Abstract
Rationale:
Lactococcus lactis and Pediococcus pentosaceus are rare pathogens which rarely caused infections in humans. Several cases with L. lactis endocarditis have been reported in the literature, among them few were caused by L. lactis subsp. Lactis. Opportunistic P. pentosaceus infections were rarely reported.
Patient concerns:
A 66-year-old man presented to our hospital due to persistent fever for 15 days. A physical checking revealed a grade II holosystolic murmur at the heart apex. A chest computed tomography (CT) scan suggested bronchitis. L. lactis subsp. lactis was identified in blood cultures. Transthoracic and transesophageal echocardiography revealed the presence of a large hyperechogenic mass in the left atrium, and a large floating vegetation on the mitral valve with a severe mitral regurgitation.
Diagnosis:
Infectious endocarditis caused by L. lactis subsp. Lactis was diagnosed.
Interventions:
Levofloxacin (0.5 g/day) was used for 20 days; however, L. lactis subsp. lactis remained to be isolated from blood culture. Therefore, vancomycin (2 g/day) was used to replace levofloxacin. Six days after the treatment with vancomycin, the blood culture revealed no L. lactis subspecies lactis, but yielded a growth of gram-positive and non-spore forming cocci; and P. pentosaceus was identified. Antimicrobial susceptibility test revealed P. pentosaceus was sensitive to penicillin and levofloxacin. Vancomycin was discontinued, and levofloxacin (0.5 g/day) was restarted and treated for another 7 days. The patient recovered with negative blood culture results, and discharged from the hospital.
Outcomes:
The patient recovered with negative blood culture results, and discharged from the hospital.
Lessons:
Our patient had a long-period of antibiotic treatment with strategy alterations. Standard interpretation criteria of Clinical and Laboratory Standards Institute (CLSI) for L. lactis should be established, and molecular tests will increase the identification rate of L. lactis infections.
Keywords: endocarditis, hemoculture, Lactococcus lactis subspecies lactis, levofloxacin, Pediococcus pentosaceus
1. Introduction
Lactococcus lactis (L. lactis), a gram-positive, catalase-negative, and non-motile spherical cocci, which can be found in pairs or short chains.[1]L. lactis includes 3 subspecies: L. lactis subsp. lactis, L. lactis subsp. cremoris, and L. lactis subsp. hordniae; L. lactis subsp. Lactis can be found in raw milk, and has been widely used in fermented dairy products such as cheese. L. lactis subsp. Lactis can be occasionally isolated as a normal flora from the ropharynx, intestine, or vagina.[2,3]Pediococcus pentosaceus (P. pentosaceus) is gram-positive, non-motile, non-spore forming cocci.[4]P. pentosaceus is commonly found in fermented plants such as pickled vegetables and silages.[5,6] Both L. lactis subsp. lactis and P. pentosaceus can cause opportunistic infections in immunocompromised hosts. Several cases with L. lactis endocarditis have been reported in the literature, among them few were caused by L. lactis subsp. Lactis.[6–11] Opportunistic P. pentosaceus infections were rarely reported.[12] We herein describe a patient with endocarditis caused by L. lactis subsp. lactis and P. pentosaceus treated with antibiotics successfully. To our knowledge, this is the first case with endocarditis caused by L. lactis subsp. lactis in China.
2. Case report
A 66-year-old man presented to our hospital due to persistent fever for 15 days. His medical history included hypertension for 20 years, cerebral hemorrhage, coronary heart disease, cerebral infarction and Alzheimer disease. On admission, he had a body temperature of 38.2 °C, 24 breaths per minute, heart rate 106 /min, blood pressure 139/77 mmHg, and degree of blood oxygen saturation, 97%. A physical checking revealed a grade II holosystolic murmur at the heart apex. No Janeway lesions, splinter hemorrhages, conjunctival hemorrhage, or Osler nodules were noted. Initial laboratory examination showed a white blood cell count of 16,690/uL, with a neutrophils ratio of 71.5%, hemoglobulin of 129 g/L and erythrocyte sedimentation rate of 62 mm/h. Urine analysis and other biochemistry tests results were all normal. A chest computed tomography (CT) scan suggested bronchitis. Blood cultures were taken on the first day of admission. All the 3 sets of blood drawn from 3 different sites showed growth of gram-positive, catalase-negative, and non-motile coccus. L. lactis subsp. lactis was identified using a VITEK-2 Compact automatic microorganism identification and drug susceptibility analysis system (BioMerieux, France). Drug susceptibility analysis results showed L. lactis subspecies lactis was susceptible to penicillin, ampicillin, tetracycline, vancomycin, linezolid, and levofloxacin; while resistant to erythromycin, ceftriaxone, and clindamycin; and mesomeric to gentamicin. Based on these results, the patient was started on levofloxacin (0.5 g/day). Penicillin was not used for this patient due to a history of drug anaphylaxis. On the third day after hospitalization, an ultrasonic cardiogram indicated that indicated an ejection fraction of 65%, and left heart dilatation with a mitral valve. Transthoracic and transesophageal echocardiography revealed the presence of a large hyperechogenic mass in the left atrium, and a large floating vegetation on the mitral valve with a severe mitral regurgitation. The patient was diagnosed with infectious endocarditis. The infection may be opportunistic because the patient was an immunocompromised old man with many underlying diseases.
