Abstract
A long-standing trend that will continue to grow in healthcare is providing high quality services for all the patient, no matter the distance and no matter the place. One approach currently being used to increase population access to healthcare services is telemedicine. This narrative review presents one branch of e-health, in particular the use of teleultrasonography (TUS) in clinical practice, the challenges and barriers encountered. Current advances in ultrasound technology, including the growth of portable and small ultrasound devices have increased the range of applications of TUS, from traumatic patients in emergency medicine, maternal ultrasound and even for monitoring and screening for chronic illnesses. Even though some barriers are still looking for a solution, like standardized training and protocols, errors in data acquisition, the lack of trained professionals to operate in remote areas, TUS has the potential to redesign future health care systems.
Keywords: telemedicine, teleultrasonography, remote medicine
Introduction
For the past 30 years, innovation, especially in the digital field, has improved many professional fields, being difficult to find a sector or industry where information technology has not been greatly influenced. In medicine, the advances in telecommunication combined with the evolution of information technology industry plays a substantial role, transforming and improving health services. The field of telemedicine, at first regarded as unreliable and unaffordable, has rapidly evolved in the past 20 years and this new modality of healthcare delivery emerged as an attractive and efficient way of improving the quality of care.
Described as the „stethoscope of the future” [1], ultrasound is the imaging technology most easily adaptable to provide a rapid and non-invasive bedside diagnosis as well as interventional procedures, such as paracentesis, thoracocentesis, pericardiocentesis, etc. Moreover, ultrasound technology become more reliable, less expensive and even reduced to hand-held devices. With the growth of portable ultrasound devices and having the technology to transmit images by using satellite and mobile networks transmission, reproducible ultrasound images can be easily referred to a specialist [2]. Teleultrasonography (TUS) has increased its range of applications, being used for traumatic patients in emergency medicine, maternal ultrasound and even for monitoring and screening for chronic illnesses such as cardiovascular disease.
Current advances in ultrasound technology coupled with telemedicine are increasingly becoming a reliable option for redesigning future health care systems, thus increasing population access to services that can provide a rapid and accurate diagnosis and so, improving the quality of patient care.
This article reviews and summarizes current literature regarding the value of TUS, highlighting successes and barriers of tele-ultrasound in clinical practice.
Historical Insight
TUS is a technique which allows interpretation of ultrasound images obtained by health-care providers or untrained care providers located at a distance from a qualified center, and thus providing diagnostic imaging services to patients from remote areas. The initial efforts in the field of TUS technology were made by National and Aeronautics and Space Administration (NASA) and allowed astronauts to conduct real-time ultrasound examination with guidance from terrestrial specialists, such as musculoskeletal ultrasound, ocular examination for trauma and even FAST (focused assessment with sonography for trauma), in the absence of any other diagnostic imaging resource [3, 4, 5, 6].
World Health Organization (WHO) is rating ultrasonography as one of the most important technologies in developing countries and considers access to an ultrasound scan as a minimum global standard [7, 8]. Starting from this statement, the use of TUS by appropriately trained professionals within the ambulatory care setting has the potential to provide better care at the bedside [9], to diagnose and manage both acute and chronic illnesses and injuries [10].
Some of the first projects using clinical TUS have been developed in the field of obstetrics (fetal scans) and cardiology (echocardiograms), and even though the transmission bandwidth and signal were limited, interest and research have evolved incrementally over the past decade [11]. Past research has shown the clinical and patient advantages of portable sonography in remote areas but there has been limited research using randomized controlled trials to compare certain advantages of remote ultrasonography over a previous standard sonography. Also, a few studies have been published concerning training of care providers from remote or isolated areas.
Data Transmission
Research in TUS is mostly divided into two categories of data transmission: asynchronous (store-and-forward) and synchronous (real-time) [Fig. 1]. Currently, the asynchronous method is the most widespread method, especially in the countries where ultrasound examinations are performed by technicians. It consists of collecting and storing images or videos data by the local health care provider and forward them to a specialist for interpretation. The need of TUS in rural sites was assessed using profile questionnaires, concluding there was a strong preference for the store-and-forward transmission of static images compared to real-time or transmission of video clips [12]. Another study indicated that store-and-forward TUS compared to the usual conventional referral system, reduces time to diagnose and increases the continuity of care in a rural setting [13]. Although older studies feared that this model has some technical limitations regarding lack of motion data, lack of color data, scan artefacts and increased scan-to-diagnosis time [14], it was mostly surpassed by technical progresses and the ubiquitous presence of GSM based mobile telephony and data connections.
Figure 1.
