Abstract
Gestational diabetes mellitus (GDM) carries many risks, where high blood pressure, preeclampsia and future type II diabetes are widely acknowledged, but less focus has been placed on its effect on cognitive function. Although the multifactorial pathogenesis of maternal cognitive impairment is not completely understood, it shares several features with type 2 diabetes mellitus (T2DM). In this review, we discuss some key pathophysiologies of GDM that may lead to cognitive impairment, specifically hyperglycemia, insulin resistance, oxidative stress, and neuroinflammation. We explain how these incidents: (i) impair the insulin-signaling pathway and/or (ii) lead to cognitive impairment through hyperphosphorylation of τ protein, overexpression of amyloid-β and/or activation of microglia. The aforementioned pathologies impair the insulin-signaling pathway primarily through serine phosphorylation of insulin receptor substances (IRS). This then leads to the inactivation of the phosphatidylinositol 3-kinase/Protein kinase B (PI3K/AKT) signaling cascade, which is responsible for maintaining brain homeostasis and normal cognitive functioning. PI3K/AKT is crucial in maintaining normal cognitive function through the inactivation of glycogen synthase kinase 3β (GSκ3β), which hyperphosphorylates τ protein and releases pro-inflammatory cytokines that are neurotoxic. Several biomarkers were also highlighted as potential biomarkers of GDM-related cognitive impairment such as AGEs, serine-phosphorylated IRS-1 and inflammatory markers such as tumor necrosis factor α (TNF-α), high-sensitivity C-reactive protein (hs-CRP), leptin, interleukin 1β (IL-1β), and IL-6. Although GDM is a transient disease, its complications may be long-term, and hence increased mechanistic knowledge of the molecular changes contributing to cognitive impairment may provide important clues for interventional strategies.
Keywords: gestational diabetes mellitus, cognitive impairment, neuroinflammation, insulin resistance, oxidative stress
1. Introduction
Gestational diabetes mellitus (GDM) is defined by the American Diabetes Association as occurring in pregnant women who were not diagnosed with diabetes before pregnancy but have high blood glucose levels during pregnancy, usually around the 24th week [1]. The overall incidence of GDM is dramatically increasing, according to the International Diabetes Federation, who estimated that 200 million women suffered from GDM in 2015. GDM is projected to increase to 300 million in 2030 [2]; furthermore, between 10% and 25% of pregnancies suffer from GDM according to World Health Organization (WHO) reports in 2016 [3]. Women who develop GDM present a metabolic condition similar to that of type 2 diabetes mellitus (T2DM), characterized by insulin resistance coupled with defective insulin signaling [4,5,6]. Due to the similar pathophysiological mechanisms between T2DM and GDM, there will be common biomarkers that contribute to the complications of both diseases [7,8]. One such complication is cognitive decline, where metabolic syndrome is an established risk factor, which was first explained in the Rotterdam Study. The Rotterdam Study is a prospective, population-based cohort study, which investigated factors that determined the presence of neurological diseases and diabetes mellitus [9]. Results from this study showed that about 8.8% of diabetes cases present cognitive impairment. Additionally, diabetes has been established as a risk factor of vascular cognitive impairment [10]. Several preclinical and clinical studies have suggested that cognitive impairment in T2DM can been correlated with pathophysiology that includes hyperglycemia, insulin resistance, inflammation, vascular changes, and amyloid lesions [11,12,13,14,15,16,17]; accordingly, GDM clearly shares some features of the multifactorial pathogenesis seen in T2DM associated cognitive dysfunction. Reduction in insulin sensitivity and impaired insulin secretion are similar in both cases. However, hyperglycemia found in GDM is generally transitory and blood glucose level will normally return to normal after delivery [5].
Cognitive decline in GDM patients was first reported by Keskin et al. [18] where the association between cognitive function and metabolic status in 44 patients with GDM and 45 normal pregnant women were evaluated. GDM women aged above 30 years with a high body mass index (BMI) and glucose level were subjected to several cognitive function tests such as Montreal Cognitive Assessment, Symbol Digit Modalities Test and Spatial Recall Test, and were compared to non-diabetic women [18]. Based on the 30-point test in Montreal Cognitive Assessment, which evaluates mild cognitive impairment, GDM women scored 21 points and healthy pregnant women scored 24 points. The Symbol Digit Modalities requires women to pair abstract symbols and specific numbers within 90 s. GDM women showed poor speed of mental activity and attention, scoring five points lower than normal healthy pregnant women. Moreover, in the Spatial Recall Test and a visual memory test, women with GDM scored 4.5 points lower than normal pregnant women, with a score of 5.4 points [18].
Similarly, the brain development of the offspring of GDM women is also suspected to be affected from the prenatal stage. In a meta-analysis study, which examined the link between maternal diabetes and cognitive performance in offspring of GDM mothers, data were extracted from different electronic databases such as SciFinder, Scopus, The Cochrane Library and ClinicalTrial.gov. Infants from a GDM mother showed lower scores of mental and psychomotor development when compared to healthy pregnant women, with a mean standardized difference of −0.41 for mental development and −0.31 for psychomotor development [19]. Another study conducted by Linder et al. [20] showed that the postprandial auditory response of fetuses of GDM mothers is slower than the fetuses of normal glucose-tolerant (NGT) mothers. The auditory response of the fetus was recorded with a fetal magnetoencephalographic device after pregnant participants had undergone an oral glucose tolerance test (OGTT, 75 g). Sixty minutes after glucose ingestion, the auditory response latency of the GDM group was longer than in the NGT group (296 ± 82 ms vs. 206 ± 74 ms, p = 0.001), suggesting that the neural activity of fetuses of GDM mothers is slower than fetuses of NGT mothers [20].
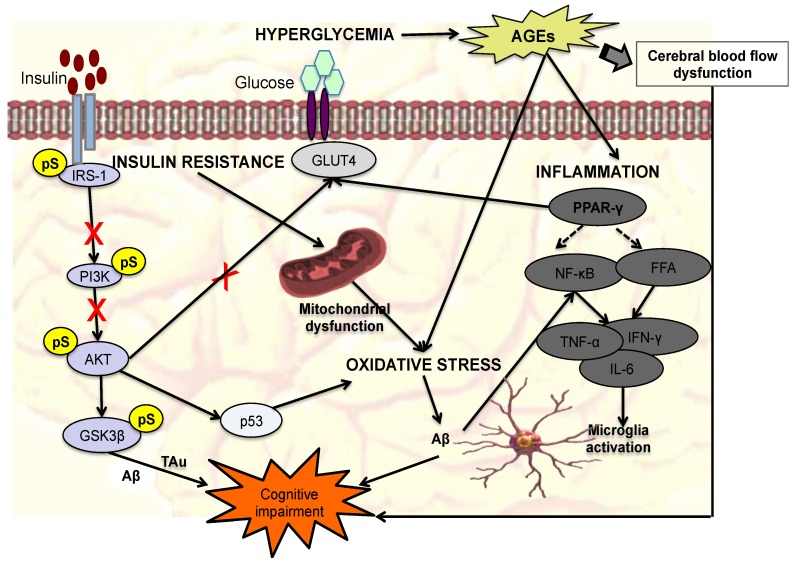
It is clear that GDM affects the cognitive function of not just the mother but also the offspring; however, the effect on the offspring is studied more than that on the mothers. Given that the genesis of GDM-induced cognitive impairment begins in the mother and is passed onto their offspring, it is important to study the possible markers for GDM-associated cognitive decline and its pathophysiology. Unfortunately, mechanistic study on this is severely lacking. In this review, we looked at several pathophysiologies of GDM, T2DM, and other neurocognitive diseases which may shed more light on the mechanism of GDM-associated cognitive function. One of the findings from Genetic Wide Association Studies (GWAS) was that several different diseases are interconnected and may share several genes [21]. Hence, it is possible to gain insight of a disease by studying other diseases with which it may share similarities, such as on a genotypic and/or phenotypic level [21,22,23]. In addition, given the overlap between genes associated with both GDM and T2DM, and the observation that GDM mothers are at an increased risk for the development of T2DM [24], cognitive impairment associated with GDM might be long-term [25]. This further highlights the importance of understanding the pathophysiology of GDM-associated cognitive function in mothers. In this review, we will examine incidents of GDM that are potentially linked to maternal cognitive impairment viz. hyperglycemia, insulin resistance, oxidative stress and neuroinflammation. A summary of each of the markers, changes, and outcomes of each of the pathophysiologies can also be found in Table 1, and a figurative summary can be found in Figure 1.
Table 1.
