Abstract
Background:
To investigate the effectiveness of Baduanjin qigong combined with cognitive-behavior therapy (CBT) on the physical fitness and psychological health of elderly housebound.
Materials and methods:
The 120 elderly housebound were randomly divided into 3 intervention groups: Baduanjin training, Baduanjin training combined with CBT, and CBT. The interventions were conducted by means of home visits over 6 months. Spirometry, SF-36 health survey of quality of life, and Lawton and Brody Instrumental Activities of Daily Living Scale (IADL) were used to collect physical health data, and self-evaluation of overall health status, self-evaluation of loneliness, and short-form geriatric depression scale (GDS-15) were used to collect mental health data at baseline, 3 months, and 6 months after intervention. Data was analyzed by repeated measures analysis of variance (rANOVA) and chi-squared test (χ2 test).
Results:
Forced vital capacity (FVC), maximum voluntary ventilation (MVV), quality of life (QOL), and self-reported health status were significantly increased (P < .05) in the group receiving joint Baduanjin and CBT intervention at 3 months and 6 months, as compared to the Baduanjin only group or the CBT only group. Activities of daily living (ADL), self-evaluated loneliness, and level of depression were significantly lowered (P < .05) in the group receiving joint Baduanjin and CBT intervention at 3 months and 6 months, as compared to the Baduanjin only group or the CBT only group.
Conclusions:
Physical and psychological statuses of elderly housebound were significantly improved by Baduanjin training combined with CBT. The effect of the combined intervention exceeded that of CBT or Baduanjin alone.
Keywords: baduanjin qigong, cognitive-behavioral therapy, elderly housebound
1. Introduction
As the aging situation in China intensifies, the number of elderly housebound also increases. The incidence of elderly housebound in northeastern China has reached 18.9% in 2011.[1] The state of being housebound greatly reduces the scope of activities of daily living (ADL), decreases the level of physical activity and cardiorespiratory function, and can even lead to physical disability and disuse syndrome.[2] Persistent housebound status is also closely related to the incidence of Alzheimer disease.[1] Housebound means social isolation and lack of social support.[3] Socially isolated and lacking adequate care, the risk of depression among elderly housebound is significantly higher than that of their peers.[4] The majority of elderly living with depression experience depressed moods and pessimism, do not have personal hobbies, and do not go outside due to fear of contracting disease, which results in reduced social interactions, loss of mental orientation, increased feelings of loss and loneliness, and a greater incidence of bedridden elderly.[5,6] With the increase of the elderly population, the incidence of elderly housebound, bedridden elderly, and elderly with dementia will continue to increase, which not only threatens health in the elderly but also poses a heavy burden for families and the society.[2]
Cognitive-behavioral therapy (CBT) is a group of short-term psychotherapeutic approaches to eliminate negative emotions and behaviors by the changing of mindsets and behaviors. It can be used to correct negative automatic thinking and disorders of consciousness and change patient behavior patterns on specific related issues.[7,8] CBT has been applied to improve mental health, including depression, anxiety, and schizophrenia,[9,10] and physical health, including chronic pain, cancer, and Parkinsonism.[11,12] The incidence of depression in Chinese elderly housebound was 36.4% in 2010,[13] and self-reported loneliness reached 39.18% in 2009[14] which signifies that the elderly housebound are a high-risk population for psychological disorders. At present, CBT is a widely used intervention for psychological health in housebound individuals.[15–17] Although remote CBT is simple to administer, research showed that it has low participation from low-income elderly.[18]
Baduanjin qigong is a Chinese traditional exercise that combines human physical activity with breathing regulation and psychological adjustment. At present, Baduanjin training has been effective in the prevention and treatment of stroke risk factors, and it was recommended to be included in stroke prevention programs.[14] Research shows that it reduced the incidence of elderly constipation,[19] assisted in type 2 diabetes glycemic control,[20] and improved pulmonary function in elderly with COPD. As of 2010, about 20% of the total number of elderly people in mainland China are housebound, with similar physical and psychological health problems as that of the aforementioned chronic diseases.[2] It is expected that Baduanjin qigong can improve the physical and psychological health of elderly housebound, but currently there lacks evidence-based research for its application in this field. In addition, elderly housebound may experience increased psychological distress due to their social isolation and physical restrictions. Thus, this study also combined CBT with Baduanjin qigong to further improve physical and psychological well-being in the elderly housebound.
