Abstract
The Centers for Disease Control and Prevention’s (CDC’s) Childhood Lead Poisoning Prevention Program (CLPPP) serves as the nation’s public health leader and resource on strategies, policies, and practices aimed at preventing lead exposure in young children. CDC supports and advises state and local public health agencies and works with other federal agencies and partners to achieve the Healthy People 2020 objective of eliminating childhood lead exposure as a public health concern. Primary prevention—the removal of lead hazards from the environment before a child is exposed—is the most effective way to ensure that children do not experience the harmful effects of lead exposure. Blood lead screening tests and secondary prevention remain an essential safety net for children who may be exposed to lead. CDC’s key programmatic strategy is to strengthen blood lead surveillance by supporting state and local programs to improve blood lead screening test rates, identify high-risk populations, and ensure effective follow-up for children with elevated blood lead levels. Surveillance plays a central role in helping measure the collective progress of federal, state, and local public health agencies in protecting children from lead, as well as enhancing our ability to target population-based interventions for primary prevention to those areas at highest risk. The CDC CLPPP has been at the front line of efforts to protect children from lead exposure and the resulting adverse health effects over the last 3 decades. As we chart our path for the future, we will continue to learn from past successes and challenges, incorporate new evidence and lessons learned, and work closely with federal, state, local, and nonprofit partners, experts in academia, and the community to advance the overarching goal of eliminating lead exposure in children.
Keywords: blood lead level, children, lead poisoning, prevention, public health
The Centers for Disease Control and Prevention (CDC) has a long-standing responsibility and commitment to protect children from lead poisoning, with its overarching goal to eliminate lead exposure in young children. Since the early 1970s, CDC has supported state and local health departments to develop lead poisoning prevention programs. Because lead exposure does not cause obvious symptoms until significant damage has already occurred, public health agencies have long relied on blood lead screening tests to identify exposed children. Blood lead screening for the purposes of primary or secondary prevention must be part of an integrated program to identify and control sources of exposure and provide case management for children with elevated blood lead levels (BLLs).1 Surveillance of children’s BLLs provides information on how well we are protecting children from exposure to lead and also provides critical information needed to identify and care for those children who are already exposed.2 State and local lead poisoning prevention programs initiate public health actions at varying BLLs based on applicable state/local laws and regulations as well as available resources. Case management for elevated BLLs involves follow-up testing, parental education, and counseling, and may include activities such as home visits to investigate and remediate the potential sources of exposure in a child’s environment and medical interventions, including chelation therapy, depending on the BLL.3 Blood lead screening and surveillance data also provide the foundation for targeting primary prevention activities to high-risk areas. Herein, we describe CDC’s congressional authorizations and appropriations, recommended approaches to blood lead screening, and role in defining the criteria for interpreting and monitoring BLLs in children.
Congressional Authorization and Appropriations of Blood Lead Screening Programs
The Lead-Based Paint Poisoning Prevention Act of 1971 required the Secretary of Health, Education, and Welfare (now Health and Human Services) to define paint chips as the primary health hazard of lead-based paint and to set the level of lead in blood warranting “concern” at 60 μg/dL (Public Law No. 91-965; January 13, 1971). Later that year, the US Surgeon General’s report on “Medical Aspects of Childhood Lead Poisoning” emphasized the need to shift the focus from identifying children with overt poisoning to prevention through early detection of children with “undue absorption of lead.”4 During the 1970s, CDC’s Division of Environmental Health Services directed by Dr Vernon Houk initiated a grant program for individual cities aimed at lead poisoning prevention.
