Abstract
There are no specific treatment drugs and vaccine for Hand Foot and Mouth Disease (HFMD). Taking effective preventive measures is particularly important for control of HFMD infection. The objective of this study is to evaluate the effect of intervention of intensive education on hand hygiene on HFMD.
We randomized 64 villages into intervention and control groups in Handan, Hebei province, China. Parents and caregivers of children 6 to 40 months age group in intervention villages received intensive education on hand hygiene. Control group received general education. The intervention period was from April 1 to July 31, 2011 and April 1 to July 31, 2012. We measured and compare the knowledge and incidences of HFMD between 2 groups.
We collected 6484 questionnaires, including 3583 in the intervention group [response rate: 96% (3583/3726)] and 2901 in the control group [response rate: 90% (2901/3224)]. We observed that hand washing habit of children and parent, knowledge of HFMD of parents, children's daily cleaning habits scores improved in the intervention group and higher than that in the control group at both the end of year 1 (April 1–July 31, 2011)and year 2 (April 1–July 31, 2012). The incidence of HFMD (2.1%) in intervention group was significantly lower than that in control group (4.2%) at year 2 (χ2 = 22.138, P <.001). The positive percent of coli-form on the hand swabs in intervention group (2.00%) were significantly lower than that in control group (9.45%) at the end of year 2.
The intervention of intensive education on hand hygiene effectively improved the personal hygiene both of children and parents, as well as reduced the incidence of HFMD. We suggested expanding the intervention measures in community to prevent HFMD.
Keywords: community trial, foot and mouth disease, hand, intervention
1. Introduction
Hand, foot, and mouth disease (HFMD) is a common infectious disease caused by various Enteroviruses (such as Coxsackievirus A16, other Coxsackieviruses, and Enterovirus 71 [EV71]), which primarily affects infants and children under 5 years of age.[1] It is usually a mild and self-limiting disease; however, recently many severe HFMD outbreaks caused by EV71 have occurred worldwide. These outbreaks are characterized by high numbers of neurological complications, which often led to death or permanent paralysis, causing significant concerns in the public health community.[2] Up to now, no specific treatment or vaccine is currently available for HFMD.
Studies conducted in China and Korea have identified risk factors for HFMD, including low socioeconomic status, existence of open-air defecation, poor sewage treatment, poor hand-washing and other poor personal hygienic habits (such as biting fingers).[3–8] Among these factors, open-air defecation and poor sewage treatment usually require expensive social engineering solutions, whereas risk factors such as hand-washing and other personal hygienic habits may be achieved by low-cost measures such as health education.
Observational studies have strongly shown the association between poor hand-hygiene and HFMD.[5–7] However, no interventional studies have been conducted to verify this association. In 2011, we conducted a community-based trial to evaluate the effect of intervention of intensive education on hand hygiene on HFMD, and to provide scientific evidence for developing strategies for preventing and controlling HFMD.
2. Methods
This study was approved by the Institutional Review Board of Hebei Center for Disease Control and Prevention, China. The institutional review board stated that written consents from patients were not required for this study because the identification numbers and personal information about participants were not included in the secondary files. All participants provided their verbal, informed consent.
We conducted an intervention trial in rural areas in Handan Prefecture, Hebei Province in Northeastern China. In 2010, the Prefecture had an estimated population of 8900000 persons. The attack rate among children 6 to 40 months age group was1652/100000 which was higher than that in other age groups in 2010. So we targeted the intervention at children in the 6 to 40 months age group because of their susceptibility to HFMD. For feasibility reasons, and to minimize cross-contamination of intervention effect, the intervention was administered at the village level rather than at sub-village levels.
We selected 4 counties with the highest incidences of HFMD during 2009 to 2010 in the prefecture as the study sites. Before intervention in 2010, the incidence of HFMD among target children in these 4 countries was about 5%, based on the data from the national notifiable disease surveillance system, which had made HFMD a notifiable disease in 2008. Expecting that the intervention would reduce the incidence by 30%, with α = 0.05 and a power of 90%, we calculated that each group would need 2900 children to participate. Assuming a 10% dropout rate, the sample size for each group would be about 3190 children.
