Abstract
Background:
Crohn's disease (CD) is a highly prevalent inflammatory bowel disease (IBD), characterized by recurring flares altered by periods of inactive disease and remission, affecting physical and psychological aspects and quality of life (QoL). The aim of this study was to determine the therapeutic benefits of soft non-manipulative osteopathic techniques in patients with CD.
Methods:
A single-blind randomized controlled trial was performed. 30 individuals with CD were divided into 2 groups: 16 in the experimental group (EG) and 14 in the control group (CG). The intervention period lasted 30 days (1 session every 10 days). Pain, global quality of life (GQoL) and QoL specific for CD (QoLCD) were assessed before and after the intervention. Anxiety and depression levels were measured at the beginning of the study.
Results:
We observed a significant effect of the treatment in both the physical and task subscales of the GQoL (P = .01 and P = .04, respectively) and also in the QoLCD (P ≤.0001) but not in pain score (P = .28). When the intensity of pain was taken into consideration in the analysis of the EG, there was a significantly greater increment in the QoLCD after treatment in people without pain than in those with pain (P = .02) The improvements in GQoL were independent from the disease status (P = .16).
Conclusions:
Soft, non-manipulative osteopathic treatment is effective in improving overall and physical-related QoL in CD patients, regardless of the phase of the disease. Pain is an important factor that inversely correlates with the improvements in QoL.
Keywords: Crohn's disease, manual therapy, osteopathy, quality of life
1. Introduction
Crohn's disease (CD) is an inflammatory bowel disease (IBD) characterized by recurring flares followed by periods of inactive disease and remission, with variable duration and intensity.[1] The incidence of CD continues to increase worldwide, with variations in prevalence between geographic regions, and a higher prevalence among women.[2] Increased mortality has been observed late in the course of the disease, being most pronounced among women younger than 50 years of age at diagnosis as well as in patients with severe CD.[3]
Clinical manifestations of CD are mainly intestinal, such as diarrhea or constipation, abdominal pain/swelling, ulcers, and so on. Extra-intestinal (i.e., joint pain, or ocular inflammation) and psychological symptoms are present in approximately 25% of CD patients.[4] These manifestations can, in turn, affect work performance[5] and especially quality of life (QoL).[6–8]
Consequently, CD imposes a substantial burden on the sufferer, with unpredictable fluctuating symptoms, time off work, the need for expensive drugs, or surgery and multidisciplinary care. Therefore, in many developed countries, CD places a major burden on public health-care resources and has a considerable impact on the health of workers.[9]
Although there is currently no cure for CD, pharmacological treatment aimed at reducing inflammation in the gut has traditionally been administered to CD patients. Surgery has been considered when the pharmacological treatment fails and the illness has a direct impact on the patient's health. In order to avoid medical and surgical complications, non-invasive and low-cost therapeutic approaches based mainly on soft physical therapies may be promising strategies for improving different symptoms of the disease.[10,11]
To date, there is little evidence of the impact of physical therapy interventions on CD. Most of the existing studies so far have focused on physical exercise-based approaches.[12–13] On the other hand, some studies have demonstrated that manipulative techniques are able to reduce abdominal pain and discomfort as well as to improve QoL in both patients with CD and irritable bowel disease (IBS).[14,15] Nevertheless, due to the particularities (possible osteopenia and osteoporosis)[16] of these patients, soft-tissue techniques should be more appropriated to treat these pain and discomfort. With this approach, the risk associated with spinal manipulation may be minimized.[17] So we think that the application of a treatment based on non-manipulative techniques could be another option to approach these patients, minimizing risks, or even for those in which manipulation may be contraindicated.
1.1. Objective
In the present study, we aimed to ascertain whether a soft non-manipulative therapeutic approach including soft tissue techniques improves QoL, decreases pain, and positively influences physical and psychological aspects in CD patients.
2. Material and methods
2.1. Subjects
Thirty participants diagnosed with CD belonging to the Valencian Association of Crohn's Disease and Ulcerative Colitis was recruited. The study was carried out from May 2016 to June 2016. The treatments have been carried out in the laboratories of the Faculty of Physiotherapy of the University of Valencia. All subjects were informed verbally and in writing about the nature of this study, including all potential risks. Written informed consent was obtained before participation. The inclusion criteria were that the subjects be aged between 18 and 62, that they had been diagnosed with CD at least 1 year before, and that they presented abdominal pain and were receiving usual treatment with an adequate diet. The exclusion criteria included non-specific inflammatory bowel pain, abdominal tenderness, infection, ischemia, physical damage, specific immunologic sensitivity, pregnancy, or breast-feeding mothers.
2.2. Procedures/study design
A single-blind randomized controlled trial was carried out. The participants were randomly allocated to 2 different groups through computer software by an external assistant who was blinded to the study objectives: experimental group (EG) (n = 16; 8 women and 8 men) and Control group (CG) (n = 14; 12 women and 2 men). The intervention lasted 30 days (1 session every 10 days).