Summary of the proposed pathophysiological alterations in maternal cognitive impairment associated with GDM.
| Evidence | Markers | Pathophysiological Changes | Adverse Effects and Outcome |
|---|---|---|---|
| Hyperglycemia | Advanced glycation end products (AGEs) [26]. |
|
|
| Insulin resistance | GLUT 4 [31], GluA1, GluN2B [32], IRS-1 [33], GSK3β [34]. |
|
|
| Oxidative stress | ROS [37], p53 [38], NOS/NOX, [38,39,40,41,42] SOD, CAT, GPX [43,44,45], GSH [46]. |
|
|
| Neuro- inflammation | IL-6 and TNF-α [53], IL-2, hs-CRP [54], IL-8,NF-κβ [55] IL-1β, [56], Leptin [57], PPAR-γ [58]. |
Figure 1.
Summary of the proposed mechanisms of maternal cognitive impairment associated with gestational diabetes mellitus (GDM). The red ‘X’ and dashed arrows indicate inhibition and negative regulation respectively. Four mechanisms of GDM-induced cognitive impairment are covered here, which are hyperglycemia, insulin resistance, oxidative stress, and inflammation. In hyperglycemic condition, advanced glycation end products (AGEs) are overproduced, leading to oxidative stress, inflammation, and dysfunction of cerebral flow. Dysfunction of cerebral flow can lead to cognitive dysfunction through disruption of blood-brain barrier (BBB) transport mechanism that transport important molecules such as choline into the brain and clears unwanted molecules such as amyloid-β (Aβ) protein. In cases of insulin resistance, the insulin-signaling pathway is inactivated primarily through serine phosphorylation of insulin receptor substance (IRS-1). This inactivates the phosphatidylinositol 3-kinase/protein kinase B (PI3K/AKT) signaling cascade, which blocks the translocation of glucose transporter 4 (GLUT4), decreasing glucose uptake. Additionally, glycogen synthase kinase 3β (GSK3β) is also activated causing the hyperphosphorylation of τ proteins and overexpression of Aβ proteins. Instances such as overexpression of AGEs, insulin resistance and mitochondrial dysfunction can lead to oxidative stress, which cause the overexpression of Aβ. Free fatty acid (FFA) triggers activation of the microglia via nuclear factor kappa β (NF-κB) signaling production of pro-inflammatory cytokines (tumor necrosis factor α; TNF-α, interleukin 1β; IL-1β, interleukin 6; IL-6) additionally, Aβ induces the production of Nuclear factor-kappa β; NF-κβ, which also releases pro-inflammatory cytokines.
2. Pathophysiology of GDM That Can Lead to Cognitive Impairment
2.1. Hyperglycemia
Hyperglycemia is the hallmark of type 1 diabetes mellitus (T1DM), T2DM, and GDM, resulting from a decline of insulin supply that is insufficient to meet tissue demands for normal blood glucose regulation and/or insensitivity of insulin towards insulin receptors [4]. Given that hyperglycemia is the common denominator among the three types of diabetes, it stands to reason that hyperglycemia may lead to cognitive impairment based on several studies [12]. Indeed, reports have demonstrated the positive correlation between glycated hemoglobin (HbA1c), a measure of blood sugar level, and cognitive decline. A study by Zeng et al. [65] looked at possible association between HbA1c levels and long-term cognitive decline where a 1 mmol/mol increase of HbA1c was significantly correlated with an increase rate of decline in tests including memory, executive function and global cognitive task [65]. Similar results were also observed in Gupta, et al. [66], although the study involves fewer participants than the former and were not conducted over a long period of time.
One possible way that hyperglycemia induces cognitive impairment is through the production of advanced glycation end products (AGEs) (see Figure 1) [26]. Several studies have demonstrated the positive correlation between AGEs and cognitive impairment, leading to the suggestion that AGEs are a biomarker of cognitive impairment in diabetic conditions. One such study is by Spauwen et al. [26], which is a part of the Maastricht Study, a population-based study involving 215 patients with T2DM. In this study, the association between AGEs, obtained through non-invasive skin autofluorescence, and cognitive function of the patients were analyzed. Cognitive function such as verbal memory, global cognitive functioning, response inhibition and information processing speed were assessed. The study showed that AGEs level was positively correlated with worse delayed-word recall and response inhibition, leading to the conclusion that AGEs level is associated with poor cognitive performance [26]. Similar findings were also observed in Wang et al. [67] where soluble receptors of advanced glycation end products (sRAGE) and AGE-peptide (AGE-P) levels were measured in T2DM patients with mild cognitive impairment (MCI). In addition, their performance on several neuropsychological tests was also evaluated. Compared to the control, the MCI group showed a lower sRAGE level (0.87 vs. 1.05 ng/mL) and higher AGE-P level (3.55 vs. 2.71 U/mL) [67]. sRAGE was negatively correlated with TMT-B score, a test for early mild cognitive impairment, and AGE-P was negatively correlated with several tests assessing different cognitive domain [67]. AGEs are formed through non-enzymatic reactions between reduced sugars (usually glucose) and amino acids contained in proteins [68]. This process takes place under oxidative stress and/or hyperglycemic conditions, and produces Schiff base, from the complex formed between glucose and protein. The Schiff base is reversible but if the reaction continues, it undergoes a rearrangement involving a non-enzymatic glycosylation forming what is called an Amadori product. Amadori products are stable but less reversible compared to Schiff bases. After several weeks, the Amadori products stabilize and reach equilibrium. They will undergo further changes, ultimately transforming to the irreversible AGEs [69]. The cross-linking and glycation of proteins (such as collagen and amyloid) to produce AGEs can impair their function and structural integrity. Furthermore, the accumulation of AGEs, and its activation via its receptor RAGEs, evokes several reactions such as oxidative stress, inflammation, and fibrotic and thrombotic reactions [67]. All of these can lead to cognitive impairment. Regarding oxidative stress and inflammation, these will be explained in separate sections.
Cognitive impairment and other central nervous system (CNS)-related dysfunction have been linked to the dysfunction of the neurovascular unit and regulation of cerebral blood flow [27,28]. The effect of hyperglycemia on the vascular system has been well documented where hyperglycemia induces abnormal proliferation of endothelial cells, thickening of capillary walls, lowering of perfusion rates and increase in vascular permeability [27]. These effects have been found to affect the integrity of the blood–brain barrier (BBB) and its transport function [27]. The BBB is the gatekeeper of the brain, where it is responsible for the maintenance of brain homeostasis by transporting essential molecules in and out of the CNS in accordance with the metabolic needs of the brain and protects the CNS from harmful substances. The BBB transport mechanism is responsible for transporting molecules such as choline across the BBB. Choline is a precursor of acetylcholine, a neurotransmitter that is responsible for functions such as memory, where lack of acetylcholine is known to be one of the causes of Alzheimer’s disease (AD). Vascular damage of the BBB can hinder the transport of choline, depriving the brain of an important neurotransmitter and affecting the homeostasis of the brain. Additionally, vascular damage can also reduce the clearance of amyloid-β (Aβ) protein, which then promotes tau (τ) phosphorylation causing cognitive impairment and disrupting the brain homeostasis. These chemicals can induce damage to the CNS through oxidative stress and inflammation. The BBB also protects the CNS from harmful substances such as free radicals and pro-inflammatory cytokines. In cases of damage to the BBB, these chemicals can easily infiltrate the CNS [29,30].
2.2. Insulin Resistance
Insulin resistance is another mechanism that can possibly contribute to the neuropathology of cognitive impairment in GDM, given the substantial amount of studies that have already been published linking cognitive dysfunction to insulin resistance [70,71,72,73]. In GDM, changes in hormones and increased adipose tissue are observed [74]. The placenta, which produces several hormones e.g., human placental lactogen, estrogen and progesterone, can cause insulin resistance by reducing the expression of glucose transporter-4 (GLUT4) and causing the dysfunction of β-cell adaptive response for enhancing insulin production. In addition, the increase in adipose tissue due to high intake of food to provide energy for the mother and for the development and growth of the fetus results in high production of adipocytokines. Adipocytokines are adipocyte hormones that are involved in the regulation of metabolism and insulin resistance such as TNF-α, adipokines, and leptin [74].