Census and childhood immunization data showed that in Handan Prefecture, each administrative village had an average of about 500 residents, and each household had an average of 0.2 children in the targeted age group. Therefore, each group would need 30 (=3190/0.2/500) administrative villages. We random chose 64 administrative villages from all the 483 villages whose incidence rates were in the mid-pack in the 4 countries, that is, 3% to 10%, to participate in this study. Those 64 villages were randomized into intervention and control groups; each group had 32 villages.
Parents and caregivers in the 32 intervention villages received intensive education on hand hygiene. Posters on hand-washing were posted on every street corner and popular gathering places; messages describing the importance and correct procedures of hand-washing were written on the villages’ information blackboards and broadcasted over the radio station of the villages. Brochures and leaflets on preventing HFMD were distributed to all parents in the intervention villages. Also, the Prefecture's Center for Disease Control and Prevention conducted train-the-trainer sessions for all village doctors on knowledge of HFMD and correct hand-washing methods. The village doctors were then asked to train the parents in their villages. The specific training received by the village doctors, who then trained the parents, included the following:
-
1)
Six steps of hand washing;
-
2)
When hand-washing is needed;
-
3)
Preparation of separate towels for each child and boiling them at least once a week;
-
4)
Preparation of separate eating utensils for each child;
-
5)
Cleaning of toys at least once a week, when being taken back home or after sharing with other children;
-
6)
Minimizing outside activities for sick children with respiratory disease, gastrointestinal disease, or HFMD, and keeping the sick children at home as much as possible. All of the intervention messages we used were taken from the official website of China center for disease control and prevention.
Parents in the 32 control villages received general health education that was implemented in the whole prefecture, which included: general knowledge of hand-washing, drinking boiled water, and avoiding activities in the crowded places.
The intervention was implemented in 2 consecutive HFMD epidemic seasons (i.e., April 1–July 31) in 2011 and 2012, respectively with the same method of intervention.
2.1. Questionnaire and data collection
We designed a standardized questionnaire to collect the following information from target children parents by face to face interviewing: demographic information, health conditions and family water conditions, the behavior of washing their hand among parents and children, the habits of cleaning children's toys and daily necessities, the knowledge of HFMD among parents, the history of HFMD among children.
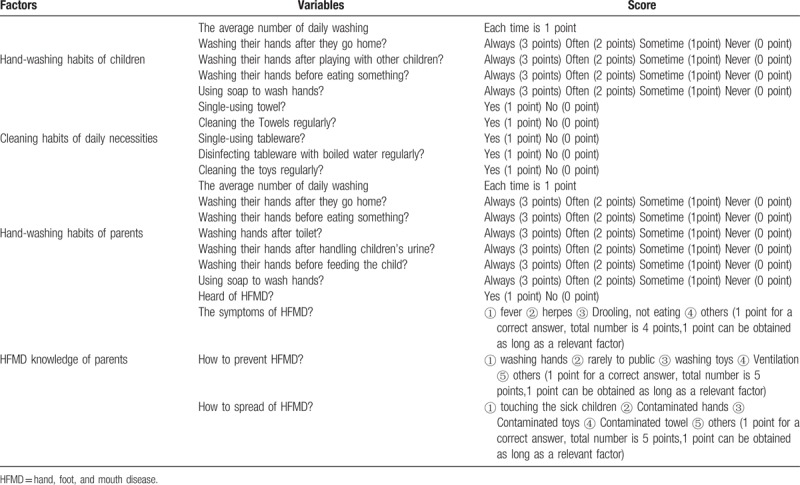
The scores given for each question were shown in Table 1. We computed a hand-washing score and a cleaning habit score for each child; and a hand-washing and an HFMD knowledge score for each caregiver of the child. For hand-washing habits of children, cleaning habits of daily necessities and hand-washing habits of parents, the higher score they got the better health habit they had. For the HFMD knowledge of parents, all the options for each question were correct. The subject will get 1 point once he choice 1 option. He will get more points if he could choice more options. The maximum points were 4 or 5.
