Abstract
Background
The use of alternative medicines and dietary supplements is constantly changing, as are dietary habits. One example of this phenomenon is the current popularity of ginger products as an everyday health boost. Ginger and licorice has also been shown to ameliorate nausea a common complaint in early pregnancy. Alternative medicines are often regarded as safe. However, they might affect fetal development, such as through alterations of hormone metabolism and cytochrome P450 function. Health care professionals may be unaware of the supplementation habits of pregnant women, which may allow adverse exposures to go unnoticed, especially if the rates of use in pregnancy are not known. We therefore investigated the use of alternative medicines and licorice among pregnant Danish women.
Methods
A total of 225 pregnant women were included in a prospective cohort when attending the national prenatal screening program at gestational weeks 10–16. Participants were asked to complete a questionnaire regarding their socio-economic status and lifestyle habits, including their intake of alternative medicine and licorice.
Results
We found that 22.7% of women reported taking alternative medicines, with 14.7% reporting daily consumption. Ginger supplements were consumed by 11.1%, mainly as health boost and 87.1% reported consumption of licorice. Regular or daily licorice consumption was reported by 38.2 and 7.1%, respectively. Notably, the use of licorice was reflected by an increase in blood pressure of the pregnant women.
Conclusions
The use of licorice and alternative medicines appears to be common in pregnant Danish women, supporting the need for further investigations into the safety of alternative medicine use during pregnancy and the importance of up-to-date personalized counseling regarding popular health trends and lifestyle habits.
Electronic supplementary material
The online version of this article (10.1186/s12906-018-2419-y) contains supplementary material, which is available to authorized users.
Keywords: Alternative medicine, First trimester pregnancy, Ginger, Herbal medicine, Licorice
Background
In modern society, everyday lifestyles are constantly changing. With the plethora of internet-based platforms, new health trends can spread rapidly among pregnant women. Such habits may escape the attention of health care professionals, allowing adverse exposures in early pregnancy to go undetected. International data supports the hypothesis that pregnant women perceive herbal and conventional medications as quite harmless [1]. Moreover, a recent study reported that recommendations to take contra-indicated herbal medicines during pregnancy may come directly from health care professionals [2].
A multinational study from 2016 suggested that up to 60% of all pregnant women use herbal-based alternative medicines [2]. However, cultural differences in the use of alternative medicine are well-established, even within the Scandinavian and Nordic countries. In Iceland, the prevalence has been reported to be as high as 35%, in contrast to Norway and Sweden where the prevalence has been reported to be 17 and 4%, respectively [3]. However, the prevalence of such use among pregnant women in Denmark has not previously been published.
Importantly, the safety of many herbal remedies has never been investigated in human pregnancies, as no strict rules for safety testing apply to alternative medicine [4] despite their teratogenic potential [5]. Several adverse effects caused by alternative medicine in pregnancy have been described, including miscarriage, preterm delivery, and malformations. Interestingly, recent data suggest that between 2.5–13% of pregnant women use alternative medicines together with prescribed medications [6]. However, there are limited published data investigating the adverse effects of alternative medicine due to their direct chemical toxicity, herbal-drug or herbal-herbal interactions.
Studies have shown that the majority (76%) of women who self-administer herbal medicine during pregnancy do not disclose their use to their doctor or midwife [7], making such use a potential safety concern.
Common exposure during pregnancy includes the use of ginger, which for decades has been the most widely used herbal remedy in the management of pregnancy-related nausea and vomiting. In addition, ginger is thought to strengthen the immune system and generally boost human health, leading to an increased popularity in recent years. At present, ginger is often added to consumables routinely sold in Danish supermarkets, such as teas and shots. The use of ginger as a health booster could lead to increased and continuous consumption throughout pregnancy, yet no guidelines currently exist in relation to the permissible amount of ginger exposure, even though ginger as a dietary supplement is not recommended by the Danish Veterinary and Food Administration. Several studies have found occasional use of ginger as an anti-emetic to be safe [8]. However, recent reports have shown that pharmacologically active substances in ginger may increase the risk of bleeding by decreasing platelet aggregation [9], and ginger-based compounds have been suspected to increase the risk of stillbirth [10]. If unaware of these potential risk pregnant women might continue their ginger habits throughout pregnancy – in particular if also obtaining a reduction of nausea that might give them the impression that ginger is well-tolerated by the body. Originally, licorice was used against upper respiratory problems and stomach inflammation while today it is primarily eaten for pleasure. However, a double-blind randomized study found a positive effect of licorice in prevention of acid reflux and vomiting [11]. Nausea and vomiting are common complains during pregnancy underlining that eating habits may also reflect a subconscious “self-medication” strategy in particular in Scandinavia were licorice based candies are well-known and popular. However, licorice can increase blood pressure, and the content of glycyrrhizin - the major active constituents of licorice - can also decrease platelet aggregation [12] making it a key problem that several candy products with licorice is increasingly being consumed during pregnancy.
As a systematic report of the current use of licorice, alternative medicines and other herbal supplements among pregnant Danish women has never been reported, the aim of this study was to assess the prevalence and characteristics of alternative medicine, ginger and licorice use among Danish pregnant women.
Methods
In this prospective cohort study, we included participants seen at the Department of Obstetrics and Gynecology, Randers Regional Hospital, Denmark between June 2016 and December 2016. The inclusion criteria was attendance at a routine ultrasound examination in gestational week 10–16, which is accepted by more than 95% of the pregnant women in the recruitment area where this scan is not offered elsewhere. Exclusion criteria included an age below 18 years and poor language skills.
The study was approved by the Regional Scientific Ethical Committee (VEK 1–10–72-75-16) and followed the Helsinki guidelines of informed consent. Due to additional obligations, we could only recruit participants 2–3 days a week. On these days all eligible women were invited in correlation with their random given times at the ultrasound unit (Table 1).
Table 1.