The insulin-signaling pathway is activated when insulin binds to an insulin receptor (IR), leading to the recruitment of adapter proteins such as insulin receptor substances (IRS) through the phosphorylation of its tyrosine residue (see Figure 1). In response, three major signaling pathways will be triggered, which are mitogen activated protein (MAP) kinase, casitas b-lineage lymphoma/Cbl-associated protein (Cbl/CAP), and phosphatidylinositol 3-kinase (PI3K) pathways. The PI3K cascade activates the AKT/PKB [47,75,76,77], causing the translocation of GLUT4 to the plasma membrane, increasing glucose uptake [31]. The insulin-signaling pathway can be impaired through two mechanisms, where (i) downstream components of the pathway (mTOR/S6K, MAPK, PKC) inhibit the upstream components, similar to the negative feedback mechanism, and (ii) inhibition by molecules (GSK3β, IKKβ, JNK, mPLK, AMPK) from other pathways. In the latter, this is achieved primarily through the serine phosphorylation of IRS, blocking further signal propagation. Serine-phosphorylated IRS has been suggested to be a biomarker of T2DM, and potentially GDM as well. Several of these IRS kinases (e.g., S6K1, PKC) are both inducers of insulin resistance and activated in response to insulin. The insulin-signaling pathway is highly conserved in all organs that express insulin receptors, including the brain [33,35]. In the brain, insulin receptors are expressed in the hippocampus region, which is responsible for memory and cognition [36]; down-regulation of IR in the hippocampus has been reported to decrease learning abilities and induce memory impairment in rats, as evaluated in a Morris Water Maze test [32]. Furthermore, this study also discovered that down-regulation of IR in the hippocampus inhibits the activation of glutamatergic system via decreasing phosphorylation of GluA1 and down-regulation of GluN2B [32]. The glutamatergic system is responsible for regulating synaptic plasticity and hence hippocampus-dependent spatial learning. The impairment of insulin signaling in the brain may also cause the activation of GSκ3β, where, under normal circumstances, it is inactivated when PI3K/AKT pathway is triggered as a result of insulin binding to IR. GSκ3β causes the phosphorylation of τ protein, consequently blocking the binding of the τ protein to microtubules. This results in the τ protein becoming unstable and will then disintegrate [34]. The unbound τ accumulates together and forms neurofibrillary tangles (NFT) [78,79,80]. Elevation of NFT will cause neuronal loss, which is associated with cognitive defects [34]. GSκ3β also releases pro-inflammatory cytokines (IL-2, IL-6 and TNF-α), which have neurotoxic effects on the CNS (see later section).
Impairment of the insulin-signaling pathway can also lead to the production of Aβ protein, which is derived from the amyloid precursor protein (APP) from sequential cleavage by β and γ secretase. Under normal conditions, APP is cleaved by α-secretase, where soluble APP fragments (sAPPα) are released into the extracellular space and partake in synaptic plasticity and cell survival. However, in memory-related diseases such as AD and dementia, APP is predominantly cleaved by β and γ secretase, induced by oxidative stress and hence produces a high concentration of Aβ. Studies by Solano et al. [81] and Gasparini et al. [82] showed that insulin treatment increased sAPPα secretion in a concentration and tyrosine kinase-dependent manner in neurons, reducing Aβ level. This suggests that sAPPα production is mediated by insulin [83] through the activation of insulin-signaling pathway [84,85]. Talbot et al. [33], in a case of cohorts from the University of Pennsylvania and the Religious Order Study, discovered a correlation between serine-phosphorylated IRS-1 and Aβ plaques, where serine-phosphorylated IRS-1 was found to be positively correlated with oligomeric Aβ plaques and negatively correlated with working and episodic memory. Besides PI3K/AKT, several other members of the insulin-signaling pathway have been studied for their involvement in cognitive dysfunction. Su et al. [86] compared the expression of 20 genes of the insulin-signaling pathway between 87 MCI subjects and 135 controls. Cognitive performance was also analyzed over a period of 35 months and it was found that 8 out of the 20 genes could be associated with cognitive performance. AKT1 and ATK2 were related to information processing speed and general cognition, respectively. Episodic memory was influenced by IGF1R and PIK3CB, and executive functioning was influenced by insulin degrading enzyme (IDE), PIK3CD, mTOR and AKT1S1 [86].
2.3. Oxidative Stress
Pregnant women experience an increase in oxygen consumption due to their increase in energy expenditure [87]. In GDM, oxidative stress, an imbalance between reactive oxygen species (ROS) and anti-oxidant enzyme levels was observed [88,89,90]. This has prompted the suggestion that oxidative stress contributes to the pathophysiology of GDM although concrete links have yet to be established; however, the link between T2DM and oxidative stress has been strongly established [91,92,93]. Alteration in free radical–anti-oxidant balance, glucose oxidation, lipid peroxidation, and production of AGEs, which are common in diabetes mellitus, can result in elevated levels of ROS, causing a state of oxidative stress. In pregnancy, a higher-than-usual level of ROS can be attributed to increased amounts of transitional metal ions e.g., iron and a mitochondria-rich placenta [91]. ROS modulates the insulin-signaling pathway via two mechanisms. The first mechanism involves the production of ROS in response to insulin where higher organisms have evolved the use of NO and ROS as signaling molecules for other physiological functions including regulation of vascular tone, monitoring of oxygen tension in the control of ventilation and signaling transduction from membrane receptors in various physiological processes. In the second mechanism, ROS negatively regulates the insulin pathway leading to reduced insulin secretion and consequently insulin resistance [37]. ROS trigger insulin resistance in the peripheral tissues by affecting various points in insulin receptor signal transduction, ultimately resulting in decreased expression of GLUT4 transporter in the cellular membrane [94]. Besides increased level of ROS, anti-oxidant enzymes such as SOD and CAT were found to be lower in diabetic control rats [43,44,45]. Superoxide dismutase activity and protein carbonyl content in the placenta were also found to be relatively low in GDM [95]. Superoxide dismutase regulates superoxides, which is a by-product of glucose metabolism and causes cellular damage.
The brain is an organ that is very sensitive to oxidative insults due to its high oxygen consumption rate, abundant lipid content and low anti-oxidant enzymes [96]. Oxidative stress in the brain may promote apoptosis, cell damage, disruption of neuronal function, and loss of synapse, all of which leads to cognitive dysfunction [47]. As previously mentioned, oxidative stress in the brain also promotes the cleavage of APP by β and γ secretase, producing a high concentration of Aβ. Brain insulin resistance may further produce high free radicals and reduce anti-oxidant enzymes in the brain that are already low in GDM to begin with. Free radicals can cause chemical modifications of proteins, lipids, DNA and RNA, thereby compromising the functional and structural integrity of neurons [48]. Consequently, loss of membrane cell functions and reduced neurotransmitter function and neuronal plasticity may be observed. The increase in free radicals also activates the NF-κβ pathway [41] that generates cytokines, where its role in GDM/cognition will be explored more in the next section.
One of the ways brain insulin resistance can increase free radical production is through inducing mitochondrial dysfunction (see Figure 1). It has been suggested that cognitive dysfunction can be attributed to mitochondrial dysfunction, which highly exposes the brain to apoptosis [97], a mechanism of cell loss in neurodegenerative diseases [97]. Mitochondria, an important organelle that converts energy into ATP but it is also a site of free radical production [47]. In the mitochondria, free radicals are produced mainly by Complex I (NADH CoQ reductase) and Complex III (bc1 complex) [98]. Insulin regulates mitochondrial function through the activation of the PI3K/AKT pathway, inhibiting the transcriptional factor, FOXO1. FOXO1 is hyperactivated in insulin resistance, inducing HMOX1, which oxidizes heme to biliverdin and ferric ion (Fe3+) [99]. Heme is important in both the function and stability of electron transport proteins. The depletion of heme roots the dysfunction of the mitochondrial electron transport chain, hence resulting in mitochondrial dysfunction [100] leading to an increased free radical production and decreased ATP production [47]. Brain insulin resistance can also lead to the reduction of anti-oxidant enzymes, by increasing the expression of p53 via inactivation of PI3K/AKT signaling cascade. Pro-apoptosis genes p53, NOS and NOX, which will result in reduced expression of genes encoding mitochondria-encoded complexes IV and V, function in the frontal lobe [38]. Undoubtedly, abnormalities in mitochondrial complexes, especially the activity of complex IV, which is the most documented reduction of mitochondrial enzyme activity that plays a vital role in cell degeneration and death, is seen in cognitive dysfunctions [49,50,51,52]. A study by Correia et al. [101] showed that rats administered with streptozotocin (STZ)-through intracerebroventricular (icv) injection experienced brain insulin resistance in addition to mitochondrial abnormalities with increased free radical levels. As stated earlier, increased production of free radicals in the brain may cause apoptosis and necrosis where it can inhibit neurogenesis [102]. Elevated levels of p53 gene activate nitric oxide synthase isoforms, mainly NOS 1–3 and NADPH-oxidase (NOX1 and 3) [38]. This inhibits anti-oxidant enzymes such as SOD, CAT, and GPX [39,40,41,42]. Hyperglycemia can also reduce the anti-oxidant enzyme level, particularly glutathione [103], produced from the reduction of glutathione disulfide (GSSG) by glutathione reductase enzyme and NADPH as a cofactor [104]. NADPH is also a cofactor for also aldose reductase, which converts glucose to sorbitol, and subsequently gets converted to fructose by sorbitol dehydrogenase in the polyol pathway [105]. In diabetic conditions, activation of the polyol pathway increases in parallel with glucose level, causing a decrease in NADPH and consequent decreases in GSH level [46].
