Abstract
Background:
The efficacy of thoracic paravertebral block for thoracoscopic surgery remains controversial. We conduct a systematic review and meta-analysis to explore the impact of thoracic paravertebral block on thoracoscopic surgery.
Methods:
We search PubMed, EMbase, Web of science, EBSCO, and Cochrane library databases through August 2018 for randomized controlled trials (RCTs) assessing the effect of thoracic paravertebral block on thoracoscopic surgery. This meta-analysis is performed using the random-effect model.
Results:
Six RCTs involving 300 patients are included in the meta-analysis. Overall, compared with control group for thoracoscopic surgery, thoracic paravertebral block results in significantly reduced pain scores within 6 hours (Std. MD = −2.15; 95% CI = −3.67 to −0.62; P = .006), postoperative anesthesia consumption during 48 hours (Std. MD = −1.81; 95% CI = −3.05 to −0.58; P = .004), and hospital stay (Std. MD = −1.19; 95% CI = −2.13 to −0.26; P = .01), but has no important impact on pain scores at 24 hours (Std. MD = −1.10; 95% CI = −2.77–0.57; P = .20), and 48 hours (Std. MD = −1.25; 95% CI = −2.86–0.36; P = .13).
Conclusions:
Thoracic paravertebral block can substantially enhance pain management for thoracoscopic surgery.
Keywords: meta-analysis, pain scores, randomized controlled trials, thoracic paravertebral block, thoracoscopic surgery
1. Introduction
Thoracoscopic surgery has become great population for treating various diseases such as esophageal cancer and lung cancer because of its smaller incision, less pain and inflammatory response, reduced recovery times compared with traditional surgery.[1–3] Systemic opioids obtain limited efficacy, and result in unsatisfactory pain control and apparent side effects.[4–6]
Multimodal analgesic regimen has become increasing important for the optimal pain management after surgery, and they include both pharmacologic and regional interventions.[7–10] Paravertebral block serves as an ideal approach for thoracic and abdominal surgery through delivering segmental anesthesia of operative sites.[11,12] The probe is placed at the level of the targeted area (e.g., T5–6 interspace), and then a needle is inserted in a lateral-to-medial direction and kept advancing until the needle tip penetrates the internal intercostal membrane. Intermittent injection with normal saline is applied to assist locating the needle tip. After a negative aspiration test, the anesthetic drug is injected into the paravertebral space.[11] It can also achieve good muscle relaxation and prolonged postoperative analgesia.[13] Thoracic paravertebral block has superior analgesia and lung function, as well as fewer complications than systemic opioids.[14,15] It has been successfully applied in sternotomy, breast surgery, abdominoplasty, and laparoscopic cholecystectomy.[16–19]
However, the efficacy of thoracic paravertebral block for thoracoscopic surgery has not been well established. Recently, several studies on the topic have been published, and the results have been conflicting.[11,14,20,21] With accumulating evidence, we therefore perform a systematic review and meta-analysis of randomized controlled trials (RCTs) to investigate the efficacy of thoracic paravertebral block for thoracoscopic surgery.
2. Materials and methods
Ethical approval and patient consent are not required because this is a systematic review and meta-analysis of previously published studies. The systematic review and meta-analysis are conducted and reported in adherence to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).[22]
3. Search strategy and study selection
Two investigators have independently searched the following databases (inception to August 2018): PubMed, EMbase, Web of science, EBSCO, and Cochrane library databases. The electronic search strategy is conducted using the following keywords paravertebral block, and thoracoscopic or thoracoscopy. We also check the reference lists of the screened full-text studies to identify other potentially eligible trials.
The inclusive selection criteria are as follows: population: patients undergoing thoracoscopic surgery; intervention: thoracic paravertebral block; comparison: placebo or nothing; study design: RCT.
4. Data extraction and outcome measures
We have extracted the following information: author, number of patients, age, male, body mass index, American Society of Anesthesiologists (ASA, I/II) and detail methods in each group etc. Data have been extracted independently by 2 investigators, and discrepancies are resolved by consensus. We also contact the corresponding author to obtain the data when necessary.
