Abstract
Many patients in China have portal hypertension secondary to liver cirrhosis. Splenectomy and devascularization have become an efficacious surgical procedure for portal hypertension, and has been recommended in China as the first choice for the treatment of portal hypertension for a long time. As a result of advances in laparoscopic equipment and techniques, splenectomy and esophagogastric devascularization have been carried out with laparoscope.
From January 2012 to December 2017, 453 patients who were diagnosed with portal hypertension and serious gastroesophageal varices received surgical management in our institution. 250 patients chose laparoscopic splenectomy and esophagogastric devascularization and 203 underwent open splenectomy and esophagogastric devascularization.
We retrospectively analyzed the perioperative data and follow-up data of these patients. The operation time of laparoscopic group was longer than open group (P ≤ .001). Intraoperative blood loss was less (P ≤ .001), the passing of flatus was earlier (P = .042), and postoperative hospital stay was shorter (P = .001) in the laparoscopic group. During postoperative follow-up of 4 to 75 months, the incidence of esophagogastric variceal rebleeding, encephalopathy, and secondary liver cancer showed no significant differences.
Laparoscopic splenectomy and esophagogastric devascularization were safe and more effective than open surgery for portal hypertension and gastroesophageal varices.
Keywords: laparoscopy, liver cirrhosis, portal hypertension, splenectomy and esophagogastric devascularization, varices
1. Introduction
Many patients in China have portal hypertension (PH) secondary to liver cirrhosis because of the high incidence of chronic hepatitis B infection. Hypersplenism and esophagogastric varices are the most common clinical manifestations of portal hypertension, occurring in 24% to 80% of cases, with a high mortality rate.[1,2] Once the varices are ruptured, the mortality is up to 15% to 20% within 6 weeks and as high as 40% within 1 year.[3,4] Liver transplantation is the most effective treatment for many chronic liver diseases with decompensated liver function. However, organ shortages and high medical costs appear to be 2 of the major problems in clinical transplantation.[5] Since the first description of splenectomy and devascularization in patients with portal hypertension by Hassab[6] this procedure, with some modifications, has become one of the most effective treatments for esophagogastric varices.[7] This surgery is currently performed in patients with gastric varices in many facilities worldwide because of its feasibility and decreased invasiveness compared with shunt surgery and transplantation.[8,9] The combination of splenectomy and esophagogastric devascularization is an efficacious surgical procedure for portal hypertension because bleeding, thrombocytopenia, and/or leukopenia can be resolved at the same time. It has been therefore recommended in China as an important choice for the treatment of portal hypertension for a long time, especially for liver cirrhosis due to chronic viral hepatitis infection.[10]
Recently, as a result of advances in laparoscopic equipment and techniques, splenectomy and esophagogastric devascularization have been carried out in a less-invasive way.[11,12] Several articles have been published on laparoscopic splenectomy or laparoscopic splenectomy and esophagogastric devascularization for liver cirrhosis and portal hypertension.[1,10,13]
This study retrospectively compared clinical data of 453 patients with portal hypertension due to cirrhosis who underwent laparoscopic splenectomy and esophagogastric devascularization (LSED) and open splenectomy and esophagogastric devascularization (OSED) from January 2012 to December 2017 in Shandong Provincial Hospital Affiliated to Shandong University, Jinan, China. The surgical technique and its clinical efficacy and safety were also discussed.
