Abstract
Purinergic signaling may be altered in diabetes accounting for endothelial dysfunction. Uridine adenosine tetraphosphate (Up4A), a novel dinucleotide substance, regulates vascular function via both purinergic P1 and P2 receptors (PR). Up4A enhances vascular contraction in isolated arteries of diabetic rats likely through P2R. However, the precise involvement of PRs in endothelial dysfunction and the vasoconstrictor response to Up4A in diabetes has not been fully elucidated. We tested whether inhibition of PRs improved endothelial function and attenuated Up4A-mediated vascular contraction using both aortas and mesenteric arteries of type 2 diabetic (T2D) Goto Kakizaki (GK) rats vs. control Wistar (WT) rats. Endothelium-dependent (EDR) but not endothelium-independent relaxation was significantly impaired in both aortas and mesenteric arteries from GK vs. WT rats. Non-selective inhibition of P1R or P2R significantly improved EDR in aortas but not mesenteric arteries from GK rats. Inhibition of A1R, P2X7R, or P2Y6R significantly improved EDR in aortas. Vasoconstrictor response to Up4A was enhanced in aortas but not mesenteric arteries of GK vs. WT rats via involvement of A1R and P2X7R but not P2Y6R. Depletion of major endothelial component nitric oxide enhanced Up4A-induced aortic contraction to a similar extent between WT and GK rats. No significant differences in protein levels of A1R, P2X7R, and P2Y6R in aortas from GK and WT rats were observed. These data suggest that altered PR sensitivity accounts for endothelial dysfunction in aortas in diabetes. Modulating PRs may represent a potential therapy for improving endothelial function.
Keywords: purinergic receptors, endothelial dysfunction, Up4A, vascular contraction, diabetes
1. Introduction
Type 2 diabetes (T2D) is an important risk factor for the development of cardiovascular disease including atherosclerosis and ischemic heart disease. Endothelial dysfunction is an early manifestation of the disease progression and plays a major role in the etiology of diabetes-induced macrovascular and microvascular complications [1,2]. The underlying cause of endothelial dysfunction is multifactorial and complex, but some of the key mechanisms include imbalance between endothelium-derived vasodilators such as nitric oxide (NO) and adenosine triphosphate (ATP), and vasoconstrictors such as endothelin, reactive oxygen species, and ATP, as well as receptor-mediated signaling activated by certain endothelium-derived factors, e.g., ATP-activated purinergic signaling [3,4].
Activation of purinergic receptors (PRs) by various extracellular nucleotides and nucleosides play a pivotal role in the control of vascular function. The purinergic receptor family consists of P1R and P2R based on their molecular structures and pharmacological moieties [5,6]. P1R, also named adenosine receptors, are divided into four subtypes: A1R, A2AR, A2BR, and A3R. P2R can be further divided into P2XR and P2YR [4]. To date, seven P2XRs and eight P2YRs have been recognized [4]. Of importance, purinergic signaling has been observed to be altered in both experimental animals and humans with T2D and such alteration may account for the development of endothelial dysfunction [7,8,9,10]. Indeed, ATP- and UTP-induced vascular contraction in mesenteric arteries was increased in rats with T2D, an effect that was attenuated by non-selective P2R inhibition [11]. In addition, the vasodilator response elicited by ATP was decreased in mesenteric arteries from rats with diabetes [12]. Similarly, the vasodilation to ATP, UTP, and adenosine was impaired in femoral arteries of patients with T2D [13]. However, due to a lack of specific antagonists for the most of PRs, the precise role of PRs in control of vascular function, in particular the contribution of those PRs to the development of endothelial dysfunction in T2D, remains to be determined.
A novel dinucleotide, uridine adenosine tetraphosphate (Up4A), was initially identified as an endothelium-derived vasoconstrictor, exerting its vasoconstrictor influence via both P1R and P2R in various vascular beds [14,15,16,17,18,19]. The vasoconstriction was shown to involve the generation of thromboxane (TxA2) [16] and reactive oxygen species (ROS) [18]. Of note, Up4A-induced contraction mediated by P2R was increased in renal arteries from type 2 diabetic Goto-Kakizaki (GK) rats [10]. Up4A-induced renal contraction was increased in Otsuka Long-Evans Tokushima Fatty (OLETF) T2D rats with age and duration of diabetes [9]. Our recent studies further revealed an altered purinergic signaling in response to Up4A in coronary microcirculation from diabetic swine [8]. Collectively, these observations support the notion that vascular purinergic singling is altered in diabetes.
The aim of our study was therefore to investigate the role of PRs in the regulation of endothelial function. We evaluated endothelial function based on acetylcholine (ACh)-induced endothelium-dependent relaxation (EDR) and used Up4A as pharmacological stimulator for purinergic activation in both conduit and resistance arteries (aortas and mesenteric arteries) from GK rats. Meanwhile, we used both the non-selective P1R and P2R antagonists as well as the specific antagonists available against A1R, P2X7R, and P2Y6R to identify the putative PRs that accounts for endothelial dysfunction in T2D.
2. Results
2.1. Characterization of Endothelial Function in Diabetic Rats
At the time of the experiment, GK rats had higher blood glucose compared to Wistar (WT) rats (10.8 ± 0.6 mmol/L in GK vs. 4.4 ± 0.2 mmol/L in WT, p < 0.001), but lower body weight (356 ± 5 g in GK vs. 481 ± 11 g in WT, p < 0.001).
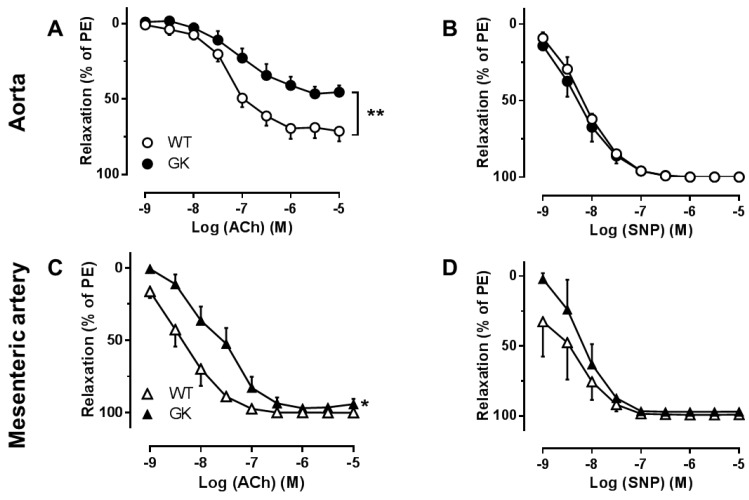
To determine endothelial function in both conduit and resistant arteries, ACh-induced EDR and sodium nitroprusside (SNP)-induced endothelium-independent relaxations (EIR) were conducted in aortas and mesenteric arteries preconstricted with phenylephrine (PE) from WT and GK rats. EDR (Figure 1A,C) but not EIR (Figure 1B,D) was significantly impaired in both aortas and mesenteric arteries isolated from GK rats as compared to WT rats (−logEC50: 8.4 ± 2.5 in WT mesenteric arteries; 7.7 ± 3.2 in GK mesenteric arteries, p < 0.05), indicating endothelial dysfunction in GK rats.