The purpose of this study is to investigate the effects of Baduanjin qigong and CBT on the physical and psychological aspects of the elderly housebound.
2. Methods and participants
2.1. Ethical considerations
Approval for this trial was obtained from the North China University of Science and Technology (No. 2013197). Written informed consent was obtained from each participant. Each participant was assured of confidentiality and given the option to decline participation or to withdraw from the trial at any time without penalty. Investigators involved in this study maintained confidentiality of information collected from research participants.
2.2. Design
This study was carried out as an open-label, randomized controlled trial.
2.3. Participants
Between March and November 2016, cluster sampling was used to select a community in Tangshan, China, as a research site, following which convenience sampling was used to select for eligible elderly housebound from this community to be invited by contacted individually to participate in this study and evaluated using the Chinese version of the housebound scale.[21] A flowchart of the selection of study participants can be seen in Figure 1.
Figure 1.
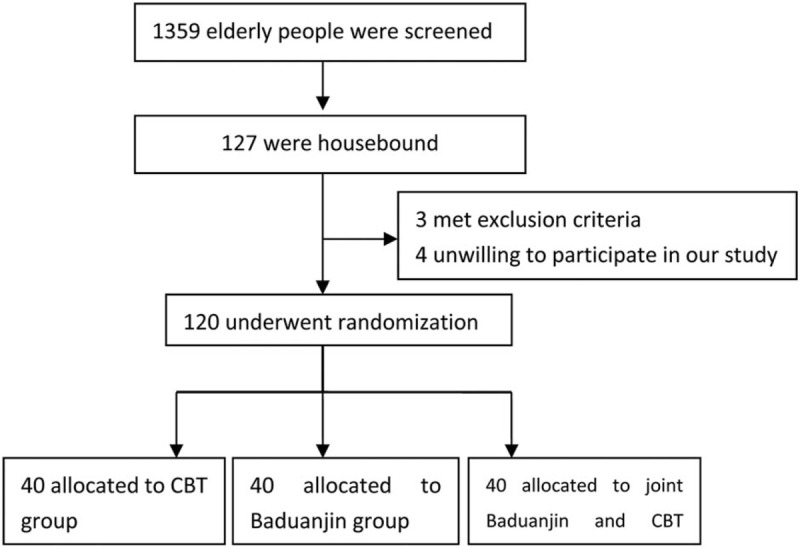
Flowchart of participant selection.
Inclusion criteria: 60 years or older; meets the international criteria for being housebound (left the house once per week or fewer over a period of at least 6 months); did not receive prior Baduanjin training or CBT intervention; and voluntarily participated in this study and signed the informed consent form.
Exclusion criteria: could not speak well or answer the questionnaire; had serious impaired hearing; bedridden elderly; and had received prior Baduanjin training or CBT (Fig. 1).
2.4. Research methods
2.4.1. Grouping
One hundred twenty qualified elderly housebound were randomly allocated into 3 groups: Baduanjin training group, CBT group, and Baduanjin training combined with CBT group (joint group).
2.4.2. Training of the researchers
Prior to interventions, four faculty members (XFM, JLW, WFL, ZXL) and 3 graduate nursing students (JYP, YT, SYY) received professional training to provide CBT and Baduanjin instruction to the participants.
2.4.3. Implementation
The duration of intervention was 6 months, and interventions were provided via home visits by the trained researchers. Participants received the interventions every 15 days over the first 3 months, totaling 6 times. Each visit lasted 1 to 1.5 h. The programme of Baduanjin qigong, see Table 1.
Table 1.