As part of the Omnibus Budget Reconciliation Act of 1981, the appropriations for maternal and child health services were cut by 25% and folded into block grants that states allocated at their own discretion among various maternal and child health priorities, including lead poisoning prevention (Public Law No. 97-35; August 13,1981). Thus, the allocation of funds among the various health programs, previously dictated by the federal government, was dispersed back to the states. In 1988, Congress reinstated the categorical lead poisoning prevention program through the Lead Contamination Control Act of 1988 (Public Law No: 100-572; October 31, 1988). This authorized CDC to initiate efforts to eliminate childhood lead poisoning in the United States by supporting state and local agencies to develop comprehensive childhood lead poisoning prevention programs (CLPPPs). The purpose of these programs is to identify and monitor children at increased risk for lead exposure through enhancing blood lead screening efforts, ensuring referral for medical and environmental intervention for lead-exposed children, and providing education about childhood lead poisoning prevention.1
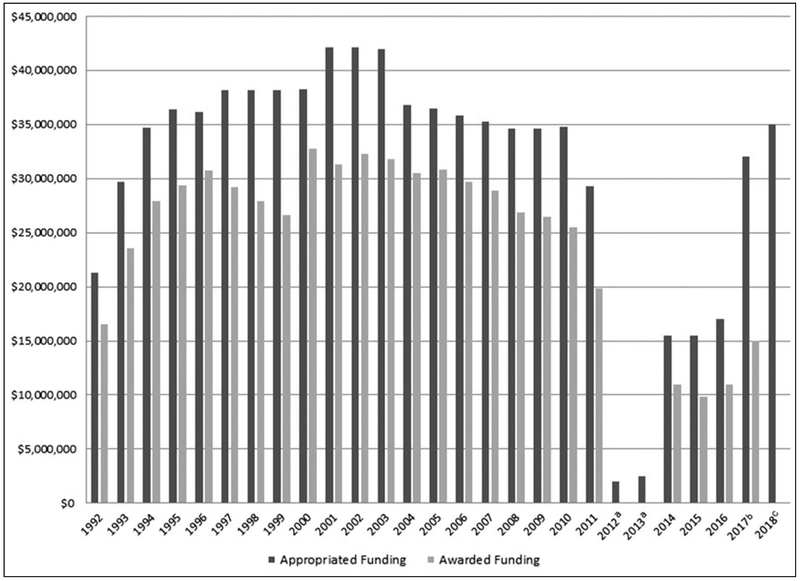
In February 1991, the Department of Health and Human Services released the Strategic Plan for the Elimination of Childhood Lead Poisoning that set forth a comprehensive agenda to eliminate childhood lead poisoning.2 The strategy for eliminating lead poisoning involved the following: (1) increasing the number of activities that led to the prevention of childhood lead poisoning and the funding of such activities; (2) increasing the abatement of lead-based paint in housing; (3) reducing children’s exposure to lead in the environment; and (4) establishing national surveillance of children with elevated BLLs. Appropriated funding levels for the CDC CLPPP averaged $36 million through the early- to mid-2000s (https://www.cdc.gov/budget/congressional-justification.html). Figure 1 shows the historical funding levels received and awarded by the CDC CLPPP. Over the last decade, 25 states have received 8 years of CDC CLPPP funding, and an additional 11 states have been funded for 5 years or more.
FIGURE 1.
Congressional Appropriations and Extramural Awards, by Year
aNo extramural funding awarded.
bAppropriated funding available for award over multiple years; does not include Flint-specific appropriations.
cExtramural funding awards pending.
Following on the Surgeon General’s “Call to Action to Promote Healthy Homes” in 2009, CDC broadened the CLPPP focus to include multiple health and safety housing hazards in addition to lead.5 In fiscal years (FY) 2012 and 2013, when congressional appropriations were reduced to $2 million, the CDC “Healthy Homes and Lead Poisoning Prevention Program” was essentially defunded. Consequently, CDC could no longer support extramural funding of state and local CLPPPs; CDC intramural staff and activities were dramatically reduced.
In FY 2014, funding was restored to $13 million— slightly more than one-third of pre-2012 funding levels. The Secretary of Health and Human Services designated lead poisoning prevention funds to be used to “support and enhance surveillance capacity” to end lead poisoning, and did not include addressing the broader issue of healthy homes. Also in 2014, the Flint water crisis brought national attention to the plight of approximately 100 000 residents in Flint, Michigan, who were exposed to lead in their drinking water.* The Water Resources Development Act (WRDA), in the 2016 Water Infrastructure Improvement for the Nation Act (WIIN), allocated $35 million in FY 2017 to CDC to develop a Flint lead exposure registry, establish an advisory committee, and enhance CDC’s childhood lead poisoning prevention activities. Thus, CDC transitioned its program emphasis back to a focus solely on lead poisoning prevention efforts.
