Abstract
Objective:
To determine the association between low maternal vitamin D levels and preterm delivery among parturients in Lagos, Nigeria.
Methods:
The present study was analytical cross-sectional study of women with preterm deliveries (defined as <37 weeks) and women with term deliveries (defined as ≥37 weeks) at the labor unit of Lagos University Teaching Hospital between December 2015 and October 2016. Relevant information was obtained via a proforma, and maternal venous samples were collected immediately after delivery. Serum 25-hydroxy vitamin D was determined by a vitamin D enzyme-linked immunoassay kit.
Results:
The study enrolled 103 women in each group. The overall prevalence of vitamin D deficiency was 14.1% (29/206). Twenty-four (23.3%) women with preterm delivery had low serum vitamin D (<30 ng/mL) as compared with only 5 (4.9%) women with term delivery (P<0.001). As compared with normal serum vitamin D levels, low maternal vitamin D had an approximately nine-fold higher likelihood of preterm delivery (adjusted odds ratio 9.41, 95% confidence interval 2.42–36.54; P<0.001).
Conclusion:
The prevalence of serum vitamin D deficiency was higher among women with preterm delivery than among those with term delivery. The potential role of prenatal vitamin D supplementation in the prevention of preterm delivery should be further investigated.
Keywords: Lagos, Nigeria, Parturients, Preterm, Term deliveries, Vitamin D deficiency
1. INTRODUCTION
Interest in the diverse functions of vitamin D in the human body continues to increase in the medical world. Vitamin D, a fat-soluble vitamin, has both classical and non-classical effects [1,2]. Its classical effects involve maintaining the skeleton by regulating calcium and phosphate homeostasis; its non-classical effects include its anti-bacterial influence, mediated through intricate interactions between vitamin D and the immune system [1]. Vitamin D supplementation enhances production of the anti-bacterial protein cathelicidin after monocyte activation [3]. Within the placenta, conversion of vitamin D from 25-hydroxyvitamin D (its most widely available form in the human body) to 1,25-dihydroxy vitamin D (its metabolically active form) in response to maternal vitamin D status exerts immunomodulatory properties [1,2].
Prematurity, resulting from preterm birth, is the leading cause of perinatal morbidity and mortality, with attendant effects on maternal health and also on the emotional and socioeconomic wellbeing of the family. It is estimated that 15 million neonates are delivered preterm annually, and this number is thought to be rising [4]. Estimates from 184 countries indicate that the frequency of preterm birth ranges from 5% to 18%, and that more than 60% of preterm neonates are delivered in Africa and south Asia [4]. Complications arising from preterm delivery are the leading cause of mortality among children younger than 5 years [5].
Preterm delivery that results from preterm rupture of membranes or spontaneous preterm labor is associated with an increased incidence of placental infection and inflammation [6]. Vitamin D plays an important role in suppressing such placental infections and inflammation [3]. Studies have reported an increased prevalence of preterm delivery among women with vitamin D deficiency when compared with women with normal vitamin D levels [7,8].
Vitamin D levels in humans are influenced by various factors such as duration of exposure of vital skin surfaces to sunlight, skin type, clothing type, availability of a vitamin D-rich diet, body mass index, and presence of chronic disease, among others. The aim of the present study was therefore to determine the levels of serum vitamin D in a matched population of women with preterm and term deliveries, and to assess whether there is an association between low serum vitamin D levels and preterm delivery among pregnant women in Lagos, Nigeria.
2. MATERIALS AND METHODS
The present analytical cross-sectional study was carried out among parturients at the labor unit of the Lagos University Teaching Hospital between December 1, 2015, and October 31, 2016. Ethical approval for the study was obtained from the research and ethics committee of the hospital. All participants were counselled before enrollment, and read and signed an informed consent form. The investigators ensured strict confidentiality of participant information.
The study enrolled two groups of women. The case group comprised women with preterm delivery, defined as delivery before a gestational age of 37 weeks; the control counterparts comprised women with term delivery, defined as delivery at and after 37 gestational weeks. The study included established parturients with a singleton fetus of at least 28 gestational weeks, those with no known medical condition, those with no history of vitamin D supplement intake, and those who provided informed written consent. The exclusion criteria were multiple gestation, and refusal of consent or withdrawal of consent during the study.
The sample size was estimated on the basis of previous studies [9,10], assuming a rate of preterm delivery of 10% for women with low serum vitamin D levels and 5% for those with normal serum vitamin D levels. Power analysis indicated that a minimum sample size of 103 women in each group (total sample size, 206 women) would be required to ensure at least 80% power to detect the anticipated between-group differences, allowing for an attrition or non-response rate of 10%.