Demographic characteristics of the cohort
| Demography | % (n) |
|---|---|
| Maternal age (years) | |
| 20–29 | 50.9 (114) |
| 30–39 | 44.6 (100) |
| ≥ 40 | 4.5 (10) |
| Parity | |
| Nulliparous | 41.5 (93) |
| Primiparous | 44.6 (100) |
| Multiparous | 13.8 (31) |
| Maternal pre-pregnancy BMI (kg/m2) | |
| Underweight (< 18,5) | 1.8 (4) |
| Normal (18,5–24,9) | 43.3 (97) |
| Overweight (25–30) | 29.9 (67) |
| Obese (> 30) | 25.0 (56) |
| Chronic health issues | 28.6 (64)a |
| No chronic health issue | 71.4 (160) |
| Married | 42.0 (94) |
| In relationship, cohabitating | 54.0 (121) |
| In relationship, non-cohabitating | 2.2 (5) |
| Single | 1.3 (3) |
| Other | 0.4 (1) |
| Highest completed education level | |
| Elementary school | 3.6 (8) |
| Upper secondary school | 7.6 (17) |
| Vocational education | 25.0 (56) |
| Shorter level of education | 12.9 (29) |
| Bachelor degree | 37.9 (85) |
| Master degree | 12.1 (27) |
| Other | 0.9 (2) |
| Household income | |
| < 103,000 DKK | 0.9 (2) |
| 103,000–200,000 DKK | 3.6 (8) |
| 200,000–500,000 DKK | 35.3 (79) |
| 500,000–800,000 DKK | 46.4 (104) |
| > 800,000 DKK | 13.8 (31) |
aChronic health issues were self-reported, such as asthma and allergies, metabolic disorders, dermatitis, cardiovascular disorders, bowel disorders, autoimmune disorders and previous cancers
The participants answered a questionnaire at recruitment or during a phone call within 1–2 weeks regarding the following information: age, parity, Body Mass Index (BMI), smoking, alcohol, licorice intake, socio-economic status, educational level, use of prescription and over the counter medicine (OTC), supplemental vitamins, and intake of alternative medications including herbal supplements (e.g., teas). If the women used any health supplements or followed a specific nutritional lifestyle, they were asked to specify the amount and duration of the various intakes. After delivery, we obtained information regarding outcomes from the women’s electronic medical records (Additional file 1: Table S2).
Statistics
Continuous variables were compared between groups using Student’s tests or Mann-Whitney testing based on the testing of normal distribution of the data. Two-tailed comparisons were performed unless otherwise noted. Data are summarized as the means ± SD. GraphPad Prism version 7.03 Software (GraphPad Software, Inc., San Diego, CA, USA) was used to analyse the Student’s t-test and Mann-Whitney test results as well as confidence intervals presented in the relevant Tables. A level of significance at or below 0.05 was considered statistically significant for all analyses.
Results
Among 297 eligible Danish women attending a routine first trimester ultrasound scan during our presence, we included 225 (75.8%) women who accepted to participate in the study, corresponding to a prevalence of 23.1% of all birth at Randers Regional Hospital in the inclusion period. Lack of time was the most common reason given for non-participation.
All women were interviewed, all but one returned the completed questionnaire living a study population for this study of 224.
The vast majority 71.8% (n = 158) had a spontaneous vaginal delivery (for details on birth complications and new born Apgar score see Additional file 1: Table S2). Of the 224 women from whom questionnaire data were available, data on birth weight and infant health was available from 217 participants. Of the seven missing individuals, four had a spontaneous abortion (1.8%), and three (1.3%) were lost to follow up at birth, because they had moved to another district (Additional file 2: Figure S1). Information regarding the correspondence between exposures and outcome was based on the 217 women that gave birth at Randers Regional Hospital. (For details on parity and lifestyle see Additional file 3: Table S1).
Up to 22.7% (n = 51) reported consumption of at least one type of alternative medicine, 14.7% (n = 33) reported doing so daily, and 4.9% (n = 11) took more than one remedy regularly. This intake was associated with chronic health issues (31.3%; 20 of 64), of which the majority reported a daily use (20.0%; 13 of 65), and a high household income (32.3%; 10 of 31; Table 2).
Table 2.
Household income, educational level and nutritional habits
| Household income and educational level | Total number | Alternative medicines and herbal remedies % (n) | Ginger consumption 1st trimester % (n) | Licorice intake 1st trimester % (n) |
|---|---|---|---|---|
| Income in Danish Kroner | ||||
| < 103,000–200,000 DKK | 10 | 0.0 (0) | 0.0 (0) | 80.0 (8) |
| 200,000–500,000 DKK | 79 | 24.1 (19) | 10.1 (8) | 84.8 (67) |
| 500,000–800,000 DKK | 104 | 21.2 (22) | 11.5 (12) | 91.3 (95) |
| > 800,000 DKK | 31 | 32.3 (10) | 16.1 (5) | 83.9 (26) |
| Educational level | ||||
| Elementary school | 8 | 12.5 (1) | 12.5 (1) | 87.5 (7) |
| Upper secondary school | 17 | 17.6 (3) | 5.9 (1) | 88.2 (15) |
| Vocational education | 56 | 21.4 (12) | 7.1 (4) | 82.1 (46) |
| Shorter level of education | 29 | 20.7 (6) | 13.8 (4) | 89.7 (26) |
| Bachelor degree | 85 | 24.7 (21) | 12.9 (11) | 91.8 (78) |
| Master degree | 27 | 25.9 (7) | 14.8 (4) | 81.5 (22) |
Two participants were not included in educational level; one did not have an educational diploma, and one had an educational level not represented by the educational categories
Summary of the socioeconomic status among the women and their use of alternative medicines and herbal remedies with focus on ginger and licorice
Ginger products were the most frequently used form of alternative medicine (11.1%, n = 25), such as through shots (7.1%; n = 16), tea, tablets, and oil. Among these, 3.1% (n = 7) reported taking them alongside prescription or OTC medicine. Only 2.7% (n = 6) used ginger for nausea and vomiting. The intake of ginger products was associated with chronic health issues (17.2%; 11 of 64), mean maternal age 31.8 years (95% CI: 29.9–33.6) among users vs. 29.5 years (95% CI: 28.6–30.1) among non-users (p = 0.02), mean birthweight 3572 g (95% CI: 3316-3827 g) among exposed vs. 3440 g (95% CI: 3355-3525 g) among unexposed (p = 0.28). Additionally, the consumption rate of ginger increased with higher levels of education, lowest among women with an upper secondary school education (5.9%; 1 of 17) and highest among women with a master’s degree (14.8%; 4 of 27).
Other frequently used products included peppermint tea for nausea (1.8%; n = 4), Psyllium Husk Fiber® for obstipation (6.7%; n = 15), and Kräuterblut® as an herbal substitute for iron supplements (2.7%; n = 6), see Table 3 and Table 4.
Table 3.