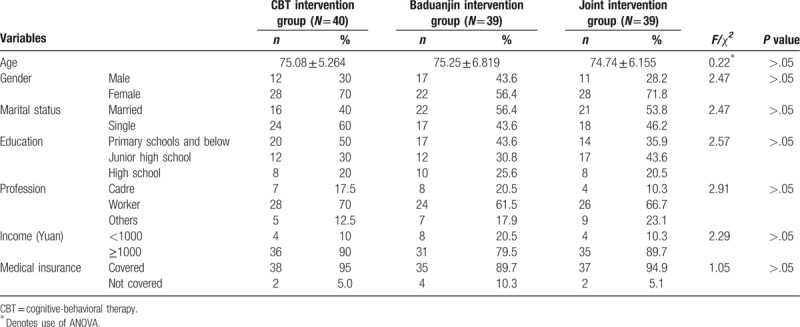
Demographic characteristics at baseline.
After 3 months, interventions were administered monthly for 3 times in total. During the first month of intervention, participants received a weekly encouragement call to continue Baduanjin training or CBT or both. At 3 months and 6 months of intervention, participants’ physical health was evaluated using spirometry and ADL scales, and participants’ psychological health was evaluated using a self-evaluation of overall health status, a self-evaluation of loneliness, and the short-form geriatric depression scale (GDS-15). Overall quality of life (QOL) of participants’ was evaluated using the self-rated SF-36 health survey (Table 2).
Table 2.
Baseline of outcome variables by intervention group.

2.5. Assessment and Instruments
2.5.1. Assessment of housebound status
The Chinese version of the housebound evaluation questionnaire was translated and back-translated from a Japanese housebound status evaluation questionnaire[22] (Cronbach α = 0.743) was adopted to evaluate the housebound status in participants. The questionnaire included 4 items, with items 1 and 4 being polar questions (no = 1, yes = 2), and items 2 and 3 being rated on frequency of occurrence (between 1 and 4). Higher scores indicated more severe housebound statuses.
2.5.2. Physical health evaluation
-
1.
Spirometry: Forced vital capacity (FVC) and maximum voluntary ventilation (MVV) were measured using the Italy MIR spirolab III portable spirometer. Formula for predicting FVC: Male: [27.63- (0.112 × age)] × height (cm); female: [27.28- (0.101 × age)] × height (cm). The normal reference range of FVC is 3.179 ± 0.117L in adult males and 2.314 ± 0.048L in adult females.[23] For the comfort of participants, MVV was measured over a 12-s time period before being extrapolated to a value for 1 min. Formula for predicting MVV: Male: (85.5–0.522 × age) × body surface area (m2); female: (71.3–0.47 × age) × body surface area (m2). The normal reference range for MVV is 104 ± 2.71L/min in adult males and 82.5 ± 2.17L/min in adult females.[24] Pulmonary function in the elderly is generally lower than the general population, scores lower than 80% of the predicted value indicated the presence of obstructive ventilatory disorders, and scores higher than the normal value ranges indicated the presence of restrictive ventilatory disorders.[24]
-
2.
ADL[25] The ADL scale comprised 2 parts: ADL and instrumental activities of daily living scale (IADL), with a total of 14 items. Each item was rated on a scale of 1 to 4, with a total score ranging between 14 and 56. A score of 14 indicated completely normal function and independence, a score of 15 to 21 indicated moderate degrees of dysfunction, and a score ≥ 22 indicated severe dysfunction.
2.5.3. Psychological health evaluation
-
1.
Health (self-evaluation): Participants provided a self-evaluation of their overall health status based on a 4-point Likert-type scale: 4 for healthy; 3 for relatively healthy; 2 for not so healthy; and 1 for unhealthy.
-
2.
Loneliness: Participants provided a self-evaluation of their degree of loneliness based on a 3-point Likert-type scale, where 3 is often lonely, 2 is sometimes lonely, and 1 is not lonely.
-
3.
Depression:[26] The Geriatric Depression Scale-Short Form (GDS-15) was used to evaluate the level of depression in the participants. The total score of GDS-15 is 15, where 0 to 5 is normal and 6 to 15 signifies depression.
