Abstract
Objective.
To explore the association of maternal health literacy (MHL), parenting self-efficacy and early parenting practices among low-income mothers with infants.
Design.
A cross-sectional, descriptive correlational design.
Participants.
Low-income mothers (N=186) with infants.
Methods.
Face-to-face interviews were conducted using English and Spanish versions of questionnaires by trained bilingual research assistants. The Newest Vital Sign (NVS) screening tool was used to measure MHL.
Results.
Nearly three-quarters (72%) of mothers were rated as having low MHL. In the bivariate analysis, MHL was positively correlated with education, household income, language, social support, parenting self-efficacy, and early parenting practices, but negatively correlated with number of children. The study findings demonstrate that parenting self-efficacy had a mediating effect on MHL and early parenting practices among mothers with infants.
Conclusion.
Results suggest that future research is needed to advance MHL in low-income mothers and to inform potential HL interventions for this target population.
Keywords: Parenting, health literacy, infant, self-efficacy, mothers
The first year of an infant’s life is a critical period of growth and development. The science of early child development is clear about the importance of parenting, especially during infancy, when the child depends entirely on the parent for safety, health, protection, nurturing, and stability.1,2 During this period, mothers have an increased need for health information as they are faced with many new caregiving skills that may include mixing and preparing infant formula, taking and interpreting temperatures using thermometers, and administering over-the-counter (OTC) and prescription medications to their infants.3,4 Literacy skills are essential for these and a host of other infant caregiving behaviors. Both negative and positive effects of mothers’ literacy skills and health literacy can be passed on to their children, with lifelong consequences.5
According to an analysis of the health literacy of parents in the U.S., approximately one in four parents have limited health literacy skills.6 More importantly, a parent’s low health literacy is related to unexpected or unintended safety concerns of the children and their development, both mentally and physically.7,8 For example, there are reports that parents with low health literacy visit the emergency room more often than parents with adequate health literacy levels.9 Even more alarming is the association between limited health literacy and inappropriate parental understanding and administration of pediatric medications, which may place the child at severe risk of an adverse medication effect.10,11 In addition, studies of parents or caregivers of young children, including infants, reported that low health literacy was related to negative caregiver health behaviors for infants, such as obesogenic infant care behaviors,12 injury prevention behaviors,13 perception of ambulatory care, upper respiratory infection knowledge and beliefs,14 understanding pediatric cough and cold medication labels, and breastfeeding.15,16
Although the relationship between health literacy and health outcomes has been established, the exact mechanisms or pathways linking the two are unclear. Thus, it is important to understand how maternal health behaviors affect infant development during this time period. Parenting self-efficacy has been identified as an important factor that influences an infant’s physical and mental health development and also as a key to enhancing parenting behavior and to support parents in their role of parenting.17–20
While much evidence has shown that the rates of limited health literacy are higher among minority groups and those with low incomes,21,22 a limited number of studies have been conducted on low-income mothers of infants. This research is designed to address critical knowledge gaps related to maternal health literacy and its effect on parenting behaviors in low-income communities. The purposes of this study are (1) to characterize the level of maternal health literacy and its correlates, (2) to determine relationships between maternal health literacy and health outcomes of families’ infants, and (3) to identify the underlying pathways that might describe the effect of maternal health literacy on theoretically selected mediators, parenting self-efficacy, and ultimately on parenting practices for infants.
Methods
Conceptual framework and study design.
A descriptive, cross-sectional correlational design was used for this study. Figure 1 presents the conceptual model for this study. This study is based on Paasche-Orlow and Wolf’s (2007)23 conceptual model, which was developed from a review of previous studies related to health literacy (Figure 1). The proposed model explains relationships between personal and environmental factors for health literacy among mothers with infants and the pathways of the effects of health literacy on health outcomes, which are mediated by critical patient-level factors such as parenting self-efficacy.
Figure 1.
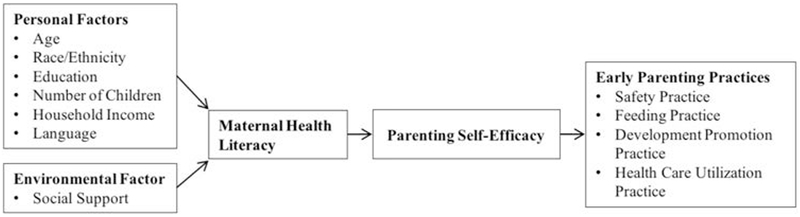
Conceptual framework.
Setting and sample.
The participants were 186 mothers of infants who received infant (birth to under 12 months) care at two federally qualified health centers in an urban county in central Texas. Federally qualified health centers (FQHCs) provide safety-net health care services to poor and underserved populations. The two clinics chosen for this study provide services to county residents whose incomes and lack of private health insurance qualify them for enrollment; it is estimated that over 60% of the mothers are Mexican immigrants.
We used a convenience sample of mothers of infants within these two clinics. Women were included as participants if they (a) were enrolled as an infant’s mother at one of the clinics, (b) had an infant aged 0 to 12 months, (c) were 18 years of age or older, (d) could speak English or Spanish, and (e) expressed a willingness to participate in the study.
Procedures.
After obtaining the participants’ informed consent, data collection occurred by face-to-face interviews at the time of the participants’ baby visits. Interviews were conducted in English or Spanish, depending on mothers’ preferences, and administered by bilingual research assistants (RAs). Each survey took approximately 30 minutes to complete, including the consent form. All surveys were administered at the clinics where the participants were enrolled, and these clinics provided a private space for the interviews. This study was approved by the Institutional Review Board of the University of Texas at Austin and all participants provided written informed consent.
