiveness and were associated with higher complications. Based on the results of our study, thulium laser, holmium laser, diode laser, greenlight laser, and plasmakinetic system are advantageous.
Compared to other procedures, 3 types of lasers exhibited ideal results in terms of Qmax, PVR, IPSS, and QoL:HoLEP was the best one for PVR improvement. TmLRP had the best efficacy in improving QoL score. Diode laser vaporization of prostate was superior in improving IPSS and Qmax. For the perioperation-related outcomes, PKRP needed the fewest operation time while holmium laser and thulium laser took the longest time. Diode laser through vaporization required the shortest catheterization time. HoLEP required the shortest hospitalization time. In general, laser operation procedures required relatively longer operation time compared with TURP.[5] In fact, catheterization and hospitalization time are more important for patients. So thulium laser, holmium laser, and diode laser showed had better surgical efficacy.
Effectiveness and safety are 2 equally important factors to evaluate the surgical techniques. For safety, thulium laser, diode laser and holmium laser have relatively higher performance. Thulium laser was first used in 2004.[109] The center wavelength of thulium laser is tunable between 1.75 and 2.22 μm, which exactly matches the 1.92 μm water absorption peak in tissues. This character implies higher energy absorption at the surface of tissue. Due to the advantage, thulium laser is performed excellently in vaporization and hemostasia. Studies also showed that histological analysis following laser transurethral resection of the prostate will be helpful for the prostate cancer screening.[110] In this meta-analysis, TmLRP led the lowest postoperative hemoglobin decrease and had the least rates of occurrence of hematuria. More rapid vaporization makes it similar to resection, vaporization or enucleation actually. The second advantage of thulium laser is the thin penetration depth, which is from 0.5 to 2 mm.[19] The thinner coagulation depth means minimal thermal injury to surrounding tissues. TmLEP had the least rates of erectile dysfunction, which may be related to the better protection for nervi erigentes.
Diode laser also has high absorption in water and hemoglobin,[25,26,111] and the hemostasia was proved by the minimum occurrence of blood transfusion in this meta-analysis. Moreover, Razzaghi et al[26] showed the coagulation rim of diode laser is from 0.2 to 1 mm. Due to the smaller thickness of coagulative range and less thermal injury, the complications, such as urethral stricture and bladder neck contracture, relatively rare in the patients who underwent diode laser vaporization.
For holmium laser, the enucleation[24,28,29,31–42] was more widely used than resection.[27,30] A large number of studies[31–42] proved that HoLEP was a safe choice for the treatment of BPH and HoLEP led to the lowest incidence of recatheterization, urinary retention, urinary tract infection, stress urinary incontinence and retrograde ejaculation in our research. But However, it is also remarkable that HoLEP has potential damage of prostate capsule because of its pulse work mode and requirement of tissue morcellatio.[35] In general, thulium laser, diode laser, and holmium laser were equally with high efficacy and safety.[23,24]
Greenlight laser is one of the most common surgical energy platforms for the treatment of BPH. The wavelength of greenlight is 532 nm, which can fully absorbed by oxyhemoglobin, but hardly absorbed by water.[49] This character means better for hemostasia but deeper thermal injury to surrounding tissues. That was the reason that PVP was associated with the most rare incidences of clot retention, but relatively worse in erectile dysfunction and bladder neck contracture in our meta-analysis. Al-Ansari et al[44] and Capitan et al[46] proved that PVP and TURP have the same complication rate.
The plasmakinetic surgical also have various advantages: ability to work in saline, more efficacious in resection, and a smooth wound surface. By virtue of the superiorities, transurethral plasmakinetic prostatectomy was proved to significantly reduce TURS and dysuria in our meta-analysis. But many studies showed that plasmakinetic surgical was inferior to thulium laser, holmium laser and diode laser in hemorrhage, recovery time, catheterization and hospitalization time.[20–22,26,39] So, further research about plasmakinetic technique is needed.
There were also some limitations for this meta-analysis. Due to the update of equipment, one kind of laser usually corresponds different sizes of power (about enrolled RCTs, thulium laser 50, 70, 90, 100, 120 W; holmium laser 80, 90, 100 W; PVP 80, 120, 180 W). The volume of prostate in every trial was not exactly equal to each other.