Consumption of alternative medicine and herbal ailments
| Intake of alternative medicine and supplements | % (n) | Possible risk in pregnancy / recommendations during pregnancy |
|---|---|---|
| Alternative medicines | 22.7(51) | |
| Psyllium Husk Fiber | 6.7(15) | Delayed absorption of other drugs, necessary insulin dosage adjustment (downward) for diabetics [30] |
| Valerian | 0.4(1) | Influence on fetal ossification, cytotoxic and mutagen [5] |
| Glucosamines | 0.4(1) | No available information |
| Ginger | 11.1(25) | Induce abortion, influence fetal testosterone metabolism and maternal vaginal bleeding from gestational week 17 [5, 31] |
| Pregnancy tea (raspberry leaves and ginger) | 0.4(1) | Antigonadotrophic effects [5] |
| Mint tea | 1.8(4) | Emmenagogue properties [30] |
| Cranberry tablets | 0.4(1) | Insufficient treatment of UVI [3] |
| Kefir | 0.4(1) | Contains small amounts of alcohol (fermented) |
| Kombucha tea | 0.4(1) | Contains small amounts of alcohol (fermented) |
| Krauterblüt (herbal iron remedy) | 2.7(6) | Iron deficiency due to insufficient supplementation [32] |
| Thyme tea | 0.4(1) | Inducing abortion [2] |
| L-lysine | 0.4(1) | No available information |
| Green tea | 0.4(1) | Contains caffeine [30] |
| Turmeric | 0.4(1) | Induces abortion [33] and is cytotoxic [34] |
| Lactic Lactobacillus acidophilus bacteria | 0.9(2) | No available information |
| Boldocynara (Boldo, dandelion, mint, artichoke) | 0.4(1) | No available information, but mint has emmenagogue properties [30] |
| Oregano | 0.4(1) | No available information |
| Essential (Norwegian remedy) | 0.4(1) | No available information |
| MK oil (Linseed, evening primrose, rosehip, caraway) | 0.4(1) | Caraway has emmenagogue properties and spasmolytic effects [30], evening primrose increases the incidence of prolonged rupture of membranes, oxytocin augmentation and vacuum extraction [31] |
Overview of the reported use of alternative medicines by the women and an outline of the current recommendation and reported risk aspects in pregnancy from the medical literature
Table 4.
Usages of alternative medicines
| Name Scientific name |
Ethnomedical use | Verified scientific use | Use in Danish setting |
|---|---|---|---|
| Artichoke, in Boldocynara Cynara scolymus |
Loss of appetite, dyspeptic complains, and prophylactic against reemission of gallstones and as a tonic in convalescence [30] | No data of clinical efficacya | Against flatulencec |
| Boldo, in Boldocynara Peumus boldus |
Dyspeptic complaints [30] | No data of clinical efficacya | Against flatulencec |
| Brown Kelp, in Krauterblüt® Macrocystis pyrifera |
Weight reduction, against hypertension and anemia in pregnancy [30] | No clinical data | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Caraway, in MK oil Carum carvi |
Gastrointestinal cramps, flatulence, feelings of fullness, improve lactation, an emmenagogue [30] | Insufficient data of clinical efficacya | Anti-ageing properties with vital vitamins, minerals and bioflavonoidsc |
| Cascarilla, in Krauterblüt® Croton eluteria |
Digestive disorders, diarrhea and vomiting [30] | No clinical data | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Cranberry Vaccinium macrocarpon |
Against urinary tract irritation, gout, rheumatism and calculus [30] | Mixed data of clinical efficacy [35] | Prevention and treatment of lighter, recurrent urinary tract infectionsb |
| Dandelion, in Boldocynara Taraxacum officinale |
Acute mastitis, urinary disorders, chronic ulcers, tuberculosis, flatulence, colic, kidney disease, gout, jaundice and biliary stones [30] | No data of clinical efficacya | Against flatulencec |
| Evening primrose, in MK oil Oenothera biennis |
Neurodermatitis, premenstrual syndrome, dietary aid, high cholesterol levels, menopausal hot flashes, mastalgia and treatment of hyperactivity in children [30] | Insufficient data of clinical efficacya | Anti-ageing properties with vital vitamins, minerals and bioflavonoidsc |
| Fennel, in Krauterblüt® Foeniculum vulgare |
Peptic discomforts, disorders of the gastrointestinal tract, feeling of fullness, flatulence and catarrh of the upper respiratory tract [30] | Clinical data limited. Pharmacological data supports the use against mild spasmodic gastro-intestinal complaints, menstrual cramps and expectorants in cough with coldsa | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Field Horsetail, in Krauterblüt® Equisetum arvense |
Tuberculosis, catarrh in the kidney and bladder regions, a hematostatic for profuse menstruation, nasal, pulmonary and gastric hemorrhages, rheumatic diseases, gout, poorly healing wounds, swelling, fractures, frostbite and loss of hair [30] | Insufficient data of clinical efficacya | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Garden angelica, in Krauterblüt® Angelica archangelica |
Used against loss of appetite, dyspeptic and menstruation complaints, liver and biliary duct conditions, coughs and bronchitis [30] | Insufficient data of clinical efficacy. However, coumarin-derivatives in Angelica archangelica are phototoxica | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Ginger Zingiber officinale |
Used as a carminative, expectorant, and astringent. To treat colds, shortness of breath, nausea, vomiting, dyspeptic symptoms and pharyngitis [30] | Antiemetica | No available data |
| Glucosamines | Originally used in veterinary medicine | Limited data | Prevention and treatment of osteoarthritisc |
| Green tea Camellia sinensis |
Stomach disorders, nausea, migraine, symptoms of fatigue, vomiting, diarrhea, cardiac and circulatory conditions, states of agitation, states of depression, pain, fever and fatigue [30] | Stimulatory effecta (corroborated with the caffeine content) | No available data |
| Hibiscus, in Krauterblüt® Hibiscus sabdariffa |
Diuretic, mild laxative, treatment of hypertension, pyrexia, cough, colds, malaria and skin inflammations [36] | Insufficient data of antihypertensive efficacy [37] | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Kefir (fermented probiotic milk product) | Limited data | Limited data | No available data |