2. Patients and methods
2.1. Clinical data
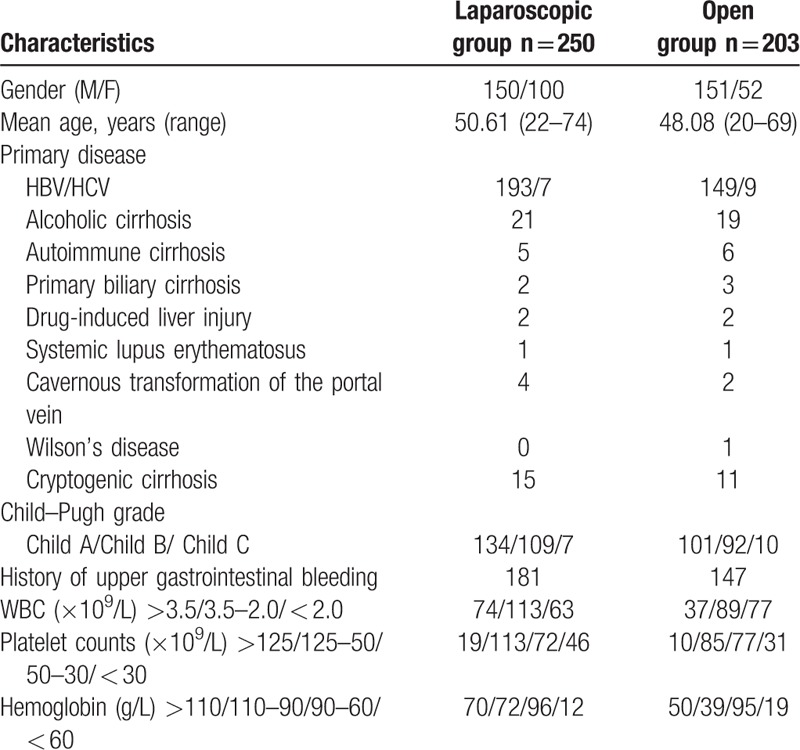
From January 2012 to December 2017, 453 patients who were diagnosed with portal hypertension and serious gastroesophageal varices received surgical management in Shandong Provincial Hospital Affiliated to Shandong University. Of them, 250 patients (150 men and 100 women), who underwent LSED, were selected in the laparoscopic group and 203 (151 men and 52 women) patients, who underwent OSED, were selected in the open group. The primary disease of laparoscopic group's patients including hepatitis B virus (HBV)-related cirrhosis (193 cases), alcoholic cirrhosis (21 cases), hepatitis C virus (HCV)-related cirrhosis (7 cases), autoimmune cirrhosis (5 cases), primary biliary cirrhosis (2 cases), drug-induced liver injury (2 cases), systemic lupus erythematosus (1 cases), cavernous transformation of the portal vein (4 cases), and cryptogenic cirrhosis (15 cases). The number of patients who underwent LSED in 2012–2017 were 6, 8, 26, 60, 74 and 76, respectively. The primary disease of open group's patients including hepatitis B virus (HBV)-related cirrhosis (149 cases), alcoholic cirrhosis (19 cases), hepatitis C virus (HCV)-related cirrhosis (9 cases), autoimmune cirrhosis (6 cases), primary biliary cirrhosis (3 cases), drug-induced liver injury (2 cases), systemic lupus erythematosus (1 cases), cavernous transformation of the portal vein (2 cases), Wilson's disease (1 case), and cryptogenic cirrhosis (11 cases) (Table 1). The number of patients who received OSED in 2012–2017 were 43, 49, 37, 26, 24, and 24, respectively. The operative indications were as follows: patients with portal hypertension and serious gastroesophageal varices (according to the grading systems of esophagogastric varices of China,[14] severe gastroesophageal varices is defined as serpent-form varices with red signs or varices with a string of beads appearance, nodular appearance or tumor-like appearance with or without red signs.); 18 to 75 years of age; thrombocytopenia and/or leucopenia (white blood cell count < 2.0 × 109/L, platelet count < 30 × 109/L) and/or esophagogastric variceal bleeding (EGVB) history due to hypersplenism; and general condition satisfying the needs for operation. The exclusion criteria included combination with uncontrollable ascites, untreatable hepatocellular carcinoma, and encephalopathy. All patients and their families were told the surgical procedures, possible complications, laparoscopic transfer laparotomy, and other relevant possibilities, and signed an Information Consent Form. This study was approved by the Medical Ethics Committee of Shandong Provincial Hospital Affiliated to Shandong University, and all experiments were performed in accordance with the relevant guidelines and regulations.
Table 1.
Clinical characteristics of patients in laparoscopic and open groups.
2.2. Operative method
Under general anesthesia with tracheal intubation, the patient was placed in the right semidecubitus position and the operating table was tilted to the reverse Trendelenburg position under pneumoperitoneum using carbon dioxide (maintenance of 10–14 mm Hg intra-abdominal pressure). The chief surgeon operated from the right side of the patient. The first assist stood at the left side of the patient. Five operation holes were chosen, the placement of port sites have a relatively fixed location; the sites can be moved slightly according to the size of spleen.[15] The trocar sites were demonstrated as in Figure 1.
Figure 1.