Measures.
All measures were available in both English and Spanish versions.
Demographic characteristics.
Information regarding individual characteristics including maternal age, race/ethnicity, education level, household income, number of children, marital status, and language fluency were obtained from participants. Infant characteristics regarding age (months) and immunization status were obtained from the medical record.
Maternal health literacy.
The Newest Vital Sign (NVS), in either English (NVS-E) or Spanish (NVS-S), was used to assess maternal health literacy. The NVS assesses quantitative literacy, prose literacy, and document literacy.24 The NVS contains an ice cream nutrition label, which participants use to answer six questions regarding information on the label. The summed scores can range from 0 to 6, and the questions should be scored as correct or incorrect. In the present study, NVS scores were categorized into low (0 to 3 questions correct, a high likelihood of limited health literacy or possibility of limited health literacy) and adequate (4 to 6 questions correct, adequate health literacy) health literacy categories.24 The NVS has shown evidence of validity and reliability in English as well as in Spanish among parents with young children. In this study, Cronbach’s alpha was 0.716.
Parenting self-efficacy.
The Karitane Parenting Confidence Scale (KPCS)25 was used for measuring mothers’ perceived parenting self-efficacy. The KPCS is a validated task-specific 15-item scale, and it was designed to measure perceived parenting efficacy in parents of infants aged 0–12 months.25 The KPCS uses a four-point scale (0–3), with higher scores indicating higher levels of parenting self-efficacy. The sum scores of the KPCS range from 0 to 45.25 The KPCS has been used to assess mothers of infants in previous studies and has been shown to have acceptable reliability.26–28 The Cronbach’s alpha for this study was .889.
Social support.
The Postpartum Social Support Scale (PSSS) was used to measure social support. The PSSS was developed by Walker26 to measure the context of caring for an infant during the postpartum period.27,28 It includes six items—three related to instrumental support and three related to emotional support. Items on the PSSS are answered on a nine-point Likert scale, ranging from 1 (not at all) to 9 (completely). The sum scores of the PSSS range from 6 to 42, with higher scores indicating greater social support. The Cronbach’s alpha coefficient for this study was .894.
Early parenting practices.
Early parenting practices were measured by the Early Parenting Practices Index (EPPI)29 with 12 parenting practices, grouped into four domains, being studied (Table 1). The four domains of early parenting practices (safety, feeding, development promotion, and health care utilization) were selected based on evidence from previous studies of their importance and appropriateness for the health and development of infants from birth to 12 months old.29,30 There is agreement in the literature that parenting practices have an important effect on children’s outcomes, but there is no agreement regarding the conceptualization of the definition and the appropriate measurement tool.29,31 To our knowledge, no scale has been used for early parenting practices; thus, the developed index was used to measure early parenting practices among mothers with infants.
Table 1.
EARLY PARENTING PRACTICES INDEX AND ASSOCIATED SURVEY QUESTIONS
| Domain and Practices | Questions | Answers Qualifying as Adherent |
|---|---|---|
| Safety Practices | ||
| Sleeping position | In what position do you usually put your baby down to sleep? On his or her side, back, or stomach? | Back |
| Sleeping bed | Does your baby sleep in the same room as you? If yes, does your baby sleep in the same bed with you? | Same room but not in the same bed |
| Car seat use | In the last 30 days, how many times has your baby been in a moving car or vehicle without being strapped in the car seat even for a brief moment? | 0 |
| Car seat position | How do you position your baby’s car seat? Front-facing or backward-facing? | Backward-facing |
| Fire safety | Do you have a working smoke detector in your home? | Yes |
| Smoking | Do you smoke inside your home? | No |
| Feeding Practice | ||
| Feeding | How are you feeding your baby? 0–5.99 months 6–12 months | Exclusively breast-feed Introduction of food |
| Development Promotion | ||
| Practices | ||
| Playing | Do you play daily with your baby? | Always, sometimes |
| Talking | Do you talk daily to your baby? | Always, sometimes |
| Follow routines | Do you try to keep a regular schedule for when your baby eats, naps, and goes to bed at night? | Always, sometimes |
| Tummy time | Does your baby practice tummy time each day? | Always, sometimes |
| Health Care Utilization Practice | ||
| Immunization | Obtained from medical records | Fully immunized |
The 12 early parenting practices included in this study were selected based on literature from the American Academy of Pediatrics (AAP), the Centers for Disease Control and Prevention (CDC), The Injury Prevention Program (TIPP), and a detailed literature review. Adherent behavior was coded as 1; non-adherent behavior was coded as 0. The summed score of each parenting practice and an overall summed score were also used, with higher scores indicating that parents exhibited greater adherence to recommended early parenting practices.
Safety practices.
As identified by the CDC, unintentional injury and sleep-related accidents are among the top five reasons for death among infants younger than one year old. For this reason, six safety practices are included. Two items addressed safe sleeping practices: putting babies to sleep on their backs and bed-sharing. Other items included the use of a car seat, properly securing the baby in a backward-facing car seat, presence of a smoke detector in the home, and the avoidance of smoking in the home.
Feeding practice.
One feeding practice (regarding breastfeeding) is included in this study. To measure breastfeeding practices, the infants were divided into two groups based on their ages: 0 to 5.99 months, and 6 to 12 months. We were particularly interested in exclusive breastfeeding practices among mothers with infants in the first group (0 to 5.99 months old infant).
Development promotion practices.
Four child development promotion daily practices were included: parent play with the child, talking to child, following three daily routines (naptime, bedtime, and meals), and practicing tummy time (supervised intervals of time when a non-sleeping infant is placed in a prone position).
Health care utilization.