Table 1.
The score assignment for the hand washing and HFMD knowledge.
Before the intervention, a baseline survey was conducted in both intervention and control villages on children's hand-washing habits and parents’ knowledge for HFMD. The village doctors collected the information with a standard questionnaire by interviewing children's parents in person. At the end of each intervention period, the same survey was repeated.
During intervention periods, the village doctors collected data on respiratory symptoms, gastroenteritis symptoms and symptoms of HFMD among children and their family members weekly, either by telephone or in person. Respiratory symptoms include a high fever, usually with a temperature higher than 38°C, and 1 or 2 symptoms such as headache, nasal discharge, cough, and sore throat. Gastrointestinal symptoms were defined as persistent or intermittent abdominal pain for more than 24 hours, diarrhea for more than 3 times in 24 hours, and vomiting more than for 3 times in 24 hours, 1 of which was monitored. A HFMD case was defined as onset with fever and rash on hand, food or mouth.
In addition to the questionnaire survey, the village doctors randomly selected 100 households before, during, and at the end of each of the 2 intervention periods, and swabbed the hands of the children and their parents (or caregivers). The hand swabs were cultured for coliform bacteria at the laboratory of the Prefecture's Center for Disease Control and Prevention.
2.2. Data analysis
We analyzed the effect of the intervention by using multivariable linear regression. The stepwise method is used to analyze the multivariate linear regression. The dependent variable was the score of hand-washing habit of the child, the score of daily cleaning habit of the child, the score of the hand-washing habit of the parents or caregivers, the knowledge score of HFMD of the parents. We selected the following independent variables based on the literatures which showed the influence factors of HFMD: variables which are relevant to immune (age and gender), health condition (family income, water source, outdoor toilets, and sewage ditch around the house), health habit (degree of education, intervention) and history of HFMD. We compared the percentages of gastrointestinal symptoms, respiratory symptoms and HFMD between intervention and control group by χ2 test. We compared the coliform-positive rates of hand swabs between the subjects in intervention and control groups by χ2 test before, during and after the intervention.
3. Results
In the baseline survey, 32 intervention villages and 31 control villages participated. We collected 6484 questionnaires, including 3583 in the intervention group [response rate: 96% (3583/3726)] and 2901 in the control group [response rate: 90% (2901/3224)]. Based on these questionnaires, the average age of the child in control group was 22.50 ± 8.4 months, compared to 22.46 ± 8.5 months in intervention group (t = 0.190, P = .850). 87% of the parents in the intervention group had a secondary school or higher education; compared to 88% in the control group (x2 = 0.2, P = .658). There was no significant statistical difference between 2 groups for hygienic risk factors such as having a private well as water source, having outdoor toilets, presence of sewage ditch around the house (Table 2).
Table 2.
Comparison of reported risk factors, hand washing and HFMD knowledge scores between intervention and control groups in the baseline survey.
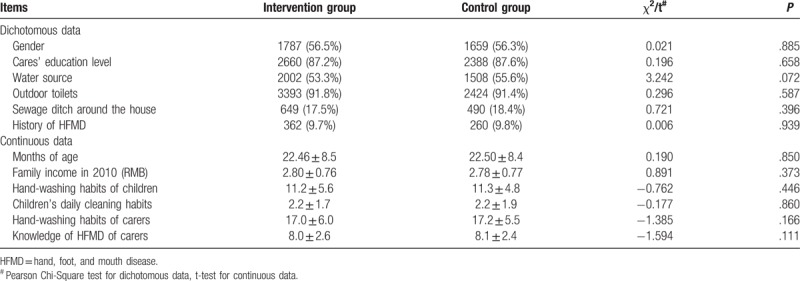
Before intervention, the 2 group had nearly identical average hand-washing scores of children (11.2 for intervention group vs 11.3 for control group; t = −0.762, P = .446), hand-washing scores of parents/caregivers (17.0 for intervention group vs 17.2 for control group; t = −1.385, P = 0.166), knowledge scores on HFMD of parents/caregivers (8.0 for intervention group vs 8.1 for control group; t = −1.594, P = .111), and children's daily cleaning habits scores (2.2 for intervention group vs 2.2 for control group; t = −0.177, P = .860) (Table 2).