Approaches to Blood Lead Screening
A central tenet of childhood lead poisoning prevention is that young children at risk for exposure are to be tested for lead. Chisolm and Kaplan6 suggested that blood lead screening tests should be routinely incorporated into laboratory tests for children living in high-risk areas. Recommendations for which children should be screened for lead have evolved over time as the risk factors for lead exposure have become better understood. In 1970, screening was recommended only for children who lived in or visited homes built before World War II.7 In 1975, CDC recommended screening for children at risk, defined primarily as those exposed to poorly maintained housing units constructed before 1960.8 Screening recommendations were updated in 1985 when CDC recommended screening for all children, if possible, with priority given to those exposed to older, dilapidated housing; who lived near heavily trafficked highways; who were siblings, housemates, visitors, or playmates of children with known lead toxicity; or whose family members had occupational lead exposures.9
In 1991, CDC strongly recommended screening by blood lead testing for virtually all children aged 1 to 5 years and that all children younger than 2 years be screened at least once.10 The Centers for Medicare & Medicaid Services (CMS) adopted these universal screening requirements for children receiving program benefits as part of a 1993 settlement of a nationwide class action lawsuit charging the federal government with failing to implement the Medicaid Act’s requirement for appropriate lead testing.11 Despite a renewed focus on lead poisoning prevention in the early- to mid-1990s, universal screening was not achieved and, in 1997, CDC recommended targeted screening efforts to focus on high-risk neighborhoods and children based on age of housing and sociodemographic risk factors.12 It was recommended that public health and clinical professionals collaborate to develop screening plans responsive to local conditions using local data. In the absence of such plans, universal blood lead testing remained the default, including the CMS requirement that all Medicaid-enrolled children be tested at 1 and 2 years of age.
Following on the recommendations of New York City and Minnesota, among others, and based on accumulating evidence of the adverse effects of early life exposure to lead, CDC charged the Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP) with reviewing the need for screening guidelines for women of reproductive age. In 2010, CDC released Guidelines for the Identification and Management of Lead Exposure in Pregnant and Lactating Women that provided scientific evidence and clinical guidance for identifying and managing lead exposure in both mothers and infants.13
Defining the Criteria for Interpreting BLLs in Children
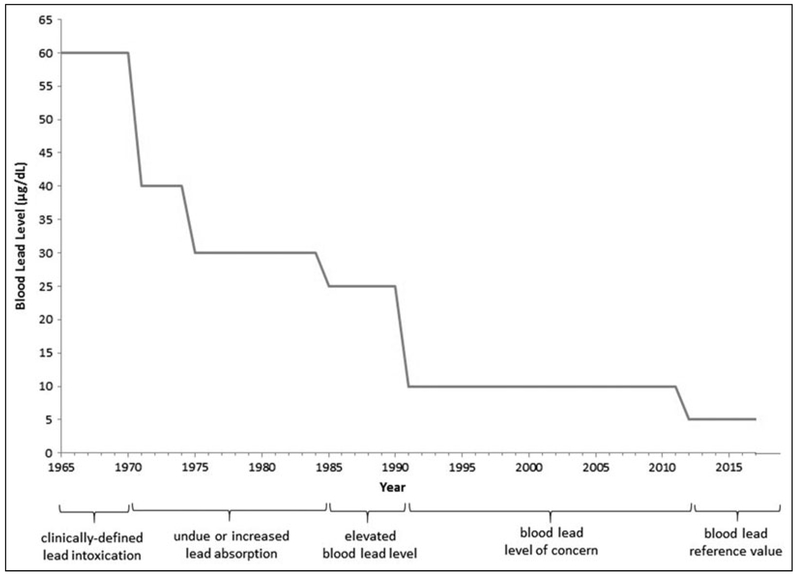
Prior to the 1970s, lead poisoning was clinically defined (Figure 2).14,15 The Surgeon General’s 1971 report defined a blood lead concentration of 40 μg/dL to be considered evidence suggestive of “undue absorption of lead, either past or present,” and defined “lead poisoning” as confirmed, on 2 successive determinations, BLLs of 80 μg/dL or more with or without symptoms.4 CDC became involved in defining the criteria for interpreting BLLs in children issuing its first statement on “Increased Lead Absorption and Lead Poisoning in Young Children.”8 With that statement, a confirmed BLL of 30 μg/dL or more was defined as “increased lead absorption.” Over the next 15 years, the criteria for defining “lead poisoning” in children were revised 3 times on the basis of new clinical and scientific evidence and improved laboratory techniques for measuring lead in blood.9,10,16 The term “elevated blood lead level” was first defined in 1978.16
FIGURE 2.