As the most important indicator of adequate health care utilization for this group of mothers, the immunization records of each infant were used. Through chart review, fully administered scheduled immunizations were categorized as adherent; some but not all vaccines, or no vaccines, having been administered was categorized as non-adherent.32
The immunization schedule in the clinics follows the CDC’s recommended immunization schedule.32 The CDC’s age-based recommendations include the following vaccinations: three doses of vaccine for hepatitis B, two doses for diphtheria/tetanus/acellular pertussis (DTaP), three doses for haemophilus influenza type B (Hib), three doses of inactivated polio vaccine, four doses of pneumococcal vaccine, and two doses for rotavirus.
Data analysis.
We compared sample characteristics using χ2 statistics for categorical variables and independent t-tests for continuous variables. Correlations among maternal health literacy, individual characteristics, and major variables were calculated using Pearson correlation coefficients (or Spearman’s rho coefficients). To determine group differences in maternal health literacy (low and adequate) and each early parenting practice (adherent and non-adherent), the chi-square test (or Fisher’s exact test) was used. The likelihood ratio chi-square was also used to assess whether statistical differences occurred between race/ethnicity (three groups) and each early parenting practice (two groups). Persons of “other” racial groups (n = 10, including Asian, Arabian, and other races/ethnicities) were excluded because of a lack of adequate numbers for analysis.
In order to examine whether parenting self-efficacy mediates the relationship between maternal health literacy and early parenting practices, regression-based mediation analyses estimating all paths were performed by employing a PROCESS from Hayes,33 and bootstrapping procedures were used to obtain estimates of the indirect effects. The bootstrapped confidence interval of the point estimate of the indirect effect through the procedure has the advantage of being independent from distributional assumptions regarding the parameter estimates for the indirect path. This study used 5,000 bootstrap samples.
Results
Characteristics of the sample and study variables.
One hundred eighty-six low-income mothers with infants participated in this study (Table 2). Their mean age was 29.0 years (SD = 6.02), with a range of 18 to 44. The majority of the mothers were Hispanic (73.7%); 11.8% were White, 9.1% were Black, and 5.4% were Asian or other ethnicity. Over one-third (35.3%) of mothers did not graduate from high school and two thirds of mothers (69.9%) reported an annual household income below $20,000. Nearly three-fourths (73.4%) of mothers had two or more children, 75.8% of mothers were married or had a partner, and about two thirds of mothers (69.9%) were not born in the United States. Regarding English fluency, 48.4% of mothers reported an inability to speak English well (Table 2).
Table 2.
CHARACTERISTICS OF PARTICIPANTS AND MAJOR VARIABLES BY MATERNAL HEALTH LITERACY LEVEL (N=186)
| Maternal Health Literacy |
||||
|---|---|---|---|---|
| Characteristics | n (%) or M ± SD | Low (score 0–3) n = 134 | Adequate (score 4–6) n = 52 | χ2 or tb |
| Age in yearsa | 29.0±6.02 (18–44) | |||
| 18 to 34 | 136 (76.3) | 96 (74.4) | 40 (78.4) | .32 |
| ≥ 35 | 44 (23.7) | 33 (25.6) | 11 (21.6) | |
| Race/Ethnicity | ||||
| White, non-Hispanic | 22 (11.8) | 11 (8.2) | 11 (21.2) | 14.62** |
| Black, non-Hispanic or Other | 27 (14.5) | 14 (10.4) | 13 (25.0) | |
| Hispanic | 137 (73.7) | 109 (81.3) | 28 (53.8) | |
| Educationa | ||||
| High school/GED education or less | 65 (35.3) | 55 (41.7) | 10 (19.2) | 8.22** |
| At least some college | 119 (64.0) | 77 (58.3) | 42 (80.8) | |
| Number of Children at Home a | ||||
| One child | 49 (26.6) | 28 (21.2) | 21 (40.4) | 7.02** |
| Two or more children | 135 (73.4) | 104 (78.8) | 31 (59.6) | |
| Household Income a | ||||
| Less than $20,000 | 95 (69.9) | 70 (73.7) | 25 (26.3) | 9.47** |
| $20,001d–$40,000 | 41 (30.1) | 19 (46.8) | 22 (21.3) | |
| Marital Status a | ||||
| Single/divorced | 45 (24.2) | 12 (23.1) | 33 (24.6) | .05 |
| Married/partnered | 141 (75.8) | 40 (76.9) | 101 (75.4) | |
| At Home, Speak a Language besides | ||||
| Englisha | ||||
| Never, once in a while, sometimes | 95 (51.1) | 61 (45.9) | 27 (51.9) | .51 |
| Always/more than half the time | 90 (48.4) | 72 (54.1) | 25 (48.1) | |
| Social Support (Score Range: 9–54) | 46.96 ± 9.49 | 44.91 ± 10.43 | 48.15 ± 6.41 | 2.56* |
| Parenting Self–Efficacy (Score Range: 0–45) | 39.69 ± 5.93 | 38.94 ± 6.67 | 41.51 ± 2.85 | 3.56** |
| Early Parenting Practices (Score Range: 0–12) | 9.32 ± 1.00 | 9.25 ± 0.97 | 9.49 ± 1.08 | 2.25 |
Notes
One or more cases with missing data
p-value for x2 or t-test
p < .05
p < .01
The total mean score for the NVS was 2.47 (SD = 1.71) out of 6. The NVS revealed that 72.0% of the mothers had low health literacy (33.3% had high likelihood of limited literacy, 38.7% had possible limited literacy), and 28.0% had adequate health literacy (4–6).