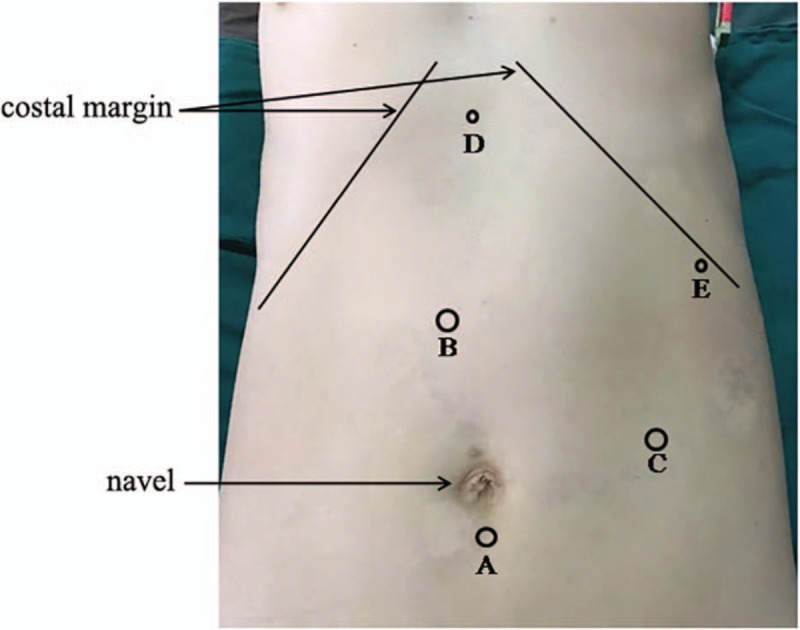
Position of trocar port for laparoscopic splenectomy and esophagogastric devascularization. (A) Laparoscope port (the position was moved down or to left according to the inferior margin of spleen): a 10-mm trocar was inserted for laparoscope; (B) main operating port (the position was shifted to right side slightly if necessary); a 12-mm trocar was inserted for laparoscopic instruments; (C) main operating port: a 12-mm trocar was inserted for main laparoscopic instruments; (D and E) ancillary operating port: a 5-mm trocar was inserted for supplementary laparoscopic instruments.
First of all, gastrocolic ligament and the splenocolic ligament were divided with a LigaSure Vessel Sealing System (LVSS) or Harmonic scalpel (Ethicon Endo-Surgery). Then, splenogastric ligament, the lienorenal ligament, and splenophrenic ligament were dissected in turn. The spleen almost became isolated after the above-mentioned ligament dissected. A tunnel behind the splenic hilum from the inferior border to superior border of the spleen was established meticulously. An Endo linear cutter (Ethicon Endo-Surgery) or an Endo-GIA universal endoscopic vascular linear stapler (Covidien) has been inserted into the tunnel, splenic hilum included the splenic artery and vein be transected en bloc. Short gastric vessel and pancreatic tail should be handled cautiously. The remaining splenodiaphragmatic ligament was divided with a Harmonic scalpel, to complete the splenectomy. To avoid possible hemorrhage in the process of splenic artery separation and reduction of portal vein system thrombosis (PVST) after splenectomy, the splenic artery was not ligated routinely before splenic hilum dissection. After confirming hemostasis, the spleen was placed into an appropriately sized impermeable sample bag, morcelated, and removed out of abdominal cavity through trocar B or C. Then, the patient was placed in a supine position and esophagogastric devascularization proceeded.
During splenectomy, partial devascularization of the upper greater curvature had already been performed. The rest of the greater curvature was devascularized from top to bottom of the stomach between the gastric serosa layer and varicose veins with LVSS, Harmonic scalpel or Hem-o-lok clip (Weck Surgical Instruments). After the greater curvature vessels were dissected, the stomach was pulled toward the abdominal wall, and devascularization of the lesser curvature was performed by the same method. The main branch of the stomach coronary vein was found and divided with Hem-o-lok or Harmonic scalpel. The esophagus was pulled downward and vessels were divided superior to a point 5 to 8 cm away from distal esophagus. One drainage tube was placed at the bottom of splenic fossa while the other one was placed at the top of splenic fossa.
In the OSED surgery, all patients were placed in a supine position and used an L-shaped incision of the upper left abdomen. Routine open splenectomy was implemented before esophagogastric devascularization. The esophagogastric devascularization procedure was similar to that of LSED.
All the perioperative clinical data, including operation time, blood loss, rate of conversion to open surgery, rate of transfusion, postoperative hospital stay, and passing of flatus, and follow-up results were collected and analyzed.