Figure 1.
Concentration-response curve for acetylcholine (ACh) (A, n = 10–18), representing endothelium-dependent relaxation (EDR) or sodium nitroprusside (SNP), representing endothelium-independent relaxation (EIDR) (B, n = 3–4) in aortas isolated from Wistar (WT) and Goto-Kakizaki (GK) rats. EDR (C, n = 8–10) as well as EIR (D, n = 3) were also evaluated in mesenteric arteries from WT and GK rats. Data are presented as mean ± SEM as percentage relaxation of PE. * p < 0.05, ** p < 0.01, calculated with two-way ANOVA.
2.2. Effects of the Non-Specific P1R and P2R Antagonists on Endothelial Function in Aortas and Mesenteric Arteries
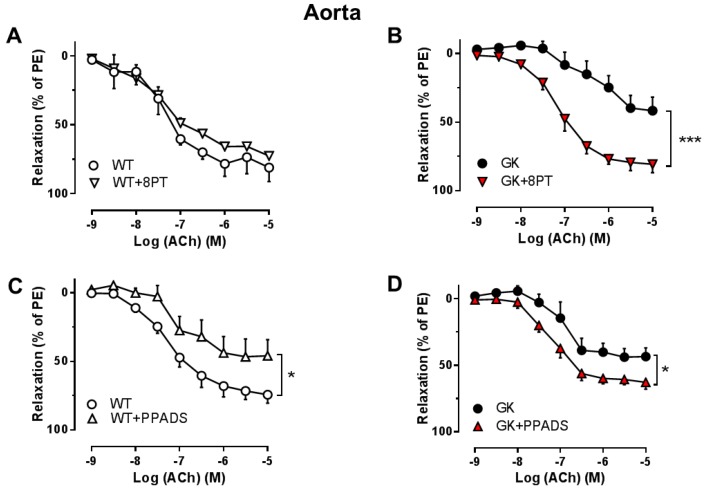
We investigated the effect of non-selective P1R and P2R inhibition on EDR in aortas and mesenteric arteries isolated from WT and GK rats. The non-selective P1R antagonist 8PT markedly improved EDR in GK aortas (Figure 2B), but had no effect on EDR in WT aortas (Figure 2A). Moreover, the non-selective P2R antagonist PPADS improved EDR in GK aortas (Figure 2D) but impaired EDR in WT aortas (Figure 2C). In contrast, neither 8PT (Figure 3A,B) nor PPADS (Figure 3C,D) affected EDR in mesenteric arteries from WT and GK rats. These observations indicate that involvement of PRs is altered contributing to endothelial dysfunction in conduit, but unlikely in resistance arteries in T2D.
Figure 2.
Effects of the P1R and P2R antagonists on EDR in aortas from WT and GK rats. Concentration-response curves for acetylcholine (ACh) in aortas preconstricted with PE in the absence and presence of the non-selective P1R antagonist (8PT, 10−5 M) from WT (A, n = 3) or GK (B, n = 6). Concentration-response curves for ACh in aortas preconstricted with PE in the absence and presence of the non-selective P2R antagonist (PPADS, 10−5 M) from WT (C, n = 5) or GK (D, n = 5). Data are presented as mean ± SEM as percentage relaxation of PE. * p < 0.05, *** p < 0.001, calculated with two-way ANOVA.
Figure 3.
Effects of P1R and P2R antagonists on EDR in mesenteric arteries from WT and GK rats. Concentration-response curves for acetylcholine (ACh) in mesenteric arteries preconstricted with PE in the absence and presence of the non-selective P1R antagonist (8PT, 10−5 M) from WT (A, n = 3) or GK (B, n = 4). Concentration-response curves for ACh in mesenteric arteries preconstricted with PE in the absence and presence of the non-selective P2R antagonist (PPADS, 10−5 M) from WT (C, n = 3) or GK (D, n = 4). Data are presented as mean ± SEM as percentage relaxation of PE. No significant differences were detected with two-way ANOVA.
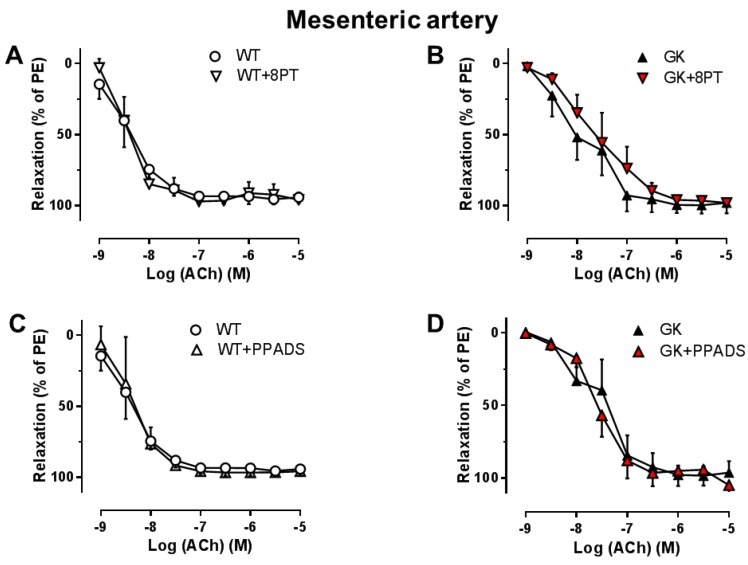
2.3. Effects of the Specific Antagonists for A1R, P2X7R, and P2Y6R on Endothelial Function in Aortas
Since both P1 and P2 inhibition affected endothelial function in aortas, but not mesenteric arteries, we further investigated involvement of specific PRs in endothelial function in aortas. A1R inhibition with DPCPX, P2X7R inhibition with A438079, and P2Y6R inhibition with MRS2578 significantly improved EDR in aortas from GK rats (Figure 4D–F), but had no effect on EDR in aortas from WT rats (Figure 4A–C).
Figure 4.
Effects of specific antagonism for A1R, P2X7R, and P2Y6R on EDR in aortas. Concentration–response curves for acetylcholine (ACh) in aortas preconstricted with PE in the absence and presence of the A1R antagonist (DPCPX, 10−8 M) (A, WT n = 3; D, GK n = 7), the P2X7R antagonist (A438079, 10−5 M) (B, WT n = 4; E, GK n = 10), and the P2Y6R antagonist (MRS2578, 10−5 M) (C, WT n = 3; F, GK n = 8). Data are presented as mean ± SEM as percentage relaxation of PE. * p < 0.05 calculated with two-way ANOVA.