2.4. Neuroinflammation
One of the characteristics of pregnancy is an altered inflammatory profile. It is crucial to have a highly regulated balance between pro- and anti-inflammatory cytokines in pregnancy, particularly for normal implantation, trophoblast invasion, and placentation [106]. However, in cases of GDM, a pro-inflammatory state has been reported [107,108,109,110]. In addition, the inflammation experienced in GDM is metabolically induced; hence the term metainflammation was coined, which leads to insulin resistance [111]. Furthermore, metainflammation displays these characteristics: (i) linked to a low metabolic rate; (ii) low-grade response; (iii) immune cells in pancreas, adipose tissue, and liver are altered to favor a pro-inflammatory state; and (iv) maintained by metabolic cells e.g., adipocytes [106]. As previously mentioned, adipose tissue release adipocytokines that induce insulin resistance and adipocytokines such as TNF-α, IL-1β, and IL-6 are pro-inflammatory cytokines, promoting a state of chronic low-grade inflammation [53,56]. Adipocytokines also releases leptin and adipokines, where leptin increases insulin sensitivity via increased insulin secretion, glucose use, glycogen synthesis, and fatty acid metabolism. Prospective studies have shown that GDM is linked to the down-regulation of anti-inflammatory cytokines (e.g., IL-4 and IL-10) and up-regulation of pro-inflammatory cytokines implicated in insulin resistance (e.g., IL-6 and TNF-α) [53]. Hyperglycemia and insulin resistance can also trigger the release of these cytokines where the former is through the formation of AGEs and the latter is through the inactivation of the PI3K/AKT signaling cascade, which activates GSK3β that releases pro-inflammatory cytokines. Neuroinflammation can lead to the development of cognitive impairment, and several studies have reported the presence of inflammation in the brains of cognitive dysfunction [62,112,113]. Another possible way that inflammation leads to cognitive decline is through the activation of microglia [55,59]. Activated microglia proliferates into macrophages, a main form of active immune defense in the CNS [60,61]. Pro-inflammatory cytokines such as IL-2, IL-6 and TNF-α are neurotoxic substances that can stimulate microglia activation (see Figure 1) [55]. Activation of microglia can cause alterations in the gene expression of various neurotoxic mediators such as TNFα, IL-1β, nitric oxide, superoxide, eicosanoids, and quinolinic acid [60,114,115]. This will attract leukocytes to the CNS, which amplifies the cycle of inflammation, inducing apoptosis and vascular breakdown, promoting glial impairment and neuronal cell death [55,116]. As explained previously, oxidative stress induces production of Aβ, which in turn activates the NF-κβ via binding of Aβ with RAGE [117,118]. NF-κβ is identified as one of the main regulator of inflammation and oxidative stress [55] that controls the expression of several important genes involved in the immune response. Activation of NF-κβ results in the release of pro-inflammatory cytokines such as TNF-α and interleukins (IL-2, IL-6, IL-8) [55]. The hippocampus region of brains derived from STZ-rats showed increased expression of NF-κβ resulted in an elevated level of pro-inflammatory cytokines [56]. In a study of 276 diabetic elderly by Gorska-Ciebiada et al. [112] several inflammatory markers e.g., TNF-α, CRP and IL-6 and its correlation with MCI, assessed through the Montreal Cognitive Assessment. It was found that the MCI groups showed a higher level of the three inflammatory markers compared to control; however, the difference between the two groups regarding IL-6 was not statistically significant [112]. However serum levels of IL-1β and leptin were higher in MCI group compared to control [119]. In normal pregnancy, leptin is usually high in early until late pregnancy [120] and will return to normal after delivery. In GDM, level of leptin is higher than in normal pregnancy and remains high after pregnancy [57]. This may be due to the high production of inflammatory cytokines such as TNF-α and IL-6 [121,122], thus further amplifying inflammatory conditions. In normal pregnancy, adiponectin level is low in the first trimester, but the level further drops in the third trimester when insulin resistance is at its peak. However, in GDM, the level of adiponectin is significantly lower than in normal pregnancy. Adiponectin exhibits an anti-inflammatory effect by inhibiting phagocytic activity of macrophages that produces TNF-α [123]. However, inflammatory mediators such as TNF-α can also block the production of adiponectin. Inflammation can also affect cerebral vasoregulation, which could accelerate the advancement of cognitive decline in diabetic cases [54,62]. Chung et al. [54] reported that a high level of vascular adhesion molecules and hs-CRP can be correlated with decreased cerebral vasodilation and vasoreactivity. Furthermore, the decrease in vasoreactivity was positively correlated with a decline in multiple cognitive tasks in diabetic patients. Peroxisome proliferator-activated receptor γ (PPAR-γ), a nuclear receptor subfamily, that causes insulin sensitization and enhances glucose metabolism [124] may be implicated in cognitive impairment in GDM. PPAR-γ mRNA level was lower by 38% in pregnant control and 48% in GDM subjects compared with non-pregnant controls [58]. More importantly, PPAR-γ also has anti-inflammatory activity where it blocks NF-κβ and reduces TNF-α level [125], and several studies have shown the neuroprotective effect of PPAR-γ agonists in animal models [63,64]. Decreased PPAR-γ and its target genes may be part of the molecular mechanism to accelerate fat catabolism to meet fetal nutrient demand in late gestation [58].
3. Future Directions and Conclusions
This review focuses on cognitive impairment in GDM and the different pathologies of GDM that can lead to cognitive impairment. The pathologies outlined are also suggested to be involved in T2DM-related cognitive decline; hence it is reasonable to consider the shared pathologies as possible contributors to their complications as well. Here, we would like to highlight several notes that can aid future research in GDM-associated maternal cognitive impairment:
-
(a)
Potential biomarkers and molecules for cognitive decline includes AGEs, serine-phosphorylated IRS-1, and cytokines such as TNF-α, hs-CRP, leptin, IL-1β, and IL-6. The level of these molecules should be evaluated in GDM cases in the future and in relation to cognitive decline.
-
(b)
The PI3K and AKT signalling cascade is important in the downstream insulin pathway in GDM. Moreover, there is also crosstalk with other pathways that are important in maintaining cognitive function through increasing or decreasing key regulators of cognitive function such as GSK3β.
However, one should also be cautious in relating complications seen in T2DM with GDM. Although the similarities between both do provide some clues when investigating GDM-related cognitive impairment, there are some differences between T2DM and GDM that need to be taken into account. Firstly, pregnancy hormones play a pivotal role in the pathophysiology of GDM and therefore its involvement in GDM-associated maternal cognitive impairment should be explored as well. Secondly, GDM is a transient disease where, in most cases, blood sugar level will return to normal after delivery. This provides a major setback in GDM research where it is difficult to determine whether complications related to GDM and its effects are long-term. Thirdly, while the diseases may share similarities on a genotypic and phenotypic level, they have different risk factors, such as age and gender, which may play contributing role in their pathophysiologies.
There is clearly a need for more research in understanding cognitive impairment in GDM even though GDM-related pathologies such as hyperglycemia, insulin resistance, oxidative stress, and neuroinflammation have been extensively explored in the cognitive impairment of different diseases e.g., AD and T2DM. As new knowledge is gained, it can be applied to develop new and improved ways to prevent and treat GDM and its related complications.