Participants belonging to the EG were treated once every 10 days. The sessions lasted 45 minutes and were conducted by a physiotherapist who had extensive experience in manual therapy. The CG only came to the evaluation sessions and received no treatment besides those recommended by the doctor. Indeed, all the patients belonging to EG or CG were advised against changing their daily routines. Participants’ attendance was registered after every session.
Subjects were assessed twice, at baseline and after completion of the study. One physiotherapist performed the assessments and was unaware of the group the patients belonged to. To reduce bias, participants were instructed not to tell the physiotherapist about the treatment they received. The statistician was also blinded to the goals of the study. This trial was registered at www.clinicaltrials.gov NCT02763293.
2.3. Sample size
Sample size calculation was based on the results obtained, in the impact of abdominal pain on QoL, in a previous study in which similar approach was used. It was calculated at 90% power to detect a mean difference of 24.1 points[14] with a standard deviation of 45.0 points (d = 0.54), on the Irritable bowel severity scoring system used in their study,[18] using a type 1 error (α) of 5%, and a type 2 error (β) of 20%. This calculation rendered 12 patients in each group. G-Power 3.1. version was used for sample size estimation (Institute for Experimental Psychology, University of Düsseldorf, Düsseldorf, Germany).
2.4. Intervention
The intervention included 6 techniques, as described in Figure 1. Following the intervention, subjects remained in supine position with a neutral head and neck position for 10 minutes, in order to obtain relaxation and diminish tension after treatment.[19,20] The cluster of techniques performed for each session includes the following:
Figure 1.
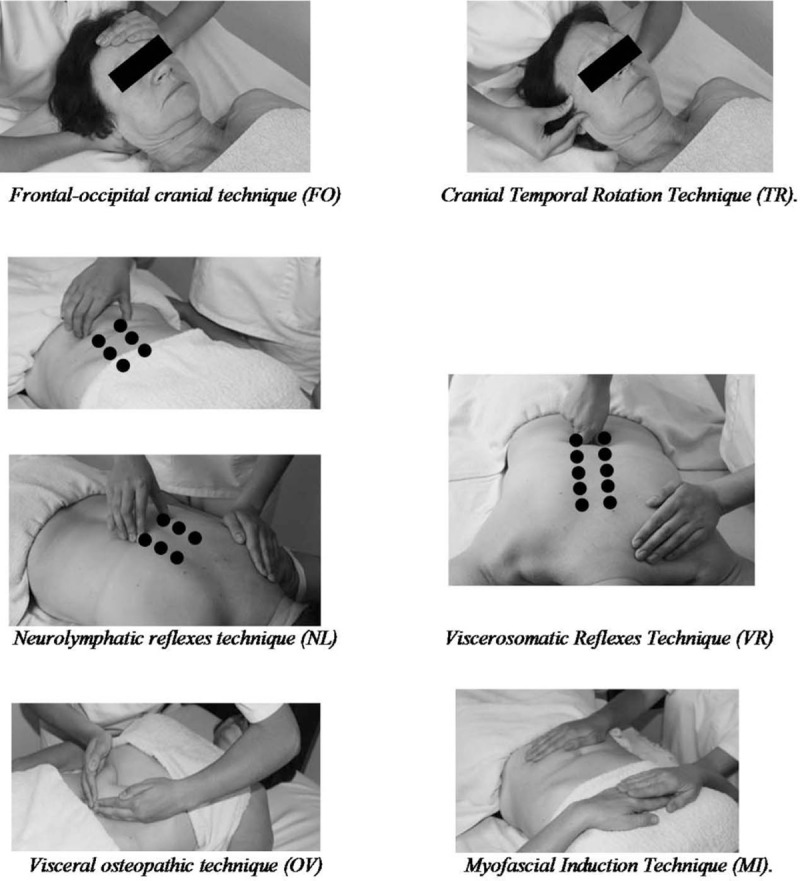
Cluster of techniques included in the soft non-manipulative osteopathic treatment. FO = frontal-occipital cranial technique, MI = myofascial Induction Technique, NL = neurolymphatic reflexes technique, OV = visceral osteopathic technique, TR = cranial temporal rotation technique, VR = viscerosomatic reflexes technique.
-
(1)
Frontal-occipital cranial technique. It focused on opening the occipitomastoid suture[21,22] in order to decompress the jugular foramen and its contents: jugular vein, cranial nerves IX (glossopharyngeal), X (vagusor pneumogastric nerve), and XI (accessory nerve). Counterpunching forces were applied with both hands (the anterior hand on the frontal bone and the posterior hand under the occiput) for 5 minutes.
-
(2)
Cranial Temporal Rotation Technique. It aimed at opening the jugular foramen. One hand was placed under the occiput and the other hand fixed the temporal bone from the ear canal. It began with a functional aggravation phase of compression of the jugular foramen by induction of temporal rotation, followed by a structural correction phase.[21,22] It was performed bilaterally for 5 minutes.