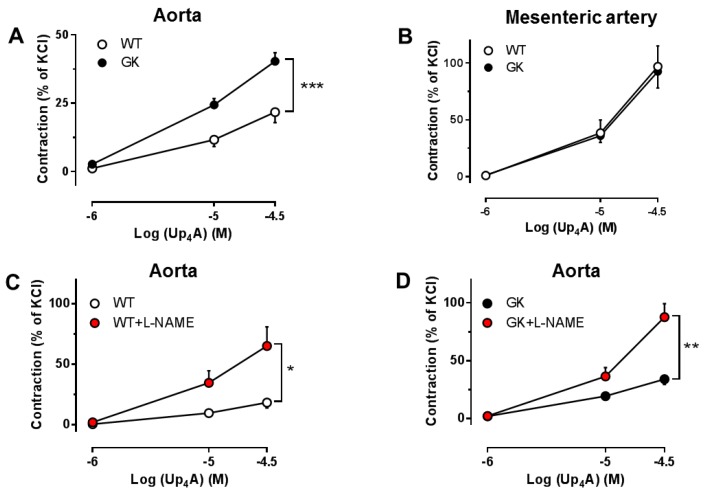
2.4. Effects of Up4A on Vascular Function in Aortas and Mesenteric Arteries
Since we observed an altered endothelial function in aortas and mesenteric arteries from T2D animals, we next applied a novel dinucleotide Up4A to stimulate PRs in aortas and mesenteric arteries from WT and GK rats. Up4A produced more potent contraction in mesenteric arteries than in aortas of WT rats (Figure 5). The vasoconstrictor response was markedly enhanced in aortas (Figure 5A), but not mesenteric arteries (Figure 5B) from GK as compared to WT rats. These observations again support that involvement of PRs is altered in aortas in T2D. Interestingly, NO synthase inhibition with N(G)-Nitro-L-arginine methyl ester (L-NAME) significantly enhanced Up4A-induced contraction in aortas in both WT and GK rats (Figure 5C,D). The effect of L-NAME on Up4A-induced contraction was similar in WT and GK groups (Δ area under the curve: 30 ± 8 in WT and 29 ± 6 in GK rats).
Figure 5.
Vasoconstrictor response to Up4A at baseline in arteries from WT and GK rats. Comparison of concentration response curves to cumulative application of Up4A in aortas (A, WT n = 18, GK n = 32) or mesenteric arteries (B, WT n = 7, GK n = 8) between WT and GK rats. Effects of nitric oxide synthase inhibitor L-NAME on Up4A-induced contraction in aortas of WT and GK rats (C, WT n = 5; D, GK n = 9). Data are presented as mean ± SEM as percentage contraction of KCl. * p < 0.05; ** p < 0.01; *** p < 0.001, calculated with two-way ANOVA.
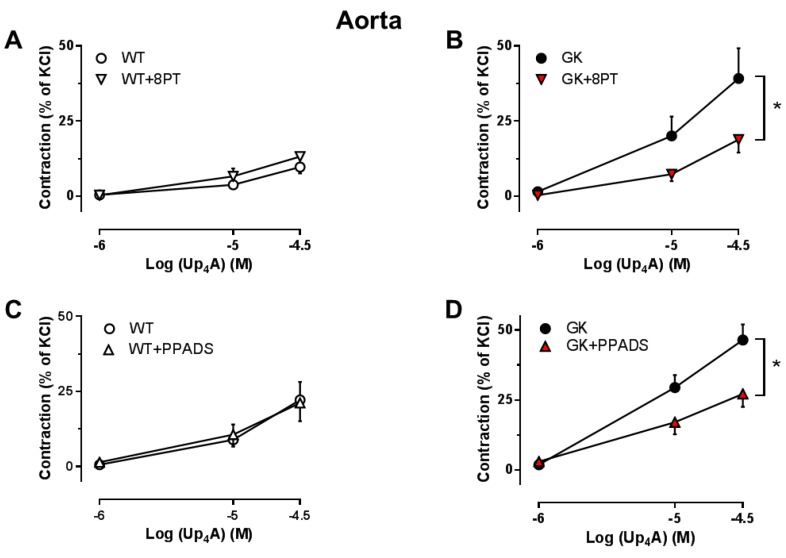
2.5. Effects of the Non-Specific P1R and P2R Antagonists on Up4A-Mediated Vascular Contraction in Aortas
Both the non-selective P1R antagonist 8PT and the non-selective P2R antagonist PPADS significantly attenuated the vasoconstrictor response to Up4A in aortas from GK rats (Figure 6B,D), but did not affect Up4A-mediated vascular contraction in aortas from WT rats (Figure 6A,C). This indicates that Up4A-enhanced aortic contraction in GK rats is attributable to activation of both P1Rs and P2Rs.
Figure 6.
Effects of the P1R and P2R antagonists on vasoconstrictor response to Up4A in aortas from WT and GK rats. Concentration response curves for Up4A in aortas in the absence and presence of the non-selective P1R antagonist (8PT, 10−5 M) (A, WT n = 3; B, GK n = 8) and the non-selective P2R antagonist (PPADS, 10−5 M) (C, WT n = 4; D, GK n = 6). Data are presented as mean ± SEM as percentage contraction of KCl. * p < 0.05, calculated with two-way ANOVA.
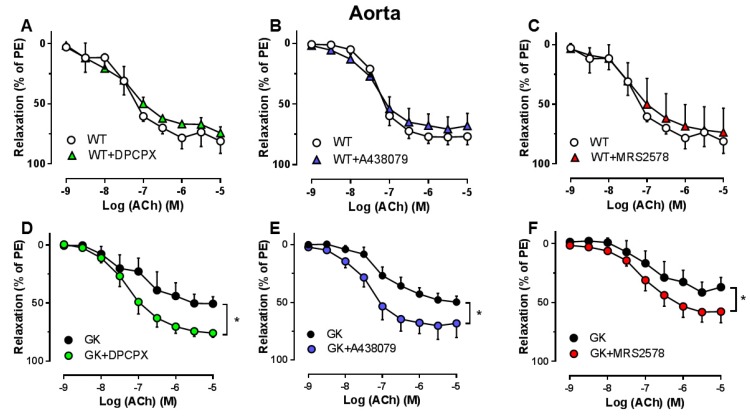
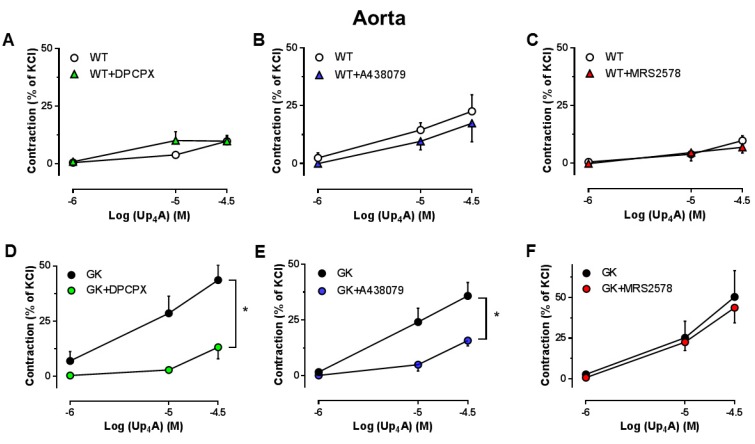
2.6. Effects of the Specific Antagonists for A1R, P2X7R and P2Y6R on Up4A-Mediated Vascular Contraction in Aortas
We next investigated the specific subtype(s) of PRs involved in the vasoconstrictor response to Up4A. A1R inhibition with DPCPX, P2X7R inhibition with A438079 but not P2Y6R inhibition with MRS2578 significantly attenuated the Up4A response in aortas from GK rats (Figure 7D–F). None of the antagonists affected the vasoconstrictor response to Up4A in aortas from WT rats (Figure 7A–C).
