Abstract
Background
Oral health related quality of life (OHRQoL) research among children and adolescents in Lithuania is just starting and no measures have been validated to date. Therefore, this study aimed to validate a Lithuanian version of the full (37 items) Child Perceptions Questionnaire (CPQ11–14) within a random sample of children aged 11 to 14.
Methods
A cross-sectional survey among a randomly selected sample of schoolchildren (N = 307) aged 11 to14 was conducted. An anonymous questionnaire included the full CPQ11–14 and items on global life satisfaction, oral health and oral life quality self-rating. The questionnaire was translated into Lithuanian using translation guidelines. In addition, an item on the oral pain was modified identifying the pain location. Standard tests (Cronbach’s α, construct validity and discriminant validity), supplemented with both exploratory and confirmatory factor analyses, were employed for psychometric evaluation of the instrument. The questionnaire was also tested by comparison students’ and their parents’ (N = 255) responses about oral symptoms and functional limitations.
Results
The modified Lithuanian version of CPQ11–14 revealed good internal consistency reliability (Cronbach’s alpha for the total scale was 0.88). The measure showed significant associations with perceived oral health status and oral well-being, as well as with global life satisfaction (p < 0.01). Discriminant validity of the instrument was approved by comparison of children’s groups defined by self-reported caries experience and malocclusion. Factor analysis revealed a complex structure with two or three factors in each of four domains of the CPQ11–14. Excellent or acceptable levels of indices of model fitting with the given data were obtained for oral symptoms, functional limitations and emotional well-being domains, but not for the social well-being domain. A significant association between child and parental responses was found (intraclass correlation coefficient was 0.56 and 0.43, correspondingly in domains of oral symptoms and functional limitations).
Conclusion
The Lithuanian version of the CPQ11–14 (with a modified item that identifies location of oral pain) appears to be a valid instrument to be used in further studies for measuring OHRQoL among 11 to 14 year old children in Lithuania.
Electronic supplementary material
The online version of this article (10.1186/s12903-018-0701-5) contains supplementary material, which is available to authorized users.
Keywords: Oral health, Quality of life, Child perceptions questionnaire, Psychometric analysis, Factorial validity, Children, Lithuania
Background
The last decades have seen an increasing importance in the literature of a concept that has come to be called oral health related quality of life (OHRQoL), which is applied in adult [1] as well as children and adolescents [2, 3] populations. Although there is no consensus on the definition of OHRQoL in children and adolescents, nor what aspects should be measured, it is generally accepted that OHRQoL is a multidimensional construct [4, 5]. It encompasses factors with four broad dimensions: the existence of discomfort or pain; functional factors; psychological factors; and social factors. Exhaustive systematic reviews [6, 7] have identified several validated instruments that currently exist to measure children’s OHRQoL: Child-Oral Impacts of Daily Performances index [8], Child Oral Health Impact Profile [9], Pediatric Oral Health-Related Quality of Life [10], and Child Perceptions Questionnaire (CPQ) [11].
The CPQ was, nevertheless, the first and most widely used inventory designed to assess the impact of oral conditions on quality of life in children [6, 7]. It was developed in 2002 by Jokovic et al. [11] as the CPQ11–14 for children aged 11 to 14 and was originally validated in children with caries, malocclusion and craniofacial anomalies. In terms of cognitive development, age specific versions of this tool have been produced [12], but the majority of studies used the original version CPQ11–14. The CPQ also has an analogous Parental Child Perceptions Questionnaire, which can be used as a proxy to CPQ [13]. The original item pool of the CPQ consists of 37 items, but the authors have also determined the psychometric properties of its shortened forms [14]. All variations of the questionnaire evaluate the impact of oral and orofacial conditions in children at symptomatic, functional, emotional and social levels. To date, the CPQ has been translated, validated and adapted to suit a number of languages and socio-cultural contexts demonstrating its applicability and perfect psychometric properties on numerous clinical and epidemiological occasions [6, 15–24].
Several methods have been employed in cross-cultural validations of the CPQ, however, the majority of such types of studies were realised without having carried out a validation process with factorial analysis. Factorial technique that includes exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) is commonly used to inform the structure of the instrument (e.g. quality of life (QoL) measures) [25–27]. Such techniques have been employed in CPQ validation studies among Hong Kong adolescents [28, 29]. Findings from these studies indicated that the model using all 37 items fitted the data below the acceptable level. Thus, in order to validate and adapt the CPQ for any culture, it is rationale to analyse its dimensional structure.
OHRQoL research among children and adolescents in Lithuania is just starting and no measures have been validated to date. Given the positive CPQ properties and its high applicability for both clinical assessments and large-scale population studies, we have chosen this instrument for measure of OHRQoL in our research. It has also been considered that the original long form (37 items) of this instrument is more sensitive to changes in oral conditions rather than its short forms [14], hence, the original questionnaire was taken in focus. Each time a measurement scale is used in a new context or with a different population group, it is necessary to test its psychometric properties [30]. However, despite widespread use of the CPQ in many languages and cultures, it has never been adapted for use as a research tool in Lithuania. Therefore, the aim of this study was to validate a Lithuanian version of the full (37 items) CPQ11–14 within a random sample of children aged 11 to 14. The specific objectives were: 1) to translate the original CPQ11–14 into Lithuanian and to make modifications if needed; 2) to explore psychometric properties of the Lithuanian instrument version, and 3) to analyse its factorial structure.
Methods
Participants and data collection
The study followed a cross-sectional design and targeted adolescents aged 11 to 14 years. A number of 323 respondents was calculated to be sufficient for assessment of the prevalence of orthodontic anomalies in children, hypothesizing their prevalence to be 30% with 95% confidence interval from 25 to 35% [31]. The hypothesized prevalence of orthodontic anomalies was in agreement with our study in Lithuania among schoolchildren aged 11–15 years [32]. With regard to factorial analysis, this number of respondents is also sufficient, as the sample size should be at least 5 × k, where k is the number of items in factorial analysis (in our study k = 37) [33]. Then, accounting for anticipated non-response and participants who do not meet age requirements (11 to 14 years), the primarily sample size was increased in 50% (480 persons). The study sample was comprised of students from general education governmental schools in Lithuania. A list of schools and number of students by class was obtained from the education management information system of the Lithuanian Centre of Information Technologies in Education.
A two-stage cluster sampling method was used to draw a representative sample of students. In the first stage, 16 schools were randomly selected, ensuring equal presentation of urban and rural administrative regions. In the second stage, classes of students attending grades six to nine were chosen with a probability proportionate to the number of students in school. Thus, the primary sampling unit (cluster) was a class. In total, 25 classes were selected with estimated a required total number of students. Although the primary sampling unit was the class, a clustered sampling design effect was not accounted for either in the sample size calculation, nor in the analyses of data, as it was considered that students within the same class were similar to each other in oral health behavior, though they may not be as similar as in other health behavior patterns (e.g. smoking or bullying [34]).
School authorities were contacted by researchers and informed about all aspects of the study. Class tutors of selected classes were instructed about the process of carrying out the survey among students and their parents. They sent a description of the study, asking for written informed consent that their child be allowed to participate in the study to students’ parents. Of the 463 parents who initially received a request for written informed consent, positive answers were obtained from 393 (85%) of them. Those parents who gave consent were also asked to complete a questionnaire about their child’s oral health and well-being. The number of correctly completed parents’ questionnaires was 315 (68% of parents who were initially contacted). The students’ questionnaires were administrated in school classrooms. Eligible participants could freely choose to participate or not in the survey. Measures of anonymity and confidentiality were ensured. Respondents did not write their name in questionnaires, and upon completing the questions, they sealed the questionnaires in provided envelopes. A total of 381 students correctly completed the questionnaires, but 74 were excluded from the present analysis because of the students’ age criterion.
The final number of students, aged 11 to 14 years, whose questionnaires were used in the present study, was 307 (66% of initial sample size). Maintaining the same fieldwork methods, the data were collected during the 2013/2014 school year (n = 179) and in 2016/2017 school year (n = 128). The number of questionnaires completed both by the child and parents was 255. The gathering of questionnaires was ensured by using codes.
Measures
CPQ instrument
The originally proposed CPQ11–14, adopted for children aged 11 to 14 years is a 37-item instrument consisting of four hypothesized health domains (subscales): (1) oral symptoms (OS, 6 items), (2) functional limitations (FL, 9 items), (3) emotional well-being (EWB, 9 items), and (4) social well-being (SWB, 13 items) [11]. The respondents were asked to indicate the frequency of a specified event in the past three months. Each question was asked to the respondents in the same way, “In the past three months, how often have you …(had/been + specified item) … because of your teeth/mouth?”. Answer options were: (0) ‘never’; (1) ‘once or twice’; (2) ‘sometimes’; (3) ‘often’; (4) ‘every or almost everyday’. The list of all of 37 CPQ items by health domains can be seen in Table 1.