-
(3)
Neurolymphatic reflexes technique. Using this technique, some kinesiology points of the body that are believed to affect specific muscles and organs (because of the increase and even lymphatic congestion) were located and treated. Firm pressure with the thumb or tip finger was applied for 1 minute on the following points: 3 abdominal points, 2.5 centimeters on the right and left side of the navel in the line of the rectus abdominis, (supine position); 3 dorsal points, 2.5 centimeters on the right and left side of the spinous processes between the T8-T9, T9-T10 and T10-T11 spaces (prone position). Subsequent massage to each area was applied in order to improve the lymphatic drainage, thus leading to positive effects in the digestive system.[23]
-
(4)
Viscerosomatic reflexes technique. The goal of this technique was to treat some sensitive and noticeable vertebral areas associated with visceral disorders, usually chronic, and which are manifested by rigidity and local alterations.[24,25] In the present study, firm digital friction was applied laterally to the spinous processes of D8 to D12, aimed at producing local changes and influencing the involved organs.
-
(5)
Myofascial induction technique. Concretely, the technique of transverse planes was applied in the abdominal region, with the purpose of releasing fascial restriction zones at abdominal level caused by pain and intestinal inflammation that alter the vegetative autonomic system response. This technique focused on the infra-umbilical area. With the patient lying supine, one hand was placed under the lumbar region and the ventral hand on the abdominal region, between the iliac crests. Meanwhile, the patient was instructed to perform a gentle and conscious breathing,[26,27] a mild 3-dimensional fascial movement was performed for 10 minutes.
-
(6)
Visceral technique. The objective of this technique was to produce a neurovascular reflex. For this purpose, the patient was placed in a supine position with knees flexed, the physiotherapist placed then the ulnar border of both hands over the lower part of the abdomen. Afterward, the patient was requested to take a deep breath and during the exhalation, a manual vibration was conducted in the cranial direction.[28,29] This technique was carried out for 2 minutes.
2.5. Outcomes measures
2.5.1. Pain
Assessed with the Visual Analogue Scale (VAS), in which the patients marked their level of pain intensity on a 10-cm horizontal line (0 = no pain to 10 = maximum pain) at the time the assessment was carried out.
2.5.2. Global quality of life (GQoL)
Evaluated by the Functional Assessment of Cancer Therapy-General questionnaire, version 4 (v4-FACT-G).[30] This version was translated into Spanish and validated by Dapuerto et al[31] and it has shown good internal consistency (Cronbach's alpha = 0.92).[32] This is a widely used QoL instrument with 27 items that evaluate the QoL in patients suffering from chronic diseases.[30] It assesses 4 primary dimensions of QoL: physical well-being (7 items), social/family well-being (7 items), emotional well-being (6 items), and functional well-being (7 items). It uses a 5-point Likert-type response categories ranging from 0 = ’not at all’ to 4 = ’very much’. The total FACT-G score is the summation of the 4 subscale scores and ranges from 0 to 108.
2.5.3. Quality of Life in CD (QoLCD)
Assessed with the Spanish version of the Inflammatory Bowel Disease Questionnaire (IBDQ-32),[33] that was validated by Masachs et al[34] This version has shown a high internal consistency (Cronbach's alpha = 0.97 for the global score).[35] The IBDQ-32 is a QoL questionnaire specific for patients with IBDs that includes 32 questions grouped into 4 dimensions: bowel, systemic, social, and emotional. Scores range from 1 (poorest QoL) to 7 (best QoL). Higher scores indicate better QoL.
2.5.4. Anxiety and depression
Evaluated with the Hospital Anxiety and Depression Scale (HADS),[36] translated and validated into Spanish with a good internal consistency.[37] The scale comprises 14items (7 relate to anxiety and 7 relate to depression), with responses being scored on a scale of 0 to 3 (3 indicates higher symptom frequencies). Scores for the entire scale (emotional distress) range from 0 to 42, with higher scores indicating more distress.
2.6. Ethics
All procedures were conducted in accordance with the principles of the Declaration of Helsinki of the World Medical Association and the protocols were approved by the Human Research Ethics Committee of the University of Valencia with the protocol number H1449647827044). All patients signed an informed consent form before inclusion in the study.
2.7. Statistical analyses
All statistical analyses were performed with SPSS v.22 (IBM SPSS, Inc., Chicago, IL, USA). Standard statistical methods were used to obtain the mean and standard deviation of the mean (SD). The main study was the analysis of the effect of the between-subject factor “treatment group” (i.e., CG and EG) on the dependent variables in 2 points of time, pre- and post-treatment (within-subject factor). For this purpose, an inferential analysis of the data with a mixed 2-factor multivariate analysis of variance (MANOVA) was conducted. Multiple comparison techniques were requested using the Bonferroni correction. We evaluated the assumption of homoscedasticity using a Levene test and it was assumed in each variable.
Besides this, we studied the effect of the pain in the IBDQ-32 improvement experienced after the treatment. For this purpose, we allocated the participants of the EG into 2 groups, the pain group (PG) which had 3 or more points in the VAS and the non-pain group (NPG) which had less than 3 points. Then we conducted an Independent Student t test.