Funding
This research and APC were funded by the Ministry of Education of Malaysia with Universiti Teknologi MARA (UiTM) through the Fundamental Research Grant Schemes (FRGS; 600-RMI/FRGS 5/3 (0020/2016) and FRGS/1/2014/SKK02/UITM/03/1).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.American Diabetes Association (2) Classification and Diagnosis of Diabetes. Diabetes Care. 2015;38:S8–S16. doi: 10.2337/dc15-S005. [DOI] [PubMed] [Google Scholar]
- 2.Ogurtsova K., da Rocha Fernandes J.D., Huang Y., Linnenkamp U., Guariguata L., Cho N.H., Cavan D., Shaw J.E., Makaroff L.E. Idf Diabetes Atlas: Global Estimates for the Prevalence of Diabetes for 2015 and 2040. Diabetes Res. Clin. Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organisation . Global Report on Diabetes. WHO Press; Geneva, Switzerland: 2016. [Google Scholar]
- 4.Buchanan A.T., Xiang A.H. Gestational Diabetes Mellitus. J. Clin. Investig. 2005;115:485–491. doi: 10.1172/JCI200524531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weijers N.R., Bekedam D.J. Relationship between Gestational Diabetes Mellitus and Type 2 Diabetes: Evidence of Mitochondrial Dysfunction. Clin. Chem. 2007;53:377–383. doi: 10.1373/clinchem.2006.077636. [DOI] [PubMed] [Google Scholar]
- 6.Herath H.R., Wickremasinghe R. Gestational Diabetes Mellitus and Risk of Type 2 Diabetes 10 Years after the Index Pregnancy in Sri Lankan Women-a Community Based Retrospective Cohort Study. PLoS ONE. 2017;12:e0179647. doi: 10.1371/journal.pone.0179647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karamanos B.A., Thanopoulou E., Anastasiou S., Assaad-Khalil N., Albache M., Bachaoui C.B., Slama H., El Ghomari A., Jotic N., Lalic A., et al. Relation of the Mediterranean Diet with the Incidence of Gestational Diabetes. Eur. J. Clin. Nutr. 2014;68:8–13. doi: 10.1038/ejcn.2013.177. [DOI] [PubMed] [Google Scholar]
- 8.Salib M.M., Hickman P.E., Oakman C., Potter J.M. Retrospective Reassessment of Gestational Diabetes Mellitus Diagnosis by Using the New Classification. Pathology. 2015;47:391–392. doi: 10.1097/PAT.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 9.Alewijn O., Stolk R.P., Van Harskamp F., Pols H.A.P., Hofman A., Breteler M.M.B. Diabetes Mellitus and the Risk of Dementia the Rotterdam Study. Neurology. 1999;53:1937. doi: 10.1212/wnl.53.9.1937. [DOI] [PubMed] [Google Scholar]
- 10.Matioli M.N.P.D.S., Suemoto C.K., Rodriguez R.D., Farias D.S., da Silva M.M., Paraizo Leite R.E., Ferretti-Rebustini R.E.L., Pasqualucci C.A., Jacob W.F., Grinberg L.T. Association between Diabetes and Causes of Dementia: Evidence from a Clinicopathological Study. Dement. Neuropsychol. 2017;11:406–412. doi: 10.1590/1980-57642016dn11-040010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ricci G., Pirillo I., Tomassoni D., Sirignano A., Grappasonni I. Metabolic Syndrome, Hypertension, and Nervous System Injury: Epidemiological Correlates. Clin. Exp. Hypertens. 2017;39:8–16. doi: 10.1080/10641963.2016.1210629. [DOI] [PubMed] [Google Scholar]
- 12.Kodl C.T., Seaquist E.R. Cognitive Dysfunction and Diabetes Mellitus. Endocr. Rev. 2008;29:494–511. doi: 10.1210/er.2007-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lutski M., Weinstein G., Goldbourt U., Tanne D. Insulin Resistance and Future Cognitive Performance and Cognitive Decline in Elderly Patients with Cardiovascular Disease. J. Alzheimer’s Dis. 2017;57:633–643. doi: 10.3233/JAD-161016. [DOI] [PubMed] [Google Scholar]
- 14.Hamed S.A. Brain Injury with Diabetes Mellitus: Evidence, Mechanisms and Treatment Implications. Expert Rev. Clin. Pharmacol. 2017;10:409–428. doi: 10.1080/17512433.2017.1293521. [DOI] [PubMed] [Google Scholar]
- 15.Mittal K., Katare D.P. Shared Links between Type 2 Diabetes Mellitus and Alzheimer’s Disease: A Review. Diabetes Metab. Syndr. 2016;10:S144–S149. doi: 10.1016/j.dsx.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 16.Okereke O.I., Kang J.H., Cook N.R., Gaziano J.M., Manson J.E., Buring J.E., Grodstein F. Type 2 Diabetes Mellitus and Cognitive Decline in Two Large Cohorts of Community-Dwelling Older Adults. J. Am. Geriat. Soc. 2008;56:1028–1036. doi: 10.1111/j.1532-5415.2008.01686.x. [DOI] [PubMed] [Google Scholar]
- 17.De Felice F.G., Lourenco M.V., Ferreira S.T. How Does Brain Insulin Resistance Develop in Alzheimer’s Disease? Alzheimer’s Dement. 2014;10:S26–S32. doi: 10.1016/j.jalz.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Keskin F.E., Ozyazar M., Pala A.S., Elmali A.D., Yilmaz B., Uygunoglu U., Bozluolcay M., Tuten A., Bingöl A., Hatipoglu E. Evaluation of Cognitive Functions in Gestational Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes. 2015;123:246–251. doi: 10.1055/s-0034-1395634. [DOI] [PubMed] [Google Scholar]
- 19.Camprubi R.M., Campoy C., Fernandez L.G., Lopez-Pedrosa J.M., Rueda R., Martin M.J. Maternal Diabetes and Cognitive Performance in the Offspring: A Systematic Review and Meta-Analysis. PLoS ONE. 2015;10:e0142583. doi: 10.1371/journal.pone.0142583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linder K., Schleger F., Kiefer-Schmidt I., Fritsche L., Kummel S., Heni M., Weiss M., Haring H.U., Preissl H., Fritsche A. Gestational Diabetes Impairs Human Fetal Postprandial Brain Activity. J. Clin. Endocrinol. Metab. 2015;100:4029–4036. doi: 10.1210/jc.2015-2692. [DOI] [PubMed] [Google Scholar]
- 21.Carson M.B., Liu C., Lu Y., Jia C., Lu H. A Disease Similarity Matrix Based on the Uniqueness of Shared Genes. BMC Med. Genom. 2017;10:26. doi: 10.1186/s12920-017-0265-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goh K.I., Cusick M.E., Valle D., Childs B., Vidal M., Barabási A.L. The Human Disease Network. Proc. Natl. Acad. Sci. USA. 2007;104:8685–8690. doi: 10.1073/pnas.0701361104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang M., Zhu C., Jacom A., Lu L.J., Jegg A.G. The Orphan Disease Networks. Am. J. Hum. Genet. 2011;88:755–766. doi: 10.1016/j.ajhg.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee A.J., Hiscock R.J., Wein P., Walker S.P., Permezel M. Gestational Diabetes Mellitus: Clinical Predictors and Long-Term Risk of Developing Type 2 Diabetes: A Retrospective Cohort Study Using Survival Analysis. Diabetes Care. 2007;30:878–883. doi: 10.2337/dc06-1816. [DOI] [PubMed] [Google Scholar]
- 25.Hopkins R., Shaver K., Weinstock R.S. Management of Adults with Diabetes and Cognitive Problems. Diabetes Spectr. 2016;29:224–237. doi: 10.2337/ds16-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spauwen P.J.J., van Eupen M.G.A., Köhler S., Stehouwer C.D.A., Verhey F.R.J., van der Kallen C.J.H., Sep S.J.S., Koster A., Schaper N.C., Dagnelie P.C., et al. Associations of Advanced Glycation End-Products with Cognitive Functions in Individuals with and without Type 2 Diabetes: The Maastricht Study. J. Clin. Endocrinol. Metab. 2015;100:951–960. doi: 10.1210/jc.2014-2754. [DOI] [PubMed] [Google Scholar]
- 27.Gorelick P.B., Scuteri A., Black S.E., Decarli C., Greenberg S.M., Iadecola C., Launer L.J., Laurent S., Lopez O.L., Nyenhuis D., et al. Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–2713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dorsemans A.C., Couret D., Hoarau A., Meilhac O., d’Hellencourt C.L., Diotel N. Diabetes, Adult Neurogenesis and Brain Remodeling: New Insights from Rodent and Zebrafish Models. Neurogenesis (Austin) 2017;4:e1281862. doi: 10.1080/23262133.2017.1281862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sochocka M., Diniz B.S., Leszek J. Inflammatory Response in the Cns: Friend or Foe? Mol. Neurobiol. 2017;54:8071–8089. doi: 10.1007/s12035-016-0297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Francis P.T., Palmer A.M., Snape M., Wilcock G.K. The Cholinergic Hypothesis of Alzheimer’s Disease: A. Review of Progress. J. Neurol. Neurosurg. Psychiatry. 1999;66:137–147. doi: 10.1136/jnnp.66.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saltiel A.R., Kahn C.R. Insulin Signalling and the Regulation of Glucose and Lipid Metabolism. Nature. 2001;414:799. doi: 10.1038/414799a. [DOI] [PubMed] [Google Scholar]