Table 1.
CPQ full questionnaire with 37 items and assessments of their impact on the domain reliability (N = 307)
| Domain | Item code | Specified eventa | Corrected item-total correlationb | Cronbach’s alpha if item deleted | Loadings in 1-factor solution |
|---|---|---|---|---|---|
| OS | O1 | Pain in teeth, lips, jaws or mouth | 0.316 | 0.626 | 0.497 |
| O2 | Bleeding gums | 0.311 | 0.634 | 0.493 | |
| O3 | Mouth sores | 0.223 | 0.647 | 0.402 | |
| O4 | Bad breath | 0.421 | 0.584 | 0.679 | |
| O5 | Food caught in or between teeth | 0.546 | 0.525 | 0.784 | |
| O6 | Food stuck to roof of mouth | 0.530 | 0.576 | 0.761 | |
| FL | F1 | Breathing trough mouth | 0.465 | 0.658 | 0.600 |
| F2 | Taken longer than others to eat a meal | 0.307 | 0.695 | 0.449 | |
| F3 | Trouble sleeping | 0.425 | 0.665 | 0.553 | |
| F4 | Difficulty to bite or chew food like apples, corn on the cob or steak | 0.382 | 0.674 | 0.538 | |
| F5 | Difficulty to open mouth wide | 0.450 | 0.667 | 0.672 | |
| F6 | Difficulty to say any words | 0.337 | 0.687 | 0.462 | |
| F7 | Difficulty to eat foods you would like to eat | 0.467 | 0.657 | 0.660 | |
| F8 | Difficulty to drink with a straw | 0.346 | 0.685 | 0.561 | |
| F9 | Difficulty to drink or eat hot or cold foods | 0.300 | 0.689 | 0.468 | |
| EWB | E1 | Irritable or frustrated | 0.320 | 0.755 | 0.247 |
| E2 | Unsure of himself | 0.174 | 0.758 | 0.165 | |
| E3 | Shy or embarrassed | 0.541 | 0.732 | 0.568 | |
| E4 | Concerned what other people think about you | 0.666 | 0.711 | 0.868 | |
| E5 | Worried that is less attractive than other people | 0.647 | 0.703 | 0.866 | |
| E6 | Upset | 0.608 | 0.712 | 0.816 | |
| E7 | Nervous or afraid | 0.376 | 0.746 | 0.342 | |
| E8 | Worried that is less healthy than other people | 0.644 | 0.708 | 0.848 | |
| E9 | Worried that is different than other people | 0.575 | 0.716 | 0.808 | |
| SWB | S1 | Missed school | 0.626 | 0.847 | 0.724 |
| S2 | Hard time paying attention in school | 0.601 | 0.848 | 0.668 | |
| S3 | Difficulty doing homework | 0.543 | 0.852 | 0.607 | |
| S4 | Avoiding to speak or read out loud in class | 0.562 | 0.851 | 0.657 | |
| S5 | Avoiding activities like sports, clubs, drama, music, school trips | 0.605 | 0.849 | 0.700 | |
| S6 | Avoiding to talk to other children | 0.625 | 0.847 | 0.718 | |
| S7 | Avoiding smiling or laughing when around other children | 0.464 | 0.864 | 0.552 | |
| S8 | Difficulty playing a musical instrument such as a recorder, flute, clarinet, trumpet | 0.402 | 0.860 | 0.464 | |
| S9 | Avoiding to spend time with other children | 0.628 | 0.847 | 0.727 | |
| S10 | Argued with other children or family | 0.546 | 0.852 | 0.633 | |
| S11 | Teased or called names by other children | 0.336 | 0.863 | 0.406 | |
| S12 | Left out by other children | 0.556 | 0.853 | 0.649 | |
| S13 | Asked questions by other children | 0.574 | 0.850 | 0.642 |
OS oral symptoms, FL functional limitations, EWB emotional well-being, SWB social well-being
aFull wording of questions was “In the past 3 months, how often have you …(had/been + specified event) … because of your teeth/mouth?” and answer options were: (0) ‘never’; (1) ‘once/twice’; (2) ‘sometimes’; (3) ‘often’; (4) ‘every/almost every day’. b p < 0.001 for all values
The Lithuanian version the CPQ instrument conformed to concepts of the original version and was elaborated on using translation procedures (see below). Nevertheless, the content of the original item on the pain in teeth, lips, jaws or mouth (item O1) was discussed due to its complexity and wide scope of meaning. It was decided upon to change this item with five sub-items specifying a location of the pain (in teeth, lips, gums, oral mucosa and jaws or joints). A response option with the highest score that occurred throughout all these sub-items was considered as a response to the original item.
Rating of oral health and oral well-being
In order to validate the CPQ instrument, which was carried out in its developers’ study [11], the respondents were asked to rate their oral health and the extent to which it affected their well-being. For each of these dimensions, five sub-items were worded in the following way: a) “How you would describe health status of the following oral parts: - teeth; - lips; - gum; - oral mucosa; - jaws or joints?” and b) “Over the last three months, how much has your overall life been affected by the conditions of the following oral parts: - teeth; - lips; - gum; - oral mucosa; - jaws or joints?” The responses were scored in the following way: with regard to oral health rating: (0) ‘excellent’; (1) ‘very good’; (2) ‘good’; (3) ‘fair’, and (4) ‘poor’; with regard to well-being: (0) ‘not at all’; (1) ‘very little’; (2) ‘somewhat’ (3) ‘a lot’; and (4) ‘very much’. The sum score of all sub-items for each dimension ran from 0 to 20.
Global life satisfaction
The global life satisfaction measure was used as an additional tool in assessing construct validity of the CPQ. Children’s global life satisfaction was rated using the measurement technique from the HBSC study [34]. Children were asked to take a look at a picture of a ladder that had steps numbered from zero (“0”) at the bottom to ten (“10”) at the top, with an instruction to suppose the top of the ladder represents the best possible life, and the bottom of the ladder represents the worst possible life. They were asked to indicate the step of the ladder at which they would place their lives at present. The response was scored from zero to ten.
Family affluence
Family affluence is an important predictor of quality of life in young people [34], and therefore, it was decided to include it into the present study as a tool in assessing discriminant validity of the CPQ. It was measured by the Family Affluence Scale (FAS), which was specially developed for the HBSC study as a measure of social position [35]. The scale is simple and easy to answer even for children. The present FAS included four questions, including questions regarding car and home computers ownership, own bedroom occupancy and travelling on holidays. A composite FAS score was calculated for each respondent based on his or her responses to these four items, and then a three-point ordinal variable was composed for the present analysis, in which: score = 0–3 indicated low affluence; score = 4–5 indicated middle affluence, and score = 6–7) indicated high affluence.
Self-reported rating of experience with caries and malocclusion
Children were asked to answer: a) whether they have dental caries (tooth decay) or cavities that need to be treated, and b) if they have ever noticed that their teeth grew or were situated in an irregular way, or they have malocclusion. The answer categories for each question were: (1) ‘yes, I just noticed myself’; (2) ‘yes, this was confirmed by dentist’; or (3) ‘no’. In analyzing each question, the first two categories were combined. Thus, two sub-groups of respondents (correspondingly ‘not healthy’ and ‘healthy’) were selected separately for caries experience and malocclusion rating.
Translation into Lithuanian
Forward translation into Lithuanian
The procedure of translation and national adaptation of the questionnaire followed guidelines proposed by Beaton et al. [36]. The principles of good practice proposed by International Society for Pharmacoeconomics and Outcomes Research were also taken into consideration [37]. The initial English version of the CPQ was taken from Shoroog Agou’s dissertation [38] and compared with the versions used in other validation studies [28]. It was first forward translated into Lithuanian by a co-author (AK) of this study, who is very familiar with the concepts included in the CPQ. Her mother-tongue language is Lithuanian and she is fluent in English. During this phase, the main focus was to achieve semantic, idiomatic, conceptual and scientific equivalence between the English and Lithuanian versions while adopting a vocabulary easily comprehensible for children. Then, the translated questionnaire was reviewed by all study co-authors. Ambiguities in translation were discussed with an invited language professional.
Back translation into English
The Lithuanian version of the CPQ was then blindly back-translated into the English language by a professional translator, fluent in English and unfamiliar with the concepts of the CPQ and original English version. The back-translated English questionnaire was compared to the original one, aiming to discern possible discrepancies and to solve any inconsistencies between the two versions. A multidisciplinary committee that comprised all the study co-authors, the back-translator and a school teacher, who had a postgraduate degree in English, discussed the differences between the initial English and Lithuanian versions of the questionnaire. A consolidated Lithuanian version was approved by consensus.