In conclusion, this study showed comprehensive comparison of transurethral surgeries. For IPSS and Qmax, diode laser vaporization of prostate was the first choice. For PVR, HoLEP was the best choice. For QoL, TmLRP was the best technique. Compared with other transurethral procedures, thulium, holmium and diode lasers were associated with better efficacy outcomes and fewer complications. It will be helpful for the doctors to make choice from different procedures for the patients with BPH.
Author contributions
Conceptualization: Feng Sun.
Data curation: Qinglu Shi.
Formal analysis: Yuzhang Zhai.
Investigation: Feng Sun, Xincheng Sun.
Methodology: Feng Sun.
Project administration: Feng Sun.
Resources: Feng Sun.
Software: Feng Sun.
Supervision: Feng Sun.
Validation: Feng Sun.
Visualization: Feng Sun.
Writing – original draft: Feng Sun.
Writing – review & editing: Feng Sun.
Footnotes
Abbreviations: BPH = benign prostatic hyperplasisa, IPSS = International Prostate Symptom Score, LUTS = lower urinary tract symptoms, M-TURP = monopolar TURP, PVR = postvoid residual, Qmax = maximum flow rate, QoL = quality of life, RCTs = randomized controlled trials, TURis = transurethral resection in saline, TURS = transurethral resection syndrome, TUVP = transurethral electrovaporization of prostate.
The authors have no conflicts of interest to disclose.
References
- [1].Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 2013;64:118–40. [DOI] [PubMed] [Google Scholar]
- [2].DeCao H, Wang J, Huang Y, et al. Comparison between thulium laser resection of prostate and transurethral plasmakinetic resection of prostate or transurethral resection of prostate. Sci Rep 2015;5:14542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Xu H, Wan X, Gu M, et al. Surgical treatment for benign prostatic hyperplasia: holmium laser enucleation of the prostate (HoLEP). J Vis Exp 2018;doi: 10.3791/56683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Mobley D, Feibus A, Baum N. Benign prostatic hyperplasia and urinary symptoms: Evaluation and treatment. Postgrad Med 2015;127:301–7. [DOI] [PubMed] [Google Scholar]
- [5].Ahyai SA, Gilling P, Kaplan SA, et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol 2010;58:384–97. [DOI] [PubMed] [Google Scholar]
- [6].Zou Z, Xu A, Zheng S, et al. Dual-centre randomized-controlled trial comparing transurethral endoscopic enucleation of the prostate using diode laser vs. bipolar plasmakinetic for the treatment of LUTS secondary of benign prostate obstruction: 1-year follow-up results. World J Urol 2018;36:1117–26. [DOI] [PubMed] [Google Scholar]
- [7].Xu P, Xu A, Chen B, et al. Bipolar transurethral enucleation and resection of the prostate: whether it is ready to supersede TURP? Asian J Urol 2018;5:48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [9].Schünemann HJ, Oxman AD, Vist GE, et al. Chapter 12: interpreting results and drawing conclusions. Cochrane Handbook for Systematic Reviews of Interventions. pp. 359–387, 2011. Available at: www.cochranehandbook org. [Google Scholar]
- [10].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [11].Yan H, Ou TW, Chen L, et al. Thulium laser vaporesection versus standard transurethral resection of the prostate: a randomized trial with transpulmonary thermodilution hemodynamic monitoring. Int J Urol 2013;20:507–12. [DOI] [PubMed] [Google Scholar]
- [12].Cui D, Sun F, Zhuo J, et al. A randomized trial comparing thulium laser resection to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: four-year follow-up results. World J Urol 2014;32:683–9. [DOI] [PubMed] [Google Scholar]
- [13].Xia SJ, Zhuo J, Sun XW, et al. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol 2008;53:382–9. [DOI] [PubMed] [Google Scholar]