- 32.Grillo C.A., Piroli G.G., Lawrence R.C., Wrighten S.A., Green A.J., Wilson S.P., Sakai R.R., Kelly S.J., Wilson M.A., Mott D.D., et al. Hippocampal Insulin Resistance Impairs Spatial Learning and Synaptic Plasticity. Diabetes. 2015;64:3927–3936. doi: 10.2337/db15-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Talbot K., Wang H.Y., Kazi H., Han L.Y., Bakshi K.P., Stucky A., Fuino R.L., Kawaguchi K.R., Samoyedny A.J., Wilson R.S. Demonstrated Brain Insulin Resistance in Alzheimer’s Disease Patients Is Associated with Igf-1 Resistance, Irs-1 Dysregulation, and Cognitive Decline. J. Clin. Investig. 2012;122:1316–1338. doi: 10.1172/JCI59903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tello P.S., Matamoros A.O., Arias C. Gsk3 Function in the Brain during Development, Neuronal Plasticity, and Neurodegeneration. Int. J. Alzheimer’s Dis. 2011;2011 doi: 10.4061/2011/189728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boucher J., Kleinridders A., Kahn C.R. Insulin Receptor Signaling in Normal and Insulin-Resistant States. Cold Spring Harb. Perspect. Biol. 2014;6 doi: 10.1101/cshperspect.a009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao W., Chen H., Xu H., Moore E., Meiri N., Quon M.J., Alkon D.L. Brain Insulin Receptors and Spatial Memory. Correlated Changes in Gene Expression, Tyrosine Phosphorylation, and Signaling Molecules in the Hippocampus of Water Maze Trained Rats. J. Biol. Chem. 1999;274:34893–34902. doi: 10.1074/jbc.274.49.34893. [DOI] [PubMed] [Google Scholar]
- 37.Droge W. Free Radicals in the Physiological Control of Cell Function. Physiol. Rev. 2002;82:47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 38.De la Monte S.M., Wands J.R. Molecular Indices of Oxidative Stress and Mitochondrial Dysfunction Occur Early and Often Progress with Severity of Alzheimer’s Disease. J. Alzheimer’s Dis. 2006;9:167–181. doi: 10.3233/JAD-2006-9209. [DOI] [PubMed] [Google Scholar]
- 39.Karacay O., Sepici-Dincel A., Karcaaltincaba D., Sahin D., Yalvaç S., Akyol M., Kandemir O., Altan N. A Quantitative Evaluation of Total Antioxidant Status and Oxidative Stress Markers in Preeclampsia and Gestational Diabetic Patients in 24–36 Weeks of Gestation. Diabetes Res. Clin. Pract. 2010;89:231–238. doi: 10.1016/j.diabres.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 40.Liu B., Chen Y., St Clair D.K. Ros and P53: A Versatile Partnership. Free Radic. Biol. Med. 2008;44:1529–1535. doi: 10.1016/j.freeradbiomed.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muriach M., Flores-Bellver M., Francisco J.R., Jorge M.B. Diabetes and the Brain: Oxidative Stress, Inflammation, and Autophagy. Oxid. Med. Cell. Longev. 2014;2014 doi: 10.1155/2014/102158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pinheiro L., de Melo A.D., Andreazzi A.E., de Caires Júnior L.C., Costa M., Gonzalez Garcia M.R. Protocol of Insulin Therapy for Streptozotocin-Diabetic Rats Based on a Study of Food Ingestion and Glycemic Variation. Scand. J. Lab. Anim. Sci. 2011;38:117–127. [Google Scholar]
- 43.Yan H., Harding J.J. Glycation-Induced Inactivation and Loss of Antigenicity of Catalase and Superoxide Dismutase. Biochem. J. 1997;328:599–605. doi: 10.1042/bj3280599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sözmen E.Y., Sözmen B., Delen Y., Onat T. Catalase/Superoxide Dismutase (Sod) and Catalase/Paraoxonase (Pon) Ratios May Implicate Poor Glycemic Control. Arch. Med. Res. 2001;32:283–287. doi: 10.1016/S0188-4409(01)00285-5. [DOI] [PubMed] [Google Scholar]
- 45.Aziz S.H.A., John C.M., Yusof N.I.S.M., Nordin M., Ramasamy R., Adam A., Fauzi F.M. Animal Model of Gestational Diabetes Mellitus with Pathophysiological Resemblance to the Human Condition Induced by Multiple Factors (Nutritional, Pharmacological, and Stress) in Rats. BioMed Res. Int. 2016;2016 doi: 10.1155/2016/9704607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Giacco F., Brownlee M. Oxidative Stress and Diabetic Complications. Circ. Res. 2010;107:1058–1070. doi: 10.1161/CIRCRESAHA.110.223545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Butterfield D.A., Di Domenico F., Barone E. Elevated Risk of Type 2 Diabetes for Development of Alzheimer Disease: A Key Role for Oxidative Stress in Brain. Biochim. et Biophys. Acta (BBA)-Mol. Basis Dis. 2014;1842:1693–1706. doi: 10.1016/j.bbadis.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lobo V., Patil A., Phatak A., Chandra N. Free Radicals, Antioxidants and Functional Foods: Impact on Human Health. Pharm. Rev. 2010;4:118. doi: 10.4103/0973-7847.70902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eckert A., Schmitt K., Götz J. Mitochondrial Dysfunction-the Beginning of the End in Alzheimer’s Disease? Separate and Synergistic Modes of Tau and Amyloid-Β Toxicity. Alzheimer’s Res. Ther. 2011;3:15. doi: 10.1186/alzrt74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moreira P.I., Carvalho C., Zhu X., Smith M.A., Perry G. Mitochondrial Dysfunction Is a Trigger of Alzheimer’s Disease Pathophysiology. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2010;1802:2–10. doi: 10.1016/j.bbadis.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 51.Valla J., Schneider L., Niedzielko T., Coon K.D., Caselli R., Sabbagh M.N., Ahern G.L., Baxter L., Alexander G., Walker D.G. Impaired Platelet Mitochondrial Activity in Alzheimer’s Disease and Mild Cognitive Impairment. Mitochondrion. 2006;6:323–330. doi: 10.1016/j.mito.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Readnower R.D., Sauerbeck A.D., Sullivan P.G. Mitochondria, Amyloid Β, and Alzheimer’s Disease. Int. J. Alzheimer’s Dis. 2011;2011:104545. doi: 10.4061/2011/104545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abell S.K., De Courten B., Boyle J.A., Teede H.J. Inflammatory and Other Biomarkers: Role in Pathophysiology and Prediction of Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2015;16:13442–13473. doi: 10.3390/ijms160613442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chung C.C., Pimentel D., Jor’dan A.J., Hao Y., Milberg W., Novak V. Inflammation-Associated Declines in Cerebral Vasoreactivity and Cognition in Type 2 Diabetes. Neurology. 2015;85:450–458. doi: 10.1212/WNL.0000000000001820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grigsby J.G., Cardona S.M., Pouw C.E., Muniz A., Mendiola A.S., Tsin A.T., Allen D.M., Cardona A.E. The Role of Microglia in Diabetic Retinopathy. J. Ophthalmol. 2014;2014 doi: 10.1155/2014/705783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kuhad A., Bishnoi M., Tiwari V., Chopra K. Suppression of Nf-Κβ Signaling Pathway by Tocotrienol Can Prevent Diabetes Associated Cognitive Deficits. Pharmacol. Biochem. Behav. 2009;92:251–259. doi: 10.1016/j.pbb.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 57.Kirwan J.P., Hauguel-De Mouzon S., Lepercq J., Challier J.C., Huston-Presley L., Friedman J.E., Kalhan S.C., Catalano P.M. Tnf-A Is a Predictor of Insulin Resistance in Human Pregnancy. Diabetes. 2002;51:2207–2213. doi: 10.2337/diabetes.51.7.2207. [DOI] [PubMed] [Google Scholar]
- 58.Catalano P.M., Nizielski S.E., Shao J., Preston L., Qiao L., Friedman J.E. Downregulated Irs-1 and Ppargamma in Obese Women with Gestational Diabetes: Relationship to Ffa during Pregnancy. Am. J. Physiol. Endocrinol. Metab. 2002;282:E522–E533. doi: 10.1152/ajpendo.00124.2001. [DOI] [PubMed] [Google Scholar]
- 59.Sawada M., Sawada H., Nagatsu T. Effects of Aging on Neuroprotective and Neurotoxic Properties of Microglia in Neurodegenerative Diseases. Neurodegener. Dis. 2008;5:254–256. doi: 10.1159/000113717. [DOI] [PubMed] [Google Scholar]
- 60.Wojtera M., Sikorska B., Sobow T. Microglial Cells in Neurodegenerative Disorders. Folia Neuropathol. 2005;43:311–321. [PubMed] [Google Scholar]