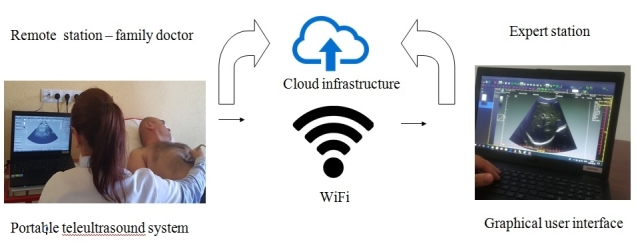
Proposed model for a national telemedicine (teleultrasonography) network with integrated software and hardware, consisting in stocking images and videos data in a database using Cloud infrastructure ("The National Research-Development-Innovation Network In Hybrid Imaging and Advanced Telemedicine in Gastro Enterology and Cardiology")
In the synchronous mode, the data is acquired and transmitted in real-time to a remote expert, whilst the examination is performed. At the remote site, the sonographic examination can be performed by an operator with limited experience or after a brief training or with vocal guidance from the expert. As ultrasound is an operator-dependent examination, the quality of the data and a final correct diagnosis depends on how the operator handles and sites the probe. Based on personal data, researchers stated that in small medical centers, untrained operators could not capture appropriate ultrasound views, even with real-time vocal guidance [15].
On the other hand, another study tested the feasibility of real-time transmission of sonographic images from a remote location and showed that synchronous TUS guided with voice commands can overcome the lack of trained operators in remote or underdeveloped regions [16]. However, these kind of systems need good communication facilities, as well as expensive and complex technology with sophisticated equipment and might not be a valid option for underdeveloped countries [15]. Recently, cheaper and robust systems showed up on the market which opened opportunities for broader usage of TUS, according to WHO principles which support universal coverage for ultrasound technologies, even in underdeveloped countries that lack adequate and expensive imaging facilities [8].
Training and Protocols
The first question to have in mind when we think about TUS operated by a non-experienced operator is: can we obtain adequate sonographic data with appropriate training and strict but simple protocols?
The ideal context to perform TUS would be to have certified sonographers in medical centers where the appropriate technology is accessible but these trained professionals are unavailable.
Nevertheless, this situation is usually not possible, especially in remote settings and the need of training for non-experienced personnel becomes an option.
Consequently, for the asynchronous mode (store-and-forward), training should aim to make the local provider familiar with basic ultrasound principles and techniques, following a standard protocol.
For the synchronous (real-time) mode, short training and vocal guidance following the same standard protocol could greatly help to provide experts with accurate and correct sonographic images.
As pioneers in the field of TUS, astronauts from the International Space Station received a short didactic and hands on ultrasound training 4 months before the mission, without any specific training in shoulder anatomy or shoulder ultrasound techniques.
On the station, with the basic terminology and having the remote experienced physician guidance for approximately 15 minutes, the crew members were able to collect ultrasound images that could be used to exclude subtle shoulder injury, concluding that it could be a useful approach for complex medical tasks [3].
On the other hand, a large study reviewed 1,510 consecutive ultrasound examinations to asses concordance of findings by technologists (sonographers) and physicians.
Even though the overall concordance was good (74%), concordance rates for a major or a minor new diagnoses were low (36% and 32%, respectively) but improved with increasing years of experience of the technologist [17].
They concluded that in order to have an accurate and complete examination report, the physician should take part in the overall conduct of the ultrasound examination, thus indicating the need of training for the sonographers.
The main pitfalls identified by the authors were related to 1) misinterpretation of a finding by the technologist, 2) non-visualization of a finding discovered by the physician performing a repeated scan, 3) technologists had a low correlation between the clinical context and ultrasound findings [17].
These errors could be a result of the lack of experience or the lack of trained examiners, which could represent a major limitation in isolated and remote places with reduced medical facilities.
In order to improve the process of acquiring good quality images, to perform a complete examination and to have an accurate diagnosis, computer assistance, with expert visual guidance (EVG) by a remote expert was proposed.
EVG system permits the examiner to monitor how the image plane is moving over an anatomical site as the probe moves over the patient’s body [18].
The examiners received a 10 minutes training held by an experienced sonographer and they examined the aorta, the kidney and specific anatomy using a standard protocol.
The result of this study indicated that EVG had a significant benefit compared to verbal instructions alone for the inexperienced examiner in acquiring images of the abdominal aorta and specified anatomy but with a smaller benefit for the kidney [18].
Currently, TUS does not have standard training protocols, with less than 5% of the literature evaluating the training of the operator but without a systematic quantification of their improvement after receiving education sessions [19].
The feasibility of telemedicine to deliver training and supervision to general practitioners performing ultrasound in patients with lower urinary tract symptoms has been also tested.