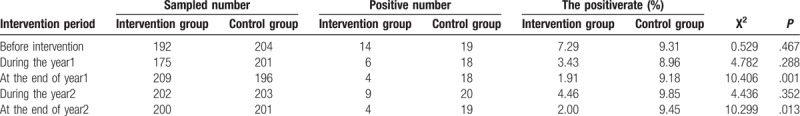
Before the intervention, the positivity rates of coliform bacteria in hand swabs for the children and their caregivers did not differ significantly between the intervention group and the control group (7.3% vs 9.3%, χ2 = 0.529, P = .467).
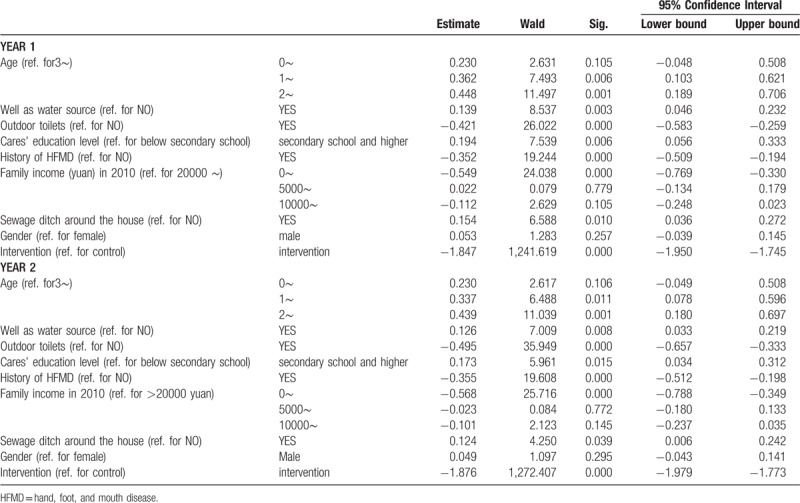
3.1. Scores of hygienic habits and knowledge of HFMD
The result of multivariable linear regression analysis is shown in Tables 3 to 6. Take the scores of hand-wasing habit of children at the end of year 1 for example, in the case of adjusting other variables, compared to the control group, the probability of intervention group's score reduced at least 1 level was 0.158 times (exp(−1.847)). It means that interventions can improve and maintain high scores of hand-wasing habit of children. This explanation applies to other coefficients in Table 3 and Table 5. For the HFMD knowledge's score of parents, control group seems more likely to get a high score, compared to the intervention group.
Table 3.
The Children's daily cleaning habits of multiple linear regression at the end of year 1 and year 2.
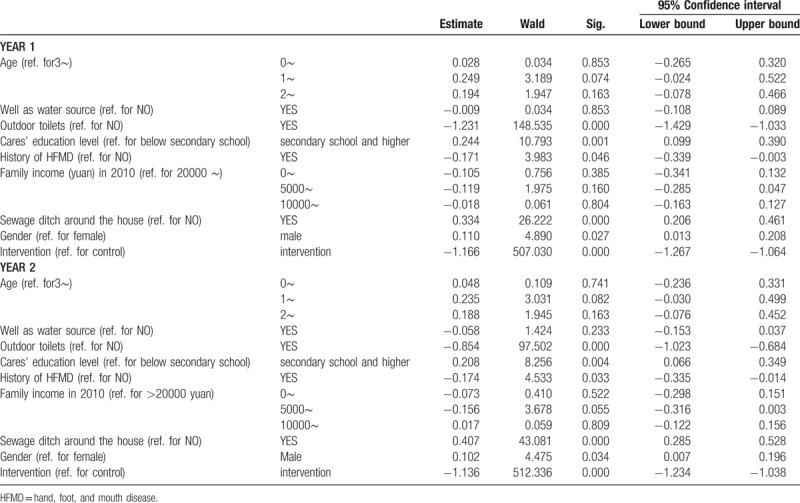
Table 6.