2.3. Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences software program (SPSS16.0 for Windows). Continuous variables values are expressed as the mean ± SD. The Student's t test, Mann–Whitney U test, Chi-square test, and Fisher's exact test were used as appropriate. P < .05 was considered statistically significant.
The datasets analysed during the current study are available from the corresponding author on reasonable request.
3. Results
There no deaths occurred during the surgery in either group. In laparoscopic group, operation was successfully performed in 213 patients while 32 cases were converted to laparotomy. Of these 32 cases, 21 patients converted to laparotomy because of uncontrollable bleeding, and 11 patients converted to laparotomy because of other reasons, such as severe perisplenitis, dense adhesion, vital signs of instability, and so on. OSED was successfully implemented in 203 cases. The operation time of laparoscopic group was significantly longer than open group (223.20 vs 188.09 minutes; P ≤ .001). The difference of transfusion rates between the 2 groups was not significant. (31.20 vs 36.45%; P = .239). Estimated blood loss of laparoscopic group was significantly less than that in open group (208.31 vs 298.54 mL; P ≤ .001). The mean postoperative hospital stay was shorter (8.42 vs 12.06 days; P = .001) and the passing of flatus was earlier (76.92 vs 92.82 hours; P = .042) in the laparoscopic group than that in open group (Table 2).
Table 2.
Perioperative clinical data of patients in laparoscopic and open groups.

There were 5 perioperative deaths in both groups. Three patients died from intra-abdominal hemorrhage and 2 from hepatic failure in the LSED group. Four patients died from intra-abdominal hemorrhage and one from hepatic failure in the OSED group. The incidence of PVST was 50.08% in the LSED group and 45.32% in the OSED group. Other postoperative complications occurred in patients after LSED as follows: 8 patients had intra-abdominal bleeding and 5 of them needed a second laparotomy to stop the bleeding. One patient had gastric leakage, 2 had encephalopathy, 2 patients had esophagogastric variceal rebleeding, 7 had refractory ascites, and 8 had infectious complications. Other postoperative complications occurred in patients after OSED as follows: 6 had intra-abdominal bleeding and 3 of them need a second laparotomy surgery to stop the bleeding. Two patients had a temporary pancreatic fistula, 2 had gastric leakage, 2 had encephalopathy, 3 had recurrent EGVB, 8 had refractory ascites, and 5 had infectious complications (Table 3).
Table 3.
Postoperative complications during hospitalization and follow-up data of patients in laparoscopic and open groups.
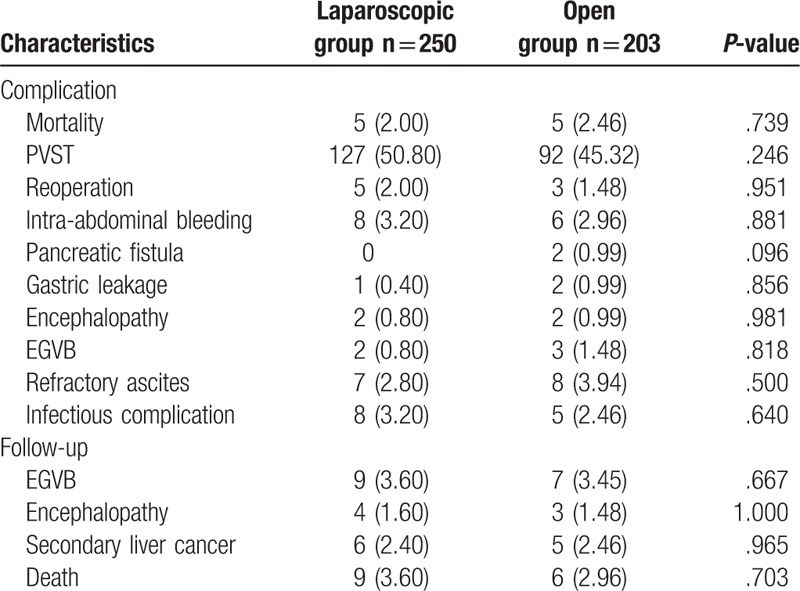
All patients were followed up for 4 to 75 months until April 2018. During postoperative follow-up, 16 of the 250 patients (6.40%) were lost to follow-up in the laparoscopic group and 14 of the 203 patients (6.89%) were lost to follow-up in the open group. EGVB recurred in nine LSED patients (3.60%) and in 7 (3.45%) OSED patients (P = .667), encephalopathy occurred in 4 LSED patients (1.60%) and 3 OSED patients (1.48%) (P = 1.000). Six patients (2.40%) occurred secondary liver cancer in laparoscopic group and 5 patients (2.46%) in open group (P = .965).