The authors concluded that the remote examiners benefited from a regular ultrasound training, achieving a satisfactory level of competence in scanning the urinary tract [20].
Another study reported that education and hands-on training should be delivered for at least one month in order to perform ultrasound examinations with sufficient technical competence [21].
Along didactic training, a minimum number of scans should be required from professionals before beginning the actual work.
Thus, it has been previously reported that the trainees that performed over 150 scans had a better probability to complete high-quality sonograms [22].
Clinical Applications
From the first applications in space, telemedicine and particularly TUS has been tested in various fields, from emergency medicine in pre-hospital settings using FAST protocol, obstetrics for remote diagnostic consultations and prenatal screening for infectious disease, transabdominal non-obstetrics or musculoskeletal ultrasound.
Despite the fact that there is limited research on the influence of portable ultrasound in remote areas, a few studies have indicated its potential in providing a significant benefit that can alter management and treatment.
A study in the Amazon jungle researched the implication of ultrasound in the differential diagnosis of local tribal people.
Making a comparison between the clinical data pre-and post-ultrasound examination (transabdominal and transvaginal), the doctors concluded that some patients needed a completely different management, with a minority of patients that needed rapid referral for surgical evaluation, indicating clearly the role of ultrasound to dramatically alter diagnosis and treatment [23].
Most of the research in the field focused on the use of remote ultrasound in obstetrics and gynecology.
Ultrasound is a safe, cheap and a harmless method for confirmation, monitoring and evaluation of pregnancy and pregnancy-related complications.
Pregnant patients with limited access to tertiary care or living in isolated places could greatly benefit from telemedicine programs by setting a tele-ultrasound link to a tertiary care prenatal ultrasonography center.
Such a tele-ultrasound platform was implemented in Australia in 2013, evaluating 90 emergency ultrasound examinations performed by a trainee and transmitted to an experimented sonologist.
More than half of the patients received additional information from the senior sonologist, while the management of more than a quarter of cases was changed.
They proved not only that the costs of medical equipment and telecommunication networks were low, but they also provided images with a satisfactory quality for diagnosis [24].
In the pre-hospital setting, ultrasound could change the course of immediate management of life threatening injuries but could also help the triage of the patients. In this way, an emergency medical technician can provide to an emergency physician real-time ultrasound images and medical information using internet connectivity, thus enhancing pre-diagnosis options as well as damage and disaster control abilities in critical moments.
One study assessed paramedics with no prior experience in ultrasound examinations, which performed a FAST examination after receiving a 20-minute lecture and having guidance from an emergency physician [25].
The paramedics were able to successfully complete all the FAST views in less than 5 minutes, thus indicating potential life-saving role that ultrasound can play in austere environments, remote, and rural settings.
For musculoskeletal injuries, as well as soft tissue injuries, ultrasound is also a rapid and ideal imaging diagnostic modality to use in remote areas.
Being used in space by astronauts that received a short training before the mission, ultrasound was able to exclude subtle shoulder injury [3].
Its application in terrestrial environments has also been tested, some studies proving its worth.
Using a portable ultrasound system and internet connection, inexperienced subjects from a rural area at the Arctic Circle could provide diagnostic quality musculoskeletal images, guided by experts from a remote center [26].
Implementation Barriers
Around 20-30 years ago, communication and internet connections were issues in telemedicine projects, but the availability and speed of telecommunications has improved significantly nowadays, allowing to expand research and interest in the field of TUS.
Nevertheless, in underdeveloped countries or a given area with modest infrastructure for telecommunications still represents a technical limitation.
In addition, the systems for real-time telesonography and data transmission, as well as software platforms for videoconferencing and other sophisticated equipment are still not available or have high costs in many developing countries.
Consequently, it has been demonstrated that good quality ultrasound images can be obtained, with satisfactory results in performing real-time TUS using a low-cost platform [15,24].
Another matter to take into consideration when setting up a TUS platform is the quality of the content transmitted to the tertiary center.
The reception and analysis of the images, in store-and-forward or real-time modes, can be influenced by many factors like transmission bandwidth, image compression, spatial resolution, contrast and other characteristic of the displaying device [27].
But streaming multimedia is evolving and further upcoming technologies will ease and improve TUS progress.
Some barriers that are still looking for a solution are related to training and protocols, errors in data acquisition, as well as lack of trained professionals to operate in remote areas. Insufficient training of the examiner coupled with the fears related to the complexity of use, the fact that training protocols are not well established or standardized can lead to an inappropriate and improper scanning technique as well as inadequate image collection.