The primary outcome is pain scores within 6 hours. Secondary outcomes include postoperative anesthesia consumption during 48 hours, pain scores at 24 and 48 hours, hospital stay.
5. Quality assessment in individual studies
Methodological quality of the included studies is independently evaluated using the modified Jadad scale.[23] There are 3 items for Jadad scale: randomization (0–2 points), blinding (0–2 points), dropouts and withdrawals (0–1 points). The score of Jadad scale varies from 0 to 5 points. An article with Jadad score ≤2 is considered to be of low quality. If the Jadad score ≥3, the study is thought to be of high quality.[24]
6. Statistical analysis
We estimate the standard mean difference (Std. MD) with 95% confidence interval (CI) for continuous outcomes (pain scores within 6 hours, postoperative anesthesia consumption during 48 hours, pain scores at 24 and 48 hours, hospital stay). A random-effects model is used regardless of heterogeneity. Heterogeneity is reported using the I2 statistic, and I2 > 50% indicates significant heterogeneity.[25] Whenever significant heterogeneity is present, we search for potential sources of heterogeneity via omitting one study in turn for the meta-analysis or performing subgroup analysis. Publication bias is not evaluated because of the limited number (<10) of included studies. All statistical analyses are performed using Review Manager Version 5.3 (The Cochrane Collaboration, Software Update, Oxford, UK).
7. Results
7.1. Literature search, study characteristics and quality assessment
A detailed flowchart of the search and selection results is shown in Fig. 1. Five hundred thirty-seven potentially relevant articles are identified initially. Finally, 6 RCTs that meet our inclusion criteria are included in the meta-analysis.[11,12,14,20,21,26]
Figure 1.
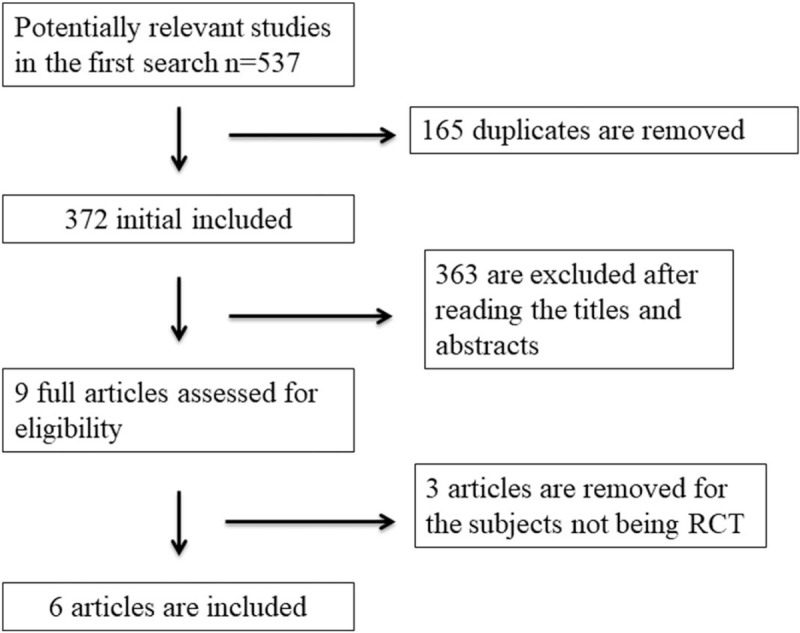
Flow diagram of study searching and selection process.
The baseline characteristics of the 6 eligible RCTs in the meta-analysis are summarized in Table 1. The 6 studies are published between 2005 and 2016, and sample sizes range from 40 to 80 with a total of 300. Three RCTs report thoracic paravertebral block with ropivacaine,[11,20,21] and the remaining 3 RCTs report the bupivacaine.[12,14,26]
Table 1.
Characteristics of included studies.