In the laparoscopic group, 4 patients died from acute upper digestive tract rebleeding, 2 from hepatic encephalopathy, and 3 from secondary liver cancer. In the open surgery group, 3 patients died from acute upper digestive tract rebleeding, one from hepatic failure and 2 from secondary liver cancer (Table 3).
4. Discussion
Around 130 million people in mainland China are carriers of HBV, which accounts for almost one third of the people infected with HBV worldwide and ∼10% of the general population in the country. Thirty million of those are chronically infected and most will develop liver cirrhosis and portal hypertension.[16] As a life-threatening disease, portal hypertension combined with hypersplenism and recurrent EGVB is one of the most serious diseases threatening human health in China. As an effective treatment for portal hypertension, splenectomy and esophagogastric devascularization have been applied for more than 30 years. This surgical procedure will continue to be the main treatment for portal hypertension, because most of the patients cannot receive liver transplantation on account of organ shortages and high medical costs in China. Additionally, the patients with portal hypertension secondary to liver cirrhosis usually have a poor general condition and a poor tolerance of operation. The optimal surgical procedure for these patients should possess less operative trauma and less surgical stress and avoid recurrence,[17] with minimal morbidity and mortality. In recent years, with advances in techniques and instruments, laparoscopy has been widely applied in clinic, including the splenectomy and esophagogastric devascularization.
Compared to the OSED, LSED showed lots of advantages, such as a magnified image and clearer vision, less operative trauma and internal environment interference, less surgical stress, and less abdominal cavity adhesions, which decreases the difficulty of potential subsequent liver transplantation.[18,19]
Patients with portal hypertension usually have liver cirrhosis for many years and their general condition is poor, such as, impaired liver function, anemia, hypoalbuminemia, thrombocytopenia, and coagulation disorders. For a long time, the presence of splenomegaly has been considered a relative or absolute contraindication for LSED.[20,21] However, several recent reports have showed that laparoscopic management is feasible and should be attempted for the removal of spleens of almost any size.[22,23] LSED has been used successfully in several medical centers around of the world.[10,24]
The technical highlights of LSED include the following. To choose the trocar port site flexibly if necessary. The trocar port sites have a relatively fixed location; the sites can be moved slightly according to the size of spleen. Reasonable procedures are used. It is reported that splenic artery ligation can shrink and soften the spleen, and the splenic artery is dissected and tied at the upper border of the pancreas before splenic hilum dissection. In our study, the splenic artery was not ligated routinely. Dissecting the splenic artery at the upper border of the pancreas sometimes can injure splenic vessels and cause hemorrhea. A combination of laparoscopic instruments is used, such as ligasure, ultrasonic scalpel, and endo-cutter. It is necessary to ensure that the power of the ultrasonic scalpel is large enough. Reasonable combined surgical approach is used. In our study, the most common approach was an anterior combined with posterolateral approach. During the LSED procedure, minor injuries may lead to life-threatening bleeding. In order to ensure a subsequent laparotomy implemented promptly, laparotomy surgical team and instruments must be prepared before the LSED procedure performed routinely.
In our study, size of spleen and emergency operation or not, was not restricted both in laparoscopic and open group. Operation indication, exclusion criteria, and operating procedure were same in laparoscopic and open group. The surgical path almost was the only difference between laparoscopic and open groups, which mean the results had more comparability.
Our data showed that estimated blood loss was significantly less, and the length of postoperative hospitalization was shorter, and the postoperative passing of flatus was earlier in the laparoscopy group. These results are identical with those reported in the literature. In both groups, postoperative complications were similar. However, in our study, the operative time in the laparoscopic group was longer than that in the open group. Less intraoperative blood loss should benefit from a clearer operative field of view, sufficient space, and advanced laparoscopic instruments. More importantly, bleeding under the laparoscopic usually interferes the operation view and may cause conversion to an open procedure, and surgeon pay more attention to prevent bleeding. Earlier mobilization due to the advantage of minimal invasion results in shorter length of postoperative hospitalization. The present data revealed that the incidence of complications was similar in both groups. However, although no significant differences were found, there seemed to be an overall trend in favor of LSED except for incidence rate of PVST. The role of LSED or OSED in the development of PVST is not yet clear. In any case, anticoagulant therapy should be given routinely in both LSED and OSED patients. According to the learning curve for some abdominal laparoscopic operations, the operation time obviously differs among centers and depends on the experience and skill of the surgeons. In our study, the operation time was longer in the laparoscopic group. Our result was consistent with the meta-analysis data.[13,25] Furthermore, we noticed that the mean operation time of LSED in our institution was reduced year by year.