Furthermore, the static images obtained by the examiner in the store-and-forward mode can lead to false diagnosis or non-diagnosis.
Concerning the limits generated from the examined patients, they could be concerned by security and confidentiality of the electronically transmitted data [28].
Conclusions
In spite of the numerous challenges, TUS has the potential to change the future in providing healthcare remotely as well as education and training of healthcare providers.
Even though the literature is scarce, more research should focus on the role of training and standardized protocols using remote mentoring or comprehensive teaching.
Future communication technologies, advances made with ultrasound machines (portable, hand-held devices) and the low-cost TUS platforms will certainly transform sonography in a diagnostic imaging tool for any healthcare provider, and thus improving worldwide healthcare delivery, no matter the setting.
Acknowledgment
„This work was supported by a grant of Ministery of Reserch and Innovation-project number ID P_34_498, within MFE 2014-2020-POC”
References
- 1.Filly RA. Ultrasound: the stethoscope of the future. Alas. Radiology. 1988;167(2):400–400. doi: 10.1148/radiology.167.2.3282260. [DOI] [PubMed] [Google Scholar]
- 2.Nelson BP, Sanghvi A. Out of hospital point of care ultrasound: current use models and future directions. European Journal of Trauma and Emergency Surgery. 2016;2(2):139–150. doi: 10.1007/s00068-015-0494-z. [DOI] [PubMed] [Google Scholar]
- 3.Fincke EM, Padalka G, Lee D, Van Holsbeeck, Sargsyan AE, Hamilton DR, Martin D, Melton SL, McFarlin K, Dulchavsky SA. Evaluation of shoulder integrity in space: first report of musculoskeletal US on the International Space Station. Radiology. 2015;234(2):319–322. doi: 10.1148/radiol.2342041680. [DOI] [PubMed] [Google Scholar]
- 4.Chiao L, Sharipov S, Sargsyan AE, Melton SL, Hamilton DR, McFarlin K, Dulchavsky SA. Ocular examination for trauma; clinical ultrasound aboard the International Space Station. Journal of Trauma. 2005;58(5):885–889. doi: 10.1097/01.ta.0000162456.37962.01. [DOI] [PubMed] [Google Scholar]
- 5.Sargsyan AE, Hamilton DR, Jones JA, Melton SL, Whitson PA, Kirkpatrick AW, Martin D, Dulchavsky SA. FAST at MACH 20: clinical ultrasound aboard the International Space Station. Journal of Trauma. 2015;58(1):35–39. doi: 10.1097/01.ta.0000145083.47032.78. [DOI] [PubMed] [Google Scholar]
- 6.Jones JA, Sargsyan AE, Barr YR, Melton S, Hamilton DR, Dulchavsky SA, Whitson PA. Diagnostic ultrasound at MACH 20: retroperitoneal and pelvic imaging in space. Ultrasound in Medicine and Biology. 2009;35(7):1059–1067. doi: 10.1016/j.ultrasmedbio.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 7.WHO World Health Organization, 2010, The Partnership for Maternal Newborn, and Child Health, From pledges to action, New Delhi, India 13-14 November. Available from: http://www.who.int/pmnch/events/2010/partnersforum_finalreport.pdf.
- 8.WHO World Health Organization, 1990, Effective Choices for Diagnostic Imaging in Clinical Practice, Report of a WHO Scientific Group, World Health Organization, Geneva, Swtizerland, 1990. Available from: http://apps.who.int/iris/bitstream/handle/10665/37646/9241561491_eng_part1.pdf?sequence=2. [PubMed]
- 9.Kirkpatrick AW. Clinician-performed focused sonography for the resuscitation of trauma. Critical Care Medicine. 2007;35(5):S162–S172. doi: 10.1097/01.CCM.0000260627.97284.5D. [DOI] [PubMed] [Google Scholar]
- 10.Pian L, Gillman LM, McBeth PB, Xiao Z, Ball CG, Blaivas M, Hamilton DR, Kirkpatrick AW. Potential use of remote telesonography as a transformational technology in underresourced and/or remote settings. Emergency Medicine International. 2013;2013:986160–986160. doi: 10.1155/2013/986160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuentes A. Remote interpretation of ultrasound images. Clin Obstet Gynecol. 2003;46:878–881. doi: 10.1097/00003081-200312000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Lewis C. A tele-ultrasound need analysis in Queensland. J telemed Telecare. 2006;11(2):S61–4. doi: 10.1258/135763305775124696. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland JE, Sutphin HD, Rawlins F, Redican K, Burton J. A comparison of telesonography with standard ultrasound care in a rural Dominican clinic. J Telemed Telecare. 2009;15(4):191–195. doi: 10.1258/jtt.2009.080909. [DOI] [PubMed] [Google Scholar]