2.5.4. Quality of life (QOL)
Participants self-reported on their QOL by completing the Short-Form 36 Health Survey (SF-36), which is divided into 8 dimensions. Higher scores represented higher quality of life.[27]
2.6. Statistical analysis
All statistical analyses were completed using SPSS17.0 for Windows and standard deviations were calculated for all variables studied. The differences between the 3 groups at baseline were determined using the chi-squared test and the multivariate analysis of variance (ANOVA). ANOVA was utilized to examine changes in housebound status and physical and mental status outcomes at 3 time points (baseline, after 3 months, after 6 months). Post hoc analysis of any significant main effects of conditions were performed using the LSD test. P < .05 and was considered to be statistically significant.
3. Results
3.1. Baseline data of demographic characteristics of the elderly in 3 groups
In the 120 cases of elderly housebound participants, the joint intervention and Baduanjin only intervention groups saw 1 death each during the course of this study, with no other participant abandoning the experiment. A final total of 118 participants received the interventions, with 39 in the joint intervention group, 40 in the CBT group, and 39 in the Baduanjin group. Joint intervention group: 17 were men, 22 were women, age range was 60 to 84 years old, and mean age was 75.08 ± 5.264 years old. CBT group: 12 were men, 28 were women, age range was 60 to 85 years, and mean age was 75.25 ± 6.819 years. Baduanjin group: 11 were men, 28 were women, age range was 62 to 85 years, and mean age was 74.74 ± 6.155 years. Gender, presence of spouse, educational level, occupation, income, and medical insurance, showed no significant statistical difference between the 3 groups at baseline (P > .05)
Baseline of housebound and other outcome variables (QOL, ADL, FVC, MVV, health self-evaluation, loneliness, and depression) in 3 groups of the elderly subjects are presented in Table 3.
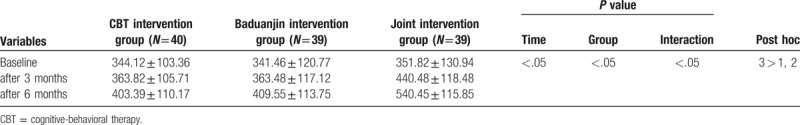
Table 3.
Quality of life after intervention.
3.2. Housebound outcomes
After 3 months’ intervention, the housebound scores in the CBT group, Baduanjin group and joint intervention group were 9.78 ± 1.51, 10.21 ± 1.22, and 8.90 ± 1.85, respectively. After 6 months’ intervention, the housebound scores were 8.85 ± 2.32, 8.05 ± 1.90, and 6.38 ± 1.71, respectively. Housebound scores were significantly lowered in the joint intervention group than in either the CBT or Baduanjin groups (P < .05), Figure 2.
Figure 2.
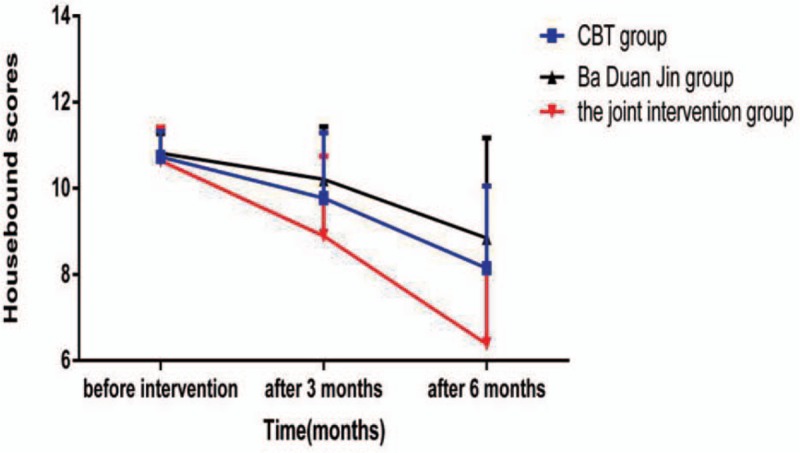
Housebound scores and time interaction diagram of the 3 groups of interventions for elderly housbound.
3.3. Overall health outcomes
After 6 months of intervention, the QOL of the 3 groups of elderly participants were significantly different from those at baseline (P < .05) (Table 4).
Table 4.
Comparison of physical condition between the 3 groups before and after intervention.