Further, we explored whether significant differences existed in the variables that improved with the treatment depending on the stage of the disease (outbreak or remission) with an Independent Student T-test.
Additionally, we compared the results of the body mass index (BMI), Harvey Bradshaw Index, Goldberg-anxiety, Goldberg-depression, HADS and VAS between the groups (GC and CG) in order to explore whether the groups were homogeneous in the baseline with the same statistical test. The type I error was established as < 5% (P <.05).
3. Results
Thirty-eight subjects were assessed for eligibility. Six of them were excluded because they had incompatible work schedules and 2 of them because of the worsening of their symptoms before the randomization. Finally, who thirty met the inclusion criteria, were included and then randomized to an EG (n = 16 in; 8 women and 8 men) or a CG (n = 14; 12 women and 2 men). All of them completed the study (Fig. 2).
Figure 2.
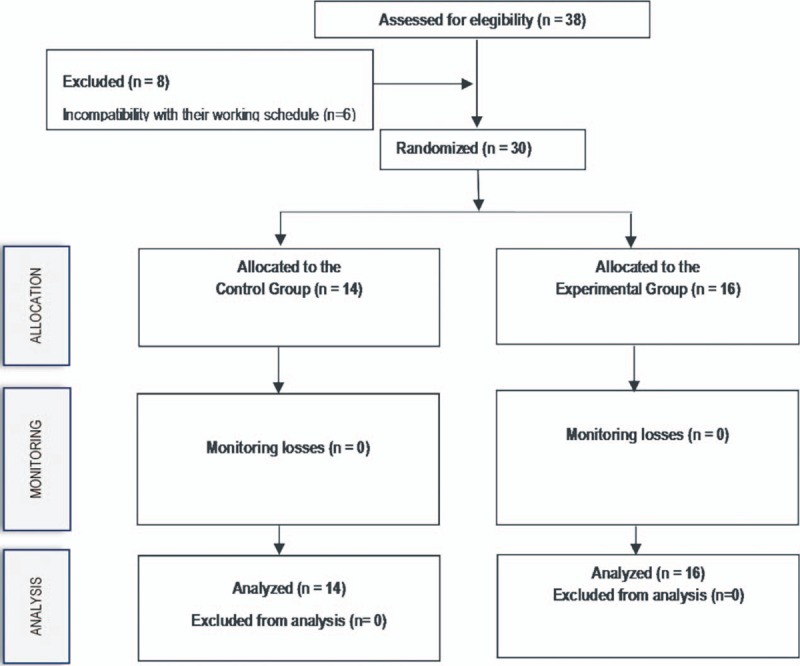
Flowchart according to CONSORT statement for the report of randomized trials.
3.1. Participants’ descriptive results
The mean (SD) age was 40.14 (12.32) years old for the CG and 42.56 (10.09) years old for the EG. The BMI was 24.04 (4.63) kg m–2 and 25.81 (5.34) kg m–2 for the CG and EG, respectively. There were no differences in the age and BMI between the CG and the EG (P >.05). Furthermore, the groups were also similar at baseline in the pain experienced, levels of anxiety and depression (P >.05). None of the participants reported any complaints or exacerbation of their symptoms at the end of the study.
3.2. Treatment
The results showed a significant multivariate effect for the interaction treatment group ∗ time: F(7,22) = 4.28, P <.01, η2P = .58.
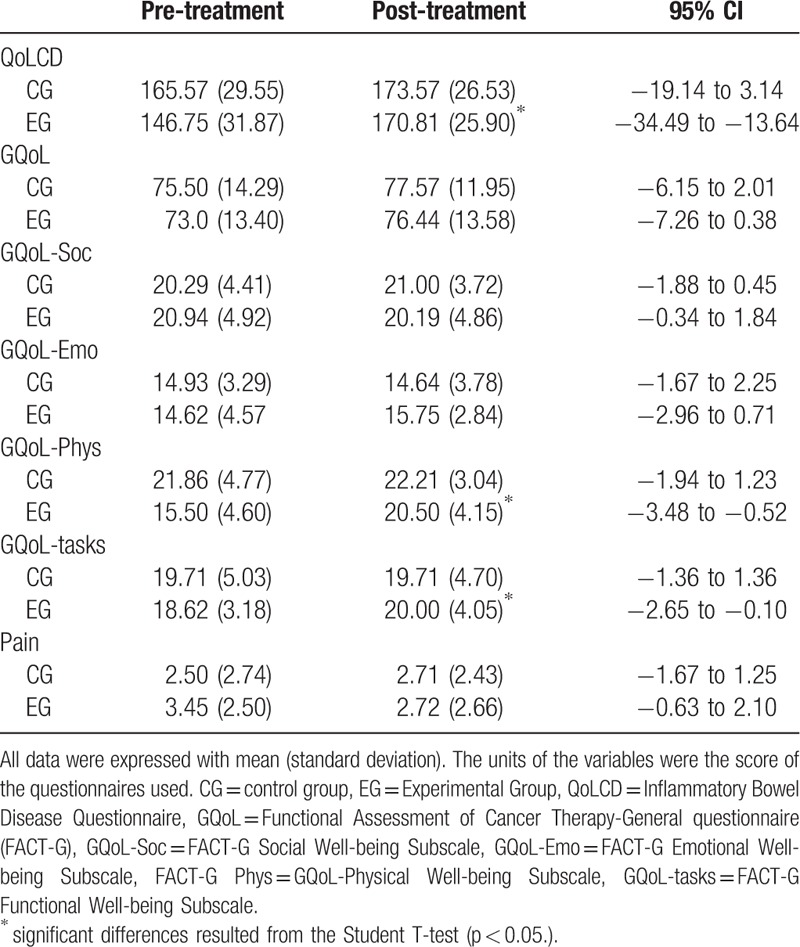
Table 1 presents the descriptive results of the variables, the statistical differences and the 95% confidence interval for each dependent variable under study.