Pre-testing
Prior to the main study, a pilot test was carried out on a sample of students (N = 48) in one school. It was aimed to verify the level of understanding of the wording used and, where appropriate, to make any necessary changes. This so called ‘face validity’ test confirmed the feasibility of the methodology and showed that the young respondents had a high level of understanding of the questionnaire, whilst their suggestions enabled slight changes to be made to the wording, specifically regarding the questions about emotional and social well-being. Pre-testing of the question on pain in teeth, lips, jaws or mouth (item O1) that was modified by specifying a location of the pain demonstrated a high level of its understanding and appropriate distribution of answers by location of the pain. The final Lithuanian version of the CPQ is presented in Additional file 1.
Statistical analysis
Descriptive statistics
The data were computerised and analysed using the SPSS statistical package supplemented with AMOS (version 21; IBM SPSS Inc., Chicago, IL, 2012). Missing responses to the CPQ items were substituted with the student’s mean score in a health domain if more than 2/3 of the domain items were completed; otherwise, the record was excluded from the analysis. The scores for each item were added together to obtain a sum score of each health domain, as well as of the total CPQ. Then, the sum scores were standardized to a percentage scale of 0–100% by dividing their value by the maximum sum score and multiplying by 100. Note that higher sum/percentage scores refer to worse OHRQoL.
The distributions of each item and the sum scores were examined. The sum scores of CPQ and its domains were found not to be normally distributed, thus, they were described using the median and the interquartile range (IQR). The null hypotheses that medians are the same across groups were therefore tested using median test. Upon the same reason, binary associations between variables were evaluated with non-parametric Spearman correlation coefficient. The cut-off level for statistical significance was set at 0.05.
Psychometric properties
A set of tests was used for examining psychometric properties of the CPQ [30, 33, 39]. The Cronbach’s alpha and intraclass correlation coefficient (ICC) average measure (one-way random effects) were used as a measure of internal consistency reliability of the total instrument and its domains. Values of ≥0.70 were considered acceptable [39]. Furthermore, other tests of internal reliability (inter-item and item-total correlations) were also investigated.
Construct validity of the instrument was tested using Spearman correlation coefficient to assess the association between the scores of total scale, as well as its domains and the respondents’ rating of their oral health, oral health related well-being and the global rating of life satisfaction. Discriminant validity was tested by comparing the medians of scores between groups (median test) defined by gender, age, social position, subjective caries experience and malocclusion traits.
A test-retest reliability test of the instrument was not employed; instead, we assessed agreement between children’s and their parents’ answers to the same questions of the OS and FL domains. The association between child and parental sum scores was assessed by Spearman correlation coefficient, and agreement between two groups of raters was evaluated by the ICC using two way mixed consistency method and the quadratic weighted kappa [39]. The quadratic weighted kappa was used due to high range of sum scores.
Exploratory factor analysis
Using the SPSS Principal Component Factor Analysis procedure, an EFA was performed on the set of items of each CPQ health domain. The suitability of the data for such analysis was tested using the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy, along with the Bartlett’s test of sphericity (KMO ≥ 0.5 and p < 0.001 show the adequacy of the data for use in the EFA). Initially, we explored 1-factor solution that ranks the items by their impact to the total variance of the domain. Then, the factors were extracted on the eigenvalues (> 1) with a Promax rotation. This solution helped to understand the interrelations among the items and to confirm the inherent structure of the instrument since factors were correlated. Factor loadings less than 0.4 indicate low item impact on the validity of the instrument [25, 33].
Confirmatory factor analysis
CFA [27, 33, 40, 41] was employed to establish factorial validity of the CPQ domains. The goodness of fit of the explored models was evaluated using multiple fit indices. Relative chi-square (χ2/df) and its p-value, comparative fit index (CFI), Tucker–Lewis index (TLI) and root mean square error of approximation (RMSEA) were taken into account. Relative chi-square is the chi-square ratio to degrees of freedom, and it is suggested that its value less than three or a non-significant p-value corresponds to an acceptable fit, however, the chi-square increases with sample size and model complexity and, therefore, this test was complemented by other tests [33, 42]. The values of CFI and TLI values close to 1 (≥.90) are commonly indicated as acceptable model fits [42]. An RMSEA value between 0.08 and 0.10 indicates an average fit, and a value below 0.08 and below 0.05 shows correspondingly a good and excellent fit [42]. We performed CFA on each of four domains (OS, FL, EWB and SWB). Initial models were based on the above EFA postulating that the domains should have as many latent variables as many common factors were established and that latent variables might be correlated. In order to achieve the optimum combination of simplicity and fit of the final models, the options of Heuristic Specification Search and Modification Indices in AMOS were employed [40].
Results
Sample characteristics
Self-reported data were collected from 307 children aged 11 to 14 years. The mean age of the children was 13.27 years (standard devition (SD) = 1.01), and 128 (41.7%) were boys. The respondents represented all social groups by family affluence levels: 32 (10.7%) of low, 105 (35.1%) of middle and 162 (54.2%) of high (8 missing cases) level; and by residence area: 221 (72.2%) of urban and 86 (27.8%) of rural residence.
Measure modification
In our study, a single item on the pain in teeth, lips, jaws or mouth from the OS domain was substituted by a series of five sub-items identifying a location of oral pain. The distribution of respondents’ answers to these sub-items is presented in Table 2. Responses provided a variety of locations of oral pain, although pain in teeth seemed to be the most frequent complaint. The new item that combined responses to all sub-items showed that 67.3% of respondents have experienced pain in teeth, lips, jaws or mouth at least one or two times in the prior three months. In further analyses, this variable was used as the original item OS1 “Pain in teeth, lips, jaws or mouth”.
Table 2.
Responses of the respondents to items on the oral pain location and distribution of the item that combined the pain in teeth/mount (N = 307)
| Item | Never | One or two times | Sometimes | Often | Everyday or almost everyday | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| O1.1 | Pain in teeth | 156 (50.8) | 111 (36.2) | 37 (12.1) | 2 (0.6) | 1 (0.3) |
| O1.2 | Pain in lips | 243 (79.2) | 43 (14.0) | 13 (4.2) | 6 (2.0) | 2 (0.6) |
| O1.3 | Pain in gum | 243 (79.2) | 54 (17.6) | 8 (2.6) | 1 (0.3) | 1 (0.3) |
| O1.4 | Pain in oral mucosa | 276 (89.9) | 20 (6.5) | 10 (3.3) | 1 (0.3) | 0 |
| O1.5 | Pain in jaws or joints | 266 (86.6) | 35 (11.5) | 5 (1.6) | 0 | 1 (0.3) |
| O1 | Pain in teeth, lips, jaws or mount | 103 (33.6) | 140 (45.6) | 50 (16.3) | 9 (2.9) | 5 (1.6) |
Reliability analysis
The response rate to the items of the CPQ ranged from 97.1 to 100% with the highest rate of blanks (2.9%) in responses to item S10 “Argued with other children or your family because of your teeth or mouth” (SWB domain).
The impacts, that is the items scored from 1 (‘1 or 2 times’) to 4 (‘everyday or almost everyday’), were reported most frequently in the OS domain (“Pain in teeth, lips, jaws or mouth” – 67.3%; “Food stuck in or between teeth” – 59.6%; “Bleeding gums” – 56.8%; “Bad breath” – 47.9%) and in the EWB domain (“Worried that he/she is not as good looking as others” – 42.4%; “Worried that he/she is not as healthy as others” – 32.4%).
Descriptive statistics of the total CPQ and its health domains are presented in Table 3. Sum scores were found to be highly skewed and not normally distributed in all the health domains with a very noticeable floor effect, especially in the SWB domain. Out of the theoretical range of 0–100% of transformed scores, their mean (except OS domain) and median did not exceed 20%.
Table 3.
Summary statistics of the CPQ and its domains (N = 307)
| Domain / total CPQ | Mean | SD | Median | IQR | Skewness |
|---|---|---|---|---|---|
| OS | 20.87 | 16.21 | 16.67 | 16.67 | 1.23 |
| FL | 7.75 | 11.65 | 3.70 | 11.11 | 2.10 |
| EWB | 12.56 | 18.86 | 7.41 | 18.52 | 2.66 |
| SWB | 4.02 | 9.94 | 0 | 2.56 | 4.54 |
| Total CPQ | 9.73 | 10.23 | 6.31 | 10.81 | 1.78 |
SD standard deviation, IQR interquartile range
Assessments of internal consistency reliability of the CPQ and its domains are displayed in Table 4. Cronbach’s alpha for the total CPQ was 0.875. For the domains, the coefficient ranged from 0.645 for OS domain to 0.862 for SWB domain, indicating from an acceptable to good internal consistency reliability. Similar assessments were found for the ICC.
Table 4.