Changes to Definitions for Interpreting Children’s Blood Lead Levels Over Time
From 1991 to 2012, according to a widely adopted CDC policy, children were identified as having a blood lead “level of concern” if a laboratory blood lead test result indicated 10 μg/dL or more of lead in blood.10 This threshold value was recommended as the “action level” to prompt public health action by state or local health departments for individual case management and follow-up activities. In 2012, CDC’s former ACCLPP recommended elimination of the term “level of concern” and a shift in priorities to primary prevention.17 The ACCLPP also recommended using a “reference value” based on the 97.5th percentile of the blood lead distribution among children aged 1 to 5 years calculated from two 2-year cycles of National Health and Nutrition Examination Survey (NHANES) data. At that time, using data from NHANES 2007-2011, a blood lead reference value equal to 5 μg/dL was established to define when a child is exposed to higher levels of lead than 97.5% of the US children in that age range.
Monitoring BLLs in US Children
Since 1976, the NHANES has measured BLLs in a nationally representative sample of adults and children in the US population. This information has played a large role in developing public health interventions and assessing the effectiveness of regulations to decrease sources of lead in the environment.18,19,† NHANES BLL data are useful to examine trends over time and assess the effectiveness of intervention efforts on a population basis but are not generalizable to the state or local level.
In 1995, the CDC CLPPP began collecting blood lead surveillance data on children younger than 16 years from state health departments20 and the Council of State and Territorial Epidemiologists designated elevated BLLs as the first noninfectious condition to be notifiable to CDC on a voluntary basis for nationwide aggregation and monitoring (https://wwwn.cdc.gov/nndss/data-collection.html). A key component for surveillance of BLLs is a state law or regulation requiring that laboratories report all blood lead test results to the state health department.20 While these data are not nationally representative, blood lead surveillance data are used to examine trends and explore factors that may be related to differences in exposure levels by location and potential sources of exposure over time.
Managing Elevated BLLs in Children
Although progress has been made, lead in older homes remains a persistent problem in many aging and neglected communities. Consequently, children living in these high-risk areas may be exposed to lead and require services if their BLLs are found to be elevated. In 1985, CDC provided treatment guidelines for lead poisoning for state and local public health agencies.9 This document laid out the basic principles of case management that remain in use today: “eliminating the source of the child’s lead exposure; providing general pediatric care, family education, and, when appropriate, chelation therapy; and correcting any nutritional deficiencies.” Suggested clinical treatment pathways were based on a child’s classification level, using blood lead screening and erythrocyte protoporphyrin results, as well as other factors. The document also emphasized the need for immediate environmental investigation and intervention for children confirmed to have lead toxicity and provided details on what lead abatement should entail.
In 1991, CDC stated that the goal of interventions was to bring children’s BLLs to below 10 μg/dL and, to accomplish this, primary prevention activities such as community-wide environmental interventions and educational and nutritional campaigns should be implemented. Case management, including more frequent screenings (ie, every 3-4 months) and nutritional and educational interventions, was recommended for children with BLLs of 15 μg/dL or more. Recommendations for children with higher BLLs were as follows: for BLLs of 20 μg/dL or more, medical evaluation and environmental investigation and remediation; for BLLs of 45 μg/dL or more, urgent environmental investigation and medical attention; and BLLs of 70 μg/dL or more were considered a medical emergency.10
CDC published “Managing Elevated Blood Lead Levels Among Young Children” in 2002, in which the components of a comprehensive case management plan are explained in detail based on recommendations from the ACCLPP.21 The elements of case management were broader than those proposed in 19859 and included specific assessment and interventions relating to the home environment, medical care, education for caregivers, nutrition and diet, and developmental surveillance. Case management professionals, typically nurses or social workers, coordinate with the child’s caregiver, health care provider, and others, which may include an environmental inspector, a health educator, a nutritionist, and the local public health agency, to provide follow-up care for a child with an elevated BLL and ensure standards are met. The recommendations in the 2002 document closely aligned with those provided in 1991 but considered the latest scientific evidence available. A 2005 update to CDC’s Preventing Lead Poisoning in Young Children lowered BLL at which home environmental investigations were recommended from 20 to 15 μg/dL.22 A summary of CDC’s current recommendations for follow-up and case management of children based on confirmed BLLs is available at https://www.cdc.gov/nceh/lead/acclpp/actions_blls.html. A CDC expert panel recently reviewed the existing scientific evidence for adverse effects of BLLs on academic performance and described actionable steps that clinical and public health practitioners, parents, and educators can take to ensure that children receive such services.23