A structured interviewer-administered questionnaire was used for data collection. Gestational age was based on the participants’ last normal menstrual period, and confirmed or modified by a first- or early second-trimester ultrasound. Maternal sociodemographic data and characteristics such as skin color and clothing type among others were obtained at presentation and from medical records.
A venous blood sample (5 mL) was collected immediately after delivery and sent to the laboratory. The samples were then centrifuged, and the serum was stored at −20oC until analysis. The level of total 25-hydroxyvitamin D in each serum sample was measured by using a solid-phase competitive enzyme-linked immunosorbent assay in accordance with the manufacturer’s instructions (Calbiotech, Spring Valley, CA, USA). Low serum vitamin D was defined as a level below 30 ng/mL.
The study data were analyzed by using SPSS version 22.0 (IBM, Armonk, NY, USA), and descriptive statistics were computed for relevant data. Quantitative data were tested for normality with the Kolmogorov–Smirnov test. The independent sample t test or Mann–Whitney U test was used to compare continuous variables. χ2 test was used to test for an association between categoric variables and preterm delivery. Maternal age and variables that had a P value by χ2 test were included in binary logistic regression models to study the relationship between low serum vitamin D levels and preterm delivery. A P value of less than 0.05 was considered statistically significant.
3. RESULTS
The characteristics of the study women in each group are shown in Table 1. The mean age of women was 31.1 ± 5.6 years for those with preterm delivery 30.8 ± 4.7 years for those with term delivery (P=0.619). There was no significant difference in parity (P=0.826), BMI (P=0.263), religion (P=0.158), or dressing style (P=0.521) between the preterm and term groups. There were, however, significant differences in educational level (P<0.001), booking status (P<0.001), alcohol use (P=0.019), tobacco smoking (P=0.008), and skin color (P=0.013) between the two groups of parturients.
Table 1.
Baseline characteristics of study participants a.
| Characteristic | Preterm delivery (n=103) | Term delivery (n=103) | P value |
|---|---|---|---|
| GA wk | 32.0 (29.0–34.0) | 39.0 (38.0–39.0) | |
| Age, y | 31.1 ± 5.6 | 30.8 ± 4.7 | 0.619 |
| Parity | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 0.826 |
| BMI | 27.7 (27.6–30.5) | 29.9 (26.7–32.4) | 0.263 |
| Educational level | <0.001 | ||
| Primary | 14 (13.6) | 12 (11.7) | |
| Secondary | 71 (68.9) | 28 (27.2) | |
| Tertiary | 18 (17.5) | 63 (61.2) | |
| Religion | 0.158 | ||
| Christianity | 65 (63.1) | 55 (53.4) | |
| Islam | 38 (36.9) | 48 (46.6) | |
| Booking status | <0.001 | ||
| Booked | 23 (22.5) | 87 (84.5) | |
| Unbooked | 79 (77.5) | 16 (15.5) | |
| Dressing style | 0.521 | ||
| Covered | 24 (23.3) | 28 (27.2) | |
| Uncovered | 79 (76.7) | 75 (72.8) | |
| Alcohol intake | 0.019 | ||
| Yes | 15 (14.6) | 5 (4.9) | |
| Never | 88 (85.4) | 98 (95.1) | |
| Smoking | 0.008 | ||
| Yes | 6 (5.8) | 2 (1.9) | |
| Never | 97 (94.2) | 101 (98.1) | |
| Skin color | 0.013 | ||
| Light | 45 (43.7) | 28 (27.2) | |
| Dark | 58 (56.3) | 75 (72.8) | |
| Vitamin D levels | <0.001 | ||
| Low (<30 ng/mL) | 24 (23.3) | 5 (4.9) | |
| Normal (≥30 ng/mL) | 79 (76.7) | 98 (95.1) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by the square of height in meters); GA, gestational age.
Values are given as mean ± SD, median (interquartile range), or number (percentage) unless stated otherwise.
Overall, 29 (14.1%) of the 206 study women had vitamin D deficiency. Twenty-four (23.3%) women with preterm delivery had low serum vitamin D level as compared with only 5 (4.9%) women with term delivery (P<0.001) (Table 1). The median (interquartile range) level of vitamin D was 46.0 ng/mL (30.0–56.5 ng/mL) in the preterm group and 57.0 ng/mL (45.0–66.0 ng/mL) in the term group.
In a multivariate analysis controlling for age, level of education, religion, booking status, alcohol intake, smoking of tobacco, and skin color as confounding variables, women with low vitamin D levels had an approximately nine-fold higher likelihood of preterm delivery as compared with women with normal vitamin D levels (adjusted odds ratio 9.41, 95% confidence interval 2.42–36.54).
4. DISCUSSION
The present study found that the prevalence of vitamin D deficiency was relatively low among parturients in Lagos, Nigeria, and that maternal hypovitaminosis D was significantly associated with preterm delivery. These findings might have future implications for the prevention of preterm delivery among women of Nigerian descent.