- 14.Macedonia C, Littlefield R, Coleman J, Satava R, Cramer T, Mogel G, Eglintin G. Three-dimensional ultrasonographic telepresence. J Telemed Telecare. 1998;4(4):224–230. doi: 10.1258/1357633981932280. [DOI] [PubMed] [Google Scholar]
- 15.Adambounou K, Farin F, Boucher A, Adjenou KV, Gbeassor M, N’dakena K, Vincent N, Arbeille P. System of telesonography with synchronous teleconsultations and asynchronus telediagnosis. Med Sante Trop. 2012;22(1):54–60. doi: 10.1684/mst.2012.0002. [DOI] [PubMed] [Google Scholar]
- 16.Popov V, Popov D, Kacar I, Harris RD. The feasibility of realtime transmission of sonographic images from a remote location over low bandwith Internet links: a pilot study. AJR Am J Roentgenol. 2007;188(3):219–222. doi: 10.2214/AJR.05.2148. [DOI] [PubMed] [Google Scholar]
- 17.Chan V, Hanbidge A, Wilson S, Pron G, Moore L. Case for active physician involvement in US practice. Radiology. 1996;199(2):555–560. doi: 10.1148/radiology.199.2.8668811. [DOI] [PubMed] [Google Scholar]
- 18.Sheehan FH, Ricci MA, Murtagh C, Clark H, Bolson EL. Expert visual guidance of ultrasound for telemedicine. Journal of telemedicine and telecare. 2010;16(2):77–82. doi: 10.1258/jtt.2009.090313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferreira AC, O’Mahony E, Oliani AH, Araujo Júnior, Costa FD. Teleultrasound: Historical Perspective and Clinical Application. International Journal of Telemedicine and Applications. 2015;2015:1–11. doi: 10.1155/2015/306259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hussain P, Deshpande A, Shridhar P, Saini G, Kay D. The feasibility of telemedicine for the training and supervision of general practitioners performing ultrasound examinations of patients with urinary tract symptoms. Journal of Telemedicine and Telecare. 2004;10(3):180–182. doi: 10.1258/135763304323070850. [DOI] [PubMed] [Google Scholar]
- 21.Cavina E, Goletti O, Lippolis PV, Zocco G. Telesonography: Technical problems, solutions and results in the routine utilization from remote areas. Studies Health Technol Informatics. 2001;81:88–89. [PubMed] [Google Scholar]
- 22.Costantino TG, Satz WA, Stahmer SA, Dean AJ. Predictors of Success in Emergency Medicine Ultrasound Education. Academic Emergency Medicine. 2003;10(2):180–183. doi: 10.1111/j.1553-2712.2003.tb00038.x. [DOI] [PubMed] [Google Scholar]
- 23.Blaivas M, Kuhn W, Reynolds B, Brannam L. Change in differential diagnosis and patient management with the use of portable ultrasound in a remote setting. Wilderness Environ Med. 2005;16(1):38–41. doi: 10.1580/1080-6032(2005)16[38:ciddap]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira AC, Ferlim R, Oliani DV, Oliani AH, Jordao JF, Meagher S, Finn M, Costa FD. Tele-ultrasound in obstetrics and gynecology: implementation, image quality analysis and clinical application of a low-cost and easy-to-use platform. Ultrasound ObstetGynecol. 2013;42(1):48–112. [Google Scholar]
- 25.O`Connell K, Bouffard AJ, Vollman A, Mercado-Young R, Sargsyan AE, Rubinfeld I, Dulchavsky SA. Extreme musculo-skeletal ultrasound: training of non-physicians in the Arctic Circle. Crit Ultrasound J. 2011;3(1):19–24. [Google Scholar]
- 26.Boniface KS, Shokoohi H, Smith ER, Scantlebury K. Tele-ultrasound and paramedics: real-time remote physician guidance of the focused assessment with sonography for trauma examination. Am J Emerg Med. 2011;29(5):477–481. doi: 10.1016/j.ajem.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 27.Bassignani M, Dwyer SJ, Ciambotti JM, Olazagasti JM, Moran R, Moynihan S, Weaver AC, Snyder AM. Review of Technology: Planning for the Development of Telesonography. Journal of Digital Imaging. 2004;17(1):18–27. doi: 10.1007/s10278-003-1721-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson JG. Social, ethical and legal barriers to e-health. Int J Med Inform. 2007;76(5-6):480–483. doi: 10.1016/j.ijmedinf.2006.09.016. [DOI] [PubMed] [Google Scholar]