Figure 7.
Effects of specific antagonism for A1R, P2X7R, and P2Y6R on vasoconstrictor response to Up4A in aortas from WT and GK rats. Concentration response curves for Up4A in aortas in the absence and presence of the A1R antagonist (DPCPX, 10−8 M) (A, WT n = 3; D, GK n = 4), the P2X7R antagonist (A438079, 10−5 M) (B, WT n = 6; E, GK n = 6), and the selective P2Y6R antagonist (MRS2578, 10−5 M) (C, WT n = 3; F, GK n = 4). Data are presented as mean ± SEM as percentage contraction of KCl. * p < 0.05 calculated with two-way ANOVA.
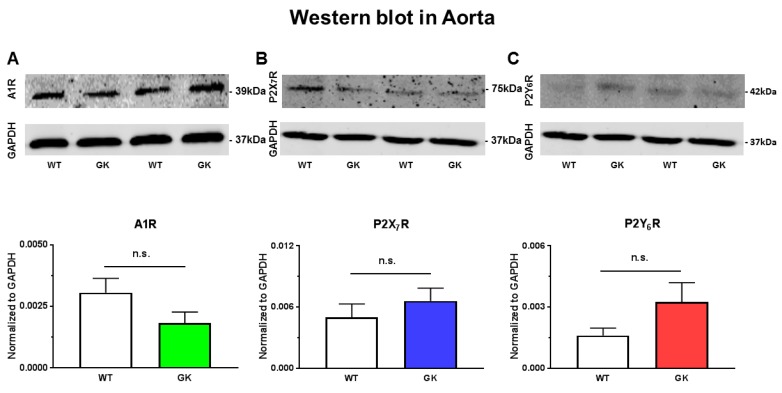
2.7. Protein Expression of A1R, P2X7R, and P2Y6R in Aortas from WT and GK Rats
An alteration in the expression of PRs in aortas could conceivably underlie the impaired endothelial function as well as the enhanced Up4A-mediated vasoconstrictor response in GK rats. We therefore determined the protein levels of A1R, P2X7R, and P2Y6R. No significant alterations in A1R (Figure 8A), P2X7R (Figure 8B), and P2Y6R (Figure 8C) were detected in aortas from GK rats as compared to WT rats.
Figure 8.
Protein expression of the A1R (A), P2X7R (B), and P2Y6R (C) in aortas from WT (n = 6) and GK rats (n = 8). Data are presented as mean ± SEM; n.s: not statistically significant with unpaired Student’s t-test.
3. Discussion
The main findings of the present study are that (1) endothelial dysfunction in aortas, but not mesenteric arteries of T2D rats was attenuated by the non-selective P1R and P2R antagonists; (2) the endothelial dysfunction in aortas was attributable to activation of A1R, P2X7R, and P2Y6R; (3) the vasoconstrictor responses to Up4A was enhanced in aortas, but not mesenteric arteries from T2D rats; (4) this enhancement in aortas was attenuated by the non-selective P1R and P2R antagonists as well as the specific antagonists for A1R and P2X7R, but was not affected by the P2Y6R antagonist; and (5) protein expression of A1R, P2X7R, and P2Y6R was unaltered in aortas from T2D rats. These results indicate that altered PR sensitivity is an important mechanism underlying endothelial dysfunction in aortas of T2D animals.
Endothelial dysfunction represents an early manifestation in vascular complications associated with diabetes and is well established in both patients and rodent models with T2D [20,21,22,23]. In accordance with previous studies, there is endothelial dysfunction in both conduit and resistance arteries in spontaneously developed T2D of non-obese GK rats [24,25].
Activation of PRs by various nucleot(s)ides plays a pivotal role in the control of vascular function [4]. Of note, endogenous nucleotides and nucleoside or their nucleotidases are altered in diabetes [26], which may affect the sensitivity of PRs on vasculature in response to pharmacological stimulations [7,8,9,10,27]. In the present study, PR sensitivity seems to be altered in conduit, but not resistance arteries, as evidenced by that non-selective inhibition for P1Rs and P2Rs with 8PT and PPADS at concentrations of 10 µM improved endothelial function in aortas, but not mesenteric arteries from GK rats. Similarly, contractions of aortas but not mesenteric arteries from GK rats were enhanced by Up4A which activates P1Rs, most P2XRs and P2YRs [8,15,28], and the enhancement in aortas by Up4A was attenuated by both P1R and P2R inhibition. This is supported by the observation that adenosine-mediated purinergic signaling is altered in aortas, but not mesenteric arteries of a diabetic mouse model [29]. In contrast, using purines as stimulators, both ATP (activates most of P2XRs and possibly P2Y1R) [30] and UTP (activates P2Y2R and P2Y4R) [30] enhanced contractions of mesenteric arteries of GK rats, an effect that was attenuated by non-selective P2R inhibition [11]. The discrepancy regarding the alteration of purinergic signaling in mesenteric arteries may be due to the age of animal used (15–18 weeks in the present study vs. 37-42 weeks in the study mentioned above). The altered purinergic activation likely appears when the vasoconstrictor response to purine stimulation e.g., ATP wanes in mesenteric arteries of older healthy rats but is maintained in aged GK rats [31]. Future studies are needed to confirm such explanations. The altered PR sensitivity in aortas from GK rats likely presents at endothelial level, as inhibition of NO, the major endothelial component, enhanced Up4A-induced contraction to a similar extent between WT and GK rats. Interestingly, the non-selective P2R antagonist PPADS at 10 µM significantly attenuated EDR in aortas from WT rats. Activation of P2X1R; P2X2R; and possibly also P2X3R, P2X4R P2X7R, P2Y1R, P2Y2R, P2Y4R, and P2Y11R on endothelial cells has been shown to produce NO and prostacyclin with subsequent vasodilation [32]. Given the ability of PPADS at concentration of 10 µM to inhibit most of P2XRs mentioned above [33], PPADS appeared to inhibit some of those vasodilator PRs resulting in an impaired EDR in aortas from WT rats [16]. These observations also indicate that there is likely a shift from the vasodilator P2Rs to vasoconstrictor P2Rs in diabetes.