The overall prevalence of vitamin D deficiency recorded in the present study was 14.1%, which is approximately one-half of the prevalence of 29% reported in a prospective study conducted in similar settings in Lagos [11]. Despite this disparity, the population of participants recruited in these two studies were mostly well educated and likely to consume diets that are rich in vitamin D and other nutrients as compared with women who delivered outside the health facilities. In studies in the United States [12] and China [8], by contrast, the reported prevalence of vitamin D deficiency was 70% and 50%, respectively. Several studies have shown that serum 25-hydroxy vitamin D deficiency is higher among dark-skinned women than among lighter skin women [13–15], because dark-complexioned women possess more melanin, which protects their skin against damage from ultraviolet B exposure as compared with fair-skinned and white women. The present study might differ from these other studies because it was conducted in Lagos, Nigeria, which is a largely sunny region all year round where a considerable proportion of women do not wear full-coverage clothing, as reflected in the present findings. The women are therefore exposed to more sunlight, which is the major source of naturally occurring vitamin D [16,17].
The present study showed that the prevalence of vitamin D deficiency was higher among women with preterm delivery than among those with term delivery. This finding is supported by a previous meta-analysis that found that vitamin D deficiency was a significant risk factor for preterm birth [7]. Several other studies comparing preterm and term delivery also found a higher prevalence of vitamin D deficiency among women with preterm than among those with term delivery [8,13,18]. However, other studies by Gbadegesin et al. [11] in Lagos, Nigeria, and Yang et al. [19] in Guangdong, China, found no association between vitamin D deficiency and pregnancy complications including preterm delivery.
The study has some limitations. Although, similar to previous studies, the study found that vitamin D deficiency is more prevalent among preterm deliveries as compared with term deliveries, a cause and effect relationship cannot be established because of the study design employed. Another limitation was the difficulty in extracting reliable information on the intake of vitamin D-rich diets from the study women, and this factor might have had a direct or indirect influence on the observed association noted in the study.
In conclusion, the present study showed that serum 25-hydroxy vitamin D deficiency was more prevalent among women with preterm delivery than among those with term delivery. It is therefore important for women to have optimized serum vitamin D levels in pregnancy to reduce this adverse pregnancy outcome. However, a large, well-designed, multicenter, randomized control trial involving black African women is recommended to further validate the role of routine prenatal vitamin D supplementation in improving maternal and perinatal outcomes including preterm delivery.
Figure 1.
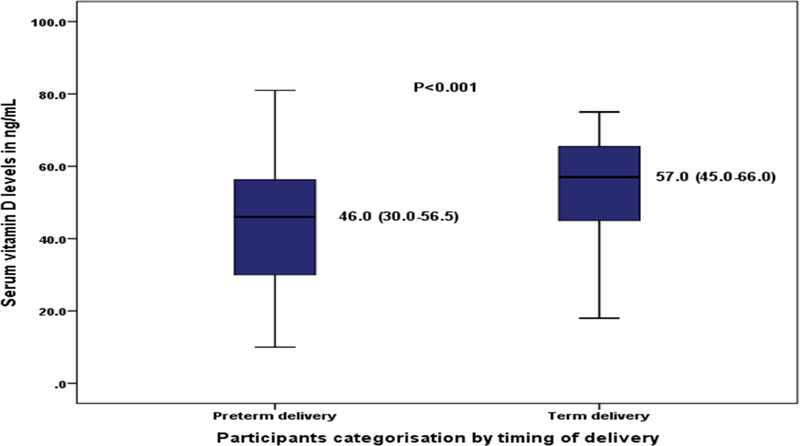
Serum vitamin D levels among the study participants by timing of delivery.
Table 2.
Multivariate analysis of the relationships between baseline characteristics and preterm delivery among study the participants (n=206).
| Characteristic | Adjusted OR (95% CI) | P value |
|---|---|---|
| Maternal age, y | ||
| <35 | 1.00 (Ref.) | |
| ≥35 | 1.25 (0.47–3.34) | 0.660 |
| Educational level | ||
| Primary | 1.00 (Ref.) | |
| Secondary | 0.60 (0.17–2.13) | 0.428 |
| Tertiary | 0.13 (0.05–0.34) | <0.001 |
| Religion | ||
| Christianity | 1.00 (Ref.) | |
| Islam | 0.53 (0.23–1.23 ) | 0.141 |
| Booking status | ||
| Booked | 1.00 (Ref.) | |
| Unbooked | 17.88 (7.36–43.40) | <0.001 |
| Alcohol intake | ||
| Yes | 1.00 (Ref.) | |
| Never | 0.18 (0.04–0.77) | 0.021 |
| Tobacco smoking | ||
| Yes | 1.00 (Ref.) | |
| Never | 0.76 (0.25–1.11) | 0.091 |
| Skin color | ||
| Light | 1.00 (Ref.) | |
| Dark | 0.61 (0.26–1.43) | 0.253 |
| Vitamin D | ||
| Normal | 1.00 (Ref.) | |
| Low | 9.41 (2.42–36.54) | 0.001 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Synopsis:
The prevalence of maternal vitamin D deficiency among pregnant women in Nigeria was low. Maternal vitamin D status was significantly associated with preterm delivery.