- [14].Swiniarski PP, Stepien S, Dudzic W, et al. Thulium laser enucleation of the prostate (TmLEP) vs. transurethral resection of the prostate (TURP): evaluation of early results. Cent European J Urol 2012;65:130–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Zhuo JXS, Liu HT, Sun XW, et al. A comparative study of thulium laser resection of the prostate-Tangerine technique and transurethral resection of the prostate for the treatment of benign prostatic hyperplasia. Chin J Urol 2007;28:38–41. [Google Scholar]
- [16].Fu WJ, Zhang X, Yang Y, et al. Comparison of 2-microm continuous wave laser vaporesection of the prostate and transurethral resection of the prostate: a prospective nonrandomized trial with 1-year follow-up. Urology 2010;75:194–9. [DOI] [PubMed] [Google Scholar]
- [17].Shao JKWY, Lu YA, Li XD. Comparison of 2 um continuous-wave laser enucleation of the prostate and transurethral resection of the prostate for benign prostatic hyperplasia. Chin J Surg 2012;50:131–4. [PubMed] [Google Scholar]
- [18].Yang SLJ, Zhang J, Zhao JY. Comparison of 2 μm continuous-wave laser vapores ecti on and trans urethral resect ion of the prostate: a randomized controlled ttrial. Chin J Min Inv Surg 2015;15:986–9. [Google Scholar]
- [19].Zhu Z, Shen Z, Tu F, et al. Thulium laser vaporesection versus transurethral electrovaporization of the prostate in high-risk patients with benign prostatic hyperplasia. Photomed Laser Surg 2012;30:714–8. [DOI] [PubMed] [Google Scholar]
- [20].Wei H, Shao Y, Sun F, et al. Thulium laser resection versus plasmakinetic resection of prostates larger than 80 ml. World J Urol 2014;32:1077–85. [DOI] [PubMed] [Google Scholar]
- [21].Peng B, Wang GC, Zheng JH, et al. A comparative study of thulium laser resection of the prostate and bipolar transurethral plasmakinetic prostatectomy for treating benign prostatic hyperplasia. BJU Int 2013;111:633–7. [DOI] [PubMed] [Google Scholar]
- [22].Feng L, Zhang D, Tian Y, et al. Thulium laser enucleation versus plasmakinetic enucleation of the prostate: a randomized trial of a single center. J Endourol 2016;30:665–70. [DOI] [PubMed] [Google Scholar]
- [23].Yang Z, Wang X, Liu T. Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology 2013;81:396–400. [DOI] [PubMed] [Google Scholar]
- [24].Zhang FB, Shao Q, Tian Y. Comparison of the diode laser and the thulium laser in transurethral enucleation of the prostate for treatment of benign prostatic hyperplasia. Beijing Da Xue Xue Bao 2013;45:592–6. [PubMed] [Google Scholar]
- [25].Zhang F, Shao Q, Herrmann TR, et al. Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology 2012;79:869–74. [DOI] [PubMed] [Google Scholar]
- [26].Razzaghi MR, Mazloomfard MM, Mokhtarpour H, et al. Diode laser (980 nm) vaporization in comparison with transurethral resection of the prostate for benign prostatic hyperplasia: randomized clinical trial with 2-year follow-up. Urology 2014;84:526–32. [DOI] [PubMed] [Google Scholar]
- [27].Xu A, Zou Y, Li B, et al. A randomized trial comparing diode laser enucleation of the prostate with plasmakinetic enucleation and resection of the prostate for the treatment of benign prostatic hyperplasia. J Endourol 2013;27:1254–60. [DOI] [PubMed] [Google Scholar]
- [28].Gilling PJ, Cass CB, Malcolm A, et al. Holmium laser resection of the prostate versus neodymium:yttrium-aluminum-garnet visual laser ablation of the prostate: a randomized prospective comparison of two techniques for laser prostatectomy. Urology 1998;51:573–7. [DOI] [PubMed] [Google Scholar]
- [29].Elmansy H, Baazeem A, Kotb A, et al. Holmium laser enucleation versus photoselective vaporization for prostatic adenoma greater than 60 ml: preliminary results of a prospective, randomized clinical trial. J Urol 2012;188:216–21. [DOI] [PubMed] [Google Scholar]
- [30].Elshal AM, Elkoushy MA, El-Nahas AR, et al. GreenLight laser (XPS) photoselective vapo-enucleation versus holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic hyperplasia: a randomized controlled study. J Urol 2015;193:927–34. [DOI] [PubMed] [Google Scholar]