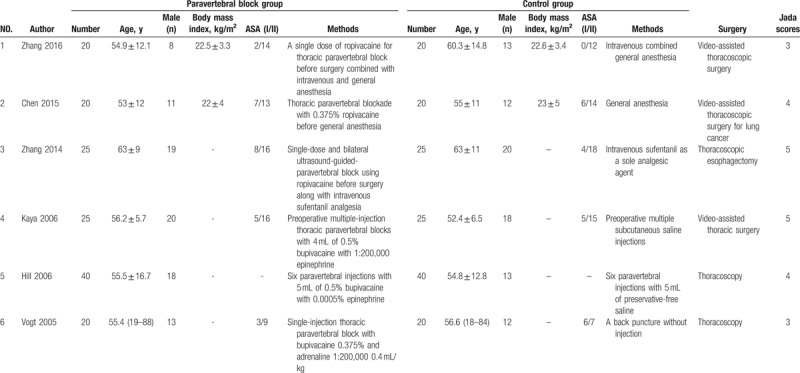
Among the 6 studies included here, 4 studies report pain scores within 6 hours,[12,14,20,21] 4 studies report postoperative anesthesia consumption during 48 hours,[11,14,20,26] 3 studies report pain scores at 24 and 48 hours,[14,20,21] and 3 studies report hospital stay.[11,14,20] Jadad scores of the 6 included studies vary from 3 to 5, and all 6 studies are considered to be high-quality ones according to quality assessment.
7.2. Primary outcome: pain scores within 6 hours
This outcome data is analyzed with the random-effects model, and the pooled estimate of the 4 included RCTs suggested that compared with control group for thoracoscopic surgery, thoracic paravertebral block is associated with significantly reduced pain scores within 6 hours (Std. MD = −2.15; 95% CI = −3.67 to −0.62; P = .006), with significant heterogeneity among the studies (I2 = 95%, heterogeneity P < .00001) (Fig. 2).
Figure 2.
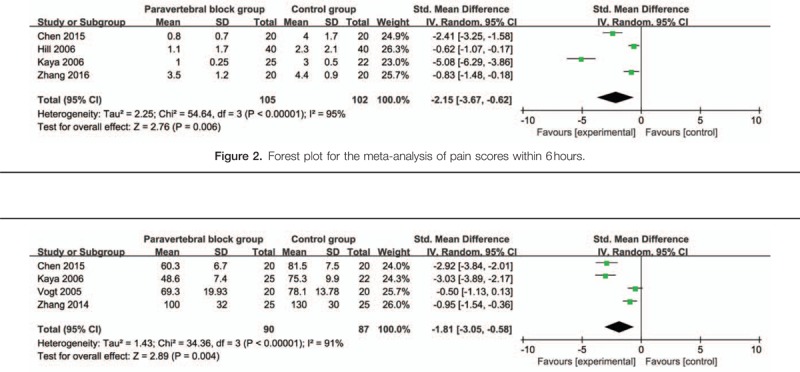
Forest plot for the meta-analysis of pain scores within 6 hours.
7.3. Sensitivity analysis
Significant heterogeneity is observed among the included studies for the primary outcomes, but there is still significant heterogeneity after when performing sensitivity analysis via omitting one study in turn or subgroup analysis based on anesthetic drug to detect the heterogeneity.
7.4. Secondary outcomes
Compared with control group for thoracoscopic surgery, thoracic paravertebral block can significantly reduce postoperative anesthesia consumption during 48 hours (Std. MD = −1.81; 95% CI = −3.05 to −0.58; P = .004; Fig. 3), but has no important impact on pain scores at 24 hours (Std. MD = −1.10; 95% CI = −2.77 to 0.57; P = .20; Fig. 4) and 48 hours (Std. MD = −1.25; 95% CI = −2.86–0.36; P = .13; Fig. 5). Hospital stay is substantially decreased by thoracic paravertebral block than control intervention (Std. MD = −1.19; 95% CI = −2.13 to −0.26; P = .01; Fig. 6).
Figure 3.
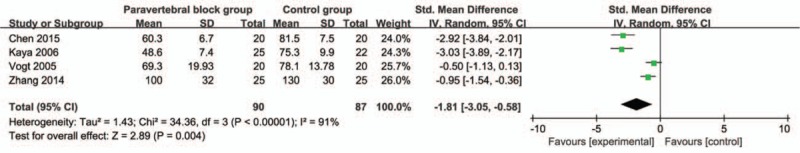
Forest plot for the meta-analysis of postoperative anesthesia consumption during 48 hours.
Figure 4.