CPQ and its domains internal consistency reliability statistics a (N = 307)
| Domain/total CPQ | Number of items | Cronbach’s alpha | ICC (95% CI) |
|---|---|---|---|
| OS | 6 | 0.645 | 0.568 (0.488–0.639) |
| FL | 9 | 0.701 | 0.691 (0.637–0.741) |
| EWB | 9 | 0.759 | 0.755 (0.712–0.794) |
| SWB | 13 | 0.862 | 0.859 (0.835–0.882) |
| Total CPQ | 37 | 0.875 | 0.860 (0.836–0.881) |
ICC intraclass correlation coefficient, CI confidence interval. a p < 0.001 for all values
All items of the OS and EWB subscales were found to be significantly inter-item correlated, while this was not achieved for the items of FL and SWB subscales (data not shown). The item-total correlations were significant at a 0.01 level for all domains, as well as for the total CPQ (see Table 1). These results, in combination with Cronbach’s alpha if item deleted and a 1-factor solution from the EFA, ranked the items by their impact to the total variance of the domain and indicate which items have the weakest impact within the domain and, consequently, could be removed from the corresponding domain. The items “Sores in mouth” (O3), “Irritable or frustrated” (E1), “Unsure of himself” (E2), “Difficulty playing a musical instrument such as a recorder, flute, clarinet, trumpet” (S8), and “Teased or called names by other children” (S11) are examples of such kind (see Table 1).
Construct validity
Table 5 displays the correlation between scale sum scores and overall ratings of oral health and well-being, as well as with global life satisfaction. All domains and total CPQ were found to be significantly (p < 0.01) and positively correlated with oral health and oral well-being. The correlations between the global life satisfaction and the domains were all significant (a negative correlation value indicates that higher life satisfaction is related to lower rating of oral problems).
Table 5.
Construct validity: Spearman correlation of the total CPQ and its domains with overall ratings of oral health, oral well-being and global life satisfaction (N = 307)
| Domain/total CPQ | Spearman correlationa | ||
|---|---|---|---|
| Oral health | Oral well-being | Global life satisfaction | |
| OS | 0.328 | 0.475 | − 0.259 |
| FL | 0.237 | 0.358 | −0.172 |
| EWB | 0.312 | 0.382 | −0.317 |
| SWB | 0.179 | 0.280 | −0.171 |
| Total CPQ | 0.359 | 0.491 | −0.327 |
aAll correlations are significant at p < 0.01
Discriminant validity
Discriminant validity of the instrument was tested by assessing CPQ scores by gender, family affluence, self-reported caries experience and malocclusion traits (Table 6). A significant gender difference in the EWB domain, as well as in the total CPQ revealed that there was poorer emotional well-being among girls. Across the groups of adolescents by family affluence level, a significant gradient within the family affluence groups was observed overall as well as in EWB and SWB domains. Adolescents who subjectively reported experience with caries in comparison with their ‘healthy’ contemporaries indicated significantly greater scores in the OS, FL and EWB domains but not in the SWB domain. In parallel with this, self-reported malocclusion also indicated a negative impact on the overall OHRQoL, but was significant within the OS and EWB domains only.
Table 6.
Discriminant validity: Median (IQR) of the CPQ and its domains, by gender, family affluence, self-reported rating of caries experience and malocclusion
| n | Domain | Total CPQ | ||||
|---|---|---|---|---|---|---|
| OS | FL | EWB | SWB | |||
| Gender | ||||||
| boys | 128 | 16.67 (16.7) | 3.70 (7.4) | 3.70 (14.8) | 0 (2.6) | 5.41 (9.2) |
| girls | 179 | 16.67 (16.7) | 3.70 (11.1) | 7.40 (18.5) | 0 (5.1) | 6.31 (10.8) |
| pa | 0.993 | 0.386 | 0.007 | 0.084 | 0.016 | |
| Family affluence: | ||||||
| low | 32 | 22.22 (22.2) | 3.70 (21.3) | 14.81 (29.6) | 1.28 (10.3) | 11.26 (16.2) |
| middle | 105 | 22.22 (22.2) | 3.70 (11.1) | 7.41 (18.5) | 0 (5.1) | 7.21 (12.2) |
| high | 162 | 16.67 (22.2) | 3.70 (7.4) | 3.70 (14.8) | 0 (2.6) | 4.51 (9.0) |
| pa | 0.159 | 0.340 | 0.010 | 0.047 | 0.009 | |
| Self-reported rating of caries experience: | ||||||
| 'healthy’ | 207 | 16.7 (16.7) | 3.7 (11.1) | 3.7 (14.8) | 0 (2.6) | 5.4 (10.8) |
| 'not healthy’ | 98 | 22.2 (22.2) | 7.4 (14.8) | 11.1 (25.9) | 0 (5.1) | 8.1 (13.1) |
| pa | < 0.001 | 0.007 | 0.013 | 0.356 | < 0.001 | |
| Self-reported rating of malocclusion: | ||||||
| 'healthy’ | 136 | 16.7 (22.2) | 3.7 (10.2) | 3.7 (11.1) | 0 (2.6) | 5.4 (8.1) |
| 'not healthy’ | 170 | 22.2 (22.2) | 3.7 (14.8) | 9.3 (25.9) | 0 (5.1) | 8.1 (12.6) |
| pa | 0.009 | 0.119 | < 0.001 | 0.076 | < 0.001 | |
aMedian test, underlined values indicate a significant difference between medians in groups
Agreement between child and parental reports
It was possible to compare 255 pairs of OS and FL as a sum score rated by children and their parents (Table 7). Positive significant correlations, which obtained value of a moderate level, were observed for sum scores of both domains. The moderate values of kappa and ICC also confirmed agreement between child and parental reports. These results suggest reliability of two subscales of the CPQ in respect of agreement between two different raters.
Table 7.
Agreement between child and parental reports about oral symptoms (OS) and functional limitations (FL) (N = 255)
| OS | FL | |
|---|---|---|
| Spearman correlation coefficient | 0.419** | 0.305** |
| Quadratic weighted kappa | 0.400*** | 0.326*** |
| Intraclass correlation coefficient (95% CI) | 0.557*** (0.433–0.654) |
0.429*** (0.269–0.553) |
** p < 0.01; *** p < 0.001
Results of the exploratory factor analysis
Table 8 presents the factor structure of each domain of the CPQ obtained from the EFA. The appropriateness of these factor models was evaluated by Bartlett’s test of sphericity (p < 0.001 for all four domains) and KMO measure of sampling adequacy (it ranged from 0.666 in FL domain to 0.862 in EWB domain). The analysis revealed a complex factor structure in all domains of the CPQ. The estimated loadings indicate that the domain of oral symptoms (OS) includes two factors that explained 38.4 and 16.6% of the total variance correspondingly. Factor 1 combined four items (“Bleeding gums” (O2), “Food caught in or between teeth” (O5), “Bad breath” (O4), and “Food stuck to roof of mouth” (O6)), while the factor 2 combined two items (“Mouth sores” (O3), and “Pain in teeth, lips, jaws or mouth” (O1)) (items are listed by loading weights). Analysis of the FL domain showed that at least two factors could be extracted, which explain 31.0 and 16.1% of the total variance correspondingly. Factor 1 combined six items on limitations of the eating function (F5, F8, F7, F9, F4, F2), and factor 2 combined breathing (F1), sleeping (F3) and speaking (F6) disorders. The items of the EWB domain were split explicitly into two factors that explained 45.2 and 20.5% of the total variance correspondingly. Factor 1 combined five items (E4, E5, E9, E8, E6) that describe adolescent emotions, while factor 2 combined the remaining four items (E1, E2, E7,E3) concerned with adolescent personality. Items of the SWB domain showed a three factor structure, explaining 40.2, 14.2 and 8.5% of the total variance by the corresponding factors. Factor 1 combined six items (S10, S7, S12, S9, S13, S6) specifying the adolescent’s isolation from his/her peers; factor 2 combined five items (S2, S3, S8, S1, S4) on adolescent difficulties in school work and out-of-school activity; and factor three combined two items (S11, S5) that measured disorders in adolescent relations with other children due to his/her oral problems.
Table 8.