L. lactis subsp. lactis remained to be isolated from blood culture after 20 days of levofloxacin treatment; therefore, vancomycin (2 g/day) was used to replace levofloxacin. Six days after the treatment with vancomycin, the blood culture revealed no L. lactis subspecies lactis, but yielded a growth of gram-positive and non-spore forming cocci; and P. pentosaceus was identified. Antimicrobial susceptibility test revealed P. pentosaceus was sensitive to penicillin and levofloxacin. Vancomycin was discontinued, and levofloxacin (0.5 g/day) was restarted and treated for another 7 days. The patient recovered with negative blood culture results, and discharged from the hospital. He was lost to follow-up after 6 months; echocardiography revealed that the size of mitral vegetation reduced in the last follow-up.
The routine isolation and identification of these bacteria were performed in accordance with the Clinical and Laboratory Standards Institute (CLSI). The research was approved by the Ethics Committee of Liaocheng People's Hospital, Liaocheng, Shangdong Province, China. A written informed consent was obtained from the patient's guardian for reporting the case details.
3. Discussion
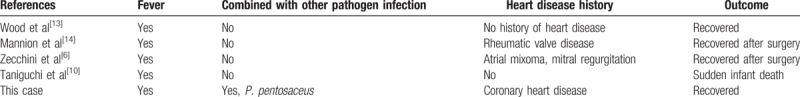
L. lactis is a gram-positive coccus, which is generally considered to be a pathogen with low virulence. Ten cases with L. lactis endocarditis have been reported in the literature, and among them 5 were infected with L. lactis subsp. lactis (Table 1).[6–10] All the L. lactis subsp. lactis infected cases presented with fever and 60% of them had a history of coronary heart diseases. Most of the cases had underlying diseases. Most were successfully treated with amoxicillin and clavulanate, except 2 cases died (1 due to sudden infant death and other due to intracerebral hemorrage). Infectious endocarditis caused by L. lactis lacks a standard antimicrobial therapy strategy due to few susceptibility data of this bacteria. Formal CLSI criteria for antibiotics use has not been defined yet. In clinical practice, antibiotics are empirically given before culture results became available, or chosen based on drug-sensitivity results; penicillin and the third-generation cephalosporin combined with gentamicin are the most common choice for L. lactis infections.
Table 1.
L. lactis subsp. Lactis related endocarditis cases through a PubMed search.
In our patient, the results of hemoculture and drug-sensitive tests indicated that L. lactis subsp. lactis was sensitive to penicillin, vancomycin, linezolid, and levofloxacin. However, penicillin cannot be used due to anaphylaxis, so we used levofloxacin for treatment. Clinical symptoms improved, but blood cultures were still positive for L. lactis after 3 weeks of levofloxacin treatment. Considering inefficacy of levofloxacin, vancomycin was administered for this patient. Further blood culture showed negative results for L. lactis subsp. Lactis, but a growth of P. pentosaceus isolated.
P. pentosaceus is a lactic acid bacteria and used in biotechnology and food industry. In previous studies, the P. pentosaceus was considered nonpathogenic. Some species including P. acidilactici and P. Pentosaceus can cause infection have been reported recently. Up to now, only 1 case of endocarditis was reported.[11] In China, P. pentosaceus was once separated in the sputum of a patient with long-term antituberculosis treatment with rifampicin and streptomycin, bringing in flora imbalance in partes oralis.[12] Iwen et al indicated that daptomycin can be used to treat endocarditis caused by Pediococcus species.[11]P. pentosaceus is naturally resistant to vancomycin, therefore, vancomycin was stopped and levofloxacin was re-started for the patient.[11]
In conclusion, endocarditis co-infected by L. lactis subspecies lactis and P. pentosaceus was rare except for those who were immunocompromised.[11] Although L. lactis subspe. lactis and P. pentosaceus had low pathogen virulence and fine response to antibacterials, endocarditis caused by L. lactis was still severe. Two cases of deaths L. lactis subsp. lactis endocarditis were reported in 2 previous studies.[10,11] Our patient had a long-period of antibiotic treatment with strategy alterations. Standard interpretation criteria of CLSI for L. lactis should be established, and molecular tests will increase the identification rate of L. lactis infections.