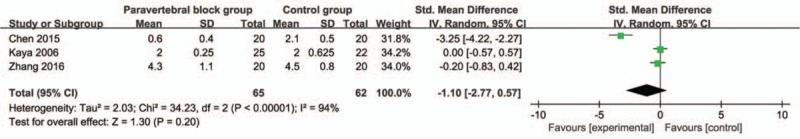
Forest plot for the meta-analysis of pain scores at 24 hours.
Figure 5.
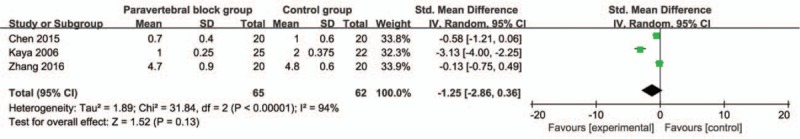
Forest plot for the meta-analysis of pain scores at 48 hours.
Figure 6.
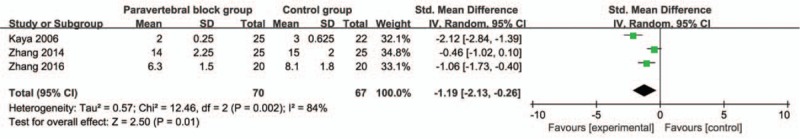
Forest plot for the meta-analysis of hospital stay (day).
8. Discussion
One meta-analysis has reported that injection (single or multilevel) and local anesthetic agent (type, concentration, and volume) can significantly affect the analgesic efficacy. 3-site and bilateral paravertebral block are performed at the right T5 and bilateral T8 levels in order to cover T3–11 right dermatomes and T6–11 left. Enhanced analgesic efficacy and decreased adverse events are produced by the method of paravertebral block.[27] The effective duration of single-injection paravertebral block is up to 12 hours.[28] This prolonged analgesia also relies on the relative avascularity of the paravertebral space which benefits to slow uptake of local anesthetics, increase a preemptive efficacy of paravertebral block, and reduce the nociceptive input to the central nervous system.[29,30]
In one RCT, thoracic paravertebral block is found to lower pain scores only at the first 8 hours for thoracoscopic surgery, and reduces the patient-controlled analgesia sufentanil consumption within postoperative 48 hours.[11] Our meta-analysis suggests that compared with control intervention for thoracoscopic surgery, thoracic paravertebral block is associated with substantially decreased pain scores within 6 hours, and postoperative anesthesia consumption during 48 hours, but shows no significant influence on pain scores at 24 and 48 hours. In addition, hospital stay is remarkably decreased after the thoracic paravertebral block intervention, which is very important for the enhanced recovery after surgery.
Regarding the sensitivity analysis, there is still significant heterogeneity when performing the analysis by via omitting one study in turn or subgroup analysis based on anesthetic drug. Several reasons may explain this significant heterogeneity. Firstly, different drugs are applied for paravertebral block including ropivacaine and bupivacaine. Secondly, these anesthetic drugs have various concentrations such as bupivacaine 0.375% and 0.5%. Thirdly, the injection numbers of paravertebral block also has the important influence on the anesthetic efficacy, and include single-level and multiple-level block. Fourthly, the detail methods and procedures of thoracoscopic surgery are different, such as for lung cancer or esophageal cancer. Wedge resection may have better analgesic efficacy than lobectomy. Fifthly, the included RCTs involve 2 levels of paravertebral space with unilateral block,[20] 3 levels of paravertebral space with unilateral block,[21] 2 levels of paravertebral space with unilateral block for T5 and bilateral block for T8,[11] 4 levels of paravertebral space with unilateral block,[14] 5 levels of paravertebral space unilateral block,[12] and single level of paravertebral space with unilateral block.[26] Multiple levels block appears to have better analgesic effect than single level block during paravertebral block for thoracoscopic surgery.
All included RCTs report no serious adverse events after paravertebral block intervention. One included RCT reports that paravertebral block results in lower incidence of adverse effects (e.g., nausea, vomiting, drowsiness, atrial arrhythmia, hypotension, and pneumonia) for thoracoscopic surgery, but with no significant difference when compared with control intervention.[11] This meta-analysis has several potential limitations. Firstly, our analysis is based on only 6 RCTs, and all of them have a relatively small sample size (n < 100). Overestimation of the treatment effect was more likely in smaller trials compared with larger samples. Next, the types, concentrations, and methods of anesthetic drugs in included RCTs are different, which may have an influence on the pooling results. Finally, thoracoscopic surgeries are performed for various diseases and operation procedures.