There were significant differences in race/ethnicity, education, household income, number of children, country of birth, and English fluency by low and adequate maternal health literacy level. Concerning education, 77 mothers who reported at least some college had low health literacy. Mothers with adequate health literacy had better social support and parenting self-efficacy compared with mothers with inadequate health literacy (Table 2).
Bivariate correlations among the main study variables are presented in Table 3. Maternal health literacy showed a significant positive relationship with education (r = .33, p < .01), household income (r = .26, p < .01), English speaking (r = .45, p < .01), social support (r = .19, p < .01), parenting self-efficacy (r = .28, p < .01), and early parenting practices (r = .18, p < .05). Maternal health literacy exhibited a negative relationship with number of children (r = −.23, p < .01).
Table 3.
CORRELATIONS AMONG INDIVIDUAL CHARACTERISTICS, MAJOR VARIABLES, AND MATERNAL HEALTH LITERACY
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Maternal Health Literacy | 1 | ||||||||
| Age | −.08 | 1 | |||||||
| Education | .33** | −.09 | 1 | ||||||
| Number of Children | .23** | .54** | −.37** | 1 | |||||
| Household Income | .27** | .07 | .29** | −.11 | 1 | ||||
| Language | .01 | −.04 | .05 | −.02** | −.06 | 1 | |||
| Social Support | .19** | −.01 | −.08 | .01 | .17 | −.08 | 1 | ||
| Parenting Self-Efficacy | .28** | .06 | .12 | .04 | .19* | −.12 | .28** | 1 | |
| Early Parenting Practices | .18* | .02 | .08 | .04 | .11 | −.02 | .07 | .25** | 1 |
Notes
p < .05
p < .01
Regarding safety practices, 16.1% of mothers reported ever placing their babies in prone or side positions to sleep, 51.8% reported ever sleeping with the baby in the same bed, 3.9% reported not using a car seat, 2.7% reported ever putting the baby in a front-facing car seat, 9.1% reported not having a smoke detector at home, and 1.1% reported smoking at home (Table 4). The adherence rate of feeding practices was as follows: breast-fed, 43.3% (babies younger than six months); introduction of solid food, 45.8% (babies six months and older). The area of development practices contains four items, and the proportions of mothers who adhere to them are as follows: play with baby, 95.7%; talk to baby at home, 98%; try to keep a regular time for when baby eats and sleeps, 94.1%; try to practice tummy time, 82.6%. The status of up-to-date immunizations at the time of the survey was used to measure health care service utilization practice. Notably, 94.6% of mothers had fully followed the immunization schedule.
Table 4.
EARLY PARENTING PRACTICES BY MATERNAL HEALTH LITERACY AND RACE/ETHNICITY (N=186)
| Maternal Health Literacy |
Race/Ethnicity |
|||||||
|---|---|---|---|---|---|---|---|---|
| Domain and Early Parenting Practices | Adherent n (%) | Low (score 0–3) (n = 134) | Adequate (score 4–6) (n = 52) | p-value | White, non-Hispanic (n = 22) | Black, non-Hispanic (n = 17) | Hispanic (n = 137) | χ2 |
| Safety Practices | ||||||||
| Put babies to sleep on their backs | 156 (83.9) | 109 (81.3) | 47 (90.4) | .13 | 21 (95.5) | 15 (88.2) | 110 (80.3) | .12b |
| Avoid sleeping with baby in the same bed | 82 (48.2) | 63 (51.6) | 19 (39.6) | .16 | 8 (40.0) | 8 (50.0) | 60 (48.0) | .78 |
| Use car seat | 171 (96.1) | 123 (95.3) | 48 (98.0) | .68a | 20 (95.2) | 15 (88.2) | 126 (96.9) | .35b |
| Put baby in backward-facing car seat | 181 (97.3) | 130 (97.0) | 51 (98.1) | 1.00a | 22 (100) | 16 (94.1) | 134 (97.8) | .43b |
| Smoke detector at home | 169 (90.9) | 119 (88.8) | 50 (96.2) | .16a | 19 (86.4) | 15 (88.2) | 125 (91.2) | .75b |
| Avoid smoking in home | 183 (98.9) | 131 (98.5) | 52 (100) | 1.00 a | 22 (100) | 17 (100) | 134 (98.5) | .60b |
| Feeding Practice | 80 (44.0) | 53 (40.5) | 27 (52.9) | .13 | 10 (45.5) | 9 (52.9) | 56 (42.1) | .69 |
| Development Promotion Practices | ||||||||
| Play with baby | 176 (97.7) | 126 (95.5) | 50 (96.2) | 1.00 a | 21 (95.5) | 17 (100) | 128 (94.8) | .43a |
| Talk to baby at home | 181 (98.4) | 129 (92.7) | 52 (100) | .56 a | 21 (100) | 17 (100) | 133 (97.8) | .47a |
| Try to keep a regular time for when baby eats, sleeps | 174 (94.5) | 128 (96.2) | 46 (88.5) | .08 a | 18 (81.8)-0.6c | 14 (82.4)-0.5c | 133 (97.8) 0.4c | .004a** |
| Try to practice tummy time | 152 (82.6) | 108 (81.8) | 44 (84.6) | .65 | 18 (81.8) 0.0c | 9 (52.9)-1.3c | 116 (85.9) 0.5c | .011a* |
| Health Care Service Utilization Practices | ||||||||
| Up-to-date immunizations | 176 (94.6) | 126 (94.0) | 50 (96.2) | .73 | 20 (90.9) | 16 (94.1) | 130 (94.9) | .78 |
Notes
Fisher’s exact test
likelihood ratio chi-square value
standardized residual
p < .05
p < .01
No differences were found in mothers’ reports of early parenting practices by maternal health literacy. Two development promotion practices among early parenting practices differed by race/ethnicity. The adherence rate of mothers trying to keep a regular time for when a baby eats and sleeps did differ based on race, χ2(3) = 11.14, p < .05. The standardized residuals demonstrate a higher-than-expected level of adherent practices among Hispanic mothers and a significantly lower-than-expected level among White mothers. The adherence rate of mothers trying to practice tummy time differed based on race, χ2(3) = 9.00, p < .05. The standardized residuals demonstrate a higher-than-expected level of adherent practices among Hispanic mothers and a significantly lower-than-expected level of adherence among African American mothers.