Acknowledgments
The study was supported, in part, by the Fogarty International Center and National Institute of Mental Health of the National Institutes of Health (no. D43TW010543). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of interest
The authors have no conflicts of interest.
References
- [1].Zitterman A, Gunmmert JF. Non-classical Vitamin D action. Nutrients 2010; 2(4): 408–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Wacker M, Holick MF. Vitamin D effects on skeletal and extra skeletal health and the need for supplementation. Nutrients 2013; 5(1): 111–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fabri M, Stenger S, Shin D-M, Yuk J-M, Liu PT, Realegeno S, et al. Vitamin D is required for IFN gamma mediated antimicrobial activity of human macrophages. Sci transl med 2011: 12; 3(104): 104–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. The Lancet 2012; 379(9832): 2162–72 [DOI] [PubMed] [Google Scholar]
- [5].Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016; 388(10063): 3027–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Galinsky R, Polglase GR, Hooper SB, Black MJ, Moss TJM. The Consequences of Chorioamnionitis: Preterm Birth and Effects on Development. J Pregnancy 2013; 2013: 412831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Qin L, Lu F, Yang S, Xu H, Luo B. Does Maternal Vitamin D Deficiency increase the Risk of Preterm Birth. A meta-analysis of Observational studies. Nutrients 2016; 8(5): 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zhu T, Liu T, Ge X, Kong J, Zhang L, Zhao Q. High prevalence of maternal vitamin D deficiency in preterm birth in Northeast China, Shenyang. Int J Clin Exp Pathol 2015. 8(2): 1459–1465 [PMC free article] [PubMed] [Google Scholar]
- [9].Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, Roberts JM, et al. High prevalence of vitamin D insufficiency in Black and White pregnant women residing in the Northern United States and their Neonates. J Nutr 2007;137(2): 447–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Oluwole AA, Adegbesan–Omilabu MA, Okunade KS. Preterm delivery and low maternal serum cholesterol level; Any correlation? Niger Med J 2014; 55(5): 406–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gbadegesin A, Sobande A, Adedeji O, Disu E, Korede O, Dosunmu A, et al. Maternal serum vitamin D levels and pregnancy outcomes: from Lagos, Nigeria. J Obstet Gynaecol 2017; 37(1): 25–28 [DOI] [PubMed] [Google Scholar]
- [12].Flood-Nichols SK, Tinnemore D, Huang RR, Napolitano PG, Ippolito DL. Vitamin D deficiency in early pregnancy. PLoS One 2015;10(4): e0123763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Thota C, Menon R, Fortunato SJ, Brou L, Lee JE, Al-Hendy A. 1,25-Dihydroxyvitamin D deficiency is associated with preterm birth in African American and Caucasian women. Reprod Sci 2014; 21(2): 244–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Al-Waria H, Abo-Ouf N. Prevalence of vitamin D deficiency in mother-infant pairs in a tertiary hospital in the west coast of Saudi Arabia. J clin Neonatol 2016; 5: 243–246 [Google Scholar]
- [15].Merewood A, Mehta SD, Grossman X, Chen TC, Mathieu JS, Holick MF, Bauchner H. Widespread vitamin D deficiency in Urban Massachusetts newborns and their mothers. Paediatrics 2010; 125(4): 640–647 [DOI] [PubMed] [Google Scholar]
- [16].Deluca H Overview of general physiologic features and function of vitamin D. Am J. Clin Nutria 2004; 80: 1689–96 [DOI] [PubMed] [Google Scholar]
- [17].Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune disease, cancer and cardiovascular disease. Am J. Clin Nutri 2004; 80(6): 1678–1688 [DOI] [PubMed] [Google Scholar]
- [18].Wagner CL, Baggerly C, McDonnell SL, Baggerly L, Hamilton SA, Winkler J, et al. Post-hoc comparison of vitamin D status at three timepoints during pregnancy demonstrates lower risk of preterm birth with higher vitamin D closer to delivery. J Steroid Biochem Mol Biol 2015; 148: 256–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Yang L, Pan S, Zhou Y, Wang X, Qin A, Huang Y, et al. The Correlation Between Serum Vitamin D Deficiency and Preterm Birth. Med Sci Monit 2016; 22: 4401–4405. [DOI] [PMC free article] [PubMed] [Google Scholar]