Table 1.
Effect of the treatment on the dependent variables in the experimental and control group.
3.3. Effect of pain
When the effect of pain was studied over the improvements experienced in the EG, 8 individuals were assigned to the PG and 8 to the NPG. The outcome derived from the IBDQ32 showed that, although both groups significantly improved their IBDQ-32 score, the PG presented significant lower improvements than the NPG, as can be observed in Figure 3. For the rest of variables, pain had no significant effect on the results (P >.05).
Figure 3.
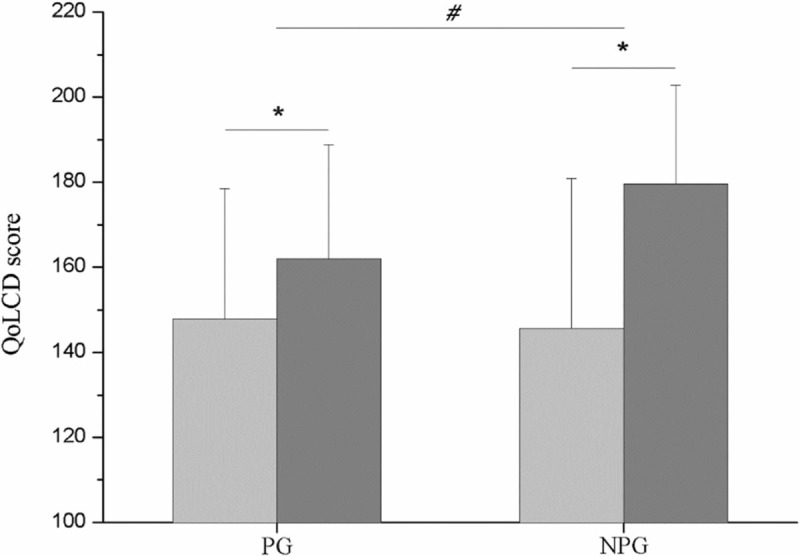
Quality of Life in the experimental group before and after treatment when divided in pain group (n = 8) and non-pain group (n = 8). NPG = no pain group, PG = pain group, QoLCD = quality of Life in CD measured with Inflammatory Bowel Disease Quality of Life-32 questionnaire score. ∗Significant differences between the IBDQ32 score after (dark grey) and before (light grey) treatment within groups; #Significant differences between the IBDQ32 improvement between groups.
3.4. Effect of the disease status
When the effect of the treatment was studied, taking into consideration the status of the disease (outbreak vs remission), the results proved that the stage of the disease had no effect on the improvements achieved with the experimental treatment (P = .16). Data not shown.
4. Discussion
The present study shows that soft non-manipulative treatment improves both the overall and the functional-related QoL in CD, in both the outbreak and remission phase, and that pain has a negative effect on these improvements. To the best of our knowledge, this is the first study to evaluate the therapeutic effect of this kind of non-manipulative approach on this particular chronic disease.
The so-called soft non-manipulative treatment included 2 cranial techniques, 2 visceral manual therapy techniques and 2 reflex techniques that aimed at avoiding any possible posterior visceral inflammation. Some of these techniques have been previously applied in the treatment of IBD. In this regard, abdominal myofascial induction technique[38] and visceral osteopathic technique[38] have been shown to be effective in decreasing chronic constipation severity and QoL improvements in IBD. The neurolymphatic reflexes technique has only been used in a case report in which authors reported that this technique was able to improve low back pain and QoL in an unusual congenital bowel abnormality.[39] To the best of our knowledge, frontal-occipital cranial technique has not been used in patients with IBD. Through this technique, we aimed to decompress the jugular foramen, because its compression can affect the vagal system and all its target organs, as well as the cranial pairs that pass through it.[40,41] We aimed therefore to assess the plausible effectiveness of the combination of these soft techniques on QoL and pain in CD patients.