| Kombucha tea | Weight loss and anticancer properties [38] | No clinical data | No available data |
| Lactic Lactobacillus acidophilus bacteria (fermented probiotic milk product) | Introduced in the early twentieth century. To normalize the bacterial flora in the gut. | Mixed data of clinical efficacy [39] | Normalization of the intestinal florab |
| Licorice Glycyrrhiza glabra |
Sore throats, appendicitis, constipation, and to increase milk production and micturition [30] | Insufficient data of clinical efficacya | Mucous release effect for cough in shorter periodsb |
| Linseed, in MK oil Linum usitatissimum |
For coughs, bronchial conditions, urethritis, diarrhea and gonorrhea [30] | Mixed data of clinical efficacy. However, effectiveness of treatment of habitual constipation and softening of stool is plausiblea | Anti-ageing properties with vital vitamins, minerals and bioflavonoidsc |
| L-lysine | Limited data | Limited data | |
| Mint Mentha piperita |
Nausea, vomiting, morning sickness, respiratory infections, dysmenorrhea and colds [30] | Symptomatic relief of digestive disordersa | Indigestion and flatulenceb |
| Nettle, in Krauterblüt® Urtica dioica |
Hematogenic, rheumatic remedy, diuretic [30]. For diabetes, hypertension and prostate cancer [40] | Insufficient data of clinical efficacya | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Oregano Origanum vulgare |
Colds, fever, cough, vomiting, dyspepsia painful menstruation, rheumatoid arthritis, urinary tract disorders, dysentery, jaundice and malnutrition for children [30] | Limited data | No available data |
| Physillium Husk Fibre Plantago ovata |
Against inflammation of the mucous membrane in the urogenital and gastrointestinal tract [30] | Treatment of habitual constipation, desirable soft stool and adjuvant to diet in hypercholesterolemiaa | Against constipation, diarrhea, to increase fiber intake and adjuvant to diet in hypercholesteremiab |
| Quackgrass, in Krauterblüt® Agropyron repens |
Urinary tract infections [30] | No data of clinical efficacya | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Raspberry leavesRubus idaeus | Relieve nausea and induce labour [30] | Insufficient data of clinical efficacya | No available data |
| Rosehip, in MK oilRosa rugosa | Disorders in the efferent urinary tract, the kidneys, kidney stones, rheumatic conditions, gout, colds, scurvy, febrile conditions [30] | Limited data | Anti-ageing properties with vital vitamins, minerals and bioflavonoidsc |
| Spinach, in Krauterblüt® Spinacia oleracea |
Ailments of the gastrointestinal tract and blood generating [30] | Limited data | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Thyme Thymus vulgaris |
Catarrh of the upper respiratory tract, asthma, laryngitis, cough, gastritis and dyspepsia [30] | No data of clinical efficacya | Expectorate by productive cough in combination with Primula verisb |
| Turmeric Curcuma longa |
Dyspeptic disorders and inflammations [30] | No data of clinical efficacya | No available data |
| Yarrow, in Krauterblüt® Achillea millefolium |
Laxative and treatments against bleeding hemorrhoids, menstrual complaints and gynecological agents [30] | No data of clinical efficacya | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
| Wormwood, in Krauterblüt® Artemisia absinthium |
Ailments of gastrointestinal tract, liver disorders, bloating, anemia, irregular menstruation, intermittent fever, loss of appetite and worm infestation [30] | No data of clinical efficacya | Ensure a good supply of iron, riboflavin, pyridoxines, cobalamin and vitamin Cc |
aAccording to scientific rapports by European Medicines Agency (EMA)
bApproved by the Danish Medicines Agency
Please note that in a Danish context an herbal remedy can only be sold if approved by the authorities. However, this approval does not demand any scientific evidence and all though the remedies can only be advertised according to their approval they are sold freely and may be used for other purposes
cNot approved as an herbal remedy. Therefore, stating manufacturers own clarification of remedy on the Danish market
Overview of the common ethnomedical indications and possible scientific verified use concerning the reported use of alternative medicines and their potential indication for use in a Danish setting
No less than 87.1% (n = 196) reported consuming licorice, 38.2% (n = 86) reported licorice consumption at least “a couple of times a week,” and 7.1% (n = 16) reported daily use. On each occasion of consumption, 33.8% (n = 76) ate at least a handful of licorice candies, and 4.4% (n = 10) reported consuming an entire bag of licorice. All participants with hypertension (1.3%; n = 3) reported a weekly consumption of licorice. Moreover, the frequency of licorice intake was also associated, albeit not significantly, with reduced birthweight (see Fig. 1). Differences in mean blood pressures between women reporting a mean daily intake of licorice (123 mmHg, 95% CI: 116–130 mmHg) and women reporting rare or no intake of licorice (119 mmHg, 95% CI: 117–121 mmHg) were significantly associated with increased maternal systolic blood pressure (p = 0.04), estimated via one-tailed Mann-Whitney testing based on the known effects of licorice on blood pressure (see Table 5).
Fig. 1.
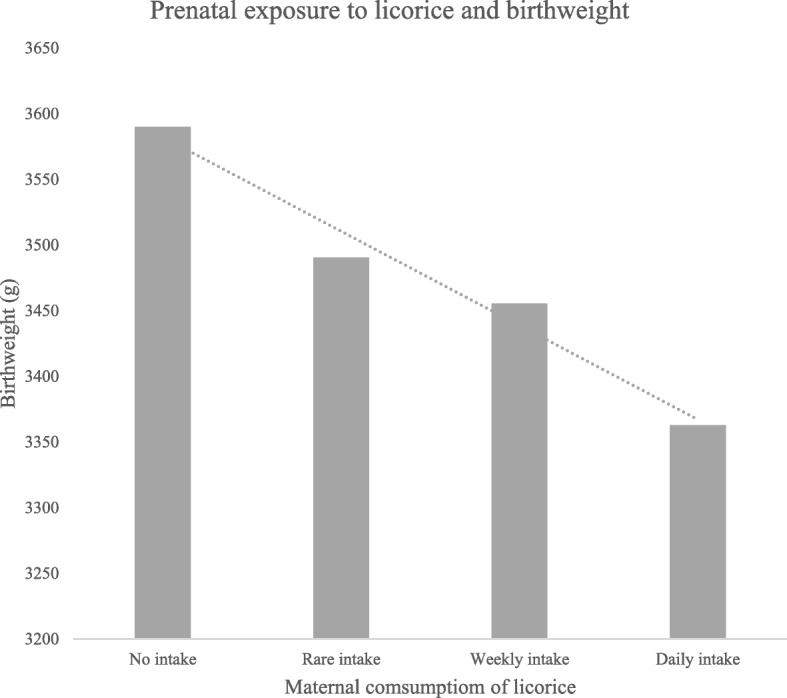
Association between birthweight and prenatal exposure to maternal licorice consumption. Maternal consumption of licorice showed an association with a reduced birthweight. Mean birthweight 3590 g, 95% CI: 3327-3853 g in the group with no intakeA, mean birthweight 3490 g, 95% CI: 3392-3589 g (p = 0.62) in the group with a rare intake, mean birthweight 3455 g, 95% CI: 3335-3575 g (p = 0.35) in the group with a weekly intake vs. mean birthweight 3363 g, 95% CI: 3010-3716 g (p = 0.29) in the group with a daily intake. AReference group
Table 5.