Knowledge of HFMD of parents of multiple linear regression at the end of year 1 and year 2.
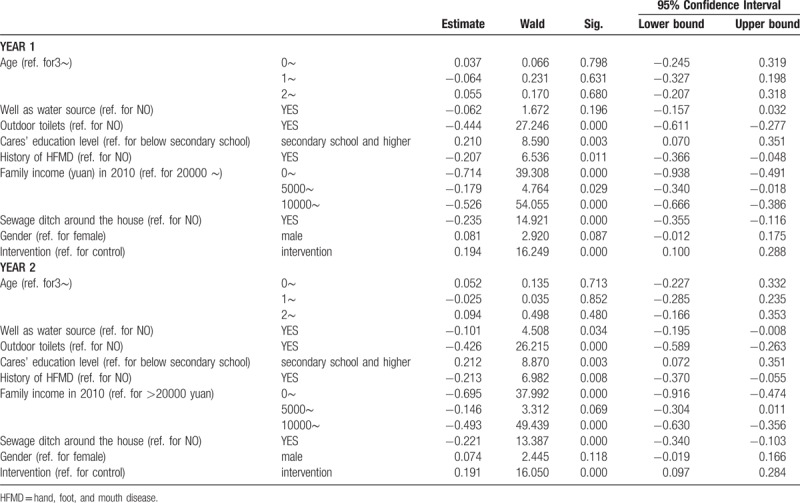
Table 5.
Hand-washing habits of parents of multiple linear regression at the end of year 1 and year 2.
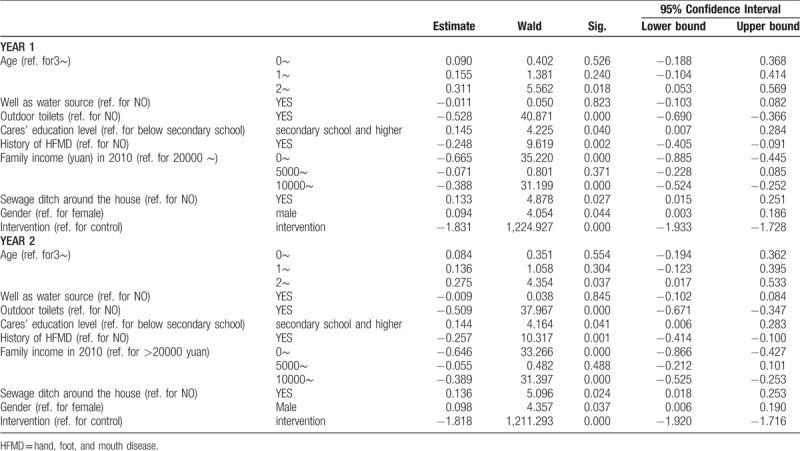
Table 4.
Hand-washing habits of children of multiple linear regression at the end of year 1 and year 2.