Regarding QoLCD, as measured by the IBDQ-32, EG patients showed an improvement in the questionnaire score of 16.40% after the treatment, whereas CG patients did not show any significant improvement. These results confirm that the proposed treatment is as effective as other manipulative treatments.[14,15,38] In fact, Piche et al showed that manipulative osteopathic treatment resulted in a slightly lower improvement (12.71%) in the IBDQ-32 score.[15] However, Brugman et al achieved a greater improvement in QoL (46%) in people with chronic constipation. The reasons for this improvement may be the type of disease or the individualized treatment, which was dependent on the reported symptoms.[38] Other approaches based on physical exercise obtained similar results in the IBDQ-32 score. This is particularly the case of the study conducted by Ng et al, in which authors report an improvement of 15.22% with a 3-month endurance program in people with CD,[16] and the study conducted by Klare et al, in which authors achieved an improvement of 19% with a 10-week endurance training program.[13]
In order to achieve a more accurate point of view about the effect of the treatment in this particular chronic disease, we determined GQoL by means of the FACT-G questionnaire overall score, and the FACT-G subscales related to physical, functional, emotional and social conditions in our patients. Our results showed non-significant improvements in the FACT-G overall score, which is reasonable because we did not apply a psychological or a social intervention. Strikingly, the EG significantly improved the physical well-being and functional well-being subscales score, both related to physical function, with an average improvement of 19.83%. Taken together, these results suggest that these physical improvements are not mediated by an emotional component, since neither the results of the emotional subscale those for nor the social or family context was affected by the intervention. Our findings are in agreement with those found by Piche et al and Florance et al, who did not observe any improvement in anxiety or depression when an osteopathic treatment was applied.[14,15] In this regard, a multidisciplinary approach including psycho-social intervention may have had a positive effect in G-QoL scale or in the emotional and social subscales.
As stated before, abdominal pain is one of the main clinical manifestations of CD, which may be accompanied by muscle stiffness, sensitive reflex areas, and sensory changes.[42,43] Furthermore, pain in gastrointestinal disorders is accompanied by a visceral hypersensitivity that can be triggered by slight stimuli. This, in turn, may affect QoL in these patients.[44,45]
The treatment applied on the thoracolumbar spine region aimed at influencing the sympathetic nerve supply to the colon.[46] However, although a slight reduction of pain was observed after the treatment (21.16%), it did not reach statistical significance, probably due to the heterogeneity observed in the pain score. When the sample size was calculated, this heterogeneity in pain was not contemplated, so this negative result should be taken cautiously because of the probability of committing a Type II error. This led us to analyze the effect of pain on IBDQ-32 scores. Interestingly, when taking pain into account, we observed that improvements were significantly lower in patients suffering from pain than in those who were not. These results strongly suggest that it is important to control the pain experienced by patients at the moment they are receiving the treatment since it could alter the outcomes. In this regard, other adjuvant physical approaches aimed at decreasing pain may be considered in order to increase the beneficial effects of the treatment. Nevertheless, this issue needs to be approached with caution and be verified in further studies.
Therefore, to the best of our knowledge, our study is the first to report significant physical improvements by means of a soft-techniques based treatment in patients with CD. In addition, we show that the proposed treatment results in an improvement in QoL, whether the patient is in the outbreak phase or the remission phase. Indeed, when analysis was conducted, the results proved that disease stage had no effect on the improvements achieved by the EG (P >.05). We believe that this fact is crucial, since this procedure may be used not only for the treatment of the outbreak period but also to reduce the duration or the intensity of the outbreak period. Since, so far, authors applying physical therapies in patients with CD have been conducted only in the remission phase of the disease,[15] future studies that verify this hypothesis are needed.
Finally, it is worth noting that none of the patients suffered any adverse effects, so the protocol used in this study can be considered a valid treatment option for this disease, alone or in combination with other physical/pharmacological therapies. This opens up the possibility of implementing this approach in patients with vertebral alterations (i.e., structural or degenerative), thus minimizing the possible risks associated with the performance of high-velocity manipulative techniques on patients with higher scores of self- reported pain.[47]
Nonetheless, this study has some limitations. There is a gender difference in the groups, however, it was due to the randomization of the sample that was (simple and not stratified). Regarding pain, the inclusion of another group receiving an adjuvant intervention aimed at reducing abdominal pain intensity would allow us to draw definite conclusions about the intervention effect on pain. On the other hand, it would have been interesting to study the implementation of a multidisciplinary approach including psycho-social intervention, in order to improve the global QoL scale or the emotional and social subscales.
5. Conclusion
Soft non-manipulative treatment is effective in improving overall and physical-related QoL in CD patients, regardless of the phase of the disease (outbreak or remission). Finally, although we did not observe a positive effect on pain reduction after the treatment, we are able to confirm that patients with higher scores of self- reported pain display lower improvements in QoL.
Acknowledgments
We express our thanks to the Valencian Association of Crohn's Disease and Ulcerative Colitis for their kind collaboration in the contribution of the sample.
Author contributions
Conceptualization: Gemma V Espí-López, Marta Inglés, Pilar Serra-Añó.
Data curation: Gemma V Espí-López, Isabel Soliva-Cazabán.
Formal analysis: Pilar Serra-Añó.