We further investigated the involvement of PR subtypes in vascular function in aortas of T2D animals. A1R inhibition with DPCPX significantly improved endothelial function in GK rats. Using Up4A as stimulator, the increased contraction was attenuated by DPCPX in GK rats, despite an unaltered A1R expression. These findings suggest that A1R sensitivity is altered involving in endothelial dysfunction in T2D. A1R is expressed in the vasculature and activation of A1R typically results in vascular contraction [34]. The A1R-mediated contraction in aortas has been observed to be reduced in a diabetic mouse model without obvious endothelial dysfunction [29]. The decreased A1R activation is due to a compensatory mechanism to counterbalance the increased adrenergic vascular contraction [29]. In addition to A1R, activation of A3R typically produces vasoconstriction [34]. However, the evidence that the selective A3R agonist did not affect vascular function in aortas of mice with diabetes [29] and Up4A-mediated aortic contraction is not altered in A3R knock-out mice [16] suggests that A3R is unlikely to be involved in endothelial dysfunction in diabetes. Similarly, P2X7R inhibition with A438079 improved endothelial function and attenuated the Up4A-increased contraction in GK rats, despite an unaltered P2X7R expression. This suggests increased P2X7R sensitivity accounts for endothelial dysfunction in T2D. The importance of P2X7R among other P2XRs in regulation of vascular function in diabetes has been addressed in several studies. Thus, renal vascular reactivity is enhanced in response to ATP in diabetic rats through P2X7R [35]. Downregulation of P2X7R in coronary microcirculation of diabetic swine is compensated by enhancement of Up4A-mediated other vasodilator PRs [8]. Moreover, P2X7R activation accelerates retinal microvascular dysfunction in diabetic rabbits [36]. Activation of P2YRs generally results in vasodilation [32]. P2Y6R has been shown to be the predominant contractile receptor for both UTP and UDP-induced contraction in coronary vasculature with larger diameter, but acts as the vasodilator receptor in vessels with smaller diameter [37]. In the present study, P2Y6R inhibition with MRS2578 significantly improved endothelial function in GK rats, suggesting an involvement of P2Y6R in endothelial dysfunction in T2D. A similar upregulation of endothelial P2Y6R mediating increased UDP-induced relaxation in aortas of diabetic OLETF rats has been identified [38]. As the expression of P2Y6R did not significantly differ between GK and WT rats, increased P2Y6R sensitivity may exist in aortas of T2D accounting for the endothelial dysfunction. In contrast, P2Y6R inhibition had no effect on the Up4A-mediated aortic contraction in GK rats. Up4A has been shown to activate P2Y6R in coronary vasculature, where the P2Y6R-mediated relaxation is preserved in diabetic swine [8]. The finding that Up4A-mediated aortic contraction was not affected by MRS2578 in GK rats is likely due to the fact that Up4A does not activate P2Y6R in aortas, as Up4A does not significantly affect P2Y6R expression in aortic endothelial cells [39]. Altered PR sensitivity but not expression in diabetes is commonly observed in previous studies. Thus, activation of P2Y1R contributes to impaired relaxation in mesenteric arteries and activation of P2Y2R and P2Y4R accounts for the increased ATP-induced contraction in mesenteric arteries in diabetes without significant changes in receptor protein expression [11,12]. Moreover, as key purinergic receptors mediating Up4A-enhanced contraction, P2X1R and P2Y2R protein expression do not differ in renal arteries of WT and GK rats [10]. This is also supported by our previous findings that the sensitivity but not mRNA level of P2Y1R is increased to Up4A in coronary vasculature of diabetes [8].
Existing evidence indicate that endogenous ROS formation is greater in aortas from GK rats as compared to WT rats [40]. We further demonstrated that ROS inhibition improves endothelial function in aortas from GK rats [21]. Of importance, activation of P2X7R results in ROS production in endothelial cells with high glucose stimulation [41]. Up4A-induced contraction in aortas from WT rats is through P1R and ROS [18]. In addition to ROS, Up4A activates P2R to generate TxA2 leading to vascular contraction in mouse aortas [16]. Of note, Up4A-mediated coronary relaxation in diabetes is reduced via increased TxA2 [8]. Up4A-enhanced renal contraction in GK rats is via increased TxA2 receptor sensitivity [10]. Taken together, these findings imply that generation of ROS and TxA2 may also result from altered PR sensitivity induced by Up4A as potential post-receptor mechanisms in GK aortas leading to vascular dysfunction. Interestingly, an interaction between A1R and P2X7R exists [42]. The speculation that A1R interacts with P2X7R resulting in ROS production in our model may explain the similar inhibitory effect of the A1R or P2X7R antagonist on Up4A-induced contraction in aortas from GK rats. Further investigations are needed to elucidate exact mechanisms.
Some limitations of the present study need to be acknowledged. All experiments and pharmacological agents were applied ex vivo, which does not reflect the in vivo situation fully. Future studies are needed to validate endothelial function in vivo and this will definitely give more insights on the purinergic regulation of vascular function in diabetes. In addition, the lack of selective antagonists targeting several subtypes of PRs limits the delineation of the involvement of other PRs in the regulation of vascular function in T2D.
In conclusion, our findings indicate that the sensitivity of PRs are altered in T2D conduit arteries. Inhibition of several PRs individually results not only in improvement in EDR, but also in attenuation of the vasoconstrictor response to Up4A in T2D. These results imply that targeting PRs could serve as potential therapy for improving vascular function in patients with T2D.
4. Materials and Methods
4.1. Animals
All experimental protocols were performed in accordance with the Guide for Care and Use of Laboratory Animals (NIH publication no. 85–23, revised 1996) and approved by the regional ethical committee for animal experiments in Stockholm (ethical number: N108/14; approval date: 22 May 2014).
A total of 21 healthy male WT rats (14–18 weeks old on the day of experiment) and 37 age and sex-matched GK rats that spontaneously developed T2D were used in the present study. WT rats were purchased from Charles River (Sulzfeld, Germany) and housed in the animal facility of Karolinska University Hospital (L5). GK rats were derived from glucose intolerant WT rats and were bred in the animal facility of the Department of Molecular Medicine and Surgery, Karolinska Institute. The GK strain was established from normoglycemic WT rats by repeated inbreeding in each successive generation of the siblings with the highest blood glucose levels during an oral glucose tolerance test [43]. All animals were kept at 22 °C with 12 h light/dark cycle with free access to standard chow and water.