Maternal blood pressure at gestational week 29 in relation to licorice consumption
| Licorice consumption | BMI Mean, 95% CI | Systolic blood pressure mmHg Mean, 95% CI |
Diastolic blood pressure mmHg Mean, 95% CI |
P-value systolic/diastolic |
|---|---|---|---|---|
| Daily | 27.44 (23.91–30.97) | 122.81 (116.01–129.61) | 75.06 (69.86–80.26) | 0.04/0.51b |
| Weekly | 27.41 (26.04–28.77) | 119.37 (116.62–122.12) | 75.35 (73.53–77.18) | 0.34/0.42b |
| Rarelya | 25.81 (24.81-26.81) | 118.82 (116.37–121.27) | 75.82 (74.10–77.53) | |
| Nevera | 27.72 (25.18-30.26) | 118.19 (113.77–122.60) | 72.93 (68.08–77.77) |
aReference groups
bOne-tailed Mann-Whitney test
Among the women reporting daily consumption of licorice in first trimester, the measured blood pressure later in pregnancy was significant higher than the women who reported a rarely or no intake
Discussion
The main finding of this cohort study of Danish pregnant women was that 23% reported using alternative medicines, with ginger products being by far the most popular item. Furthermore, 87% reported consuming licorice, with 7% reporting daily use.
Performing the study in an unbiased manner where the eligible population was representative of the entire population in the geographic area, and achieving an overall participation rate of 76%, strengthen the value and validity of the findings. Notably, we cannot exclude that selection bias occurred, as the women had to accept participation. However, ultra-performance liquid chromatography with high-resolution time-of-flight mass spectrometry (UPLC-HR-TOFMS) analysis of the pharmacological content of the blood samples from the same cohort (Volqvartz and Vestergaard et al. in prep) indicates a high degree of consistence between results from this cohort and a similar UPLC-HR-TOFMS analysis of unselected, unbiased pregnant women from the same region performed by Aagaard and co-workers [13]. Also, the organisation of the maternal care system supports that all women from all parts of society attends the same, free-of-charge prenatal diagnostic system. On the other hand, limiting our study to one single interview means we did not assess all exposures occurring in pregnancy and, the size of the cohort limits the power to demonstrate possible associations between exposure and adverse obstetric outcomes in particular if the exposures are rare. However, by asking the women specifically if ginger or other substances were used do to pregnancy related nausea or for other reasons we obtained indication of the duration of the use.
Finally, we did not specifically inquire regarding the intake of red-clover-containing pregnancy tonics, which might explain why this was not mentioned by any participant. Notably, red clover is rich in phytoestrogens [14], and prenatal exposure is suspected to have deleterious effects on the developing male reproductive system; knowledge of the red-clover use among our subjects would thus be valuable. Analysis of 7928 boys in the cohort of “The Avon Longitudinal Study of Parents and Children” (ALSPAC) found that a maternal vegetarian diet rich in phytoestrogens in pregnancy was associated with an increased risk of hypospadias [15].
The fraction (23%) of pregnant women taking alternative medicines in this Danish study is relatively high compared to previous studies in Sweden (4%), Finland (9%), Norway (17%), and Iceland (35%) [3], but not compared to a number of non-Nordic countries (29%) [3]. However, the fraction appears lower than that among non-pregnant Danish pre-surgical patients of both genders (50%) [16]. The comparison of these studies is limited to some extent by different study designs and different definitions of alternative medicine. However, the positive associations with household income and education level is consistent across several studies [1]. With the size of this study, assessing specific adverse effects on fetal development might not be possible even with our focus on the time of organogenesis. However, studies of the Danish National Birth Cohort have found a higher risk for malformations after prenatal exposure to St. John’s wort [17]. This herbal medicine is a “natural anti-depressant” known to affect the serotonin system in ways similar to conventional antidepressants, which is a potential safety concern in pregnancy. With the high prevalence of users of alternative medicines identified in this study, further studies into the teratogenic effects of other exposures are warranted.
In particular, it appears important to focus on the use of ginger products among pregnant women. In Denmark, supermarkets expect to double the selling of ginger shots in coming years [18], even though 77% of the ginger consumers in our study did not declare their intake to be caused by a need to relieve symptoms. Ginger, or its active compound 6-gingerol (see Fig. 2) interacts with the cytochrome P450 system (e.g., CYP3A4, CYP2C9) [19] and fetal testosterone metabolism [20], thus serving as a potential teratogenic item. Furthermore, a cohort study from Korea showed 4 stillbirths among 159 singleton-pregnancy women receiving dried ginger (OR = 7.8; 95% CI 2.9–21) compared to the general population [10]. In addition, ginger decreases platelet aggregation, which may increase the risk of post-partum bleeding.
Fig. 2.
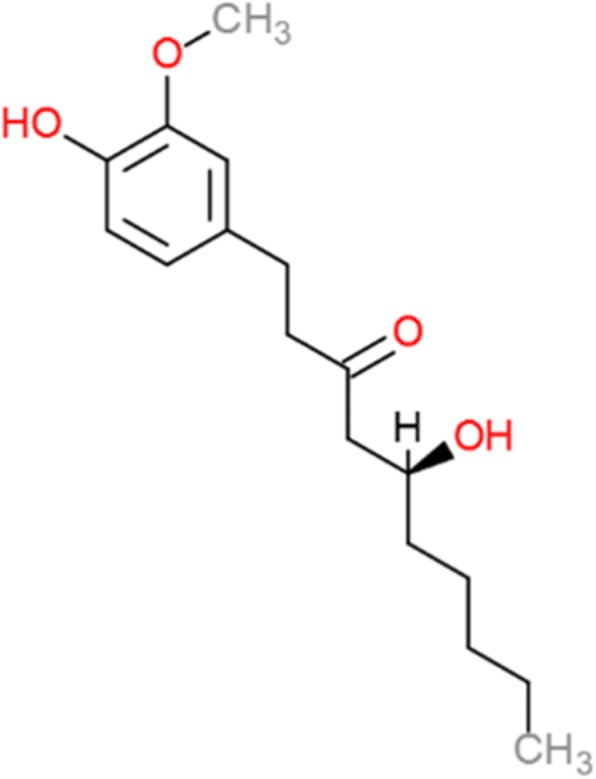
The chemical structure of 6-gingerols, the main active constituent of ginger, Zingiber officinale. Modified after Qui et al. [19]. 6-gingerol is derived from the phenylalanine pathway and has potential to be anti-septic, to have anti-cancer properties and reducing nausea and migraine
Additionally, the high use of licorice among pregnant women in Denmark deserves further attention. Regular consumption of licorice – and hence the active compound glycyrrhizin (see Fig. 3) - inhibits the 11-β-hydroxysteroid dehydrogenase type 2 (11-β-HSD2) enzyme, thereby activating cortisol and generating hypokalaemic hypertension [21]. Notably, we observed a minor increase in maternal systolic blood pressure (p = 0.04) and lower birthweights among children exposed to frequent maternal intake of licorice. The downregulation of 11-β-HSD2 in the placenta may contribute to several of the pathways leading to an increased risk of preeclampsia [21], miscarriage [22], preterm birth [23], toxicological effects [24], and lower intelligence quotient, poor memory and increased risk of attention deficit in the child [25]. Furthermore, the phytoestrogen found in licorice, glabridin, might explain the pubertal advancement seen in girls prenatally exposed to licorice [25, 26].