Core Public Health Functions in Relation to Childhood Lead Poisoning Prevention
The initial comprehensive lead poisoning prevention programs of the 1970s and 1980s involved the direct provision of health services particularly when administered as part of the block grants intended “to provide and to assure [that] mothers and children (in particular those with low income or with limited availability of health services) [have] access to quality maternal and child health services” (Social Security Act, §501 [42 USC 701] (a)(1)(A)). In 1988, the same year that the Lead Poisoning Prevention Control Act was enacted, the Institute of Medicine (IOM) published a landmark report on The Future of Public Health.24 In that seminal report, the IOM recommended that every public health agency focus on the 3 core functions of public health: assessment, policy development, and assurance. The CDC CLPPP uses this approach by applying the core public health functions to the prevention of childhood lead poisoning.25
Assessment
Since 1976, CDC has used NHANES data to assess and monitor trends in the population distribution of BLLs in US children and adults.19 The first report to Congress on The Nature and Extent of Lead Poisoning in Children in the United States was published in 1988 by the CDC/Agency for Toxic Substances and Disease Registry.26 CDC developed and maintains the Childhood Blood Lead Surveillance (CBLS) system that serves as the repository for surveillance data submitted by state and local health departments to monitor blood lead testing and trends in BLLs over time. CDC published the first CBLS report based on 19961999 data.27 In addition, over the past 2 decades, CDC and its cooperative agreement recipients have used geospatial information systems and mapping techniques to identify high-risk areas and populations. Collectively, these data sets and tools help programs identify where lead exposure is occurring so that resources can be directed to where they can be most impactful. For more than 40 years, CDC has developed and disseminated reports on trends in BLLs and testing and other information that continues to chart the course for future lead poisoning prevention strategies and activities.
Policy development
CDC has a well-documented track record in developing and disseminating guidance and recommendations aimed at helping state and local agencies fulfill the mission of identifying and protecting young children from lead exposure and its adverse health effects. Historically, CDC has convened experts from among federal partners; academia; nonprofit organizations; affected communities; and the general public—including parents of lead-exposed children— to advise the program and make evidence-based recommendations that also consider the practicalities of real-world implementation. The ACCLPP made important contributions to CDC policy development on topics such as establishing the blood lead reference value and reducing children’s lead exposures from imported products (https://www.cdc.gov/nceh/lead/acclpp/acclpp_main.htm). CDC recently participated in cataloging the Key Federal Programs to Reduce Childhood Lead Exposures and Eliminate Associated Health Impacts that enabled increased coordination and collaboration among federal agencies and is currently collaborating with other agencies to develop a comprehensive federal strategy to reduce childhood lead exposures and health impacts. (For more information, see https://ptfceh.niehs.nih.gov/activities/lead-exposures/index.htm.) By identifying clear goals, objectives, and actions, federal agencies can more easily work together and identify priorities to improve children’s health. In addition, CDC has recently established a charter for the Lead Exposure and Prevention Advisory Committee to review research, federal programs, and services related to lead poisoning and to identify effective services and best practices for addressing and preventing lead exposures in communities (https://www.federalregister.gov/documents/2018/02/13/2018-02823/lead-exposure-and-prevention-advisory-committee-lepac-notice-of-establishment).
Assurance
CDC provides funding to support state and local public health agencies to strengthen their capacity to engage in primary and secondary lead poisoning prevention activities in high-risk areas and populations. CDC provides technical assistance to ensure that federal policies and recommendations are carried out at the state and local levels. In recent years, CDC cooperative agreement award recipients have been primarily responsible for oversight of blood lead testing, surveillance, public education, and outreach activities and ensuring that environmental and clinical followup for children with elevated BLLs occurs. This involves developing and maintaining partnerships with responsible agencies, health care providers, clinical laboratories, nonprofit organizations, and other partners. Well-designed and properly utilized blood lead surveillance systems are able to fulfill these functions, including laws and regulations requiring blood lead testing and reporting of test results to state and health agencies. In 1990, only 5 states had comprehensive lead poisoning prevention laws; by 2010, the number had increased to 23 states with such laws.18,28 In addition, CDC is assisting programs to develop targeted population-based interventions aimed at improving the ability to identify high-risk children and link them to recommended services.