9. Conclusions
Thoracic paravertebral block has important beneficial effects on pain control for thoracoscopic surgery.
Author contributions
Conceptualization: Tianyang Dai.
Formal analysis: Zhi Hu, Tianyang Dai.
Methodology: Zhi Hu, Dan Liu.
Software: Dan Liu.
Supervision: Zhi-Zhen Wang.
Writing – original draft: Zhi-Zhen Wang, Biao Wang.
Writing – review & editing: Biao Wang.
Footnotes
Abbreviations: CI = confidence interval, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCTs = randomized controlled trials, SMD = standard mean difference.
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
The authors declare that they have no competing interests.
Funding: Not applicable.
Authors have no conflicts of interest to disclose.
References
- [1].Murakawa T, Sato H, Okumura S, et al. Thoracoscopic surgery versus open surgery for lung metastases of colorectal cancer: a multi-institutional retrospective analysis using propensity score adjustmentdagger. Eur J Cardiothorac Surg 2017;51:1157–63. [DOI] [PubMed] [Google Scholar]
- [2].Kinjo Y, Kurita N, Nakamura F, et al. Effectiveness of combined thoracoscopic-laparoscopic esophagectomy: comparison of postoperative complications and midterm oncological outcomes in patients with esophageal cancer. Surg Endosc 2012;26:381–90. [DOI] [PubMed] [Google Scholar]
- [3].Pham TH, Perry KA, Dolan JP, et al. Comparison of perioperative outcomes after combined thoracoscopic-laparoscopic esophagectomy and open Ivor-Lewis esophagectomy. Am J Surg 2010;199:594–8. [DOI] [PubMed] [Google Scholar]
- [4].Karnik PP, Dave NM, Garasia M. Comparison of analgesic efficacy and safety of continuous epidural infusion versus local infiltration and systemic opioids in video-assisted thoracoscopic surgery decortication in pediatric empyema patients. Saudi J Anaesth 2018;12:240–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Beltran R, Veneziano G, Bhalla T, et al. Postoperative pain management in patients undergoing thoracoscopic repair of pectus excavatum: a retrospective analysis of opioid consumption and adverse effects in adolescents. Saudi J Anaesth 2017;11:427–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Rahman NM, Pepperell J, Rehal S, et al. Effect of opioids vs NSAIDs and larger vs smaller chest tube size on pain control and pleurodesis efficacy among patients with malignant pleural effusion: the TIME1 randomized clinical trial. JAMA 2015;314:2641–53. [DOI] [PubMed] [Google Scholar]
- [7].Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy--a systematic review and meta-analysis of randomized trials. Br J Anaesth 2006;96:418–26. [DOI] [PubMed] [Google Scholar]
- [8].Sztain JF, Gabriel RA, Said ET. Thoracic epidurals are associated with decreased opioid consumption compared to surgical infiltration of liposomal bupivacaine following video-assisted thoracoscopic surgery for lobectomy: a retrospective cohort analysis. J Cardiothorac Vasc Anesth 2018;pii: S1053-0770(18)30403-8. [DOI] [PubMed] [Google Scholar]
- [9].Adhikary SD, Pruett A, Forero M, et al. Erector spinae plane block as an alternative to epidural analgesia for post-operative analgesia following video-assisted thoracoscopic surgery: a case study and a literature review on the spread of local anaesthetic in the erector spinae plane. Indian J Anaesth 2018;62:75–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wang X, Wang K, Wang B, et al. Effect of oxycodone combined with dexmedetomidine for intravenous patient-controlled analgesia after video-assisted thoracoscopic lobectomy. J Cardiothorac Vasc Anesth 2016;30:1015–21. [DOI] [PubMed] [Google Scholar]