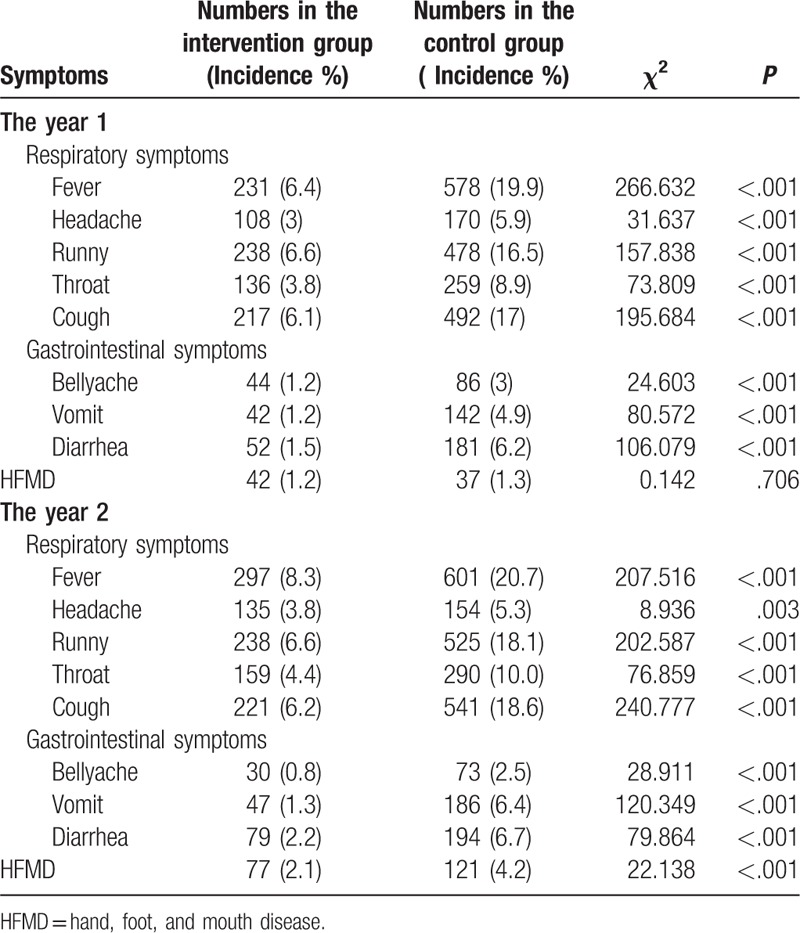
3.2. Respiratory symptoms, gastrointestinal symptoms, and HFMD
At the end of year 1, the incidence rates of respiratory-related symptom including fever (6.4%), headache (3.0%), runny nose (6.6%), throat (3.8%), and cough (6.1%) in the intervention group were all significantly lower than those in the control group (19.9%,5.9%,16.5%,8.9% and 17%, respectively). the incidence rates of gastrointestinal-related symptom including bellyache (1.2%), vomit (1.2%), and diarrhea (1.5%) in the intervention group were all significantly lower than those in the control group (3.0%,4.9%, and 6.2%, respectively). The incidence of HFMD was 1.2% in intervention group, a little lower than that in control group (1.3%)(P = .706). At the end ofyear2 the incidence rates of respiratory-related symptom including fever (8.3%), headache (3.8%), runny nose (6.6%), throat (4.4%), and cough (6.2%) in the intervention group were all significantly lower than those in the control group (20.7%,5.3%,18.1%,10.0%, and 18.6%, respectively). the incidence rates of gastrointestinal-related symptom including bellyache (0.8%), vomit (1.3%), and diarrhea (2.2%) in the intervention group were all significantly lower than those in the control group (2.5%,6.4%, and 6.7%, respectively). The incidence of HFMD in intervention group was significantly lower than that in the control group (2.1% vs. 4.2%, P = .000) (Table 7).
Table 7.
Incidences in intervention group and control group at the end of year 1 and year 2.
3.3. Positive rate of Coliform bacteria
The positive rates of Coliform bacteria were significantly lower in the intervention group than in the control group during (3.4% vs 9.0%, P = .288) and at the end of year 1 (1.9% vs 9.2%, P = .001). Similarly, the positive rates in the intervention group were significantly lower than in control group during (4.5% vs 9.9%) and at the end of year 2 (2.0% vs 9.5%) (Table 8).
Table 8.
The positive rate of Coli-form bacteria in hand swab specimens before, during and after intervention.