Our results show the rate of conversion to an open procedure in LSED group is 12.8%, and is higher than some previous studies. The possible reasons as follows: splenic artery was not ligated routinely before splenic hilum dissection in our procedure; these can avoid possible hemorrhage in the process of splenic artery separation, but may increase the difficulty of perisplenic ligament separation. Some emergency patients and poor liver function patients (Child class C) were included in the statistical analysis. The tolerance of these patients to pneumoperitoneum pressure and long duration anesthesia were poor, and operation must be finished as soon as possible. The size of the spleen had no restrictions in our study. The size of the spleen was an important influencing factor, because huge spleen blocked the surgical view and increased the difficulty of laparoscopic surgery. As the operators’ laparoscopic skill level and experience improved, the rate of conversion to laparotomy decreased in the laparoscopic group year by year. However, it is worth emphasizing that conversion to an open procedure should be performed immediately if life-threatening bleeding occurred.
There were some limitations for the present study. First of all, it was a retrospective study; therefore, selection bias may exist in this study. Then, this study did not utilize randomization and blinding, which may be considered the weakness of this study. Third, this study based on a single-center experience, which may cause representativeness is poor. In addition, the follow-up duration was also relatively short for comparing long-term outcomes.
5. Conclusions
In conclusion, our results showed perioperative data, short-term follow-up effects, and middle-term follow-up effects of LSED group are better than OSED group, except the operation time. The effects of laparoscopic splenectomy and esophagogastric devascularization were better than those for open surgery. LSED is a safe, minimally invasive alternative for patients with portal hypertension and gastroesophageal varices.
Author contributions
Conceptualization: Shunzhen Zheng.
Data curation: Ping Sun.
Formal analysis: Ping Sun.
Investigation: Xihan Liu.
Methodology: Xihan Liu.
Project administration: Jun Liu.
Resources: Guangbing Li.
Software: Guangbing Li, Wei Gong.
Supervision: Wei Gong.
Writing – original draft: Shunzhen Zheng.
Writing – review & editing: Jun Liu.
Footnotes
Abbreviations: EGVB = esophagogastric variceal bleeding, HBV = hepatitis B virus, HCV = hepatitis C virus, LSED = laparoscopic splenectomy and esophagogastric devascularization, LVSS = LigaSure Vessel Sealing System, OSED = open splenectomy and esophagogastric devascularization, PH = portal hypertension, PVST = portal vein system thrombosis.
The authors have no funding and no conflicts of interest to disclose.
References
- [1].Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med 2010;362:823–32. [DOI] [PubMed] [Google Scholar]
- [2].Hong WD, Zhu QH, Huang ZM, et al. Predictors of esophageal varices in patients with HBV-related cirrhosis: a retrospective study. BMC Gastroenterol 2009;9:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].de Franchis R. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol 2010;53:762–8. [DOI] [PubMed] [Google Scholar]
- [4].Tomikawa M, Akahoshi T, Sugimachi K, et al. An assessment of surgery for portal hypertensive patients performed at a single community hospital. Surg Today 2010;40:620–5. [DOI] [PubMed] [Google Scholar]
- [5].Bosch J, Iwakiri Y. The portal hypertension syndrome: etiology, classification, relevance, and animal models. Hepatol Int 2017;12:1–0. [DOI] [PubMed] [Google Scholar]
- [6].Akahoshi T, Uehara H, Tomikawa M, et al. Comparison of open, laparoscopic, and hand-assisted laparoscopicdevascularization of the upper stomach and splenectomy for treatment of esophageal and gastric varices: a single-center experience. Asian J Endosc Surg 2014;7:138–44. [DOI] [PubMed] [Google Scholar]