4.2. Tissue Preparations and Wire Myograph Protocols
Rats were anesthetized with pentobarbital sodium (50 mg/kg i.p) followed by thoracotomy and removal of aortas and guts. The rat aortas and mesenteric arteries were dissected, placed into Krebs–Henseleit (KH) buffer on ice and cleaned by removing fat and connective tissues under microscope, and subsequently cut transversely into 2 mm rings. Arterial segments were either used immediately for functional experiments or stored in −80 °C for later expression analysis. The aortic rings and mesenteric arteries were mounted in wire myograph (Danish Myo Technology, Aarhus, Denmark) in separate 6 ml organ baths containing KH buffer. The KH buffer (pH 7.4) containing (in mM) 118 NaCl, 4.7 KCl, 1.2 MgSO4, 1.2 KH2PO2, 25 NaHCO3, 11 glucose, and 2.4 CaCl2 was maintained at 37 °C and aerated with 95% O2/5% CO2. Changes in contractile forces were recorded with a Harvard isometric transducer. Following a 30 min stabilization period, the internal diameter was set at a tension equivalent to 0.9 times the estimated diameter at 100 mmHg effective transmural pressure [6,21]. At the end of the equilibration period, the vessels were exposed to KCl twice (50 mM and 100 mM, respectively for aortas; 50 mM each time for mesenteric arteries) to check the contractility. Thereafter, vessels were allowed to equilibrate in fresh KH buffer for 30 min before initiating different experimental protocols. For determination of PR involvement, the non-selective P1R antagonist 8PT (10 µM) [8,44], the non-selective P2R antagonist PPADS (10 µM) [8,45], the A1R antagonist DPCPX (10 nM) [16,46], the P2X7R antagonist A438079 (10 µM) [8,47], and the P2Y6R antagonist MRS2578 (10 µM) [8,38,39] were added in the organ bath 30 min before pre-constriction with 10−6 M phenylephrine (PE). EDR and EIR were determined by administration of increasing concentrations (10−9–10−5 µM) of ACh and SNP, respectively [21]. In separate experiments, Up4A contraction responses (10−6–3 × 10−5 µM) were conducted in vessel segments without preconstriction in the absence and presence of the purinergic antagonists mentioned above as well as the NO synthase inhibitor L-NAME (100 µM) [17].
4.3. Western Blotting
Rat aortas were lyzed with RIPA lysis buffer (Amresco, Solon, OH, USA) containing protease inhibitors (Roche, Mannheim, Germany) with subsequent homogenization and centrifugation at 12,000 g at 4 °C for 20 min. Protein content was quantified with bicinchoninic acid protein assay kit (Pierce Biotechnology, Life Technologies). The proteins were separated on 10% SDS gel (30 μg per sample) and transferred onto 0.45 μm nitrocellulose blotting membranes (Amersham, Freiburg, Germany). Membranes were blocked with 5% milk for 1 h at room temperature and incubated overnight at 4 °C with primary antibodies against A1R (1:500, Sigma-Aldrich, SL, USA, product number: A-268), P2X7R (1:200, Alomone Labs, Israel, product number: APR-004), P2Y6R (1:200, Alomone Labs, Israel, product number: APR-011) and GAPDH (1:2500, Sigma-Aldrich, MO, USA, product number: G9545), followed by incubation with secondary antibodies for 1 h at room temperature (goat anti-rabbit, 1:20,000, LICOR IR Dye 800CW, product number: 926-32211) [21]. Band densities were analyzed with Image Studio Lite Version 5.2 (LI-COR Bio-sciences, Bad Homburg, Germany). Data obtained were normalized to GAPDH and displayed with arbitrary units.
4.4. Statistical Analysis
Vascular relaxation to ACh or SNP was expressed as percentage of contraction to PE. Vascular contraction responses to Up4A were expressed as percentage of contraction to the second exposure to KCl. The effect of drug treatment on the relaxation and contraction responses were assessed using two-way analysis of variance for repeated measures. Unpaired t-test was used for comparison between two groups. n refers to the number of animals each analysis was made upon. All data are represented as means ± SEM. All the statistical analysis in the present study were performed with Prism 7.0, GraphPad, San Diego, CA, USA. Two-sided p < 0.05 was considered as statistically significant.
Acknowledgments
This work was supported by the Loo and Hans Ostermans Foundation 2018-01213 (Z.Z.), the Karolinska Institute Grant 2016 (Z.Z.), the Sigurt and Elsa Goljes Memorial Foundation (Z.Z.), the Swedish Research Council 10857 (J.P.), the Swedish Heart and Lung Foundation 20160239 (J.P.), the Diabetes Research Wellness Foundation 720-1519-16 (J.P.), the Söderberg Foundation M60/15 (J.P.), and the Stockholm County Council ALF 20160084 (J.P.).
Abbreviations
| Ach | acetylcholine |
| DPCPX | dipropylcyclopentylxanthine |
| EDR | endothelium-dependent relaxation |
| EIDR | endothelium-independent relaxation |
| GK | Goto Kakizaki |
| L-NAME | N(G)-Nitro-L-arginine methyl ester |
| OLETF | Otsuka Long-Evans Tokushima fatty |
| PE | phenylephrine |
| PPADS | pyridoxal phosphate-6-azo(benzene-2,4-disulfonic acid) |
| PR | purinergic receptor |
| ROS | reactive oxygen species |
| SNP | sodium nitroprusside |
| T2D | type 2 diabetes |
| Up4A | uridine adenosine tetraphosphate |
| WT | Wistar |
Author Contributions
Conceptualization, A.M., J.P., and Z.Z.; Methodology, A.M., T.J., and Z.Z.; Formal Analysis, A.M. and Z.Z.; Investigation, A.M., J.T., Y.T., and Z.Z.; Resources, J.P. and Z.Z.; Data Curation, A.M. and Z.Z.; Writing—Original Draft Preparation, A.M. and Z.Z.; Writing—Review and Editing, A.M., T.J., Y.T., J.Y., C-G.Ö., J.P., and Z.Z.; Visualization, A.M. and Z.Z.; Supervision, J.P. and Z.Z.; Project Administration, J.P. and Z.Z.; Funding Acquisition, J.P. and Z.Z.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Paneni F., Beckman J.A., Creager M.A., Cosentino F. Diabetes and vascular disease: Pathophysiology, clinical consequences, and medical therapy: Part I. Eur. Heart J. 2013;34:2436–2443. doi: 10.1093/eurheartj/eht149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Labazi H., Trask A.J. Coronary microvascular disease as an early culprit in the pathophysiology of diabetes and metabolic syndrome. Pharmacol. Res. 2017;123:114–121. doi: 10.1016/j.phrs.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi Y., Vanhoutte P.M. Macro- and microvascular endothelial dysfunction in diabetes. J. Diabetes. 2017;9:434–449. doi: 10.1111/1753-0407.12521. [DOI] [PubMed] [Google Scholar]