Discussion
Eliminating childhood lead poisoning is an achievable goal through continued use of evidence-based practices at the individual and population levels. First, intensive efforts to identify and provide services to children who have elevated BLLs have proven to be effective. Evidence-based practices developed for children affected by lead involve ensuring that they receive timely and appropriate medical, nutritional, environmental, and educational interventions. Primary prevention strategies that control or eliminate sources of lead before children are exposed remain the preeminent public health approach to address lead poisoning and the only effective way to prevent the neurodevelopmental and behavioral abnormalities associated with lead exposure. The economic benefit of lowering lead levels among children by preventing lead exposure has been estimated at $213 billion per year.29
CDC remains committed to supporting state and local efforts to engage pediatric health care providers in identifying and evaluating children who are exposed to lead and providing these children with necessary follow-up services. CDC supports the proven practice of blood lead testing as the best method to screen children for lead exposure. CDC is committed to achieving the Healthy People 2020 objective of eliminating childhood lead exposure as a public health concern and recognizes that this can only be accomplished with the commitment and cooperation of pediatric health care providers. The CDC CLPPP has been at the front line of efforts to protect children from lead exposure for more than 4 decades. As we chart the path for the future, we will continue to learn from past successes and challenges, incorporate new evidence-based practices and interventions, and work closely with federal, state, local, and nonprofit partners, experts in academia and medicine, and the community to advance the overarching goal of eliminating lead exposure in children.
Implications for Policy & Practice.
Primary prevention is the most effective way to prevent lead exposures in young children; however, blood lead screening tests and secondary prevention remain a proven and essential safety net for children exposed to lead. The CDC CLPPP will continue to strongly support local and state programs’ use of evidence-based practices and strategies to improve blood lead screening test rates, identify high-risk populations, and provide effective follow-up for children with elevated BLLs.
Surveillance plays a central role in helping measure the collective progress of federal, state, and local public health agencies in protecting children from lead, as well as in enhancing our ability to target children at highest risk. CDC will continue to update and improve its surveillance capabilities and work with state and local programs to do the same.
Fundamentals of the approaches currently used to address lead poisoning have, for the most part, remained intact since being delineated decades ago. Although as the evidence base underlying these approaches has evolved, changes have been made to recommendations about how or when interventions are implemented. CDC supports evidence-based approaches by continuing to work with experts to update scientific and practice-based evidence.
Acknowledgments
The authors acknowledge the state and local health department programs and the dedicated staff who fulfill the mission of identifying and protecting young children from lead exposure and its adverse health effects.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
Human Participant Compliance Statement: This information was reviewed and deemed not human subjects research by the Centers for Disease Control and Prevention.
The authors declare that they have no conflicts of interest.
Editor’s note: For more information about the Flint Water Crisis, see the article by Ruckart et al on page S84 of this special issue.
Editor’s note:For more information about the control of sources of lead, see the article by Dignam et al on page S13 of this special issue.