Investigation: Gemma V Espí-López.
Methodology: Gemma V Espí-López, Marta Inglés, Pilar Serra-Añó.
Project administration: Gemma V Espí-López.
Resources: Gemma V Espí-López, Marta Inglés, Isabel Soliva-Cazabán.
Software: Gemma V Espí-López, Pilar Serra-Añó.
Supervision: Gemma V Espí-López.
Writing – original draft: Gemma V Espí-López, Marta Inglés, Pilar Serra-Añó.
Writing – review & editing: Gemma V Espí-López, Pilar Serra-Añó.
Gemma V Espí-López orcid: 0000-0003-0042-8034.
Footnotes
Abbreviations: BMI = body mass index, CD = Crohn's disease, CG = control group, EG = experimental group, GQoL = global quality of life, IBD = inflammatory bowel disease, NPG = non-pain group, QoL = quality of life, QoLCD = quality of life specific for CD, VAS = Visual Analogue Scale.
GVE-L and MI contributed equally to this work.
ClinicalTrials.gov Protocol: NCT02763293
Approval was obtained from the author′s institution ethics committee (H1393258758403).
The authors declare that there is no conflict of interest.
References
- [1].Vermeire S, Van Assche G, Rutgeerts P. Review article: altering the natural history of Crohn's disease–evidence for and against current therapies. Aliment Pharmacol Ther 2007;25:3–12. [DOI] [PubMed] [Google Scholar]
- [2].Loftus EV. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology 2004;126:1504–17. [DOI] [PubMed] [Google Scholar]
- [3].Jess T, Winther KV, Munkholm P, et al. Mortality and causes of death in Crohn's disease: follow-up of a population-based cohort in Copenhagen County, Denmark. Gastroenterology 2002;122:1808–14. [DOI] [PubMed] [Google Scholar]
- [4].Ephgrave K. Extra-intestinal manifestations of Crohn's disease. Surg Clin North Am 2007;87:673–80. [DOI] [PubMed] [Google Scholar]
- [5].Feagan BG, Bala M, Yan S, et al. Unemployment and disability in patients with moderately to severely active Crohn's disease. J Clin Gastroenterol 2005;39:390–5. [DOI] [PubMed] [Google Scholar]
- [6].Becker HM, Grigat D, Ghosh S, et al. Living with inflammatory bowel disease: a Crohn's and Colitis Canada survey. Can J Gastroenterol Hepatol 2015;29:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cohen RD. The quality of life in patients with Crohn's disease. Aliment Pharmacol Ther 2002;16:1603–9. [DOI] [PubMed] [Google Scholar]
- [8].Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: Results of the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis 2007;1:10–20. [DOI] [PubMed] [Google Scholar]
- [9].Feagan BG, Vreeland MG, Larson LR, et al. Annual cost of care for Crohn's disease: a payor perspective. Am J Gastroenterol 2000;95:1955–60. [DOI] [PubMed] [Google Scholar]
- [10].Langhorst J, Wulfert H, Lauche R, et al. Systematic review of complementary and alternative medicine treatments in inflammatory bowel diseases. J Crohns Colitis 2014;9:86–106. [DOI] [PubMed] [Google Scholar]
- [11].Shanahan EM, Buchbinder R. The painful shoulder. Med Today 2011;11:73–9. [Google Scholar]
- [12].Bilski J, Brzozowski B, Mazur-Bialy A, et al. The role of physical exercise in inflammatory bowel disease. BioMed Res Int 2014;2014:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ng V, Millard W, Lebrun C, et al. Low-intensity exercise improves quality of life in patients with Crohn's disease. Clin J Sport Med 2007;17:384–8. [DOI] [PubMed] [Google Scholar]
- [14].Florance B-M, Frin G, Dainese R, et al. Osteopathy improves the severity of irritable bowel syndrome: a pilot randomized sham-controlled study. Eur J Gastroenterol Hepatol 2012;24:944–9. [DOI] [PubMed] [Google Scholar]
- [15].Piche T, Pishvaie D, Tirouvaziam D, et al. Osteopathy decreases the severity of IBS-like symptoms associated with Crohn's disease in patients in remission. Eur J Gastroenterol Hepatol 2014;26:1392–8. [DOI] [PubMed] [Google Scholar]
- [16].Schoon EJ, Wouters RS, Stockbrügger RW, et al. Osteopenia and osteoporosis in Crohn's disease: prevalence in a Dutch population-based cohort. Scand J gastroenterol 2000;(Supp 232):43–7. [PubMed] [Google Scholar]
- [17].Stevinson C, Ernst E. Risks associated with spinal manipulation. Am J Med 2002;112:566–71. [DOI] [PubMed] [Google Scholar]
- [18].Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. [DOI] [PubMed] [Google Scholar]
- [19].Espí-López GV, Rodríguez-Blanco C, Oliva-Pascual-Vaca A, et al. Effect of manual therapy techniques on headache disability in patients with tension-type headache. Randomized controlled trial. Eur J Phys Rehabil Med 2014;50:641–7. [PubMed] [Google Scholar]