- 4.Burnstock G. Purinergic Signaling in the Cardiovascular System. Circ. Res. 2017;120:207–228. doi: 10.1161/CIRCRESAHA.116.309726. [DOI] [PubMed] [Google Scholar]
- 5.Dalziel H.H., Westfall D.P. Receptors for adenine nucleotides and nucleosides: Subclassification, distribution, and molecular characterization. Pharmacol. Rev. 1994;46:449–466. [PubMed] [Google Scholar]
- 6.Zhou Z., Merkus D., Cheng C., Duckers H.J., Jan Danser A.H., Duncker D.J. Uridine adenosine tetraphosphate is a novel vasodilator in the coronary microcirculation which acts through purinergic P1 but not P2 receptors. Pharmacol. Res. 2013;67:10–17. doi: 10.1016/j.phrs.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Burnstock G., Novak I. Purinergic signalling and diabetes. Purinergic Signal. 2013;9:307–324. doi: 10.1007/s11302-013-9359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou Z., Sorop O., de Beer V.J., Heinonen I., Cheng C., Jan Danser A.H., Duncker D.J., Merkus D. Altered purinergic signaling in uridine adenosine tetraphosphate-induced coronary relaxation in swine with metabolic derangement. Purinergic Signal. 2017;13:319–329. doi: 10.1007/s11302-017-9563-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsumoto T., Kobayashi S., Ando M., Iguchi M., Takayanagi K., Kojima M., Taguchi K., Kobayashi T. Alteration of Vascular Responsiveness to Uridine Adenosine Tetraphosphate in Aortas Isolated from Male Diabetic Otsuka Long-Evans Tokushima Fatty Rats: The Involvement of Prostanoids. Int. J. Mol. Sci. 2017;18:2378. doi: 10.3390/ijms18112378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsumoto T., Watanabe S., Kawamura R., Taguchi K., Kobayashi T. Enhanced uridine adenosine tetraphosphate-induced contraction in renal artery from type 2 diabetic Goto-Kakizaki rats due to activated cyclooxygenase/thromboxane receptor axis. Pflugers Arch. 2014;466:331–342. doi: 10.1007/s00424-013-1330-0. [DOI] [PubMed] [Google Scholar]
- 11.Ishida K., Matsumoto T., Taguchi K., Kamata K., Kobayashi T. Mechanisms underlying altered extracellular nucleotide-induced contractions in mesenteric arteries from rats in later-stage type 2 diabetes: Effect of ANG II type 1 receptor antagonism. Am. J. Physiol. Heart Circ. Physiol. 2011;301:H1850–H1861. doi: 10.1152/ajpheart.00502.2011. [DOI] [PubMed] [Google Scholar]
- 12.Ishida K., Matsumoto T., Taguchi K., Kamata K., Kobayashi T. Mechanisms underlying reduced P2Y(1) -receptor-mediated relaxation in superior mesenteric arteries from long-term streptozotocin-induced diabetic rats. Acta Physiol. (Oxf) 2013;207:130–141. doi: 10.1111/j.1748-1716.2012.02469.x. [DOI] [PubMed] [Google Scholar]
- 13.Thaning P., Bune L.T., Hellsten Y., Pilegaard H., Saltin B., Rosenmeier J.B. Attenuated purinergic receptor function in patients with type 2 diabetes. Diabetes. 2010;59:182–189. doi: 10.2337/db09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jankowski V., Tolle M., Vanholder R., Schonfelder G., van der Giet M., Henning L., Schluter H., Paul M., Zidek W., Jankowski J. Uridine adenosine tetraphosphate: A novel endothelium- derived vasoconstrictive factor. Nat. Med. 2005;11:223–227. doi: 10.1038/nm1188. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto T., Goulopoulou S., Taguchi K., Tostes R.C., Kobayashi T. Constrictor prostanoids and uridine adenosine tetraphosphate: Vascular mediators and therapeutic targets in hypertension and diabetes. Br. J. Parmacol. 2015;172:3980–4001. doi: 10.1111/bph.13205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou Z., Sun C., Tilley S.L., Mustafa S.J. Mechanisms underlying uridine adenosine tetraphosphate-induced vascular contraction in mouse aorta: Role of thromboxane and purinergic receptors. Vascul. Pharmacol. 2015;73:78–85. doi: 10.1016/j.vph.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou Z., Yadav V.R., Sun C., Teng B., Mustafa J.S. Impaired Aortic Contractility to Uridine Adenosine Tetraphosphate in Angiotensin II-Induced Hypertensive Mice: Receptor Desensitization? Am. J. Hypertens. 2017;30:304–312. doi: 10.1093/ajh/hpw163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linder A.E., Tumbri M., Linder F.F., Webb R.C., Leite R. Uridine adenosine tetraphosphate induces contraction and relaxation in rat aorta. Vascul. Pharmacol. 2008;48:202–207. doi: 10.1016/j.vph.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teng B., Labazi H., Sun C., Yang Y., Zeng X., Mustafa S.J., Zhou Z. Divergent coronary flow responses to uridine adenosine tetraphosphate in atherosclerotic ApoE knockout mice. Purinergic Signal. 2017;13:591–600. doi: 10.1007/s11302-017-9586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahdi A., Kovamees O., Checa A., Wheelock C.E., von Heijne M., Alvarsson M., Pernow J. Arginase inhibition improves endothelial function in patients with type 2 diabetes mellitus despite intensive glucose-lowering therapy. J. Intern. Med. 2018;284:388–398. doi: 10.1111/joim.12785. [DOI] [PubMed] [Google Scholar]
- 21.Zhou Z., Mahdi A., Tratsiakovich Y., Zahoran S., Kovamees O., Nordin F., Uribe Gonzalez A.E., Alvarsson M., Ostenson C.G., Andersson D.C., et al. Erythrocytes From Patients With Type 2 Diabetes Induce Endothelial Dysfunction Via Arginase I. J. Am. Coll. Cardiol. 2018;72:769–780. doi: 10.1016/j.jacc.2018.05.052. [DOI] [PubMed] [Google Scholar]
- 22.Costantino S., Paneni F., Battista R., Castello L., Capretti G., Chiandotto S., Tanese L., Russo G., Pitocco D., Lanza G.A., et al. Impact of Glycemic Variability on Chromatin Remodeling, Oxidative Stress, and Endothelial Dysfunction in Patients With Type 2 Diabetes and With Target HbA1c Levels. Diabetes. 2017;66:2472–2482. doi: 10.2337/db17-0294. [DOI] [PubMed] [Google Scholar]
- 23.Neves K.B., Nguyen Dinh Cat A., Alves-Lopes R., Harvey K.Y., da Costa R.M., Lobato N.S., Montezano A.C., de Oliveira A.M., Touyz R.M., Tostes R.C. Chemerin receptor blockade improves vascular function in diabetic obese mice via redox-sensitive- and Akt-dependent pathways. Am. J. Physiol. Heart Circ. Physiol. 2018 doi: 10.1152/ajpheart.00285.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goulopoulou S., Hannan J.L., Matsumoto T., Ogbi S., Ergul A., Webb R.C. Reduced vascular responses to soluble guanylyl cyclase but increased sensitivity to sildenafil in female rats with type 2 diabetes. Am. J. Physiol. Heart Circ. Physiol. 2015;309:H297–H304. doi: 10.1152/ajpheart.00079.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nemoto S., Kobayashi T., Taguchi K., Matsumoto T., Kamata K. Losartan improves aortic endothelium-dependent relaxation via proline-rich tyrosine kinase 2/Src/Akt pathway in type 2 diabetic Goto-Kakizaki rats. Am. J. Physiol. Heart Circ. Physiol. 2011;301:H2383–H2394. doi: 10.1152/ajpheart.00178.2011. [DOI] [PubMed] [Google Scholar]