- [7].Wu YK, Wang YH, Tsai CH, et al. Modified Hassab procedure in the management of bleeding esophageal varices—a two-year experience. Hepatogastroenterology 2002;49:205–7. [PubMed] [Google Scholar]
- [8].Hashizume M, Akahoshi T, Tomikawa M. Management of gastric varices. J Gastroenterol Hepatol 2011;26suppl 1:102–8. [DOI] [PubMed] [Google Scholar]
- [9].Tomikawa M, Hashizume M, Saku M, et al. Effectiveness of gastric devascularization and splenectomy for patients with gastric varices. J Am Coll Surg 2000;191:498–503. [DOI] [PubMed] [Google Scholar]
- [10].Cheng Z, Li JW, Chen J, et al. Therapeutic effects of laparoscopic splenectomy and esophagogastric devascularization on liver cirrhosis and portal hypertension in 204 cases. J Laparoendosc Adv Surg Tech A 2014;24:612–6. [DOI] [PubMed] [Google Scholar]
- [11].Zhan XL, Ji Y, Wang YD. Laparoscopic splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension. World J Gastroenterol 2014;20:5794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Tomikawa M, Akahoshi T, Sugimachi K, et al. Laparoscopic splenectomy may be a superior supportive intervention for cirrhotic patients with hypersplenism. J Gastroenterol Hepatol 2010;25:397–402. [DOI] [PubMed] [Google Scholar]
- [13].Zheng X, Dou C, Yao Y, et al. A meta-analysis study of laparoscopic versus open splenectomy with or without esophagogastric devascularization in the management of liver cirrhosis and portal hypertension. J Laparoendosc Adv Surg Tech A 2015;25:103–11. [DOI] [PubMed] [Google Scholar]
- [14].Cheng LF, Jia JD, Xu XY, et al. Esophagogastric variceal bleeding in cirrhotic portal hypertension: consensus on prevention and management (2008). Chin Med J (Engl) 2009;122:766–75. [PubMed] [Google Scholar]
- [15].Hong D, Cheng J, Wang Z, et al. Comparison of two laparoscopic splenectomy plus pericardial devascularization techniques for management of portal hypertension and hypersplenism. Surg Endosc 2015;29:3819–26. [DOI] [PubMed] [Google Scholar]
- [16].Zou L, Zhang W, Ruan S. Modeling the transmission dynamics and control of hepatitis B virus in China. J Theor Biol 2010;262:330–8. [DOI] [PubMed] [Google Scholar]
- [17].Yu H, Guo S, Wang L, et al. Laparoscopic splenectomy and esophagogastric devascularization for liver cirrhosis and portal hypertension is a safe, effective, and minimally invasive operation. J Laparoendosc Adv Surg Tech A 2016;26:524–30. [DOI] [PubMed] [Google Scholar]
- [18].Moris D, Chakedis J, Rahnemai-Azar AA, et al. Postoperative abdominal adhesions: clinical significance and advances in prevention and management. J Gastrointest Surg 2017;21:1713–22. [DOI] [PubMed] [Google Scholar]
- [19].Zhe C, Jian-wei L, Jian C, et al. Laparoscopic versus open splenectomy and esophagogastric devascularization for bleeding varices or severe hypersplenism: a comparative study. J Gastrointest Surg 2013;17:654–9. [DOI] [PubMed] [Google Scholar]
- [20].Patel AG, Parker JE, Wallwork B, et al. Massive splenomegaly is associated with significant morbidity after laparoscopic splenectomy. Ann Surg 2003;238:235–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Habermalz B, Sauerland S, Decker G, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc 2008;22:821–48. [DOI] [PubMed] [Google Scholar]
- [22].Zheng X, Liu QG, Yao YM. Total laparoscopic versus open splenectomy and esophagogastric devascularization in the management of portal hypertension: a comparative study. Dig Surg 2009;26:499–505. [DOI] [PubMed] [Google Scholar]
- [23].Feldman LS, Demyttenaere SV, Polyhronopoulos GN, et al. Refining the selection criteria for laparoscopic versus open splenectomy for splenomegaly. J Laparoendosc Adv Surg Tech A 2008;18:13–9. [DOI] [PubMed] [Google Scholar]
- [24].Hama T, Takifuji K, Uchiyama K, et al. Laparoscopic splenectomy is a safe and effective procedure for patients with splenomegaly due to portal hypertension. J Hepatobiliary Pancreat Surg 2008;15:304–9. [DOI] [PubMed] [Google Scholar]
- [25].Al-raimi K, Zheng SS. Postoperative outcomes after open splenectomy versus laparoscopicsplenectomy in cirrhotic patients: a meta-analysis. Hepatobiliary Pancreat Dis Int 2016;15:14–20. [DOI] [PubMed] [Google Scholar]