Fig. 3.
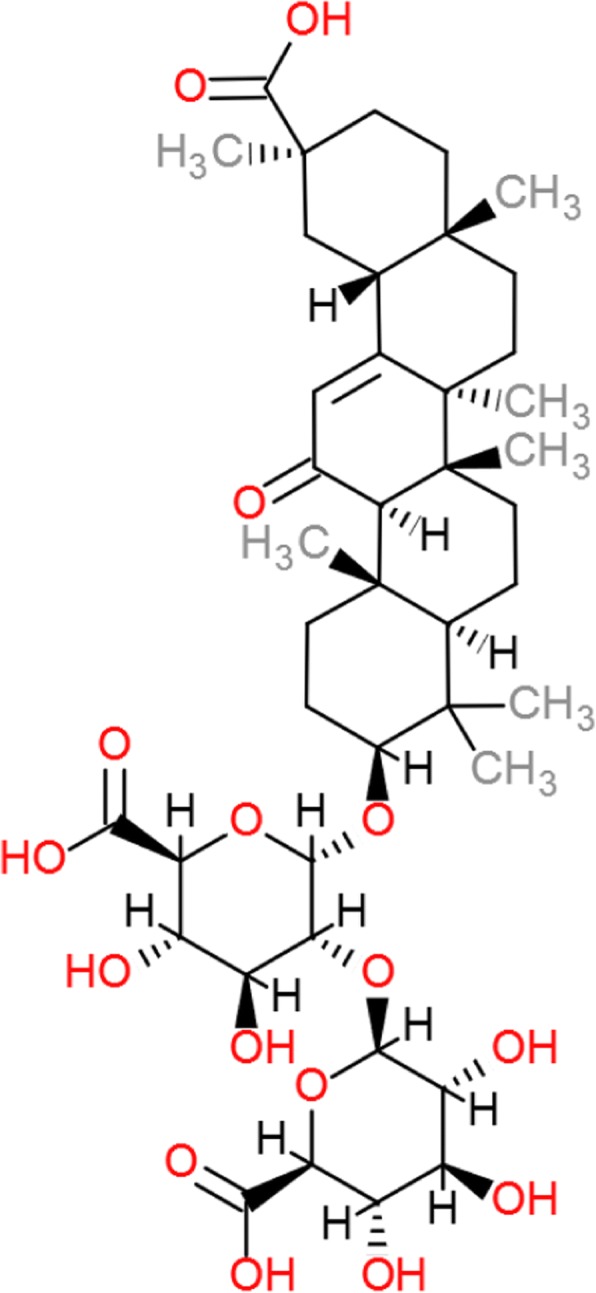
The chemical structure of licorice, glycyrrhizin. Modified after Li et al. [29]. Glycyrrhizin is the sweet component of licorice which is metabolized to glycyrrhetinic acid. Glycyrrhizin has potential to be anti-inflammatory. However, it also has the ability to cause retention of sodium and loss of potassium, increasing blood pressure, causing edema and affecting the renin-angiotensin-aldosterone system
In this study, we characterized lifestyle habits at the end of the first trimester of pregnancy, which is a very critical period of organogenesis [27]. Notably, several studies into the Developmental Origins of Health and Disease Hypothesis (DOHaD) have shown that different effect occur in responds to reprogramming at different part of the pregnancy (for a review see Roseboom and coworkers [28]). Further studies should be aimed at including additional information of the habits in later pregnancy and expand the number of participants as it cannot be excluded that changes in habits occur during pregnancy which could also affect offspring health.
Conclusions
In a Danish context, ginger and liquorice are commonly ingested by pregnant women as are alternative medications. Based on our results and the discussion above, we recommend that health providers actively seek to increase their knowledge of the eating habits and alternative medicine use of pregnant women to avoid unnecessary health risk in pregnancy.
Additional files
Table S2. Overview of pregnancy outcomes at birth. (DOCX 13 kb)
Figure S1. Flow diagram of participant involvement. (DOCX 24 kb)
Table S1. Summary of the relationship between parity and maternal lifestyle among the pregnant women. (DOCX 13 kb)
Acknowledgements
We would like to thank all doctors, midwives, health care workers and secretaries for their collaboration, financial support and for taking the time to help with the completion of this study at the Department of Obstetrics and Gynecology and the Research Unit, Randers Regional Hospital.
Funding
This study was financially funded by the A.P. Møller Foundation, the Grosserer L. F. Foghts Foundation, the Foundation of the 1870s and the Linex Foundation. These Foundations had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI
Body Mass Index
- DOHaD
Developmental Origins of Health and Disease Hypothesis
- OTC
Over-The-Counter
- UPLC-HR-TOFMS
Ultra-Performance Liquid Chromatography with High-Resolution Time-Of-Flight Mass Spectrometry Analysis
Authors’ contributions
TV and ALV participated in the design of the study and drafted the manuscript with inputs from AL and PB. TV conducted the analyses in collaboration with ALV, NU, AL and PB. SKA, MFA, IL, NU, AL, PB all participated in the design of the study, interpretation of data and revision of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All participants gave oral and written informed consent before participating. The study was approved by the Regional Scientific Ethical Committee (VEK 1–10–72-75-16).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Tabia Volqvartz and Anna-Louise Vestergaard shared first authorship
Agnete Larsen and Pinar Bor shared senior authorship
Contributor Information
Tabia Volqvartz, Email: tv@biomed.au.dk.