References
- 1.Centers for Disease Control and Prevention. Implementation of the Lead Contamination Control Act of 1988. MMWR Morb Mortal Wkly Rep. 1992;41(17):288–290. [PubMed] [Google Scholar]
- 2.Health and Human Services. Strategic Plan for the Elimination of Childhood Lead Poisoning. Washington, DC: US Department of Health and Human Services; 1991. [Google Scholar]
- 3.American Academy of Pediatrics. Council on Environmental Health Policy statement: prevention of childhood lead toxicity [Erratum in: Pediatrics. 2017;140(2):e20161493]. Pediatrics. 2016;138(1):1–17. [DOI] [PubMed] [Google Scholar]
- 4.Public Health Service. The Surgeon General’s Policy Statement on Medical Aspects of Childhood Lead Poisoning. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1971. [Google Scholar]
- 5.Health and Human Services. The Surgeon General’s Call to Action to Promote Healthy Homes. Washington, DC: US Department of Health and Human Services; 2009. [Google Scholar]
- 6.Chisolm JJ Jr, Kaplan E. Lead poisoning in childhood— comprehensive management and prevention. J Pediatr. 1968;73(6): 942–950. [DOI] [PubMed] [Google Scholar]
- 7.Chisolm JJ. Screening techniques for undue lead exposure in children: biological and practical considerations. J Pediatr. 1971; 79(5):719–725. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Increased Lead Absorption and Lead Poisoning in Young Children: A Statement by the Centers for Disease Control (CDC). Atlanta, GA: US Department of Health, Education, and Welfare, Public Health Service; 1975. [Google Scholar]
- 9.Centers for Disease Control and Prevention. Preventing Lead Poisoning In Young Children: A Statement by the Centers for Disease Control (CDC). Atlanta, GA: US Department of Health and Human Services, Public Health Service; 1985. [Google Scholar]
- 10.Centers for Disease Control and Prevention. Preventing Lead Poisoning in Young Children: A Statement by the Centers for Disease Control (CDC). Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 1991. [Google Scholar]
- 11.Thompson v Raiford, No. 3:92-CV-1539-R, 1993 WL 497232, reprinted in Medicare & Medicaid Guide (CCH) & 41,776 (ND Tex, September 24, 1993). [Google Scholar]
- 12.Centers for Disease Control and Prevention. Screening Young Children for Lead Poisoning: Guidance for State and Local Public Health Officials. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 1997. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Guidelines for the Identification and Management of Lead Exposure in Pregnancy and Lactation. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2010. [Google Scholar]
- 14.Chisolm JJ. Childhood lead intoxication. Diagnosis, management, and prevention. Med Times. 1970;98(9):92–106. [PubMed] [Google Scholar]
- 15.Graef JW, Kopito L, Shwachman H. Lead intoxication in children. Diagnosis and treatment. Postgrad Med. 1971;50(6):133–138. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Preventing Lead Poisoning in Young Children: A Statement by the Centers for Disease Control (CDC). Atlanta, GA: US Department of Health, Education, and Welfare, Public Health Service; 1978. [Google Scholar]
- 17.Advisory Committee for Childhood Lead Poisoning Prevention. Low Level Lead Exposure Harms Children: A Renewed Call of Primary Prevention (A Report by Advisory Committee on Childhood Lead Poisoning Prevention). Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 18.Centers for Disease Control and Prevention. Ten great public health achievements—United States, 2001-2010. MMWR Morb Mortal WklyRep. 2011;60:619–623. [PubMed] [Google Scholar]
- 19.Jl Annest, JL Pirkle, D Makuc, JW Nesse, DD Bayse, MG Kovar. Chronological trend in blood lead levels between 1976 and 1980. N Engl J Med. 1983;308:1373–1377. [DOI] [PubMed] [Google Scholar]
- 20.Pertowski C Lead poisoning In: From Data to Action: CDC’s Public Health Surveillance for Women, Infants, and Children. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 1994:311–319. [Google Scholar]
- 21.Centers for Disease Control and Prevention. Managing Elevated Blood Lead Levels Among Young Children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2002. [Google Scholar]
- 22.Centers for Disease Control and Prevention. Preventing Lead Poisoning in Young Children: A Statement by the Centers for Disease Control and Prevention. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2005. [Google Scholar]
- 23.Centers for Disease Control and Prevention. Educational Interventions for Children Affected by Lead. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2015. [Google Scholar]
- 24.Institute of Medicine. The Future of Public Health. Washington, DC: National Academies Press; 1988. [Google Scholar]
- 25.Niskar AS, Buchanan S, Meyer PA. A federal agency’s role in fulfilling the public health core functions: the Childhood Lead Poisoning Prevention Program model. J Public Health Manag Pract. 2005;11(1):50–58. [DOI] [PubMed] [Google Scholar]
- 26.Agency for Toxic Substances and Disease Registry. The Nature and Extent of Lead Poisoning in Children in the United States: A Report to Congress. Atlanta, GA: Agency for Toxic Substances and Disease Registry, US Department of Health and Human Services; 1988. [Google Scholar]
- 27.Blood lead levels in young children—United States and selected states, 1996-1999. MMWR Morb Mortal Wkly Rep. 2000; 49(50):1133–1137. [PubMed] [Google Scholar]
- 28.Dickman J. Children at Risk: Gaps in State Lead Screening Policies. Washington, DC: Safer Chemicals Healthy Families; 2017. [Google Scholar]
- 29.Grosse SD, Matte TD, Schwartz J, et al. Economic gains resulting from the reduction in children’s exposure to lead in the United States. Environ Health Perspect. 2002;110:563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]