4. Discussion
We conducted an intervention study to evaluate the effect of intensive education on hand hygiene on prevention HFMD in Handan, Hebei province, China from 2010 to 2013. The result showed that the intervention measures could improve the hand washing habit in both children and parents, children hygiene habit, HFMD knowledge in parents after intervention period. It also decreased the incidences of respiratory and intestinal related symptoms among children and their family members. The hands in intervention group were less contaminated with col-form bacteria than I control group after intervention. Importantly, through repeated intervention, the incidence of HFMD was markedly reduced.
HFMD could cause severe disease such as central nervous system, respiratory system damage which caused widespread concern in the community. Because there is no effective vaccine, therefore, strengthening the HFMD knowledge for children and parents, and promoting them to develop healthy behavior is necessary. We showed the effect of the intensive education on hand hygiene on preventing HFMD in this study from the knowledge, behavior, disease incidence, and hand contamination status. These measures are easy to be implemented and could be used widely in communities in the future.
This study included 2 stages. At the end of year 1, the HFMD knowledge, hand washing habits, and hygiene habit were all improved, but the HFMD incidence did not decrease significantly. However, at the end of year 2, the HFMD incidence in the intervention group was lower significantly than that in control group. That means the ongoing intervention was important to achieve the objective of decreasing HFMD among children. We suggested expanding the intervention measures in community to prevent HFMD. On the other hand, it was estimated that the incidence rate of HFMD were122.54/100 000 in 2010, 34.90/100 000 in 2011 and 97.01/100 000 in 2012 in Handan City, respectively. It was possible that any intervention will not expect to have a very significant effect because of a relatively mild epidemic in 2011.
Our study had some limitations. One major limitation was that this study used various interventions, that is, hand-washing and other hygienic improvement measures. Therefore, our study could not demonstrate whether it was hand-washing alone that reduced the symptoms, and it was not possible to know which intervention worked. It was difficult to use blind method in this community trial, which was the second limitation. And the control group might receive intervention measures in some degree, that is, posters, broadcasted over the radio station from the neighboring, intervention group villagers, which would reduce the study effects. The results would show bigger difference if the control group did not receive any intervention measures.
Author contributions
NG and HM have contributed equally to this work. Conception and design: NG, JD, HM and LZ; administrative support: JD; collection and assembly of data: all authors; data analysis and interpretation: NG, YM, HM and LZ; manuscript writing: NG, JD and LZ; and final approval of manuscript: all authors.
Conceptualization: Lijie Zhang.
Data curation: Nana GUO, Huilai MA, Jian Deng, Yanxia MA, ruiling GUO, Lijie Zhang.
Formal analysis: Huilai MA, Jian Deng, Lijie Zhang.
Funding acquisition: Lijie Zhang.
Investigation: Nana GUO, Huilai MA, Jian Deng, Yanxia MA, Liang HUANG, ruiling GUO, Lijie Zhang.
Methodology: Nana GUO, Liang HUANG, Lijie Zhang.
Project administration: Lijie Zhang.
Resources: Lijie Zhang.
Software: Huilai MA, Yanxia MA, Lijie Zhang.
Writing – original draft: Nana GUO, Jian Deng, Lijie Zhang.
Writing – review & editing: Lijie Zhang.
Footnotes
Abbreviations: EV71 = Enterovirus 71, HFMD = hand, foot, and mouth disease.
NG and HM contributed equally to this article.
The authors have no conflicts of interest to disclose.