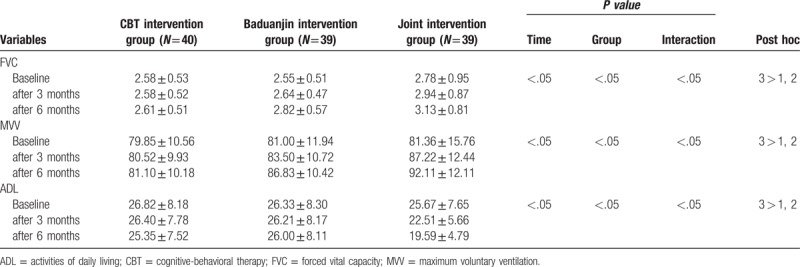
3.4. Physical condition outcomes
After 6 months of intervention, the lung function (FVC, MVV) and ADL scores of the 3 groups of elderly patients were significantly different from those at baseline (P < .05) (Table 5).
Table 5.
Comparison of psychological status between the 3 groups before and after intervention.
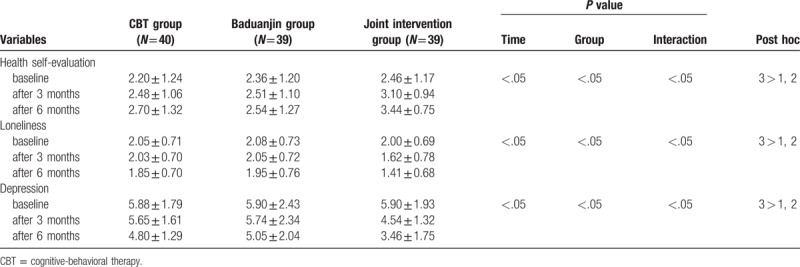
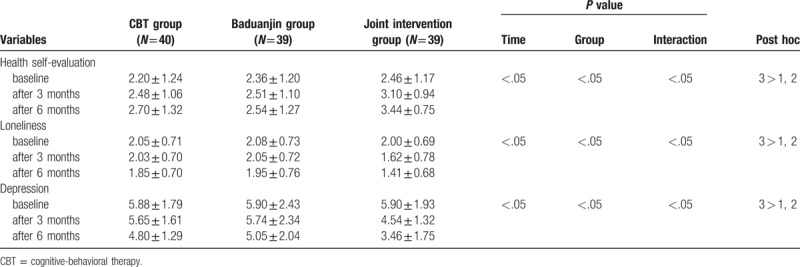
3.5. Psychological status outcomes
Pre-intervention scores compared with 3 months and 6 months post-intervention showed that the effect of joint intervention on psychological status was superior to CBT or Baduanjin interventions alone. The differences were statistically significant (P < .05) (Table 6).
Table 6.
Comparison of psychological status between the 3 groups before and after intervention.
4. Discussion
Housebound status negatively affects emotional, physical, and behavioral outcomes in the elderly,[28,29] in order to improve the quality of life in the elderly, it is necessary to improve their housebound status.
4.1. Baduanjin combined with CBT can effectively improve the housebound status and physical condition of the elderly
The results of this study showed that the housebound status of all 3 groups of elderly participants improved after 3 months of intervention, and further improvements were observed at 6 months after intervention. Results of the joint intervention significantly exceeded that of the CBT or Baduanjin interventions alone (P < .05). The elderly are susceptible to age-related osteoporosis and are prone to falls,[30,31] and falls are the leading cause of fractures in the elderly.[24] Due to these concerns, elderly housebound may not want to leave their homes. Long-term practice of Baduanjin can enhance muscle strength of the lower extremities and lumbar region, improve forward and backward balance control, and enhance both dynamic and static balance in the elderly, thereby enhancing stability of gait and reducing the risk of falls.[32] Studies have also shown that long-term practice of Baduanjin facilitated a reduction in limb pain and that it has some supporting role in the treatment of arthritis.[33,34]
Long-term practice of Baduanjin has been indicated to enhance cardiac contractility and vascular filling and rhythm, thicken myocardial fibres, and improve circulatory system function in the elderly.[35] This would thereby increase the tolerance of elderly housebound to exercise and provides possible safeguards for the elderly to experience life outside of the home.