- 61.Kreutzberg G.W. Microglia: A Sensor for Pathological Events in the Cns. Trends Neurosci. 1996;19:312–318. doi: 10.1016/0166-2236(96)10049-7. [DOI] [PubMed] [Google Scholar]
- 62.Song I.-U., Chung S.-W., Kim Y.-D., Maeng L.-S. Relationship between the Hs-Crp as Non-Specific Biomarker and Alzheimer’s Disease According to Aging Process. Int. J. Med. Sci. 2015;12:613–617. doi: 10.7150/ijms.12742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Denner L.A., Rodriguez-Rivera J., Haidacher S.J., Jahrling J.B., Carmical J.R., Hernandez C.M., Zhao Y., Sadygov R.G., Starkey J.M., Spratt H. Cognitive Enhancement with Rosiglitazone Links the Hippocampal Pparγ and Erk Mapk Signaling Pathways. J. Neurosci. Off. J. Soc. Neurosci. 2012;32:16725–16735. doi: 10.1523/JNEUROSCI.2153-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rodriguez-Rivera J., Denner L., Dineley K.T. Rosiglitazone Reversal of Tg2576 Cognitive Deficits Is Independent of Peripheral Gluco-Regulatory Status. Behav. Brain Res. 2011;216:255–261. doi: 10.1016/j.bbr.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zheng F., Yan L., Yang Z., Zhong B., Xie W. Hba1c, Diabetes and Cognitive Decline: The English Longitudinal Study of Ageing. Diabetologia. 2018;61:839–848. doi: 10.1007/s00125-017-4541-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gupta A., Singh A., Deka R.C., Gupta R., Jha R. To Investigate Role of Glycosylated Hemoglobin (Hba1c) as a Biomarker for Prediction of Dementia and Cognitive Dysfunction in Type 2 Diabetic Patients. J. Alzheimers Dis. Parkinsonism. 2018;8:437. doi: 10.4172/2161-0460.1000437. [DOI] [Google Scholar]
- 67.Wang P., Huang R., Lu S., Xia W., Cai R., Sun H., Wang S. Rage and Ages in Mild Cognitive Impairment of Diabetic Patients: A Cross-Sectional Study. PLoS ONE. 2016;11:e0145521. doi: 10.1371/journal.pone.0145521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mayeda E.R., Haan M.N., Neuhaus J., Yaffe K., Knopman D.S., Sharrett A.R., Griswold M.E., Mosley T.H. Type 2 Diabetes and Cognitive Decline over 14 Years in Middle-Aged African Americans and Whites: The Aric Brain Mri Study. Neuroepidemiology. 2014;43:220–227. doi: 10.1159/000366506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Luchsinger J.A. Type 2 Diabetes and Cognitive Impairment: Linking Mechanisms. J. Alzheimers Dis. 2012;30:S185–S198. doi: 10.3233/JAD-2012-111433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Craft S. Insulin Resistance and Alzheimer’s Disease Pathogenesis: Potential Mechanisms and Implications for Treatment. Curr. Alzheimer Res. 2007;4:147–152. doi: 10.2174/156720507780362137. [DOI] [PubMed] [Google Scholar]
- 71.Dineley K.T., Jahrling J.B., Denner L. Insulin Resistance in Alzheimer’s Disease. Neurobiol. Dis. 2014;72:92–103. doi: 10.1016/j.nbd.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Diehl T., Mullins R., Kapogiannis D. Insulin Resistance in Alzheimer’s Disease. Transl. Res. 2017;183:26–40. doi: 10.1016/j.trsl.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ho L., Qin W., Pompl P.N., Xiang Z., Wang J., Zhao Z., Peng Y., Cambareri G., Rocher A., Mobbs C.V., et al. Diet-Induced Insulin Resistance Promotes Amyloidosis in a Transgenic Mouse Model of Alzheimer’s Disease. FASEB J. 2004;18:902–904. doi: 10.1096/fj.03-0978fje. [DOI] [PubMed] [Google Scholar]
- 74.Al-Noaemi M.C., Shalayel M.H.F. Gestational Diabetes. InTech; Rijeka, Croatia: 2011. Pathophysiology of Gestational Diabetes Mellitus: The Past, the Present and the Future. [Google Scholar]
- 75.de la Monte M.S. Brain Insulin Resistance and Deficiency as Therapeutic Targets in Alzheimer’s Disease. Curr. Alzheimer Res. 2012;9:35–66. doi: 10.2174/156720512799015037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Johnston A.M., Pirola L., Van Obberghen E. Molecular Mechanisms of Insulin Receptor Substrate Protein-Mediated Modulation of Insulin Signalling. FEBS Lett. 2003;546:32–36. doi: 10.1016/S0014-5793(03)00438-1. [DOI] [PubMed] [Google Scholar]
- 77.Šalković-Petrišić M., Zdravko L. Insulin Resistant Brain State and Its Link to Diabetes Mellitus. Period. Biol. 2005;107:137–146. [Google Scholar]
- 78.Nees S., Weiss D.R., Senftl A., Knott M., Förch S., Schnurr M., Weyrich P., Juchem G. Isolation, Bulk Cultivation, and Characterization of Coronary Microvascular Pericytes: The Second Most Frequent Myocardial Cell Type in Vitro. Am. J. Physiol. Heart Circ. Physiol. 2012;302:H69–H84. doi: 10.1152/ajpheart.00359.2011. [DOI] [PubMed] [Google Scholar]
- 79.Ertl L., Sanftenberg L., Schelling J. Medical Certificates and Examinations in Family Doctor’s Office. Indications, Barriers and Relevance of Standardization. MMW Fortschr. Med. 2016;158:1–4. doi: 10.1007/s15006-016-9052-9. [DOI] [PubMed] [Google Scholar]
- 80.Bosco D., Fava A., Plastino M., Montalcini T., Pujia A. Possible Implications of Insulin Resistance and Glucose Metabolism in Alzheimer’s Disease Pathogenesis. J. Cell. Mol. Med. 2011;15:1807–1821. doi: 10.1111/j.1582-4934.2011.01318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Solano D.C., Sironi M., Bonfini C., Solerte S.B., Govoni S., Racchi M. Insulin Regulates Soluble Amyloid Precursor Protein Release Via Phosphatidyl Inositol 3 Kinase-Dependent Pathway. FASEB J. 2000;14:1015–1022. doi: 10.1096/fasebj.14.7.1015. [DOI] [PubMed] [Google Scholar]
- 82.Gasparini L., Gouras G.K., Wang R., Gross R.S., Beal M.F., Greengard P., Xu H. Stimulation of Β-Amyloid Precursor Protein Trafficking by Insulin Reduces Intraneuronal Β-Amyloid and Requires Mitogen-Activated Protein Kinase Signaling. J. Neurosci. 2001;21:2561–2570. doi: 10.1523/JNEUROSCI.21-08-02561.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mattson M.P. Cellular Actions of Beta-Amyloid Precursor Protein and Its Soluble and Fibrillogenic Derivatives. Physiol. Rev. 1997;77:1081–1132. doi: 10.1152/physrev.1997.77.4.1081. [DOI] [PubMed] [Google Scholar]
- 84.Vincent B., Govitrapong P. Activation of the A-Secretase Processing of Aβpp as a Therapeutic Approach in Alzheimer’s Disease. J. Alzheimer’s Dis. 2011;24:75–94. doi: 10.3233/JAD-2011-110218. [DOI] [PubMed] [Google Scholar]
- 85.Ferreira S.T., Klein W.L. The Aβ Oligomer Hypothesis for Synapse Failure and Memory Loss in Alzheimer’s Disease. Neurobiol. Learn. Mem. 2011;96:529–543. doi: 10.1016/j.nlm.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Su F., Shu H., Ye Q., Wang Z., Xie C., Yuan B., Zhang Z., Bai F. Brain Insulin Resistance Deteriorates Cognition by Altering the Topological Features of Brain Networks. NeuroImage Clin. 2017;13:280–287. doi: 10.1016/j.nicl.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pivarnik J.M., Stein A.D., Rivera J.M. Effect of Pregnancy on Heart Rate/Oxygen Consumption Calibration Curves. Med. Sci. Sports Exerc. 2002;34:750–755. doi: 10.1097/00005768-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 88.Li H., Yin Q., Li N., Ouyang Z., Zhong M. Plasma Markers of Oxidative Stress in Patients with Gestational Diabetes Mellitus in the Second and Third Trimester. Obs. Gynecol. Int. 2016;2016 doi: 10.1155/2016/3865454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhu C., Yang H., Geng Q., Ma Q., Long Y., Zhou C., Chen M. Association of Oxidative Stress Biomarkers with Gestational Diabetes Mellitus in Pregnant Women: A Case-Control Study. PLoS ONE. 2015;10:e0126490. doi: 10.1371/journal.pone.0126490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Genc S., Kusku-Kiraz Z., Dervisoglu E., Oztop N., Dinccag N., Gurdol F. The Relation of Oxidative Stress Biomarkers with Proinflammatory Cytokines in Gestational Diabetes. Clin. Investig. 2017;7:44–48. doi: 10.4172/Clinical-Investigation.1000110. [DOI] [Google Scholar]
- 91.Pan H.Z., Zhang L., Guo M.Y., Sui H., Li H., Wu W.H., Qu N.Q., Liang M.H., Chang D. The Oxidative Stress Status in Diabetes Mellitus and Diabetic Nephropathy. Acta Diabetol. 2010;47:71–76. doi: 10.1007/s00592-009-0128-1. [DOI] [PubMed] [Google Scholar]