- [31].Elmansy HM, Elzayat E, Elhilali MM. Holmium laser ablation versus photoselective vaporization of prostate less than 60 cc: long-term results of a randomized trial. J Urol 2010;184:2023–8. [DOI] [PubMed] [Google Scholar]
- [32].Gupta N, Sivaramakrishna, Kumar R, et al. Comparison of standard transurethral resection, transurethral vapour resection and holmium laser enucleation of the prostate for managing benign prostatic hyperplasia of >40 g. BJU Int 2006;97:85–9. [DOI] [PubMed] [Google Scholar]
- [33].Rigatti L, Naspro R, Salonia A, et al. Urodynamics after TURP and HoLEP in urodynamically obstructed patients: are there any differences at 1 year of follow-up? Urology 2006;67:1193–8. [DOI] [PubMed] [Google Scholar]
- [34].Fraundorfer MR, Gilling PJ, Kennett KM, et al. Holmium laser resection of the prostate is more cost effective than transurethral resection of the prostate: results of a randomized prospective study. Urology 2001;57:454–8. [DOI] [PubMed] [Google Scholar]
- [35].Wilson LC, Gilling PJ, Williams A, et al. A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur Urol 2006;50:569–73. [DOI] [PubMed] [Google Scholar]
- [36].Gilling PJ, Wilson LC, King CJ, et al. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int 2012;109:408–11. [DOI] [PubMed] [Google Scholar]
- [37].Fayad AS, Elsheikh MG, Zakaria T, et al. Holmium laser enucleation of the prostate versus bipolar resection of the prostate: a prospective randomized study. “Pros and Cons”. Urology 2015;86:1037–41. [DOI] [PubMed] [Google Scholar]
- [38].Kuntz RM, Ahyai S, Lehrich K, et al. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol 2004;172:1012–6. [DOI] [PubMed] [Google Scholar]
- [39].Ahyai SA, Lehrich K, Kuntz RM. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol 2007;52:1456–63. [DOI] [PubMed] [Google Scholar]
- [40].Chen YB, Chen Q, Wang Z, et al. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year followup. J Urol 2013;189:217–22. [DOI] [PubMed] [Google Scholar]
- [41].Eltabey MASH, Hussein AA. Holmium laser enucleation versus transurethral resection of the prostate. Can J Urol 2010;17:5447–52. [PubMed] [Google Scholar]
- [42].Sun N, Fu Y, Tian T, et al. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a randomized clinical trial. Int Urol Nephrol 2014;46:1277–82. [DOI] [PubMed] [Google Scholar]
- [43].Montorsi F, Naspro R, Salonia A, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol 2004;172:1926–9. [DOI] [PubMed] [Google Scholar]
- [44].Al-Ansari A, Younes N, Sampige VP, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol 2010;58:349–55. [DOI] [PubMed] [Google Scholar]
- [45].Lukacs B, Loeffler J, Bruyere F, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol 2012;61:1165–73. [DOI] [PubMed] [Google Scholar]
- [46].Capitan C, Blazquez C, Martin MD, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: a randomized clinical trial with 2-year follow-up. Eur Urol 2011;60:734–9. [DOI] [PubMed] [Google Scholar]
- [47].Telli O, Okutucu TM, Suer E, et al. A prospective, randomized comparative study of monopolar transurethral resection of the prostate versus photoselective vaporization of the prostate with GreenLight 120-W laser, in prostates less than 80 cc. Ther Adv Urol 2015;7:3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Bachmann A, Tubaro A, Barber N, et al. 180-W XPS GreenLight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European Multicentre Randomised Trial—the GOLIATH study. Eur Urol 2014;65:931–42. [DOI] [PubMed] [Google Scholar]
- [49].Thomas JA, Tubaro A, Barber N, et al. A multicenter randomized noninferiority trial comparing GreenLight-XPS laser vaporization of the prostate and transurethral resection of the prostate for the treatment of benign prostatic obstruction: two-yr outcomes of the GOLIATH study. Eur Urol 2016;69:94–102. [DOI] [PubMed] [Google Scholar]