Using the simple mediation model shown in Figure 2, parenting self-efficacy mediated the relationship between maternal health literacy and early parenting practices. The analyses revealed the significant influence of health literacy on early parenting practices (Path C, b = .10, SE = .04, p < .05) and that health literacy was significantly related to parenting self-efficacy (Path A, b = .06, SE = .02, p < .01). Parenting self-efficacy was significantly related to early parenting practices (Path B, b = .05, SE = .19, p < .05). When health literacy was examined as a mediator of early parenting practices, the effect of health literacy was reduced: b = .07, SE = .04, p > .05 (Path C).
Figure 2.
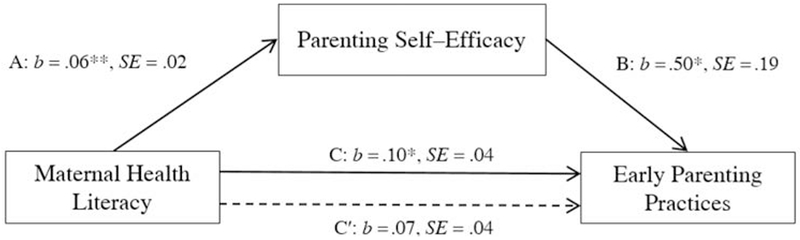
Relationship between maternal health literacy and early parenting practices by parenting self-efficacy.a
Note
a The indirect path was significant (Bias corrected 95% CI .01, .06) (based on 5,000 bootstrap samples, 95% CI do not cross zero). Solid lines represent significant pathways, and dashed lines represent nonsignificant pathways. Variance explained 3%. A=Path A, B=Path B, C=total effect=AB+C’, C’=direct effect.
*p <.05; **p < .01
b= Regression Coefficients; SE= Standard Errors
The indirect effect of health literacy on early parenting practices through parenting self-efficacy was significant, as indicated by the 95% CI (.01, .06) using 5,000 bootstrap estimations (Path AB). The overall model was significant with an adjusted R2 of .03, p < .01.
Discussion
The main finding of this research is consistent with the health literacy literature, in which an ethnic minority status and low education levels have been identified as having a significant correlation with a lower level of health literacy. Throughout the prevailing literature, Hispanic parents have been reported to have lower health literacy levels than their non-Hispanic counterparts6,12,22 and maternal education has been associated with poor health outcomes in children.6,34 Notably, in this study, although the significant correlation of maternal education and health literacy was obtained in bivariate analysis, 77 mothers who reported at least some college education also exhibited limited health literacy. One possible reason for this might be found in their nationality or place of education. Sixty-three mothers with low health literacy and with higher education were not born in the U.S. This study did not determine how long mothers have been living in the U.S., when they came to the U.S., or where they were educated. Based on the findings of this study, even if mothers reported a higher educational level, their health literacy levels should not be assumed to be adequate and should be examined carefully by health care providers. Further study is needed to obtain more information.
While most mothers in our study are implementing recommended safety and development promotion practices well, there are some notable exceptions including the sleeping arrangement of infants and activites promoting development (in safety practice, putting babies to sleep on their backs, and avoiding bed-sharing; in development promotion practice, practicing tummy time). Although it was not statistically significant, there was a trend toward an association between early parenting practices and health literacy. The percentage of mothers who had adequate health literacy was slightly higher than the percentage of mothers who had low health literacy in some recommended parenting practices. For example, mothers who had adequate health literacy tended to put babies to sleep on their backs, breastfeed until six months or introduce food after six months, and try to practice tummy time. In early parenting practices by race/ethnicity, only two infant development promoting practices (following daily routines and practicing tummy time) showed statistically significant differences by racial/ethnic group.
Sleep environment.
Many mothers reported non-adherence to utilizing safe sleeping environments for their infants (putting babies to sleep on their backs and bed-sharing). The results for sleeping position showed no statistically significant differences by health literacy level. However, the low health literacy group demonstrated a higher percentage of non-adherence to back-to-sleep infant positioning recommendations. To date, only one study has investigated the relationship between health literacy and infant sleeping position,13 and its results are consistent with those of the present study.
In the present study, 51.8% of the mothers reported that they had slept with their infants in the same bed. Sudden Infant Death Syndrome (SIDS), can occur when a sleeping infant is suffocated, strangled, or entrapped while in the parent’s bed. While parent-infant bed-sharing continues to be controversial, a recent meta-analysis of 11 studies that investigated the association between bed-sharing and SIDS revealed 2.88 times greater SIDS risk with bed-sharing than with infants who were not sharing the bed with their parents.34 In a 2016 policy statement published by the American Academy of Pediatrics (AAP), it is recommended that infants up to one year of age sleep on a separate sleeping surface from their parents (a standard or portable crib, bassinet, or playpen) within the same room as their parents. The AAP also identifies the first four months of an infant’s life as the most susceptible period for SIDS.35
As important as the sleep environment is for the prevention of SIDS, the positioning of an infant supine for every sleep until one year of age has been shown to be the most important AAP recommendation contributing to the dramatic decline in SIDS rates over the last 30 years. Positioning an infant in any position other than supine (prone, side-lying, seated in a car seat) for sleep places the infant at an increased risk of SIDS. In the present study, 16.1% of mothers reported a lack of consistency in positioning their infant supine for sleep.