- [20].Hanten WP, Olson SL, Hodson JL, et al. The effectiveness of CV-4 and resting position techniques on subjects with tension-type headaches. J Man Manip Ther 1999;7:64–70. [Google Scholar]
- [21].Liem T. Cranial osteopathy: a practical textbook. Seattle: Eastland Press; 2009. [Google Scholar]
- [22].Nicholas AS, Nicholas EA. Atlas of osteopathic techniques. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- [23].Goodheart GJ. Applied Kinesiology Research Manuals privately published yearly, Detroit, MI; 1964. [Google Scholar]
- [24].Beal MC. Viscerosomatic reflexes: a review. J Am Osteopath Assoc 1985;85:786–801. [PubMed] [Google Scholar]
- [25].Nelson KE. Viscerosomatic and somatovisceral reflexes. Somat Dysfunct Osteopath Fam Med. 2007;Philadelphia: Lippincott Williams & Wilkins, 33–55. [Google Scholar]
- [26].Elsevier Health Sciences, Chaitow L, Jones R. Chronic pelvic pain and dysfunction: Practical physical medicine. 2012. [Google Scholar]
- [27].Handspring Publishing Limited, Pilat A. Myofascial Induction: Therapy, theory and practice. 2016. [Google Scholar]
- [28].Elsevier Health Sciences, Barral J-P, Croibier A. Visceral vascular manipulations. 2011. [Google Scholar]
- [29].Ricard F. Tratamiento osteopático de las lumbalgias y ciáticas. Madr Panam 1998. 20. [Google Scholar]
- [30].Cella DF, Tulsky DS, Gray G, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 1993;11:570–9. [DOI] [PubMed] [Google Scholar]
- [31].Dapueto JJ, Francolino C, Servente L, et al. Evaluation of the functional assessment of cancer therapy-general (FACT-G) Spanish version 4 in South America: classic psychometric and item response theory analyses. Health Qual Life Outcomes 2003;1:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Winstead-Fry P, Schultz A. Psychometric analysis of the functional assessment of cancer therapy-general (FACT-G) scale in a rural sample. Cancer 1997;79:2446–52. [PubMed] [Google Scholar]
- [33].Guyatt G, Williams N, Goodacre R, et al. A new measure of health status for clinical trials in inflammatory bowel. Gastroenterology 1989;96:804–10. [PubMed] [Google Scholar]
- [34].Masachs M, Casellas F, Malagelada JR. Spanish translation, adaptation, and validation of the 32-item questionnaire on quality of life for inflammatory bowel disease (IBDQ-32)]. Rev Espanola Enfermedades Dig Organo Of Soc Espanola Patol Dig 2007;99:511–9. [DOI] [PubMed] [Google Scholar]
- [35].Verissimo R. Quality of life in inflammatory bowel disease: psychometric evaluation of an IBDQ cross-culturally adapted version. J Gastrointestin Liver Dis 2008;17:439–44. [PubMed] [Google Scholar]
- [36].Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- [37].Herrero MJ, Blanch J, Peri JM, et al. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen Hosp Psychiatry 2003;25:277–83. [DOI] [PubMed] [Google Scholar]
- [38].Brugman R, Fitzgerald K, Fryer G. The effect of osteopathic treatment on chronic constipation–a pilot study. Int J Osteopath Med 2010;13:17–23. [Google Scholar]
- [39].Caso M. Evaluation of Chapman's neurolymphatic reflexes via applied kinesiology: a case report of low back pain and congenital intestinal abnormality. J Manipulative Physiol Ther 2004;27:66–72. [DOI] [PubMed] [Google Scholar]
- [40].Upledger JE. Craniosacral therapy American Chiropractor 2004; 26:24–25 [Google Scholar]
- [41].Upledger JE, Vredevoogd JD. Craniosacral therapy. Seattle: Eastland Press; 1983. [Google Scholar]
- [42].Ashby EC. Abdominal pain of spinal origin. Value of intercostal block. Ann R Coll Surg Engl 1977;59:242–6. [PMC free article] [PubMed] [Google Scholar]
- [43].Perl ER. Mode of action of nociceptors. Cerv Pain. 1992;Oxford: Pergamon, 157–164. [Google Scholar]
- [44].Faure C, Giguere L. Functional gastrointestinal disorders and visceral hypersensitivity in children and adolescents suffering from Crohn's disease. Inflamm Bowel Dis 2008;14:1569–74. [DOI] [PubMed] [Google Scholar]
- [45].Van Oudenhove L, Demyttenaere K, Tack J, et al. Central nervous system involvement in functional gastrointestinal disorders. Best Pract Res Clin Gastroenterol 2004;18:663–80. [DOI] [PubMed] [Google Scholar]
- [46].Greenman PE. Principles of manual medicine. Philadelphia: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- [47].Cleland JA, Childs MJD, McRae M, et al. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther 2005;10:127–35. [DOI] [PubMed] [Google Scholar]