The results of this study also showed that pulmonary function (FVC, MVV) improvement in the interventions including Baduanjin was greater than that in the CBT group alone after 6 months of intervention. This may be attributed to the practice of these Baduanjin exercises: “2 hands hold up the heavens triple burner”, “separate heaven and earth”, and “2 hands hold the feet to strengthen the kidneys and waist”, where respiratory rate and depth may be increased through the increase of diaphragm movement. By performing these particular exercises, the respiratory muscles are fully exercised, thereby increasing lung capacity. At the same time, the combination of chest and abdominal breathing increases the activity of the diaphragm and abdominal muscles, thereby regulating the intercostal muscles and respiratory function, causing further increase in pulmonary ventilation.[35] The physical outcomes of the joint intervention group were more improved than the Baduanjin group or the CBT group. Since the Baduanjin exercises were performed for 6 months, this allowed the elderly to gradually adapt to and develop the habit of daily exercise.
The results of this study showed that Baduanjin combined with CBT improved ADL in elderly housebound. The long-term housebound state of some elderly may lead to a drastic reduction in the scope of ADL and a more pronounced decline in ADL levels.[36] Studies have shown that physiology is the major factor affecting ADL.[36] Baduanjin exercises the upper and lower extremities in all directions and trains finger, wrist, shoulder, and waist rotations, applying a type of spinning aerobic workout.[35] These exercises facilitate a comprehensive and systematic exercise for muscles, bones, and joints and improve body function,[35] which all help to restore and improve ADL levels.
4.2. Baduanjin training combined with CBT can effectively improve the psychological status of elderly housebound
The results of this study showed that after 6 months of intervention, the joint intervention group yielded greater positive results in psychological status than that of Baduanjin or CBT alone (P < .05), and at both 3 months and 6 months, the intervention effect of the CBT group on psychological condition surpassed (see Table 5) that of the Baduanjin group. This may be due to how the psycho-social approach of CBT encourages the elderly housebound to individually take initiative to comprehend psychological problems they may be facing.
Baduanjin exercises such as “2 hands hold the feet to strengthen the kidneys and waist” have a certain effect on emotional improvement. For example, “2 hands hold up the heavens triple trinity” has a good regulatory role on mood depression and irritability.[36] Baduanjin training increases the excitation of the middle cerebral cortex, helping to down-regulate anxiety and negative emotions.[37] The exercise component of Baduanjin improved mental health in the elderly but saw a lesser effect than that of CBT. When applied together, Baduanjin and CBT combined functional therapy and progressive psychological intervention, enhancing the cooperative effect of the two. This could account for why the psychological status of the joint intervention group was much better than that of the other 2 groups.
5. Conclusion
Baduanjin qigong has become a common practice in Chinese communities, promoting outdoor physical activity for the elderly and encouraging social interactions between the elderly and their peers as they exercise together; they can freely express their feelings and enhance their subjective well-being, and finally enhanced their quality of life.
6. Advantages and limitations
Advantages: This study assessed the effect of traditional Chinese Baduanjin Qigong in elderly housebound, with results suggesting that Baduanjin can improve housebound status, physical health, mental health, and overall quality of life. Its effectiveness is enhanced when combined with CBT. This method is simple, feasible, and economical.
Limitations: In this study, taking into account the feasibility of home visits during implementation of the interventions and the compliance of participants, the randomization of all communities in the city was not achieved during the screening stage. Future multi-center studies to affirm these results are recommended.
Author contributions
Conceptualization: Liwei Jing, Yuyu Song, and Fengmei Xing.
Data curation: Liwei Jing and Yanpeng Jin.
Formal analysis: Yanpeng Jin and Yuyu Song.
Investigation: Yuyu Song.
Methodology: Fenglan Wang.
Software: Xiaoli Zhang.
Supervision: Fenglan Wang.
Writing – original draft: Yanpeng Jin, Xiaoli Zhang, and Fengmei Xing.
Writing – review & editing: Yanpeng Jin and Fengmei Xing.
Footnotes
Abbreviations: ADL = activities of daily living, CBT = cognitive-behavioral therapy, FVC = forced vital capacity, IADL = instrumental activities of daily living scale, MVV = maximum voluntary ventilation, QOL = overall quality of life, rANOVA = repeated measures analysis of variance.