Black and Hispanic mothers in our sample were more likely to report bed-sharing with their infants, although the difference was not large enough to be statistically significant. Other studies have reported that African American infants were more likely to be placed in a prone position by their caregivers.36,37 However, due to the limited variability of education level among the African American mothers in the present study, we were not able to draw a conclusion about whether or not it is purely a cultural issue or the result of less education. Previous studies related to bed-sharing have shown that African American and Latino American parents are more likely than others to share the bed with their infants.38 Bed-sharing is more common in low-income families and parents living in Southern states compared with those living in the Midwest and the West.38 The present study did not reveal a significant relationship between sleep practices and health literacy, but the trends were similar to those seen in previous studies.
Development promotion practices.
The study participants reported high adherence on development promotion practice guidelines such as trying to keep a regular feeding and sleeping time for their babies. Another development activity that has been recommended is tummy time, as noted previously. Tummy time has been recommended by researchers to prevent head deformity, strengthen trunk and neck muscles, and promote motor development among infants.39,40 However, studies of tummy time practice and the relationship with health literacy are limited. Only one study, Yin et al.,12 assessed the relationship between parental health literacy and tummy time by asking for actual tummy time adherence; 66% of parents did not meet the current tummy time recommendation (at least 30 minutes per day) and a caregiver’s low health literacy significantly increased the odds of a parent’s reporting inadequate tummy time.
In our study sample, both development promotion practices differed by race/ethnicity. African American mothers reported less tummy time than did White or Hispanic mothers and reported no regular time for when a baby eats and sleeps. No significant differences were found in development promotion practices by maternal health literacy level. It is plausible that culture influences parenting practices to the same extent as formal education, health literacy, and information-seeking behaviors.
The results of this study also clearly indicate that, while maternal health literacy was associated with early parenting practices, its associations were fully mediated by parenting self-efficacy. Parenting self-efficacy has been identified as one determinant of positive parenting behaviors,20,41 but few studies have tested for mediators of early parenting practices in mothers with infants. Studies that have measured the mediating effects of self-efficacy on health outcomes are controversial, and the literature regarding the relationship between health literacy and self-efficacy is inconsistent. Previous studies’ findings suggest that health literacy influences self-efficacy and self-efficacy influences health outcomes.42 One study found that low health literacy was associated with worse health outcomes, but that relationship was not mediated by self-efficacy.43 One previous study revealed that parenting self-efficacy acted as a mediator among mothers with autistic children as they worked to solve behavior problems.44
This finding complements those of research studies in other fields, especially on parenting, in that self-efficacy was identified as an important variable in understanding the relationship between health literacy and mothers’ parenting practices. For mothers, improving self-efficacy should have a direct impact on improvements in infant health and, equal in importance, safety. Self-efficacy may be improved via knowledge enhancement.45,46 Providing mothers with the necessary skills to obtain, understand, and act upon parenting-related information has the potential to increase their ability to cope with the demands of their infants and ultimately lead to improved infant health outcomes.
Limitations.
The study has some limitations concerning the interpretation of its findings and inferences that can be drawn from them. First, the sampling method was non-probability sampling and participants were recruited from selected low-income outpatient wellness clinics in an FQHC. Thus, the study’s findings may not be generalizable to other populations and regions. Second, to make robust causal inferences, data must be collected longitudinally, which we were unable to do. The result of our path analysis has inference limitations due to the inherent limitation associated with crosssectional data collection. Third, our relatively small sample size and the skewedness of the data regarding health literacy poses some challenges to interpretation. One of the most critical limitations is that we could not separate the effects of culture, education, and health literacy of the mother on certain parenting behaviors.
Conclusion.
Despite a number of limitations, the present study makes several important contributions to the current body of knowledge regarding health literacy among low-income mothers with infants. It provides information about an underserved population of mothers with infants, the role of health literacy, and its relationship with parenting self-efficacy and early parenting practices, which are addressed under the broad domains of safety, feeding, development promotion, and health care utilization.
Further research is warranted to advance knowledge regarding the independent role of health literacy on parenting behaviors and children’s outcomes among low-income mothers and to inform future interventions for this target population.
Acknowledgments
The authors are grateful to study participants and the staff of CommUnityCare Health Centers for their assistance with the research.
Contributor Information
Ju-Young Lee, College of Nursing, The Catholic University of Korea, Seoul, South Korea.
Nicole Murry, School of Nursing, at the University of Texas at Austin.
Jisook Ko, School of Nursing, at the University of Texas at Austin.
Miyong T. Kim, School of Nursing, at the University of Texas at Austin.