- [50].Horasanli K, Silay MS, Altay B, et al. Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology 2008;71:247–51. [DOI] [PubMed] [Google Scholar]
- [51].Shingleton WB, Terrell F, Renfroe DL, et al. A randomized prospective study of laser ablation of the prostate versus transurethral resection of the prostate in men with benign prostatic hyperplasia. Urology 1999;54:1017–21. [DOI] [PubMed] [Google Scholar]
- [52].Peng M, Yi L, Wang Y. Photoselective vaporization of the prostate vs plasmakinetic resection of the prostate: a randomized prospective trial with 12-month follow-up in mainland China. Urology 2016;87:161–5. [DOI] [PubMed] [Google Scholar]
- [53].Mohanty NK, Vasudeva P, Kumar A, et al. Photoselective vaporization of prostate vs. transurethral resection of prostate: A prospective, randomized study with one year follow-up. Indian J Urol 2012;28:307–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Xue B, Zang Y, Zhang Y, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a prospective randomized trial. J Xray Sci Technol 2013;21:125–32. [DOI] [PubMed] [Google Scholar]
- [55].Bouchier-Hayes DM, Van Appledorn S, Bugeja P, et al. A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int 2010;105:964–9. [DOI] [PubMed] [Google Scholar]
- [56].Anson K, Nawrocki J, Buckley J, et al. A multicenter, randomized, prospective study of endoscopic laser ablation versus transurethral resection of the prostate. Urology 1995;46:305–10. [DOI] [PubMed] [Google Scholar]
- [57].Keoghane SR, Cranston DW, Lawrence KC, et al. The Oxford Laser Prostate Trial: a double-blind randomized controlled trial of contact vaporization of the prostate against transurethral resection; preliminary results. Brit J Urol 1996;77:382–5. [DOI] [PubMed] [Google Scholar]
- [58].Keoghane SR, Lawrence KC, Gray AM, et al. A double-blind randomized controlled trial and economic evaluation of transurethral resection vs contact laser vaporization for benign prostatic enlargement: a 3-year follow-up. BJU Int 2000;85:74–8. [DOI] [PubMed] [Google Scholar]
- [59].Tuhkanen K, Heino A, Alaopas M. Hybrid laser treatment compared with transurethral resection of the prostate for symptomatic bladder outlet obstruction caused by a large benign prostate: a prospective, randomized trial with a 6-month follow-up. BJU Int 1999;84:805–9. [DOI] [PubMed] [Google Scholar]
- [60].Razzaghi MR, Habibi G, Djavid GE, et al. Laser prostatectomy versus transurethral resection of prostate in the treatment of benign prostatic hyperplasia. Saudi Med J 2007;28:68–72. [PubMed] [Google Scholar]
- [61].Cowles RS, 3rd, Kabalin JN, Childs S, et al. A prospective randomized comparison of transurethral resection to visual laser ablation of the prostate for the treatment of benign prostatic hyperplasia. Urology 1995;46:155–60. [DOI] [PubMed] [Google Scholar]
- [62].Carter A, Sells H, Speakman M, et al. A prospective randomized controlled trial of hybrid laser treatment or transurethral resection of the prostate, with a 1-year follow-up. BJU Int 1999;83:254–9. [DOI] [PubMed] [Google Scholar]
- [63].van Melick HH, van Venrooij GE, Eckhardt MD, et al. A randomized controlled trial comparing transurethral resection of the prostate, contact laser prostatectomy and electrovaporization in men with benign prostatic hyperplasia: analysis of subjective changes, morbidity and mortality. J Urol 2003;169:1411–6. [DOI] [PubMed] [Google Scholar]
- [64].Hoekstra RJ, Van Melick HH, Kok ET, et al. A 10-year follow-up after transurethral resection of the prostate, contact laser prostatectomy and electrovaporization in men with benign prostatic hyperplasia; long-term results of a randomized controlled trial. BJU Int 2010;106:822–6. [DOI] [PubMed] [Google Scholar]