Acknowledgments
Thank you.
Author contributions
Conceptualization: Zhigang Zhang.
Data curation: Fei Chen.
Formal analysis: Fei Chen.
Project administration: Zhigang Zhang.
Supervision: Jianzhong Chen.
Writing – original draft: Jianzhong Chen.
Footnotes
Abbreviations: CLSI = Clinical and Laboratory Standards Institute, CT = computed tomography, L. lactis = Lactococcus lactis, P. pentosaceus = Pediococcus pentosaceus.
The authors have no conflicts of interest to disclose.
References
- [1].Mori S, Mori K, Suzuki I, et al. Phylogenetic analysis of Lactococcus lactis subspecies based on decoding the sequence of the pepT tripeptidase gene, the pepV dipeptidase gene and 16S rRNA. Syst Appl Microbiol 2004;27:414–22. [DOI] [PubMed] [Google Scholar]
- [2].Schlundt J, Saadbye P, Lohmann B, et al. Conjugal transfer of plasmid DNA between lactococcus lactis strains and distribution of transconjugants in the digestive tract of gnotobiotic rats. Microb Ecol Health Dis 1994;7:59–69. [Google Scholar]
- [3].Akhaddar A, El Mostarchid B, Gazzaz M, et al. Cerebellar abscess due to lactococcus lactis. A new pathogen. Acta Neurochir (Wien) 2002;144:305–6. [DOI] [PubMed] [Google Scholar]
- [4].Department of Energy Joint Genome Project. 2001-2006 The Regents of the University of California. 01 May 2007. http://genome.jgi-psf.org/finished_microbes/pedpe/pedpe.home.html Accessed Nov 7, 2018). [Google Scholar]
- [5].Finegold SM, Sutter VL, Mathisen GE. Normal indigenous intestinal flora. New York: Academic Press; 1983. [Google Scholar]
- [6].Zechini B, Cipriani P, Papadopoulou S, et al. Endocarditis caused by lactococcus lactis subsp. Lactis in a patient with atrial myxoma: a case report. Diagn Microbiol Infect Dis 2006;56:325–8. [DOI] [PubMed] [Google Scholar]
- [7].Rostagno C, Pecile P, Stefano PL. Early lactococcus lactis endocarditis after mitral valve repair: a case report and literature review. Infection 2013;41:897–9. [DOI] [PubMed] [Google Scholar]
- [8].Aguirre M, Collins MD. Lactic acid bacteria and human clinical infection. J Appl Bacteriol 1993;75:95–107. [DOI] [PubMed] [Google Scholar]
- [9].Lin KH, Sy CL, Chen CS, et al. Infective endocarditis complicated by intracerebral hemorrhage due to lactococcus lactis subsp. Cremoris. Infection 2010;38:147–9. [DOI] [PubMed] [Google Scholar]
- [10].Taniguchi K, Nakayama M, Nakahira K, et al. Sudden infant death due to Lactococcal infective endocarditis. Leg Med (Tokyo) 2016;19:107–11. [DOI] [PubMed] [Google Scholar]
- [11].Iwen PC, Mindru C, Kalil AC, et al. Pediococcus acidilactici endocarditis successfully treated with daptomycin. J Clin Microbiol 2012;50:1106–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen DK, Sun CG. Testing and profiles of practical clinical microbiology. Beijing: People's Medical Publishing House; 2011. [Google Scholar]
- [13].Wood HF, Jacobs K, McCarty M. Streptococcus lactis isolated from a patient with subacute bacterial endocarditis. Am J Med 1955;18:345–7. [DOI] [PubMed] [Google Scholar]
- [14].Mannion PT, Rothburn MM. Diagnosis of bacterial endocarditis caused by Streptococcus lactis and assisted by immunoblotting of serum antibodies. J Infect 1990;21:317–8. [DOI] [PubMed] [Google Scholar]