References
- 1.Armstrong KL, Fraser JA, Dadds MR, et al. Promoting secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. J Paediatr Child Health. 2000. December;36(6):555–62. 10.1046/j.1440-1754.2000.00591.x PMID: [DOI] [PubMed] [Google Scholar]
- 2.Bornstein M, ed. Handbook of parenting: (vol. 1) children and parenting. Mahwah, NJ: Lawrence Erlbaum Associates, 2002. 10.1207/S15327922PAR0203_04 [DOI] [Google Scholar]
- 3.Ferguson B Health literacy and health disparities: the role they play in maternal and child health. Nurs Womens Health. 2008. August;12(4):286–98. 10.1111/j.1751-486X.2008.00343.x PMID: [DOI] [PubMed] [Google Scholar]
- 4.Kumar D, Sanders L, Perrin EM, et al. Parental understanding of infant health information: health literacy, numeracy, and the Parental Health Literacy Activities Test (PHLAT). Acad Pediatr. 2010. Sep-Oct;10(5):309–16. Epub 2010 Aug 2. 10.1016/j.acap.2010.06.007 PMID: PMCid:PMC2933956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buultjens M, Robinson P, Milgrom J. Online resources for new mothers: opportunities and challenges for perinatal health professionals. J Perinat Educ. 2012. Spring;21(2):99–111. 10.1891/1058-1243.21.2.99 PMID: PMCid:PMC3400244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin HS, Johnson M, Mendelsohn AL, et al. The health literacy of parents in the United States: a nationally representative study. Pediatrics. 2009. November;124 Suppl 3:S289–98. 10.1542/peds.2009-1162E PMID: [DOI] [PubMed] [Google Scholar]
- 7.DeWalt DA, Dilling MH, Rosenthal MS, et al. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007. Jan-Feb;7(1):25–31. 10.1016/j.ambp.2006.10.001 PMID: PMCid:PMC1797805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009. November;124 Suppl 3:S265–74. 10.1542/peds.2009-1162B PMID: [DOI] [PubMed] [Google Scholar]
- 9.Mortensen EL, Michaelsen KF, Sanders SA, et al. The association between duration of breastfeeding and adult intelligence. JAMA. 2002. May 8;287(18):2365–71. 10.1001/jama.287.18.2365 PMID: [DOI] [PubMed] [Google Scholar]
- 10.Sleath BL, Jackson E, Thomas KC, et al. Literacy and perceived barriers to medication taking among homeless mothers and their children. Am J Health Sys Pharm. 2006. February 15;63(4):346–51. 10.2146/ajhp050070 PMID: [DOI] [PubMed] [Google Scholar]
- 11.Yin HS, Dreyer BP, van Schaick L, et al. Randomized controlled trial of a pictogram-based intervention to reduce liquid medication dosing errors and improve adherence among caregivers of young children. Arch Pediatr Adolesc Med. 2008. September;162(9):814–22. 10.1001/archpedi.162.9.814 PMID: [DOI] [PubMed] [Google Scholar]
- 12.Yin HS, Sanders LM, Rothman RL, et al. Parent health literacy and “obesogenic” feeding and physical activity-related infant care behaviors. J Pediatr. 2014. March;164(3):577–83. Epub 2013 Dec 25. 10.1016/j.jpeds.2013.11.014 PMID: PMCid:PMC3943839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heerman WJ, Perrin EM, Yin HS, et al. Health literacy and injury prevention behaviors among caregivers of infants. Am J Prev Med. 2014. May;46(5):449–56. 10.1016/j.amepre.2014.01.005 PMID: PMCid:PMC4040284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahlers-Schmidt CR, Chesser AK, Paschal AM, et al. Parent opinions about use of text messaging for immunization reminders. J Med Internet Res. 2012. June 6;14(3):e83 10.2196/jmir.1976 PMID: PMCid:PMC3415063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaufman H, Skipper B, Small L, et al. Effect of literacy on breast-feeding outcomes. South Med J. 2001. March;94(3):293–6. 10.1097/00007611-200194030-00005https://doi.org/10.1097/00007611-200103000-00005 PMID: [DOI] [PubMed] [Google Scholar]
- 16.Lokker N, Sanders L, Perrin EM, et al. Parental misinterpretations of over-the-counter pediatric cough and cold medication labels. Pediatrics. 2009. June;123(6):1464–71. 10.1542/peds.2008-0854 PMID: PMCid:PMC2911576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bloomfield L, Kendall S, Applin L, et al. A qualitative study exploring the experiences and views of mothers, health visitors and family support centre workers on the challenges and difficulties of parenting. Health Soc Care Community. 2005. January;13(1):46–55. 10.1111/j.1365-2524.2005.00527.x PMID: [DOI] [PubMed] [Google Scholar]
- 18.Hnatiuk JA, Salmon J, Campbell KJ, et al. Tracking of maternal self-efficacy for limiting young children’s television viewing and associations with children’s television viewing time: a longitudinal analysis over 15-months. BMC Public Health. 2015. May 30;15:517 10.1186/s12889-015-1858-3 PMID: PMCid:PMC4448909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verhage ML, Oosterman M, Schuengel C. The linkage between infant negative temperament and parenting self-efficacy: the role of resilience against negative performance feedback. Br J Dev Psychol. 2015. November;33(4):506–18. Epub 2015 Aug 28. 10.1111/bjdp.12113 PMID: [DOI] [PubMed] [Google Scholar]
- 20.Coleman PK, Karraker KH. Self-efficacy and parenting quality: findings and future applications. Dev Rev. 1998. March;18(1):47–85. 10.1006/drev.1997.0448 [DOI] [Google Scholar]