Anna Louise Vestergaard, Email: annalouise_4@hotmail.com.
Sissel Kramer Aagaard, Email: sissel.kramer.aagaard@clin.au.dk.
Mette Findal Andreasen, Email: mfa@forens.au.dk.
Iana Lesnikova, Email: LESNIKOVAI16@ECU.EDU.
Niels Uldbjerg, Email: uldbjerg@clin.au.dk.
Agnete Larsen, Email: al@biomed.au.dk.
Pinar Bor, Phone: +45 22504767, Email: isipinbo@rm.dk, Email: isibor@rm.dk.
References
- 1.Hall HG, Griffiths DL, McKenna LG. The use of complementary and alternative medicine by pregnant women: a literature review. Midwifery. 2011;27(6):817–824. doi: 10.1016/j.midw.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy DA, Lupattelli A, Koren G, Nordeng H. Safety classification of herbal medicines used in pregnancy in a multinational study. BMC Complement Altern Med. 2016;16:102. doi: 10.1186/s12906-016-1079-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kennedy DA, Lupattelli A, Koren G, Nordeng H. Herbal medicine use in pregnancy: results of a multinational study. BMC Complement Altern Med. 2013;13(1):355. doi: 10.1186/1472-6882-13-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danish Medicines Agency. Guidance on marketing authorization for herbal remedies (Markedsføringstilladelse til naturlægemidler) [Internet]. Lægemiddelstyrelsen. [cited 2017 Nov 30]. Available from: https://laegemiddelstyrelsen.dk/da/godkendelse/godkendelse-af-medicin/markedsfoeringstilladelse/ansoegning-om-markedsfoeringstilladelse/markedsfoeringstilladelse-til-naturlaegemidler/
- 5.Mills E, Dugoua J-J, Perri D. Herbal medicines in pregnancy and lactation: an evidence-based approach. 1st edition. United Kingdom: CRC Press. Taylor & Francis Group; 2006.
- 6.McLay JS, Izzati N, Pallivalapila AR, Shetty A, Pande B, Rore C, et al. Pregnancy, prescription medicines and the potential risk of herb-drug interactions: a cross-sectional survey. BMC Complement Altern Med. 2017;17(1):543. doi: 10.1186/s12906-017-2052-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frawley J, Adams J, Steel A, Broom A, Gallois C, Sibbritt D. Women’s use and self-prescription of herbal medicine during pregnancy: an examination of 1,835 pregnant women. Womens Health Issues Off Publ Jacobs Inst Womens Health. 2015;25(4):396–402. doi: 10.1016/j.whi.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Heitmann K, Nordeng H, Holst L. Safety of ginger use in pregnancy: results from a large population-based cohort study. Eur J Clin Pharmacol. 2013;69(2):269–277. doi: 10.1007/s00228-012-1331-5. [DOI] [PubMed] [Google Scholar]
- 9.Marx W, McKavanagh D, McCarthy AL, Bird R, Ried K, Chan A, et al. The Effect of Ginger (Zingiber officinale) on Platelet Aggregation: A Systematic Literature Review. PLoS ONE [Internet]. 2015 [cited 2017 Nov 23];10(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4619316/ [DOI] [PMC free article] [PubMed]
- 10.Choi JS, Han JY, Ahn HK, Lee SW, Koong MK, Velazquez-Armenta EY, et al. Assessment of fetal and neonatal outcomes in the offspring of women who had been treated with dried ginger (Zingiberis rhizoma siccus) for a variety of illnesses during pregnancy. J Obstet Gynaecol J Inst Obstet Gynaecol. 2015;35(2):125–130. doi: 10.3109/01443615.2014.941342. [DOI] [PubMed] [Google Scholar]
- 11.Raveendra KR, Jayachandra, Srinivasa V, Sushma KR, Allan JJ, Goudar KS, et al. An Extract of Glycyrrhiza glabra (GutGard) Alleviates Symptoms of Functional Dyspepsia: A Randomized, Double-Blind, Placebo-Controlled Study. Evid-Based Complement Altern Med ECAM [Internet]. 2012 [cited 2018 Nov 6];2012. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123991/ [DOI] [PMC free article] [PubMed]
- 12.Okuda-Tanino A, Sugawara D, Tashiro T, Iwashita M, Obara Y, Moriya T, et al. Licochalcones extracted from Glycyrrhiza inflata inhibit platelet aggregation accompanied by inhibition of COX-1 activity. PLoS One. 2017;12(3):e0173628. doi: 10.1371/journal.pone.0173628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aagaard SK, Larsen A, Andreasen MF, Lesnikova I, Telving R, Vestergaard AL, et al. Prevalence of xenobiotic substances in first-trimester blood samples from Danish pregnant women: a cross-sectional study. BMJ Open. 2018;8(3):e018390. doi: 10.1136/bmjopen-2017-018390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Humfrey CD. Phytoestrogens and human health effects: weighing up the current evidence. Nat Toxins. 1998;6(2):51–59. doi: 10.1002/(SICI)1522-7189(199804)6:2<51::AID-NT11>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 15.North K, Golding J. A maternal vegetarian diet in pregnancy is associated with hypospadias. The ALSPAC study team. Avon longitudinal study of pregnancy and childhood. BJU Int. 2000;85(1):107–113. doi: 10.1046/j.1464-410x.2000.00436.x. [DOI] [PubMed] [Google Scholar]
- 16.Vaabengaard P, Clausen LM. Surgery patients’ intake of herbal preparations and dietary supplements. Ugeskr Laeger. 2003;165(35):3320–3323. [PubMed] [Google Scholar]
- 17.Kolding L, Pedersen LH, Henriksen TB, Olsen J, Grzeskowiak LE. Hypericum perforatum use during pregnancy and pregnancy outcome. Reprod Toxicol Elmsford N. 2015;58:234–237. doi: 10.1016/j.reprotox.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Bleeg MT. Danskerne drikker ingefærshots som aldrig før: Det er unødvendigt - TV 2. livsstil.tv2.dk [Internet]. 2016 [cited 2017 Nov 23]; Available from: http://livsstil.tv2.dk/sundhed/2016-04-19-danskerne-drikker-ingefaershots-som-aldrig-foer-det-er-unoedvendigt