The authors declare that they do not have any potential conflict of interests in relation to the contents of this manuscript.
References
- [1].Jing Li-wei, Wang Yu-jing, Zhang Chao ct. The status of community elderly housebound and its influencing factors in Hebei. ChinJ Pub Health 2015;1182–4. [Google Scholar]
- [2].Xing Feng-mei, Yao San-qiao. Research status of elderly housebound and its influencing factors in foreign countries. Chin J Gerontol 2010;30:268–9. [Google Scholar]
- [3].Barry Tom J, Sc Amy R, Sewart B, et al. Deficits in disengaging attention from threat predict improved response to cognitive behavioral therapy for anxiety. Depression Anxiety 2015;32:197–221. [DOI] [PubMed] [Google Scholar]
- [4].Mccrae Niall, Correa Ana, Chan Tom, et al. Long-term conditions and medically-unexplained symptoms: feasibility of cognitive behavioural interventions within the improving access to psychological therapies programme. J Ment Health 2015;24:1–6. [DOI] [PubMed] [Google Scholar]
- [5].Sunnhed Rikard, Jansson-Fröjmark Markus Cognitive arousal, unhelpful beliefs and maladaptive sleep behaviors as mediators in cognitive behavior therapy for insomnia: a quasi-experimental study. Cogn TherRes 2015;14:1–2. [Google Scholar]
- [6].Choi NG, Kunik ME, Wilson N. Mental health service use among depressed, low-income homebound middle-aged and older adults, J Aging Health. J Aging Health 2013;25:638–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Choi Namkee G, Marti C. Nathan, Bruce Martha L, et al. Depression in homebound older adults: problem-solving therapy and personal and social resourcefulness. Behav Ther 2013;44:489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zheng G, Chen B, Fang Q, et al. Primary prevention for risk factors of ischemic stroke with Baduanjin exercise intervention in the community elder population: study protocol for a randomized controlled trial. Trials 2014;15:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Xing Feng-mei, Zhang Xiao-li, Wang Jian-hua ct. Relationship between health status and self-rated health and depression in elderly people. Chin J Publ Health 2010;249–50. [Google Scholar]
- [10].Dong Sheng-lian, Liu Hai-juan, Xing Feng-mei The status of housebound and its psychologic factor in community elderly. Chin J Publ Health 2009;969–70. [Google Scholar]
- [11].Zhang Ji-hua Research on the teaching of eight-length broeade exercise. Wushu Sci 2009;6:83–4. [Google Scholar]
- [12].Liu Rui-hua, Hao Ying-xiu, Hou Shu-min Effect of eight-length broeade exereise combined with abdominal massage and acupoint massage on constipation after stroke. Chin J Gerontol 2013;33:904–6. [Google Scholar]
- [13].Wu Yun-chuan, Wei Qing-bo Clinical observation of eight-length broeade exereise adjuvant treatment of type 2 diabetes mellitus. Chin J Gerontol 2015. [Google Scholar]
- [14].Beijing Univ Chin Med, Xue Guang-wei The efficacy of fitness qigong Ba Duan Jin in pulmonary rehabilitation of patients with COPD at stable stage. 2014. [Google Scholar]
- [15].Solaimani Khashab A, Ghamari Kivi H, Fathi D. Effectiveness of cognitive behavioral therapy on spiritual well-being and emotional intelligence of the elderly mourners. Iran J Psychiatry 2017;12:93–9. [PMC free article] [PubMed] [Google Scholar]
- [16].Chen YX, Hung YP, Chen HC. Mobile application-assisted cognitive behavioral therapy for insomnia in an older adult. Telemed J E Health 2016;22:332–4. [DOI] [PubMed] [Google Scholar]
- [17].Barrera TL, Cummings JP, Armento M, et al. Telephone-delivered cognitive-behavioral therapy for older, rural veterans with depression and anxiety in home-based primary care. Clin Gerontol 2017;40:114–23. [DOI] [PubMed] [Google Scholar]
- [18].Lv Aiping, Ren Aihong, Hao Chunjie, et al. Relationship between dynamic pulmonary function and aging in elderly people. J Fourth MiI Med Univ 2005;545–7. [Google Scholar]