- [65].Kursh ED, Concepcion R, Chan S, et al. Interstitial laser coagulation versus transurethral prostate resection for treating benign prostatic obstruction: a randomized trial with 2-year follow-up. Urology 2003;61:573–8. [DOI] [PubMed] [Google Scholar]
- [66].Fung BT, Li SK, Yu CF, et al. Prospective randomized controlled trial comparing plasmakinetic vaporesection and conventional transurethral resection of the prostate. Asian J Surg 2005;28:24–8. [DOI] [PubMed] [Google Scholar]
- [67].Muslumanoglu AY, Yuruk E, Binbay M, et al. Transurethral resection of prostate with plasmakinetic energy: 100 months results of a prospective randomized trial. BJU Int 2012;110:546–9. [DOI] [PubMed] [Google Scholar]
- [68].Erturhan S, Erbagci A, Seckiner I, et al. Plasmakinetic resection of the prostate versus standard transurethral resection of the prostate: a prospective randomized trial with 1-year follow-up. Prostate Cancer Prostatic Dis 2007;10:97–100. [DOI] [PubMed] [Google Scholar]
- [69].He JWXJ, Chen GY, Guan DH. Therapeutic efficacy of bipolar plasmakinetic resection compared with transurethral resection on benign prostate hyperplasia. Chin J Endourol (Electronic Edn) 2010;4:302–4. [Google Scholar]
- [70].Xie CY, Zhu GB, Wang XH, et al. Five-year follow-up results of a randomized controlled trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Yonsei Med J 2012;53:734–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Zhao Z, Zeng G, Zhong W, et al. A prospective, randomised trial comparing plasmakinetic enucleation to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: three-year follow-up results. Eur Urol 2010;58:752–8. [DOI] [PubMed] [Google Scholar]
- [72].Autorino R, Damiano R, Di Lorenzo G, et al. Four-year outcome of a prospective randomised trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Eur Urol 2009;55:922–9. [DOI] [PubMed] [Google Scholar]
- [73].Stucki P, Marini L, Mattei A, et al. Bipolar versus monopolar transurethral resection of the prostate: a prospective randomized trial focusing on bleeding complications. J Urol 2015;193:1371–5. [DOI] [PubMed] [Google Scholar]
- [74].Giulianelli R, Albanesi L, Attisani F, et al. Comparative randomized study on the efficaciousness of endoscopic bipolar prostate resection versus monopolar resection technique. 3 year follow-up. Arch Ital Urol Androl 2013;85:86–91. [DOI] [PubMed] [Google Scholar]
- [75].Hon NH, Brathwaite D, Hussain Z, et al. A prospective, randomized trial comparing conventional transurethral prostate resection with PlasmaKinetic vaporization of the prostate: physiological changes, early complications and long-term followup. J Urol 2006;176:205–9. [DOI] [PubMed] [Google Scholar]
- [76].Geavlete B, Georgescu D, Multescu R, et al. Bipolar plasma vaporization vs monopolar and bipolar TURP-A prospective, randomized, long-term comparison. Urology 2011;78:930–5. [DOI] [PubMed] [Google Scholar]
- [77].Patankar S, Jamkar A, Dobhada S, et al. PlasmaKinetic Superpulse transurethral resection versus conventional transurethral resection of prostate. J Endourol 2006;20:215–9. [DOI] [PubMed] [Google Scholar]
- [78].Akcayoz M, Kaygisiz O, Akdemir O, et al. Comparison of transurethral resection and plasmakinetic transurethral resection applications with regard to fluid absorption amounts in benign prostate hyperplasia. Urol Int 2006;77:143–7. [DOI] [PubMed] [Google Scholar]
- [79].Seckiner I, Yesilli C, Akduman B, et al. A prospective randomized study for comparing bipolar plasmakinetic resection of the prostate with standard TURP. Urol Int 2006;76:139–43. [DOI] [PubMed] [Google Scholar]
- [80].Bhansali M, Patankar S, Dobhada S, et al. Management of large (>60 g) prostate gland: PlasmaKinetic Superpulse (bipolar) versus conventional (monopolar) transurethral resection of the prostate. J Endourol 2009;23:141–5. [DOI] [PubMed] [Google Scholar]
- [81].de Sio M, Autorino R, Quarto G, et al. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology 2006;67:69–72. [DOI] [PubMed] [Google Scholar]