Factor loadings from the Exploratory Factor Analysis, by the CPQ domainsa (N = 307)
| Domain | Item | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|---|
| OS (KMO = 0.746) | O2 Bleeding gums | 0.721 | −0.343 | |
| O5 Food caught in or between teeth | 0.712 | 0.187 | ||
| O4 Bad breath | 0.705 | 0.013 | ||
| O6 Food stuck to roof of mouth | 0.657 | 0.239 | ||
| O3 Mouth sores | −0.129 | 0.927 | ||
| O1 Pain in teeth, lips, jaws or mouth | 0.290 | 0.474 | ||
| Total variance explained (%) | 38.4 | 16.6 | ||
| FL (KMO = 0.666) | F5 Difficult to open mouth wide | 0.843 | −0.070 | |
| F8 Difficult to drink with a straw | 0.805 | −0.177 | ||
| F7 Difficult to eat foods you would like to eat | 0.601 | 0.198 | ||
| F9 Difficult to drink or eat hot or cold foods | 0.528 | 0.021 | ||
| F4 Difficult to bite or chew food like apples, corn on the cob or steak | 0.400 | 0.267 | ||
| F2 Taken longer than others to eat a meal | 0.291 | 0.273 | ||
| F1 Breathed trough mouth | −0.002 | 0.824 | ||
| F3 Trouble sleeping | −0.046 | 0.812 | ||
| F6 Difficult to say any words | 0.005 | 0.626 | ||
| Total variance explained (%) | 31.0 | 16.1 | ||
| EWB (KMO = 0.862) | E4 Concerned what other people think about you | 0.887 | −0.004 | |
| E5 Worried that is less attractive than other people | 0.884 | −0.002 | ||
| E9 Worried that is different than other people | 0.862 | −0.091 | ||
| E8 Worried that is less healthy then other people | 0.852 | 0.032 | ||
| E6 Upset | 0.838 | −0.015 | ||
| E1 Irritable or frustrated | −0.077 | 0.784 | ||
| E2 Unsure of himself | −0.153 | 0.764 | ||
| E7 Nervous or afraid | 0.047 | 0.720 | ||
| E3 Shy or embarrassed | 0.345 | 0.557 | ||
| Total variance explained (%) | 45.2 | 20.5 | ||
| SWB (KMO = 0.788) | S10 Argued with other children or family | 0.862 | −0.173 | 0.059 |
| S7 Avoiding smiling or laughing when around other children | 0.772 | 0.029 | −0.180 | |
| S12 Left out by other children | 0.754 | −0.075 | 0.103 | |
| S9 Avoiding to spend time with other children | 0.693 | 0.188 | −0.009 | |
| S13 Asked questions by other children | 0.603 | 0.040 | 0.147 | |
| S6 Avoiding to talk to other children | 0.484 | 0.029 | 0.417 | |
| S2 Hard time paying attention in school | 0.000 | 0.863 | −0.016 | |
| S3 Difficulty doing homework | −0.184 | 0.863 | 0.123 | |
| S8 Difficulty playing a musical instrument such as a recorder, flute, clarinet, trumpet | 0.050 | 0.767 | −0.266 | |
| S1 Missed school | 0.375 | 0.667 | −0.172 | |
| S4 Avoiding to speak or read out loud in class | −0.168 | 0.590 | 0.489 | |
| S11 Teased or called names by other children | 0.006 | −0.252 | 0.874 | |
| S5 Avoiding activities like sports, clubs, drama, music, school trips | 0.140 | 0.180 | 0.643 | |
| Total variance explained (%) | 40.2 | 14.2 | 8.5 |
aExtraction Method: Principal Component Analysis on eigenvalue > 1. Rotation Method: Promax with Kaiser Normalization. The underlined terms indicate the main loadings for corresponding factors. KMO: Kaiser-Meyer-Olkin measure
A complex factor structure of the CPQ domains was also seen from noticeable loadings of several items (F2, F4, E3, S4, S6); therefore, they might be attributed to more than one specified factor. Further, the dimensionality of the CPQ domains was assessed employing CFA.
Results of the confirmatory factor analysis
We performed CFA on each of four domains (OS, FL, EWB and SWB). Table 9 reports the goodness-of-fit statistics for the final models of each domain.
Table 9.
Model fit estimations in the Confirmatory Factor Analysis, by the CPQ domains (N = 307)
| Domain | χ2 | df | χ2 / df | p-value | CFI | TLI | RMSEA (90% CI) |
|---|---|---|---|---|---|---|---|
| OS | 12.1 | 8 | 1.511 | 0.147 | 0.977 | 0.956 | 0.041 (0.000–0.085) |
| FL | 67.0 | 22 | 3.048 | < 0.001 | 0.911 | 0.854 | 0.082 (0.060–0.104) |
| EWB | 41.3 | 24 | 1.722 | 0.015 | 0.986 | 0.980 | 0.049 (0.021–0.073) |
| SWB | 347.3 | 57 | 6.093 | < 0.001 | 0.852 | 0.797 | 0.129 (0.116–0.142) |
df degrees of freedom, CFI comparative fit index, TLI Tucker–Lewis index, RMSEA root mean square error of approximation, CI confidence limits
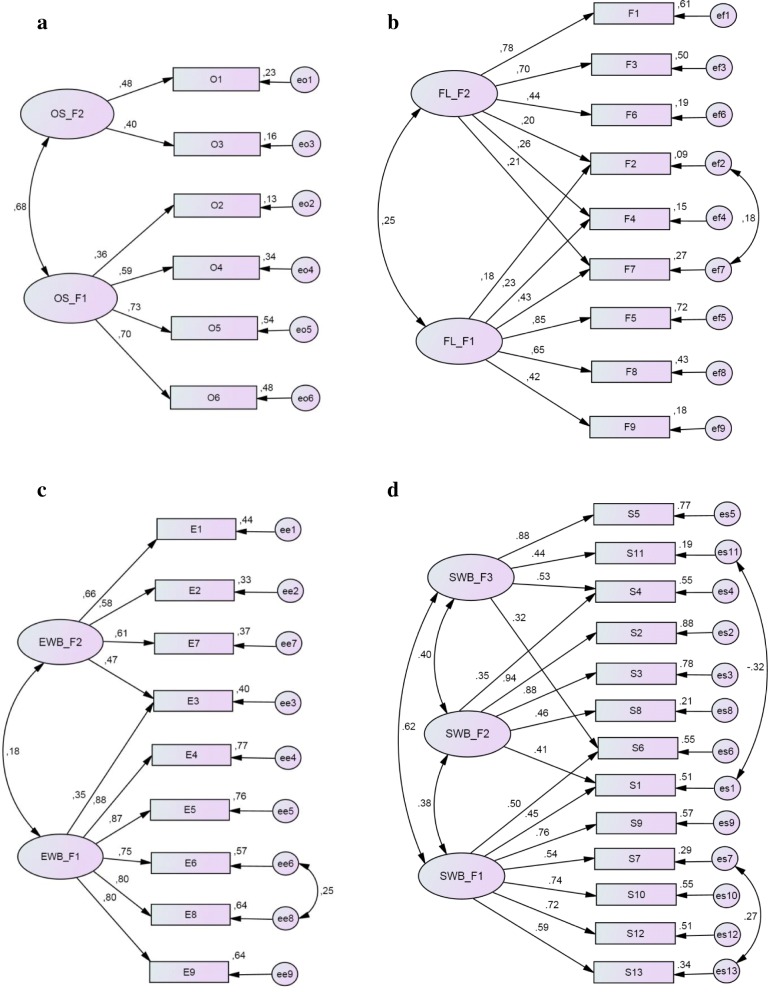
Among four domains, the OS domain model had the best fit estimations, unless its internal consistency reliability (Cronbach’s alpha) was the lowest. Its goodness-of-fit indices showed excellent model fitting to the given data including relatively great p-value, which is not uncommon for such a sample size. As presented in Fig. 1a, the model includes two latent variables (factors). In accordance with the EFA solution, the items “Bleeding gums” (O2), “Food caught in or between teeth” (O5), “Bad breath” (O4) and “Food stuck to roof of mouth” (O6) went to factor one and the items “Pain in teeth, lips, jaws or mouth” (O1) and “Mouth sores” (O3) went to factor two. The item “Pain in teeth, lips, jaws or mouth” (O1) that was modified in our study had a significant positive impact on the factor two. Both factors were significantly correlated (r = 0.68, p < 0.001).
Fig. 1.
Path diagrams with standardized estimations of the final CFA models: a) oral symptoms (OS), b) functional limitations (FL), c) emotional well-being (EWB), d) social well-being (SWB)
The model of the FL domain had acceptable fitting to the concerned data. It was in accordance with the two factors structure that was revealed in the EFA. Results shown in Fig. 1b illustrate a positive association between selected factors (r = 0.25, p < 0.001), unless they reflect different aspects of life quality related to limitations of oral functions. Both EFA and CFA confirmed low effect of the functional limitation “Taken longer than others to eat a meal” (F2).
The model of the EWB domain had excellent fitting indices and confirmed a two factor structure, as well as being revealed in the EFA (Fig. 1c). There was a positive correlation between factors (r = 0.33, p < 0.001). The item “Shy and embarrassed” (E3) provided unspecified position in factorial structure.
The model of the SWB, which included three latent variables, was checked. As a result, this model had a complex structure and was not well-fitted to the research data (Fig. 1d).
Discussion
The CPQ11–14 inventory has long been acknowledged as a valid tool in OHRQoL research worldwide [15–22]. It has also been found to be valid in children with dental caries, malocclusion and craniofacial anomalies [6, 43]. Therefore, the present study aimed to validate a Lithuanian version of the CPQ and explore its psychometric properties in a sample of school children from national schools. Considering this point, our study is innovative in OHRQoL research in Lithuania, as past studies indicated that dental caries and orthodontic anomalies are widely spread among children in different age groups in Lithuania [32, 44].