- [11].Zhang W, Fang C, Li J, et al. Single-dose, bilateral paravertebral block plus intravenous sufentanil analgesia in patients with esophageal cancer undergoing combined thoracoscopic-laparoscopic esophagectomy: a safe and effective alternative. J Cardiothorac Vasc Anesth 2014;28:966–72. [DOI] [PubMed] [Google Scholar]
- [12].Hill SE, Keller RA, Stafford-Smith M, et al. Efficacy of single-dose, multilevel paravertebral nerve blockade for analgesia after thoracoscopic procedures. Anesthesiology 2006;104:1047–53. [DOI] [PubMed] [Google Scholar]
- [13].Richardson J, Lonnqvist PA, Naja Z. Bilateral thoracic paravertebral block: potential and practice. Br J Anaesth 2011;106:164–71. [DOI] [PubMed] [Google Scholar]
- [14].Kaya FN, Turker G, Basagan-Mogol E, et al. Preoperative multiple-injection thoracic paravertebral blocks reduce postoperative pain and analgesic requirements after video-assisted thoracic surgery. J Cardiothorac Vasc Anesth 2006;20:639–43. [DOI] [PubMed] [Google Scholar]
- [15].Abo-Zeid MA, Elgamal MM, Hewidy AA, et al. Ultrasound-guided multilevel paravertebral block versus local anesthesia for medical thoracoscopy. Saudi J Anaesth 2017;11:442–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Canto M, Sanchez MJ, Casas MA, et al. Bilateral paravertebral blockade for conventional cardiac surgery. Anaesthesia 2003;58:365–70. [DOI] [PubMed] [Google Scholar]
- [17].Rudkin GE, Gardiner SE, Cooter RD. Bilateral thoracic paravertebral block for abdominoplasty. J Clin Anesth 2008;20:54–6. [DOI] [PubMed] [Google Scholar]
- [18].Naja ZM, El-Rajab M, Ziade F, et al. Preoperative vs. postoperative bilateral paravertebral blocks for laparoscopic cholecystectomy: a prospective randomized clinical trial. Pain Pract 2011;11:509–15. [DOI] [PubMed] [Google Scholar]
- [19].Stamatiou G, Athanasiou E, Simeoforidou M, et al. Thoracic paravertebral block for breast surgery. Anaesthesia 2004;59:723–4. [DOI] [PubMed] [Google Scholar]
- [20].Zhang B, Liu DY. Application of thoracic paravertebral nerve block in video-assisted thoracosopic surgery: a randomized controlled trial. Nan Fang Yi Ke Da Xue Xue Bao 2016;37:460–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chen J, Zhang Y, Huang C, et al. Effects of thoracic paravertebral block on postoperative analgesia and serum level of tumor marker in lung cancer patients undergoing video-assisted thoracoscopic surgery. Zhongguo Fei Ai Za Zhi 2015;18:104–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Moher D, Liberati A, Tetzlaff J, et al. Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. [DOI] [PubMed] [Google Scholar]
- [23].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [24].Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med 2001;135:982–9. [DOI] [PubMed] [Google Scholar]
- [25].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [26].Vogt A, Stieger DS, Theurillat C, et al. Single-injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery. Br J Anaesth 2005;95:816–21. [DOI] [PubMed] [Google Scholar]
- [27].Kotze A, Scally A, Howell S. Efficacy and safety of different techniques of paravertebral block for analgesia after thoracotomy: a systematic review and metaregression. Br J Anaesth 2009;103:626–36. [DOI] [PubMed] [Google Scholar]
- [28].Klein SM, Bergh A, Steele SM, et al. Thoracic paravertebral block for breast surgery. Anesth Analg 2000;90:1402–5. [DOI] [PubMed] [Google Scholar]
- [29].Matyal R, Montealegre-Gallegos M, Shnider M, et al. Preemptive ultrasound-guided paravertebral block and immediate postoperative lung function. Gen Thorac Cardiovasc Surg 2015;63:43–8. [DOI] [PubMed] [Google Scholar]
- [30].Kaya FN, Turker G, Mogol EB, et al. Thoracic paravertebral block for video-assisted thoracoscopic surgery: single injection versus multiple injections. J Cardiothorac Vasc Anesth 2012;26:90–4. [DOI] [PubMed] [Google Scholar]