References
- [1].Wen-bo XU. Epidemiological characteristics and control strategy of HFMD. J Exp Clin Virol 2007;21:3. [Google Scholar]
- [2].Hongmei Guo, Qirong Zhu. Enterovirus 71 infection of the nervous system[J]. Foreign Med (Infect Dis Epidemiol Branch) 2002;29:19–21. [Google Scholar]
- [3].Wang Lai, Yichuan Li. Hand foot and mouth disease epidemiology and preventive measures. Anhui Med 2010;14:112–3. [Google Scholar]
- [4].Lijun Cai. Hand foot and mouth disease popular trend. Pediatr Pharma 2008;14:64–6. [Google Scholar]
- [5].Park SK, Park B, Kim H, et al. Transmission of seasonal outbreak of childhood enteroviral aseptic meningitis and Hand-foot-mouth disease. J Korean Med Sci 2010;25:677–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].RuNing Guo, Zhengmin Zhang, Fen Yang, et al. Study the epidemiological characteristics of HFMD and risk factors in Guangdong Province. Chin J Epidemiol 2009;30:530. [Google Scholar]
- [7].Wenti Xu, Lu Gao, Ying Zhang, et al. Control study of the risk factors in HFMD children in Tianjin. Chin J Epidemiol 2009;30:100. [Google Scholar]
- [8].Guixuan Xiao, Yang Kun, Wuyuan Liu, et al. The evaluation of health education on controlling intestinal infectious diseases. Chin Public Health Manag 2008;24:423–6. [Google Scholar]
- [9].Carabin H, Gyorkos TW, Soto JC, et al. Effectiveness of a training program in reducing infections in toddlers attending day care centers. Epidemiology 1999;10:219–27. [PubMed] [Google Scholar]
- [10].Dyer DL, Shinder A, Shinder F. Alcohol-free instant hand sanitizer reduces elementary school illness absenteeism. Fam Med 2000;32:633–8. [PubMed] [Google Scholar]
- [11].Falsey AR, Criddle MM, Kolassa JE, et al. Evaluation of a handwashing intervention to reduce respiratory illness rates in senior day-care centers. Infect Control Hosp Epidemiol 1999;20:200–2. [DOI] [PubMed] [Google Scholar]
- [12].Larson EL, Lin SX, Gomez-Pichardo C, et al. Effect of antibacterial home cleaning and handwashing products on infectious disease symptoms: a randomized, double-blind trial. Ann Intern Med 2004;140:321–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Luby SP, Agboatwalla M, Feikin DR, et al. Effect of handwashing on child health: a randomised controlled trial. Lancet 2005;366:225–33. [DOI] [PubMed] [Google Scholar]
- [14].Ponka A, Poussa T, Laosmaa M. The effect of enhanced hygiene practices on absences due to infectious diseases among children in day care centers in Helsinki. Infection 2004;32:2–7. [DOI] [PubMed] [Google Scholar]
- [15].Roberts L, Smith W, Jorm L, et al. Effect of infection control measures on the frequency of upper respiratory infection in child care: a randomized, controlled trial. Pediatrics 2000;105:738–42. [DOI] [PubMed] [Google Scholar]
- [16].Ryan MA, Christian RS, Wohlrabe J. Handwashing and respiratory illness among young adults in military training. Am J Prev Med 2001;21:79–83. [DOI] [PubMed] [Google Scholar]
- [17].Sandora TJ, Taveras EM, Shih MC, et al. A randomized, controlled trial of a multifaceted intervention including alcohol- based hand sanitizer and hand-hygiene education to reduce illness transmission in the home. Pediatrics 2005;116:87–94. [DOI] [PubMed] [Google Scholar]
- [18].White C, Kolble R, Carlson R, et al. The effect of hand hygiene on illness rate among students in university residence halls. Am J Infect Control 2003;31:364–70. [DOI] [PubMed] [Google Scholar]
- [19].Chang LY, Tsao KC, Hsia SH, et al. Transmission and clinical features of enterovirus 71 infections in household contacts in Taiwan. JAMA 2004;291:222–7. [DOI] [PubMed] [Google Scholar]
- [20].Haamann P, Kessel L, Larsen M. Monofocal outer retinitis associated with hand, foot, and mouth disease caused by coxsackievirus. Am J Ophthalmol 2000;129:552–3. [DOI] [PubMed] [Google Scholar]
- [21].Mori M, Takagi K, Kuwabara S, et al. Guillain-Barre syndrome following hand-foot-and-mouth disease. Intern Med 2000;39:503–5. [DOI] [PubMed] [Google Scholar]
- [22].Yan-ting LI. Epidemiological characteristics and the prevention and control of HFMD. Shanghai Prevent Med 2008;20:316–7. [Google Scholar]