The first specific objective of our research was to elaborate a Lithuanian version of the CPQ. We fulfilled guidelines translating the original questionnaire into Lithuanian, including back translation [36, 37]. In order to make the questionnaire more acceptable to the Lithuanian children, several changes were incorporated in the questionnaire. For instance, when the questionnaire was piloted, most of the children could not recall that they need to choose option ‘not at all’ if the health complaint was due to reasons other than those related to their oral health. In order to avoid this confusion, wording of several health complaints was appended with the phrase ‘because of your teeth or mouth’.
In the Lithuanian version of the CPQ the only one modification was done which is related with the first item of the OS domain “Pain in your teeth, lips, jaws or mouth” (O1). In our opinion, this item is very general, while a specification of the pain location could be important for further analysis of the CPQ properties. For instance, it is important to distinguish well-being between children with dental caries, malocclusion and craniofacial anomalies [11]. This may also reflect the difficulties children may have with the concept of ‘oral health’, because of that they may be referring oral health complains to gingival health and caries status rather than malocclusion [45]. Participants of the pilot test also commented that a group of questions with specification of the pain location was easy to answer. Moreover, this item modification could not restrict the properties of the originally designed CPQ as the value of original item could be restored using mostly expressed paint. Unfortunately, a discussion of whether this change could be meaningful was not included in any of validation studies of the CPQ.
A wide range of statistical tools have been used in previous studies and their results for validity and reliability of the original instrument and its versions translated into other languages were rated positively in all studies [6]. The findings of the second specific objective of our study also confirmed high internal consistency of the original CPQ with national data. Cronbach α for the total CPQ was 0.875, which is in accordance with that reported by the developers of the CPQ in their validation study [11]. In general, the internal consistency of our survey was in any case as high as that reported by other CPQ validation studies [15–24]. However, Cronbach α of the OS domain (the domain which was modified in our study) was below an acceptable level of 0.70. Its value (0.645) was lower than that found from the Brazilian version (0.75) [46] and the Italian version (0.90) [20]. However, this value was as low as that obtained in many other studies, e.g. from the Australian version (0.68) [24], the Canadian version (0.64) [11], the Korean version (0,64) [21], the Indian version (0.629) [22] and the UK version (0.59) [23]. There may be several reasons for explaining the low Cronbach α of the OS domain. Since the value of Cronbach α depends on the number of items that make up the scale [33, 39], the lowest its value can be explained by the fact that OS domain contains the smallest number of items. Moreover, the OS domain describes the variety of oral symptoms that may be not so much associated, so there is no need to expect a high value of internal consistency. On the other hand, our study found other good parameters (p-value > 0.05, CFI > 0.95; TLI close to 1; and RMSEA< 0.08) which indicate that the model of associations between items in the OS domain presented a good fit to real data. These findings have confirmed good validity of the CPQ including its OS domain.
Similarly to other studies, we analysed construct validity of the instrument by assessing correlation between sum scores of the scale and overall ratings of oral health and well-being. In contrast with other studies, we estimated additionally the relationship of sum scores with the child’s global life satisfaction that is essential dimension of young people well-being [34, 47]. All estimations of correlation were significant that indicates adequate construct validity of the Lithuanian CPQ version.
To confirm discriminant validity, the distributions of sum scores of the instrument between the sub-groups of respondents were compared. Girls comparing with boys demonstrated significantly greater sum scores of the total CPQ. With regard to health domains, a significant difference was found for EWB domain only. These findings are in accordance with conclusions reported by several other authors [20, 48]. Difference between genders may be attributed to the poorer girls’ perception life satisfaction [34, 49], as well as of OHRQoL [48, 50]. Olivieri et al. [20] in validation study of the CPQ Italian version and Simoes et al. [51] in their study of Brazilian schoolchildren described a significant gradient within the social classes overall as well as in the emotional and social well-being domains. Findings from our study confirmed conclusions of Italian and Brazilian studies. There are suggestions in the literature that children from high-income families usually present better oral hygiene habits and have more access to prevention and dental treatment; hence, these conditions may reflect in a better OHRQoL [51, 52]. These findings confirm the need to consider family wealth when studying OHRQoL and planning oral health strategies in children [50].
Distribution of the CPQ scores identified significant differences between ‘healthy’ and ‘not healthy’ sub-groups defined on the basis of subjective rating of caries experience and malocclusion. We found that children with self-reported caries experience, comparing with those who were aware not having caries in their teeth, reported significantly greater scores in all health domains. In literature, the evidence that CPQ is associated with dental caries in the general population is not still clarified yet as there have been conflicting findings from the validation studies with some findings confirming such association [15–17, 21] and others not [18–20, 22, 23, 46]. Concerning subjective rating of malocclusion, we found that malocclusion as well as caries experience has a significant negative impact on the OHRQoL of children in terms of the CPQ scores, except SWB health domain. This effect was mostly noticeable for OS and EWB domains. Systematic reviews confirm that there is an association between malocclusion/orthodontic treatment need and poor OHRQoL in children seeking orthodontic treatment [43, 53–55]. It was concluded that malocclusion has a considerable negative impact on psychosocial functioning of both children and their families [56]. Therefore, it has been suggested that severe malocclusions have an impact on OHRQoL predominantly in the emotional and social dimensions [43, 53, 54] or, in contrast with our findings, in social dimension only [45].
In the present study, test-retest reliability of the CPQ instrument was not assessed due to organizational and logical reasons. With regard to organizational reasons, a retest appeared problematic as organizing another survey at several schools participating in our study would have a complex endeavour. With the respect to logical reasons, a retest of the same students was replaced with an alternative analysis that included comparison of children’s and their parents’ answers to the same questions of the OS and FL sub-scales. Such comparison was not performed for the EWB and SWB sub-scales, because some parents may have limited knowledge about their children’s OHRQoL, particularly the impact on social and emotional well-being [57]. As in other similar studies in this field [57–59], findings of the present study confirmed an agreement between child and parental reports suggesting on reliability of the CPQ in respect of its repeatability by two different raters.
Finally, the third specific objective of our study sought to explore the factorial structure of the Lithuanian CPQ. This technique allows for a more detailed assessment of the questionnaire validity [30]. In the literature, the hypothesized factor structure of the CPQ in terms how well the items reflect their corresponding health domains hasn’t been set out so widely as in researches of other instruments [26, 60]. To our knowledge, a CFA has been applied only by Lau et al. (2009) in the CPQ validation study for children in Hong Kong [28, 29]. Based on the five supplementary goodness-of-fit indices, the authors concluded that full CPQ model with four first-order factors fit the data below acceptable level. Among the four health domains, only the OS and FL fitted the data adequately but not for the domains EWB and SWB. We adopted factorial analysis, including both EFA and CFA, into validation of a Lithuanian version of the CPQ. The EFA revealed a non-homogenous structure of each health domain, which consisted of two or three dimensions. The CFA tested the structure of each health domain. Excellent or acceptable characteristics of the goodness-of-fit for data of the national sample of children were found for three of four domains: OS, FL and EWB. The item “Pain in teeth, lips, jaws or mouth” (O1) had a significant positive loading in the OS structure, which demonstrates the success of its modification in our study. The SWB domain fitted the data as poorly as for children in Hong Kong [28], consequently, this domain may be considered as an object of future research.
Strengths of the study
This study analysed data that were collected in cross-sectional population survey of young people samples but not within samples of patients attending dental treatment as in several studies [11, 45, 61, 62]. The children completed their questionnaires at school anonymously without any influence of their parents‘opinion, thus, children could express their own feelings towards their QoL that is an important condition comparing children’s and their parents responses. Employment of a CFA in testing of the CPQ instrument reliability that is unusual by most of the previous cross-cultural validation studies of CPQ11–14 also can to be considered as a novelty and strength of the study.
Limitations
There are several limitations in the current study. First and foremost, in the present study the CPQ sum scores were compared with the self-reported caries experience and malocclusion traits/orthodontic treatment need but not with clinical dental examination outcomes. The literature also shows that several studies did not reveal any effect of caries and malocclusion on the OHRQoL [18–20, 22, 23, 46]. Moreover, although our modification in the studied instrument helped to identify the kind of oral pain but the discriminant validation on the instrument was limited to caries and malocclusion. We believe that these comparisons are worth of greater attention, so their analysis will be an objective for another study. Next, given the aim of the present study, we worked on the “long form” (37 items) of the original CPQ11–14 together with other scales, including such as eating behaviour and self-esteem. Practical guides to develop measurement scales show that an increase of number of items in the questionnaire may affect respondent’s accuracy, especially for children, providing inaccurate answers, which may, consequently, reduce reliability of the tested scale [30]. Moreover, we added five sub-items for the first OS item, increasing the number of items in the questionnaire. We believe that this type of change would be better applied to the short-form CPQ, and further research should confirm this. Another important consideration is the age limitation (from 11 to 14 years old) of children to whom the instrument is addressed. Jokovic et al. [11] discussed the role of child’s cognitive abilities on self-report health status and suggested to be used age-specific questionnaires for children younger than 11-year-old. Therefore, we raise the hypothesis that the CPQ11–14 measure in older adolescent group (e.g. aged 16–18 years) is more reliable as it is in 11–14-year-olds, however, to date we haven’t found any studies confirming this hypothesis [63]. Finally, in the present study, test-retest reliability of the CPQ instrument was replaced with an alternative analysis that included comparison of children’s and their parents’ responses to the same questions of the OS and FL domains. This approach is not free from limitations, especially in relation to its accuracy because children and parents may not share the same views about illness and health [11].