- 26.Fotino C., Dal Ben D., Adinolfi E. Emerging Roles of Purinergic Signaling in Diabetes. Med. Chem. 2018;14:428–438. doi: 10.2174/1573406414666180226165204. [DOI] [PubMed] [Google Scholar]
- 27.Matsumoto T., Watanabe S., Ando M., Yamada K., Iguchi M., Taguchi K., Kobayashi T. Diabetes and Age-Related Differences in Vascular Function of Renal Artery: Possible Involvement of Endoplasmic Reticulum Stress. Rejuvenation Res. 2016;19:41–52. doi: 10.1089/rej.2015.1662. [DOI] [PubMed] [Google Scholar]
- 28.Zhou Z., Lankhuizen I.M., van Beusekom H.M., Cheng C., Duncker D.J., Merkus D. Uridine Adenosine Tetraphosphate-Induced Coronary Relaxation Is Blunted in Swine With Pressure Overload: A Role for Vasoconstrictor Prostanoids. Front Pharmacol. 2018;9:255. doi: 10.3389/fphar.2018.00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Labazi H., Teng B., Mustafa S.J. Functional changes in vascular reactivity to adenosine receptor activation in type I diabetic mice. Eur. J. Pharmacol. 2018;820:191–197. doi: 10.1016/j.ejphar.2017.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burnstock G. Purine and pyrimidine receptors. Cell Mol. Life Sci. 2007;64:1471–1483. doi: 10.1007/s00018-007-6497-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Konishi C., Naito Y., Ohara N. Age-related changes in adenosine 5′-triphosphate-induced constriction of isolated, perfused mesenteric arteries of rats. Life Sci. 1999;64:1265–1273. doi: 10.1016/S0024-3205(99)00061-2. [DOI] [PubMed] [Google Scholar]
- 32.Burnstock G. Control of vascular tone by purines and pyrimidines. Br J Pharmacol. 2010;161:527–529. doi: 10.1111/j.1476-5381.2010.00937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ralevic V., Burnstock G. Involvement of purinergic signaling in cardiovascular diseases. Drug News Perspect. 2003;16:133–140. doi: 10.1358/dnp.2003.16.3.876886. [DOI] [PubMed] [Google Scholar]
- 34.Headrick J.P., Ashton K.J., Rose′meyer R.B., Peart J.N. Cardiovascular adenosine receptors: Expression, actions and interactions. Pharmacol. Ther. 2013;140:92–111. doi: 10.1016/j.pharmthera.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Kreft E., Kowalski R., Jankowski M., Szczepanska-Konkel M. Renal vasculature reactivity to agonist of P2X7 receptor is increased in streptozotocin-induced diabetes. Pharmacol. Rep. 2016;68:71–74. doi: 10.1016/j.pharep.2015.06.140. [DOI] [PubMed] [Google Scholar]
- 36.Sugiyama T., Oku H., Komori A., Ikeda T. Effect of P2X7 receptor activation on the retinal blood velocity of diabetic rabbits. Arch. Ophthalmol. 2006;124:1143–1149. doi: 10.1001/archopht.124.8.1143. [DOI] [PubMed] [Google Scholar]
- 37.Haanes K.A., Spray S., Syberg S., Jorgensen N.R., Robaye B., Boeynaems J.M., Edvinsson L. New insights on pyrimidine signalling within the arterial vasculature - Different roles for P2Y2 and P2Y6 receptors in large and small coronary arteries of the mouse. J. Mol. Cell Cardiol. 2016;93:1–11. doi: 10.1016/j.yjmcc.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 38.Kobayashi S., Matsumoto T., Ando M., Iguchi M., Watanabe S., Taguchi K., Kobayashi T. UDP-induced relaxation is enhanced in aorta from female obese Otsuka Long-Evans Tokushima Fatty rats. Purinergic Signal. 2018;14:91–96. doi: 10.1007/s11302-017-9595-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou Z., Chrifi I., Xu Y., Pernow J., Duncker D.J., Merkus D., Cheng C. Uridine adenosine tetraphosphate acts as a proangiogenic factor in vitro through purinergic P2Y receptors. Am. J. Physiol. Heart Circ. Physiol. 2016;311:H299–H309. doi: 10.1152/ajpheart.00578.2015. [DOI] [PubMed] [Google Scholar]
- 40.Chettimada S., Ata H., Rawat D.K., Gulati S., Kahn A.G., Edwards J.G., Gupte S.A. Contractile protein expression is upregulated by reactive oxygen species in aorta of Goto-Kakizaki rat. Am. J. Physiol. Heart Circ. Physiol. 2014;306:H214–H224. doi: 10.1152/ajpheart.00310.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sathanoori R., Sward K., Olde B., Erlinge D. The ATP Receptors P2X7 and P2X4 Modulate High Glucose and Palmitate-Induced Inflammatory Responses in Endothelial Cells. PLoS ONE. 2015;10:e0125111. doi: 10.1371/journal.pone.0125111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sichardt K., Nieber K. Adenosine A(1) receptor: Functional receptor-receptor interactions in the brain. Purinergic Signal. 2007;3:285–298. doi: 10.1007/s11302-007-9065-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ostenson C.G., Khan A., Abdel-Halim S.M., Guenifi A., Suzuki K., Goto Y., Efendic S. Abnormal insulin secretion and glucose metabolism in pancreatic islets from the spontaneously diabetic GK rat. Diabetologia. 1993;36:3–8. doi: 10.1007/BF00399086. [DOI] [PubMed] [Google Scholar]
- 44.Gunduz D., Aslam M., Krieger U., Becker L., Grebe M., Arshad M., Sedding D.G., Hartel F.V., Abdallah Y., Piper H.M., et al. Opposing effects of ATP and adenosine on barrier function of rat coronary microvasculature. J. Mol. Cell Cardiol. 2012;52:962–970. doi: 10.1016/j.yjmcc.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 45.Abbas Z.S.B., Latif M.L., Dovlatova N., Fox S.C., Heptinstall S., Dunn W.R., Ralevic V. UDP-sugars activate P2Y14 receptors to mediate vasoconstriction of the porcine coronary artery. Vascul. Pharmacol. 2018;103–105:36–46. doi: 10.1016/j.vph.2017.12.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grbovic L., Radenkovic M. Analysis of adenosine vascular effect in isolated rat aorta: Possible role of Na+/K+-ATPase. Pharmacol. Toxicol. 2003;92:265–271. doi: 10.1034/j.1600-0773.2003.920603.x. [DOI] [PubMed] [Google Scholar]
- 47.Donnelly-Roberts D.L., Namovic M.T., Han P., Jarvis M.F. Mammalian P2X7 receptor pharmacology: Comparison of recombinant mouse, rat and human P2X7 receptors. Br. J. Pharmacol. 2009;157:1203–1214. doi: 10.1111/j.1476-5381.2009.00233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]