- [82].Sinanoglu O, Ekici S, Tatar MN, et al. Postoperative outcomes of plasmakinetic transurethral resection of the prostate compared to monopolar transurethral resection of the prostate in patients with comorbidities. Urology 2012;80:402–6. [DOI] [PubMed] [Google Scholar]
- [83].Kaplan SA, Laor E, Fatal M, et al. Transurethral resection of the prostate versus transurethral electrovaporization of the prostate: a blinded, prospective comparative study with 1-year followup. J Urol 1998;159:454–8. [DOI] [PubMed] [Google Scholar]
- [84].Talic RF, El Tiraifi A, El Faqih SR, et al. Prospective randomized study of transurethral vaporization resection of the prostate using the thick loop and standard transurethral prostatectomy. Urology 2000;55:886–90. discussion 90-1. [DOI] [PubMed] [Google Scholar]
- [85].Hammadeh MY, Fowlis GA, Singh M, et al. Transurethral electrovaporization of the prostate—a possible alternative to transurethral resection: a one-year follow-up of a prospective randomized trial. Br J Urol 1998;81:721–5. [DOI] [PubMed] [Google Scholar]
- [86].Hammadeh MY, Madaan S, Singh M, et al. A 3-year follow-up of a prospective randomized trial comparing transurethral electrovaporization of the prostate with standard transurethral prostatectomy. BJU Int 2000;86:648–51. [DOI] [PubMed] [Google Scholar]
- [87].Hammadeh MY, Madaan S, Hines J, et al. 5-year outcome of a prospective randomized trial to compare transurethral electrovaporization of the prostate and standard transurethral resection. Urology 2003;61:1166–71. [DOI] [PubMed] [Google Scholar]
- [88].Dunsmuir WD, McFarlane JP, Tan A, et al. Gyrus bipolar electrovaporization vs transurethral resection of the prostate: a randomized prospective single-blind trial with 1 y follow-up. Prostate Cancer Prostatic Dis 2003;6:182–6. [DOI] [PubMed] [Google Scholar]
- [89].McAllister WJ, Karim O, Plail RO, et al. Transurethral electrovaporization of the prostate: is it any better than conventional transurethral resection of the prostate? BJU Int 2003;91:211–4. [DOI] [PubMed] [Google Scholar]
- [90].Shokeir AA, al-Sisi H, Farage YM, et al. Transurethral prostatectomy: a prospective randomized study of conventional resection and electrovaporization in benign prostatic hyperplasia. Brit J Urol 1997;80:570–4. [DOI] [PubMed] [Google Scholar]
- [91].Kupeli S, Baltaci S, Soygur T, et al. A prospective randomized study of transurethral resection of the prostate and transurethral vaporization of the prostate as a therapeutic alternative in the management of men with BPH. Eur Urol 1998;34:15–8. [DOI] [PubMed] [Google Scholar]
- [92].Kupeli S, Yilmaz E, Soygur T, et al. Randomized study of transurethral resection of the prostate and combined transurethral resection and vaporization of the prostate as a therapeutic alternative in men with benign prostatic hyperplasia. J Endourol 2001;15:317–21. [DOI] [PubMed] [Google Scholar]
- [93].Gallucci M, Puppo P, Perachino M, et al. Transurethral electrovaporization of the prostate vs. transurethral resection. Results of a multicentric, randomized clinical study on 150 patients. Eur Urol 1998;33:359–64. [DOI] [PubMed] [Google Scholar]
- [94].Nuhoglu B, Ayyildiz A, Fidan V, et al. Transurethral electrovaporization of the prostate: is it any better than standard transurethral prostatectomy? 5-year follow-up. J Endourol 2005;19:79–82. [DOI] [PubMed] [Google Scholar]
- [95].Hammadeh MY, Madaan S, Singh M, et al. Two-year follow-up of a prospective randomised trial of electrovaporization versus resection of prostate. Eur Urol 1998;34:188–92. [DOI] [PubMed] [Google Scholar]
- [96].Ho HS, Yip SK, Lim KB, et al. A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. Eur Urol 2007;52:517–22. [DOI] [PubMed] [Google Scholar]