- 21.Easton P, Entwistle VA, Williams B. Health in the ‘hidden population’ of people with low literacy: a systematic review of the literature. BMC Public Health. 2010. August 5;10:459 10.1186/1471-2458-10-459 PMID: PMCid:PMC2923110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fry-Bowers EK, Maliski S, Lewis MA, et al. The association of health literacy, social support, self-efficacy and interpersonal interactions with health care providers in low-income Latina mothers. J Pediatr Nurs. 2014. Jul-Aug;29(4):309–20. Epub 2014 Jan 15. 10.1016/j.pedn.2014.01.006 PMID: PMCid:PMC4062609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007. Sep-Oct;31 Suppl 1:S19–26. 10.5993/AJHB.31.s1.4 PMID: [DOI] [PubMed] [Google Scholar]
- 24.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005. Nov-Dec;3(6):514–22. 10.1370/afm.405 PMID: PMCid:PMC1466931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Črnčec R, Barnett B, Matthey S. Development of an instrument to assess perceived self-efficacy in the parents of infants. Res Nurs Health. 2008. October;31(5):442–53. 10.1002/nur.20271 PMID: [DOI] [PubMed] [Google Scholar]
- 26.Walker LO. Weight and weight-related distress after childbirth: relationships to stress, social support, and depressive symptoms. J Holist Nurs. 1997. December;15(4):389–405. 10.1177/089801019701500406 PMID: [DOI] [PubMed] [Google Scholar]
- 27.Walker LO, Grobe SJ. The construct of thriving in pregnancy and postpartum. Nurs Sci Q. 1999. April;12(2):151–7. 10.1177/089431849901200216 PMID: [DOI] [PubMed] [Google Scholar]
- 28.Walker LO, Sterling BS. The structure of thriving/distress among low-income women at 3 months after giving birth. Fam Community Health. 2007. Jan-Mar;30(1 Suppl):S95-S103. 10.1097/00003727-200701001-00012 PMID: [DOI] [PubMed] [Google Scholar]
- 29.Walker LO, Kirby RS. Conceptual and measurement issues in early parenting practices research: an epidemiologic perspective. Matern Child Health J. 2010. November;14(6):958–70. 10.1007/s10995-009-0532-8 PMID: [DOI] [PubMed] [Google Scholar]
- 30.McLearn KT, Minkovitz CS, Strobino DM, et al. The timing of maternal depressive symptoms and mothers’ parenting practices with young children: implications for pediatric practice. Pediatrics. 2006. July;118(1):e174–82. 10.1542/peds.2005-1551 PMID: [DOI] [PubMed] [Google Scholar]
- 31.Tramonte L, Gauthier AH, Willms JD. Engagement and guidance the effects of maternal parenting practices on children’s development. J Fam Issues. 2015;36(3):396–420. 10.1177/0192513X13489959 [DOI] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC). Immunization schedules: for everyone: easy-to-read formats. Atlanta, GA: CDC, 2016. Available at: https://www.cdc.gov/vaccines/schedules/easy-to-read/. [Google Scholar]
- 33.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach (1st ed.). New York, NY: Guilford Press, 2013. [Google Scholar]
- 34.Vennemann MM, Hense HW, Bajanowski T, et al. Bed-sharing and the risk of sudden infant death syndrome: can we resolve the debate? J Pediatr. 2012. January;160(1):44–8. e2 Epub 2011 Aug 24. 10.1016/j.jpeds.2011.06.052 PMID: [DOI] [PubMed] [Google Scholar]
- 35.Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: updated 2016 recommendations for a safe infant sleeping environment. Pediatrics. 2016. November;138(5). Epub 2016 Oct 24. [DOI] [PubMed] [Google Scholar]
- 36.Sanders LM, Federico S, Klass P, et al. Literacy and child health: a systematic review. Arch Pediatr Adolesc Med. 2009. February;163(2):131–40. 10.1001/archpediatrics.2008.539 PMID: [DOI] [PubMed] [Google Scholar]
- 37.Mathews AA, Joyner BL, Oden RP, et al. Comparison of infant sleep practices in African-American and US Hispanic families: implications for sleep-related infant death. J Immigr Minor Health. 2015. June;17(3):834–42. 10.1007/s10903-014-0016-9 PMID: PMCid:PMC4185304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Willinger M, Ko CW, Hoffman HJ, et al. Trends in infant bed-sharing in the United States, 1993–2000: the National Infant Sleep Position study. Arch Pediatr Adolesce Med. 2003. January;157(1):43–9. 10.1001/archpedi.157.1.43 PMID: [DOI] [PubMed] [Google Scholar]
- 39.Charlton S The importance of tummy time. Every Child J. 2015;21(2):30. [Google Scholar]
- 40.Cummings C Positional plagiocephaly. Paediatr Child Health. 2011. October;16(8):493–6. 10.1093/pch/16.8.493https://doi.org/10.1093/pch/16.8.495 PMID: PMCid:PMC3202394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanders MR, Woolley M. The relationship between maternal self-efficacy and parenting practices: implications for parent training. Child Care Health Dev. 2005. January;31(1):65–73. 10.1111/j.1365-2214.2005.00487.x PMID: [DOI] [PubMed] [Google Scholar]
- 42.Osborn CY, Paasche-Orlow MK, Bailey SC, et al. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011. Jan-Feb;35(1):118–28. 10.5993/AJHB.35.1.11 PMID: PMCid:PMC3085858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011. September;26(9):979–86. Epub 2011 Mar 3. 10.1007/s11606-011-1668-y PMID: PMCid:PMC3157534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hastings RP, Brown T. Behavior problems of children with autism, parental self-efficacy, and mental health. Am J Ment Retard. 2002. May;107(3):222–32. [DOI] [PubMed] [Google Scholar]
- 45.Renz AN, Newton JT. Changing the behavior of patients with periodontitis. Periodontol 2000. 2009;51:252–68. 10.1111/j.1600-0757.2009.00314.x PMID: [DOI] [PubMed] [Google Scholar]
- 46.Stewart JE, Wolfe GR, Maeder L, et al. Changes in dental knowledge and self-efficacy scores following interventions to change oral hygiene behavior. Patient Educ Couns. 1996. April;27(3):269–77. 10.1016/0738-3991(95)00843-8 [DOI] [PubMed] [Google Scholar]