- 19.Qiu J-X, Zhou Z-W, He Z-X, Zhang X, Zhou S-F, Zhu S. Estimation of the binding modes with important human cytochrome P450 enzymes, drug interaction potential, pharmacokinetics, and hepatotoxicity of ginger components using molecular docking, computational, and pharmacokinetic modeling studies. Drug Des Devel Ther. 2015;9:841–866. doi: 10.2147/DDDT.S74669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Søndergaard K. [Ginger, pregnancy nausea and possible fetal injuries (testosterone effect)]. Ugeskr Laeger. 2008;170(5):359; author reply 359. [PubMed]
- 21.Räikkönen K, Pesonen A-K, Heinonen K, Lahti J, Komsi N, Eriksson JG, et al. Maternal licorice consumption and detrimental cognitive and psychiatric outcomes in children. Am J Epidemiol. 2009;170(9):1137–1146. doi: 10.1093/aje/kwp272. [DOI] [PubMed] [Google Scholar]
- 22.Cuzzolin L, Francini-Pesenti F, Verlato G, Joppi M, Baldelli P, Benoni G. Use of herbal products among 392 Italian pregnant women: focus on pregnancy outcome. Pharmacoepidemiol Drug Saf. 2010;19(11):1151–1158. doi: 10.1002/pds.2040. [DOI] [PubMed] [Google Scholar]
- 23.Strandberg TE, Järvenpää AL, Vanhanen H, McKeigue PM. Birth outcome in relation to licorice consumption during pregnancy. Am J Epidemiol. 2001;153(11):1085–1088. doi: 10.1093/aje/153.11.1085. [DOI] [PubMed] [Google Scholar]
- 24.Nazari S, Rameshrad M, Hosseinzadeh H. Toxicological effects of Glycyrrhiza glabra (licorice): a review. Phytother Res PTR. 2017;31(11):1635–1650. doi: 10.1002/ptr.5893. [DOI] [PubMed] [Google Scholar]
- 25.Räikkönen K, Martikainen S, Pesonen A-K, Lahti J, Heinonen K, Pyhälä R, et al. Maternal licorice consumption during pregnancy and pubertal, cognitive, and psychiatric outcomes in children. Am J Epidemiol. 2017;185(5):317–328. doi: 10.1093/aje/kww172. [DOI] [PubMed] [Google Scholar]
- 26.Simmler C, Pauli GF, Chen S-N. Phytochemistry and biological properties of glabridin. Fitoterapia. 2013;90:160–184. doi: 10.1016/j.fitote.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roseboom TJ, van der Meulen JH, Ravelli AC, Osmond C, Barker DJ, Bleker OP. Effects of prenatal exposure to the Dutch famine on adult disease in later life: an overview. Mol Cell Endocrinol. 2001;185(1–2):93–98. doi: 10.1016/S0303-7207(01)00721-3. [DOI] [PubMed] [Google Scholar]
- 28.Roseboom TJ, Painter RC, van Abeelen AFM, Veenendaal MVE, de Rooij SR. Hungry in the womb: what are the consequences? Lessons from the Dutch famine. Maturitas. 2011;70(2):141–145. doi: 10.1016/j.maturitas.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 29.Li J, Cao H, Liu P, Cheng G, Sun M. Glycyrrhizic Acid in the Treatment of Liver Diseases: Literature Review. BioMed Res Int [Internet]. 2014 [cited 2018 Nov 30];2014. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4052927/ [DOI] [PMC free article] [PubMed]
- 30.Fleming T, editor. PDR for herbal medicines. 2., rev. ed. Montvale, N.J: Medical Economics Co; 2000.
- 31.Dante G, Bellei G, Neri I, Facchinetti F. Herbal therapies in pregnancy: what works? Curr Opin Obstet Gynecol. 2014;26(2):83–91. doi: 10.1097/GCO.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 32.Holst L, Nordeng H, Haavik S. Use of herbal drugs during early pregnancy in relation to maternal characteristics and pregnancy outcome. Pharmacoepidemiol Drug Saf. 2008;17(2):151–159. doi: 10.1002/pds.1527. [DOI] [PubMed] [Google Scholar]
- 33.de Boer HJ, Cotingting C. Medicinal plants for women’s healthcare in Southeast Asia: a meta-analysis of their traditional use, chemical constituents, and pharmacology. J Ethnopharmacol. 2014;151(2):747–767. doi: 10.1016/j.jep.2013.11.030. [DOI] [PubMed] [Google Scholar]
- 34.Huang F-J, Lan K-C, Kang H-Y, Liu Y-C, Hsuuw Y-D, Chan W-H, et al. Effect of curcumin on in vitro early post-implantation stages of mouse embryo development. Eur J Obstet Gynecol Reprod Biol. 2013;166(1):47–51. doi: 10.1016/j.ejogrb.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 35.National Center for Complementary and Integrative Health. Cranberry [Internet]. NCCIH. 2011 [cited 2018 Nov 13]. Available from: https://nccih.nih.gov/health/cranberry
- 36.Abat JK, Kumar S, Mohanty A. Ethnomedicinal, Phytochemical and Ethnopharmacological Aspects of Four Medicinal Plants of Malvaceae Used in Indian Traditional Medicines: A Review. Medicines [Internet]. 2017 [cited 2018 Nov 13];4(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5750599/ [DOI] [PMC free article] [PubMed]
- 37.Serban C, Sahebkar A, Ursoniu S, Andrica F, Banach M. Effect of sour tea (Hibiscus sabdariffa L.) on arterial hypertension: a systematic review and meta-analysis of randomized controlled trials. J Hypertens. 2015;33(6):1119–1127. doi: 10.1097/HJH.0000000000000585. [DOI] [PubMed] [Google Scholar]
- 38.Teoh AL, Heard G, Cox J. Yeast ecology of Kombucha fermentation. Int J Food Microbiol. 2004;95(2):119–126. doi: 10.1016/j.ijfoodmicro.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 39.National Center for Complementary and Integrative Health. Probiotics: In Depth [Internet]. NCCIH. 2011 [cited 2018 Nov 13]. Available from: https://nccih.nih.gov/health/probiotics/introduction.htm
- 40.El Haouari M, Rosado JA. Phytochemical, Anti-Diabetic And Cardiovascular Properties Of Urtica dioica L. (Urticaceae): A Review. Mini Rev Med Chem. 2019;19(1):63–71. Epub ahead of print [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S2. Overview of pregnancy outcomes at birth. (DOCX 13 kb)
Figure S1. Flow diagram of participant involvement. (DOCX 24 kb)
Table S1. Summary of the relationship between parity and maternal lifestyle among the pregnant women. (DOCX 13 kb)
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.