Conclusions
The translated Lithuanian version of the CPQ11–14 with a modified item on the oral pain by identification its location demonstrated good internal consistency and construct and discriminant validity and appears to be a valid instrument to be used in further studies for measuring OHRQoL in Lithuanian children aged 11 to 14 years. However, employment of the factorial analysis revealed several weaknesses in dimensional structure of the social well-being domain, thus, a continuous psychometric analysis of the utilized instrument is recommended.
Additional file
Lithuanian version of the CPQ. (DOCX 44 kb)
Acknowledgements
The authors would like to thank the schoolchildren and their parents for their participation in this study as well as the teachers for their help during fieldwork.
Ethics and consent to participate
The study was conformed to the principles outlined in the Declaration of Helsinki. Ethical approval for the study was granted by the Kaunas Regional Biomedical Research Ethics Committee (reference number BE-2-27). In line with local practice for general school surveys, the study was agreed with national and local educational institutions. Additionally, written informed consent for child’s participation in the study was sought from both parents.
Funding
This study was funded by the Lithuanian University of Health Sciences.
Availability of data and materials
Not applicable.
Abbreviations
- CI
Confidence interval
- CFA
Confirmatory factor analysis
- CFI
Comparative fit index
- CPQ
Child perceptions questionnaire
- EFA
Explanatory factor analysis
- EWB
Emotional well-being
- FAS
Family affluence scale
- FL
Functional limitations
- HBSC
Health Behaviour in School-aged Children, a World Health Organization cross-national study
- IQR
Interquartile range
- KMO
Kaiser-Meyer-Olkin
- N
Number of subjects/respondents/cases
- OHRQoL
Oral health related quality of life
- OS
Oral symptoms
- QoL
Quality of life
- RMSEA
Root mean square error of approximation
- SWB
Social well-being
- TLI
Tucker-Lewis index
Authors’ contributions
AK performed the data collection, conducted the literature review and drafted the manuscript, AS supervised the study, conceptualized the rationale and designed the study, AZ performed statistical analysis and interpretation of its results, drafted the methodological parts of the manuscript, provided final editing of the manuscript. All authors read and approved the final manuscript.
Consent for publication
There are no details on individual participants within the paper.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Aistė Kavaliauskienė, Email: aiste.kavaliauskiene@lsmuni.lt.
Antanas Šidlauskas, Email: antanas.sidlauskas@lsmuni.lt.
Apolinaras Zaborskis, Email: apolinaras.zaborskis@lsmuni.lt.
References
- 1.Rozier RG, Pahel BT. Patient- and population-reported outcomes in public health dentistry: oral health-related quality of life. Dent Clin N Am. 2008;52(2):345–365. doi: 10.1016/j.cden.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Gherunpong S, Sheiham A, Tsakos G. A sociodental approach to assessing children's oral health needs: integrating an oral health-related quality of life (OHRQoL) measure into oral health service planning. Bull World Health Organ. 2006;84(1):36–42. doi: 10.2471/blt.05.022517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGrath C, Broder H, Wilson-Genderson M. Assessing the impact of oral health on the life quality of children: implications for research and practice. Community Dent Oral Epidemiol. 2004;32(2):81–85. doi: 10.1111/j.1600-0528.2004.00149.x. [DOI] [PubMed] [Google Scholar]
- 4.Sischo L, Broder HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. 2011;90(11):1264–1270. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennadi D, Reddy CV. Oral health related quality of life. J Int Soc Prev Community Dent. 2013;3(1):1–6. doi: 10.4103/2231-0762.115700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilchrist F, Rodd H, Deery C, Marshman Z. Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health. 2014;14:40. doi: 10.1186/1472-6831-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Genderson MW, Sischo L, Markowitz K, Fine D, Broder HL. An overview of children's oral health-related quality of life assessment: from scale development to measuring outcomes. Caries Res. 2013;47(Suppl 1):13–21. doi: 10.1159/000351693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gherunpong S, Tsakos G, Sheiham A. Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent Health. 2004;21(2):161–169. [PubMed] [Google Scholar]
- 9.Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the child Oral health impact profile (COHIP Child's version) Community Dent Oral Epidemiol. 2007;35(Suppl 1):20–31. doi: 10.1111/j.1600-0528.2007.0002.x. [DOI] [PubMed] [Google Scholar]
- 10.Huntington NL, Spetter D, Jones JA, Rich SE, Garcia RI, Spiro A., 3rd Development and validation of a measure of pediatric oral health-related quality of life: the POQL. J public health Dent. 2011;71(3):185–193. [PMC free article] [PubMed] [Google Scholar]
- 11.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81(7):459–463. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 12.Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26(6):512–518. [PubMed] [Google Scholar]
- 13.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Measuring parental perceptions of child oral health-related quality of life. J Public Health Dent. 2003;63(2):67–72. doi: 10.1111/j.1752-7325.2003.tb03477.x. [DOI] [PubMed] [Google Scholar]
- 14.Jokovic A, Locker D, Guyatt G. Short forms of the Child Perceptions Questionnaire for 11-14-year-old children (CPQ11-14): Development and initial evaluation. Health Qual Life Outcomes. 2006;4:4. doi: 10.1186/1477-7525-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foster Page LA, Thomson WM, Jokovic A, Locker D. Validation of the child perceptions questionnaire (CPQ 11–14) J Dent Res. 2005;84:649–652. doi: 10.1177/154405910508400713. [DOI] [PubMed] [Google Scholar]
- 16.Brown A, Al-Khayal Z. Validity and reliability of the Arabic translation of the child oral-health-related quality of life questionnaire (CPQ11-14) in Saudi Arabia. Int J Paediatr Dent. 2006;16(6):405–411. doi: 10.1111/j.1365-263X.2006.00775.x. [DOI] [PubMed] [Google Scholar]
- 17.Goursand D, Paiva SM, Zarzar PM, Ramos-Jorge ML, Cornacchia GM, Pordeus IA, et al. Cross-cultural adaptation of the Child Perceptions Questionnaire 11–14 (CPQ11–14) for the Brazilian Portuguese language. Health Qual Life Outcomes. 2008;6:2. doi: 10.1186/1477-7525-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gururatana O, Baker S, Robinson PG. Psychometric properties of long and short forms of the child perceptions questionnaire (CPQ11-14) in a Thai population. Community Dent Health. 2011;28(3):232–237. [PubMed] [Google Scholar]
- 19.Bekes K, John MT, Zyriax R, Schaller HG, Hirsch C. The German version of the child perceptions questionnaire (CPQ-G11-14): translation process, reliability, and validity in the general population. Clin Oral Investig. 2012;16(1):165–171. doi: 10.1007/s00784-010-0496-5. [DOI] [PubMed] [Google Scholar]
- 20.Olivieri A, Ferro R, Benacchio L, Besostri A, Stellini E. Validity of Italian version of the child perceptions questionnaire (CPQ11-14) BMC Oral Health. 2013;13:55. doi: 10.1186/1472-6831-13-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shin HS, Han DH, Shin MS, Lee HJ, Kim MS, Kim HD. Korean version of child perceptions questionnaire and dental caries among Korean children. PLoS One. 2015;10(2):e0116011. doi: 10.1371/journal.pone.0116011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar S, Kroon J, Lalloo R, Johnson NW. Psychometric Properties of Translation of the Child Perception Questionnaire (CPQ11-14) in Telugu Speaking Indian Children. PLoS One. 2016;11(3):e0149181. doi: 10.1371/journal.pone.0149181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marshman Z, Rodd H, Stern M, Mitchell C, Locker D, Jokovic A, Robinson PG. An evaluation of the child perceptions questionnaire in the UK. Community Dent Health. 2005;22(3):151–155. [PubMed] [Google Scholar]
- 24.Do LG, Spencer AJ. Evaluation of oral health-related quality of life questionnaires in a general child population. Community Dent Health. 2008;25(4):205–210. [PubMed] [Google Scholar]
- 25.Tabachnick BG, Fidell LS. Using multivariate statistics. 6. Boston: Pearson; 2013. [Google Scholar]
- 26.Marsh HW, Morin AJ, Parker PD, Kaur G. Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annu Rev Clin Psychol. 2014;10:85–110. doi: 10.1146/annurev-clinpsy-032813-153700. [DOI] [PubMed] [Google Scholar]
- 27.Schumacker RE, Lomax RG. A beginner's guide to structural equation modeling. 3rd ed. New York London: Routledge; 2010.