- [97].Chen Q, Zhang L, Fan QL, et al. Bipolar transurethral resection in saline vs traditional monopolar resection of the prostate: results of a randomized trial with a 2-year follow-up. BJU Int 2010;106:1339–43. [DOI] [PubMed] [Google Scholar]
- [98].Komura K, Inamoto T, Takai T, et al. Could transurethral resection of the prostate using the TURis system take over conventional monopolar transurethral resection of the prostate? A randomized controlled trial and midterm results. Urology 2014;84:405–11. [DOI] [PubMed] [Google Scholar]
- [99].Yee CH, Wong JH, Chiu PK, et al. Short-stay transurethral prostate surgery: a randomized controlled trial comparing transurethral resection in saline bipolar transurethral vaporization of the prostate with monopolar transurethral resection. Asian J Endosc Surg 2015;8:316–22. [DOI] [PubMed] [Google Scholar]
- [100].Fagerstrom T, Nyman CR, Hahn RG. Bipolar transurethral resection of the prostate causes less bleeding than the monopolar technique: a single-centre randomized trial of 202 patients. BJU Int 2010;105:1560–4. [DOI] [PubMed] [Google Scholar]
- [101].Mamoulakis C, Skolarikos A, Schulze M, et al. Results from an international multicentre double-blind randomized controlled trial on the perioperative efficacy and safety of bipolar vs monopolar transurethral resection of the prostate. BJU Int 2012;109:240–8. [DOI] [PubMed] [Google Scholar]
- [102].Mamoulakis C, Schulze M, Skolarikos A, et al. Midterm results from an international multicentre randomised controlled trial comparing bipolar with monopolar transurethral resection of the prostate. Eur Urol 2013;63:667–76. [DOI] [PubMed] [Google Scholar]
- [103].Mamoulakis C, Skolarikos A, Schulze M, et al. Bipolar vs monopolar transurethral resection of the prostate: evaluation of the impact on overall sexual function in an international randomized controlled trial setting. BJU Int 2013;112:109–20. [DOI] [PubMed] [Google Scholar]
- [104].Akman T, Binbay M, Tekinarslan E, et al. Effects of bipolar and monopolar transurethral resection of the prostate on urinary and erectile function: a prospective randomized comparative study. BJU Int 2013;111:129–36. [DOI] [PubMed] [Google Scholar]
- [105].Zhu L, Chen S, Yang S, et al. Electrosurgical enucleation versus bipolar transurethral resection for prostates larger than 70 ml: a prospective, randomized trial with 5-year followup. J Urol 2013;189:1427–31. [DOI] [PubMed] [Google Scholar]
- [106].Mendez-Probst CE, Nott L, Pautler SE, et al. A multicentre single-blind randomized controlled trial comparing bipolar and monopolar transurethral resection of the prostate. Can Urol Assoc J 2011;5:385–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Cormio L, Lucarelli G, Selvaggio O, et al. Absence of bladder outlet obstruction is an independent risk factor for prostate cancer in men undergoing prostate biopsy. Medicine (Baltimore) 2016;95:e2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Nørby B, Nielsen HV, Frimodt-Møller PC. Cost-effectiveness of new treatments for benign prostatichyperplasia: results of a randomized trial comparing the short-term cost-effectiveness of transurethral interstitial laser coagulation of the prostate, transurethral microwave thermotherapy and standard transurethral resection or incision of the prostate. Scand J Urol Nephrol 2002;36:286–95. [DOI] [PubMed] [Google Scholar]
- [109].Fried NM. High-power laser vaporization of the canine prostate using a 110 W thulium fiber laser at 1.91 microm. Lasers Surg Med 2005;36:52–6. [DOI] [PubMed] [Google Scholar]
- [110].Nafie S, Dormer J, Khan MA. The significance of histological analysis following laser transurethral resection of the prostate. Int Urol Nephrol 2017;49:1343–6. [DOI] [PubMed] [Google Scholar]
- [111].Wendt-Nordahl G, Huckele S, Honeck P, et al. 980-nm diode laser: a novel laser technology for vaporization of the prostate. Eur Urol 2007;52:1723–8. [DOI] [PubMed] [Google Scholar]