- [19].Wang Su-dong, Guo Jing-xian, Xing Xiao-ling Reliability and validity of Chinese version of housebound scale in Chinese community elderly. Chin J Behav Med Brain Sci 2013;22:758–60. [Google Scholar]
- [20].Health Qigong management center of State General Administration of sport Fitness Qigong Eight-Length Broeade Exereise. 2013;Beijing: People's Physical Culture Publishing House, 195. [Google Scholar]
- [21].Lv He-ping, Ren Ai-hong, Hao Chun-jie Relationship between dynamic pulmonary function and aging in elderly people. Negative 2005;26:545–7. [Google Scholar]
- [22].Wang Sudong, Guo Jingxian, Xing Xiaoling, et al. Eliability and validity of Chinese version of housebound scale in Chinese elderly people. Chin J Behav Med Brain Sci 2013;22:758–60. [Google Scholar]
- [23].Jun Bo, Xu Yongjian Medicin (Version 8), BeiJing, People's Medical Publishing House, 2013. [Google Scholar]
- [24].Yu Mei, Ma Yuan-zheng, Tang Wen Research progress on prevention of falls in elderly people with osteoporosis. Chin J Osteoporos 2012;1157–60. [Google Scholar]
- [25].Chen P, Yu ES, Zhang M, et al. ADL dependence and medical conditions in Chinese older persons: a population-based survey in Shanghai, China. J Am Geriatr Soc 1995;43:378–83. [DOI] [PubMed] [Google Scholar]
- [26].Wang Cui-min, Meng Ling-gang Clinical study of eight-length broeade exereise intervention in elderly patients with knee osteoarthritis. Cardiovasc Dis J Integr Tradit Chin Western Med 2016;158. [Google Scholar]
- [27].Li Lu, Wang Hong-mei, Shen Yi Development and performance test of Chinese version of SF-36 health survey scale. Chin J Prevent Med 2002;36:109–13. [PubMed] [Google Scholar]
- [28].Zhu AQ, Kivork C, Vu L, et al. The association between hope and mortality in homebound elders. Int J Geriatr Psychiatry 2017;32:e150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Soones T, Federman A, Leff B, et al. Two-year mortality in homebound older adults: an analysis of the national health and aging trends study. J Am Geriatr Soc 2017;65:123–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Reuben DB, Gazarian P, Alexander N, et al. The strategies to reduce injuries and develop confidence in elders intervention: falls risk factor assessment and management, patient engagement, and nurse co-management. J Am Geriatr Soc 2017;65:2733–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Askari M, Eslami S, van Rijn M, et al. Erratum to: assessment of the quality of fall detection and management in primary care in the Netherlands based on the ACOVE quality indicators. Osteoporos Int 2016;27:577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Xiao Chun-mei Gender characteristics of balance ability in the elderly. Sports Sci Res 2001;26–8. [Google Scholar]
- [33].Wang Cui-min, Meng Ling-gang Clinical study of Eight-Length Broeade Exereise intervention in elderly patients with knee osteoarthritis. Cardiovasc Dis J Integr Tradi Chin Western MedMedicine 2016;158. [Google Scholar]
- [34].Ming Hong-min The role of Chinese traditional sports in health education of rheumatoid arthritis. World Latest Medicine Information (Electronic Version) 2017;202–5. [Google Scholar]
- [35].Zhang Li-fen Study on the effect of Eight-Length Broeade Exereise on balance ability of the elderly. Capital University of physical education and sports 2012. [Google Scholar]
- [36].Geng Yuan-qing, Wang Xu-dong Effect of eight-length broeade exereise on mental sub-health regulation based on the theory of emotion controlled by five zang-organs. China J Tradi Chin Med Pharm 2008;23:348–9. [Google Scholar]
- [37].Ma Su-hui, Dou Na, Chen Chang-xiang ct Effect of the traditional Ba duan jin Exercise in women with peri-menopausal syndrome and depression. Medica of China Family Phys 2010;13:2864–5. [Google Scholar]