- 28.Lau AWH, Wong MCM, Lam KF, McGrath C. Confirmatory factor analysis on the heath domains of the child perception questionnaire. Community Dent Oral Epidemiol. 2009;37(2):163–170. doi: 10.1111/j.1600-0528.2008.00452.x. [DOI] [PubMed] [Google Scholar]
- 29.Wong MCM, Lau AWH, Lam KF, McGrath C, Hai-Xia L. Assessing consistency in oral health-related quality of life (OHRQoL) across gender and stability of OHRQoL over time for adolescents using Structural Equation Modeling. Community Dent Oral Epidemiol. 2011;39:325–335. doi: 10.1111/j.1600-0528.2010.00600.x. [DOI] [PubMed] [Google Scholar]
- 30.Streiner D, Norman G. Health measurement scales. A practical guide to their development and use. 2. New York: Oxford University Press; 2000. [Google Scholar]
- 31.Lwanga SK, Lemeshow S. A practical manual. Geneva: World Health Organization; 1991. Sample size determination in health studies. [Google Scholar]
- 32.Kavaliauskienė A, Sidlauskas A, Zaborskis A. Demographic and social inequalities in need for orthodontic treatment among schoolchildren in Lithuania. Medicina (Kaunas) 2010;46(11):767–773. [PubMed] [Google Scholar]
- 33.Pakalniškienė V. Metodinė priemonė. Vilnius: Vilniaus universiteto leidykla; 2012. Tyrimo ir įvertinimo priemonių patikimumo ir validumo nustatymas. [Google Scholar]
- 34.Inchley J, Currie D, Young T, Samdal O, Torsheim T, Augustson L, et al., editors. Growing up unequal: gender and socioeconomic differences in young people‘s health and well-being. Health behaviour in school-aged children (HBSC) study: international report from the 2013/2014 survey. Copenhagen: World Health Organization Regional Office for Europe; 2016. [Google Scholar]
- 35.Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med. 2008;66:1429–1436. doi: 10.1016/j.socscimed.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 36.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 37.Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, Erikson P. Principles of good practice for the translation and cultural adaption process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaption. Value Health. 2005;8:94–104. doi: 10.1111/j.1524-4733.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 38.Agou S. Oral health related quality of life outcomes of orthodontics in children. A dissertation. University of Toronto, 2009.
- 39.Aldridge V. Reliability assessment using SPSS. University of York, Centre for Applied Statistics Courses, UCL Institute of Child Health, 2015. http://www.spssusers.co.uk/Events/2015/ALDRIDGE2015.pdf. Accessed 23 Dec 2018.
- 40.Arbuckle JL. IBM SPSS AMOS 21 User's guide. Amos Development Corporation; 2012.
- 41.Confirmatory factor analysis using AMOS, LISREL, and MPLUS. 2006–2008 The Trustees of Indiana University. http://www.iu.edu/~statmath/stat/all/cfa/cfa2008.pdf. Accessed 23 Dec 2018.
- 42.Schermelleh-Engel K, Moosbrugger H, Muller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Meth Psychol Res. 2003;8:23–74. [Google Scholar]
- 43.Liu Z, McGrath C, Hägg U. The impact of malocclusion/orthodontic treatment need on the quality of life. A systematic review. Angle Orthod. 2009;79(3):585–591. doi: 10.2319/042108-224.1. [DOI] [PubMed] [Google Scholar]
- 44.Žemaitienė M. Prevalence and experience of dental caries and analysis of biohavioural and biological risk indicators among Lithuanian schoolchildren in late adolescence. A doctoral dissertation. Biomedical Sciences, Odontology (07B). Medical Academy of Lithuanian University of Health Sciences, Kaunas, 2017.
- 45.O'Brien C, Benson PE, Marshman Z. Evaluation of a quality of life measure for children with malocclusion. J Orthod. 2007;34(3):185–193. doi: 10.1179/146531207225022185. [DOI] [PubMed] [Google Scholar]
- 46.Barbosa TS, Tureli MCM, Gavião MBD. Validity and reliability of the Child Perceptions Questionnaires applied in Brazilian children. BMC Oral Health. 2009;9:13. doi: 10.1186/1472-6831-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kavaliauskienė A, Šidlauskas A, Zaborskis A. Association between Global Life Satisfaction and Self-Rated Oral Health Conditions among Adolescents in Lithuania. Int J Environ Res Public Health. 2017;14(11):1338. [DOI] [PMC free article] [PubMed]
- 48.Locker D. Disparities in oral health-related quality of life in a population of Canadian children. Community Dent Oral Epidemiol. 2007;35(5):348–356. doi: 10.1111/j.1600-0528.2006.00323.x. [DOI] [PubMed] [Google Scholar]
- 49.Watt RG, Listl S, Peres M, Heilmann A (Eds). Social inequalities in oral health: from evidence to action. International Centre for Oral Health Inequalities Research & policy. 2015. http://media.news.health.ufl.edu/misc/cod-oralhealth/docs/posts_frontpage/SocialInequalities.pdf. Accessed 23 Dec 2018.
- 50.Watt R, Sheiham A. Inequalities in oral health: a review of the evidence and recommendations for action. Br Dent J. 1999;187(1):6–12. [DOI] [PubMed]
- 51.Simoes RC, Goettems ML, Schuch HS, Torriani DD, Demarco FF. Impact of malocclusion on oral health-related quality of life of 8-12 years old schoolchildren in southern Brazil. Brazilian Dental J. 2017;28(1):105–112. doi: 10.1590/0103-6440201701278. [DOI] [PubMed] [Google Scholar]
- 52.Locker D, Frosina C, Murray H, Wiehe D, Wiebe P. Identifying children with dental care needs: evaluation of a targeted school-based dental screening program. J Public Health Dent. 2004;64:63–70. doi: 10.1111/j.1752-7325.2004.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 53.Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod. 2015;37(3):238–247. doi: 10.1093/ejo/cju046. [DOI] [PubMed] [Google Scholar]
- 54.Zhou Y, Wang Y, Wang X, Volière G, Hu R. The impact of orthodontic treatment on the quality of life a systematic review. BMC Oral Health. 2014;14:66. doi: 10.1186/1472-6831-14-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM. The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig. 2016;20(8):1881–1894. doi: 10.1007/s00784-015-1681-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Johal A, Cheung MY, Marcene W. The impact of two different malocclusion traits on quality of life. Br Dent J. 2007;202(2):E2. doi: 10.1038/bdj.2007.33. [DOI] [PubMed] [Google Scholar]
- 57.Barbosa Tde S, Gavião MB. Validation of the parental-caregiver perceptions questionnaire: agreement between parental and child reports. J Public Health Dent. 2015;75(4):255–264. doi: 10.1111/j.1752-7325.2012.00371.x. [DOI] [PubMed] [Google Scholar]
- 58.Barbosa TS, Gavião MB. Oral health-related quality of life in children: part III. Is there agreement between parents in rating their children's oral health-related quality of life? A systematic review. Int J Dent Hyg. 2008;6(2):108–113. doi: 10.1111/j.1601-5037.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 59.Li YJ, Gao YH, Zhang Y. The impact of oral health status on the oral health-related quality of life (OHRQoL) of 12-year-olds from children's and parents' perspectives. Community Dent Health. 2014;31(4):240–244. [PubMed] [Google Scholar]
- 60.Meuleners LB, Lee AH, Binns CW, Lower A. Quality of life for adolescents: assessing measurement properties using structural equation modelling. Qual Life Res. 2003;12(3):283–290. doi: 10.1023/a:1023221913292. [DOI] [PubMed] [Google Scholar]
- 61.Benson PE, Cunningham SJ, Shah N, Gilchrist F, Baker SR, Hodges SJ, Marshman Z. Development of the Malocclusion Impact Questionnaire (MIQ) to measure the oral health-related quality of life of young people with malocclusion: part 2 - cross-sectional validation. J Orthod. 2016;43(1):14–23. doi: 10.1080/14653125.2015.1114223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.De Baets E, Lambrechts H, Lemiere J, Diya L, Willems G. Impact of self-esteem on the relationship between orthodontic treatment need and oral health-related quality of life in 11- to 16-year-old children. Eur J Orthod. 2012;34(6):731–737. doi: 10.1093/ejo/cjr088. [DOI] [PubMed] [Google Scholar]
- 63.Kavaliauskienė A, Šidlauskas A, Zaborskis A. Validity of Lithuanian version of the child perceptions questionnaire among adolescents up to the ages of 18. J Clin Res Med. 2018;1(2):1–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lithuanian version of the CPQ. (DOCX 44 kb)
Data Availability Statement
Not applicable.