- 92.Peerapatdit T., Sriratanasathavorn C. Lipid Peroxidation and Antioxidant Enzyme Activities in Erythrocytes of Type 2 Diabetic Patients. J. Med. Assoc. Thai. 2010;93:682–693. [PubMed] [Google Scholar]
- 93.Chang C., Hsieh C.-J., Huang J.-C., Huang I.-C. Acute and Chronic Fluctuations in Blood Glucose Levels Can Increase Oxidative Stress in Type 2 Diabetes Mellitus. Acta Diabetol. 2012;49:171–177. doi: 10.1007/s00592-012-0398-x. [DOI] [PubMed] [Google Scholar]
- 94.Ismail H.M., Scapozza L., Ruegg U.T., Dorchies O.M. Diapocynin, a Dimer of the Nadph Oxidase Inhibitor Apocynin, Reduces Ros Production and Prevents Force Loss in Eccentrically Contracting Dystrophic Muscle. PLoS ONE. 2014;9:e110708. doi: 10.1371/journal.pone.0110708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coughlan M.T., Vervaart P.P., Permezel M., Georgiou H.M., Rice G.E. Altered Placental Oxidative Stress Status in Gestational Diabetes Mellitus. Placenta. 2004;25:78–84. doi: 10.1016/S0143-4004(03)00183-8. [DOI] [PubMed] [Google Scholar]
- 96.Pistell P.J., Morrison C.D., Gupta S., Knight A.G., Keller J.N., Ingram D.K., Bruce-Keller A.J. Cognitive Impairment Following High Fat Diet Consumption Is Associated with Brain Inflammation. J. Neuroimmunol. 2010;219:25–32. doi: 10.1016/j.jneuroim.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.De la Monte S.M., Luong T., Neely T.R., Robinson D., Wands J.R. Mitochondrial DNA Damage as a Mechanism of Cell Loss in Alzheimer’s Disease. Lab. Investig. 2000;80:1323. doi: 10.1038/labinvest.3780140. [DOI] [PubMed] [Google Scholar]
- 98.Kim J., Wei Y., James R.S. Role of Mitochondrial Dysfunction in Insulin Resistance. Circ. Res. 2008;102:401–414. doi: 10.1161/CIRCRESAHA.107.165472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cheng Z., Tseng Y., White M.F. Insulin Signaling Meets Mitochondria in Metabolism. Trends Endocrinol. Metab. 2010;21:589–598. doi: 10.1016/j.tem.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Larsen R., Gouveia Z., Miguel P.S., Gozzelino R. Heme Cytotoxicity and the Pathogenesis of Immune-Mediated Inflammatory Diseases. Front. Pharm. 2012;3:77. doi: 10.3389/fphar.2012.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Correia S.C., Santos R.X., Santos M.S., Casadesus G., Lamanna J.C., Perry G., Smith M.A., Moreira P.I. Mitochondrial Abnormalities in a Streptozotocin-Induced Rat Model of Sporadic Alzheimer’s Disease. Curr. Alzheimer Res. 2013;10:406–419. doi: 10.2174/1567205011310040006. [DOI] [PubMed] [Google Scholar]
- 102.Merad-Boudia M., Nicole A., Santiard-Baron D., Saillé C., Ceballos-Picot I. Mitochondrial Impairment as an Early Event in the Process of Apoptosis Induced by Glutathione Depletion in Neuronal Cells: Relevance to Parkinson’s Disease. Biochem. Pharmacol. 1998;56:645–655. doi: 10.1016/S0006-2952(97)00647-3. [DOI] [PubMed] [Google Scholar]
- 103.Alvarez L.A., Kovačič L., Rodríguez J., Gosemann J.H., Kubica M., Pircalabioru G.G., Friedmacher F., Cean A., Ghişe A., Sărăndan M.B. Nadph Oxidase-Derived H2o2 Subverts Pathogen Signaling by Oxidative Phosphotyrosine Conversion to Pb-Dopa. Proc. Natl. Acad. Sci. USA. 2016;113:10406–10411. doi: 10.1073/pnas.1605443113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rosales-Corral S., Tan D.-X., Manchester L., Reiter R.J. Diabetes and Alzheimer Disease, Two Overlapping Pathologies with the Same Background: Oxidative Stress. Oxid. Med. Cell. Longev. 2015;2015:14. doi: 10.1155/2015/985845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lee A.Y., Chung S.S. Contributions of Polyol Pathway to Oxidative Stress in Diabetic Cataract. FASEB J. 1999;1999:23–30. doi: 10.1096/fasebj.13.1.23. [DOI] [PubMed] [Google Scholar]
- 106.Pantham P., Aye I.L., Powell T.L. Inflammation in Maternal Obesity and Gestational Diabetes Mellitus. Placenta. 2015;36:709–715. doi: 10.1016/j.placenta.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gueuvoghlanian-Silva B.Y., Torloni M.R., Mattar R., de Oliveira L.S., Scomparini F.B., Nakamura M.U., Daher S. Profile of Inflammatory Mediators in Gestational Diabetes Mellitus: Phenotype and Genotype. Am. J. Reprod. Immunol. 2012;67:241–250. doi: 10.1111/j.1600-0897.2011.01090.x. [DOI] [PubMed] [Google Scholar]
- 108.White S.L., Pasupathy D., Sattar N., Nelson S.M., Lawlor D.A., Briley A.L., Seed P.T., Welsh P., Poston L., UPBEAT Consortium Metabolic Profiling of Gestational Diabetes in Obese Women during Pregnancy. Diabetologia. 2017;60:1903–1912. doi: 10.1007/s00125-017-4380-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ryan A.S. Inflammatory Markers in Older Women with a History of Gestational Diabetes and the Effects of Weight Loss. J. Diabetes Res. 2018;2018:7. doi: 10.1155/2018/5172091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Korkmazer E., Solak N. Correlation between Inflammatory Markers and Insulin Resistance in Pregnancy. J. Obs. Gynaecol. 2015;35:142–145. doi: 10.3109/01443615.2014.948408. [DOI] [PubMed] [Google Scholar]
- 111.Gregor M.F., Hotamisligil G.S. Inflammatory Mechanisms in Obesity. Annu. Rev. Immunol. 2011;29:415–445. doi: 10.1146/annurev-immunol-031210-101322. [DOI] [PubMed] [Google Scholar]
- 112.Gorska-Ciebiada M., Saryusz-Wolska M., Borkowska A., Ciebiada M., Loba J. Serum Levels of Inflammatory Markers in Depressed Elderly Patients with Diabetes and Mild Cognitive Impairment. PLoS ONE. 2015;10:e0120433. doi: 10.1371/journal.pone.0120433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Magaki S., Mueller C., Dickson C., Kirsch W. Increased Production of Inflammatory Cytokines in Mild Cognitive Impairment. Exp. Gerontol. 2007;42:233–240. doi: 10.1016/j.exger.2006.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.McGuire S.O., Ling Z.D., Lipton J.W., Sortwell C.E., Collier T.J., Carvey P.M. Tumor Necrosis Factor A Is Toxic to Embryonic Mesencephalic Dopamine Neurons. Exp. Neurol. 2001;169:219–230. doi: 10.1006/exnr.2001.7688. [DOI] [PubMed] [Google Scholar]
- 115.Boje K.M., Arora P.K. Microglial-Produced Nitric Oxide and Reactive Nitrogen Oxides Mediate Neuronal Cell Death. Brain Res. 1992;587:250–256. doi: 10.1016/0006-8993(92)91004-X. [DOI] [PubMed] [Google Scholar]
- 116.Allan S.M., Rothwell N.J. Inflammation in Central Nervous System Injury. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2003;358:1669–1677. doi: 10.1098/rstb.2003.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Goedert M. Neuronal Localization of Amyloid Beta Protein Precursor Mrna in Normal Human Brain and in Alzheimer’s Disease. EMBO J. 1987;6:3627–3632. doi: 10.1002/j.1460-2075.1987.tb02694.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sinha S., Lieberburg I. Cellular Mechanisms of Β-Amyloid Production and Secretion. Proc. Natl. Acad. Sci. USA. 1999;96:11049–11053. doi: 10.1073/pnas.96.20.11049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gorska-Ciebiada M., Saryusz-Wolska M., Borkowska A., Ciebiada M., Loba J. Adiponectin, Leptin and Il-1 Β in Elderly Diabetic Patients with Mild Cognitive Impairment. Metab. Brain Dis. 2016;31:257–266. doi: 10.1007/s11011-015-9739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tsuchida A., Yamauchi T., Kadowaki T. Nuclear Receptors as Targets for Drug Development: Molecular Mechanisms for Regulation of Obesity and Insulin Resistance by Peroxisome Proliferator-Activated Receptor &Gamma, Creb-Binding Protein, and Adiponectin. J. Pharmacol. Sci. 2005;97:164–170. doi: 10.1254/jphs.fmj04008x2. [DOI] [PubMed] [Google Scholar]
- 121.Al-Badri M.R., Zantout M.S., Azar S.T. The Role of Adipokines in Gestational Diabetes Mellitus. Ther. Adv. Endocrinol. Metab. 2015;6:103–108. doi: 10.1177/2042018815577039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Saini V.M., Yadav K.A., Jain A. Role of Leptin and Adiponectin in Gestational Diabetes Mellitus: A Study in a North Indian Tertiary Care Hospital. Int. J. Med. Update. 2015;10:11–14. doi: 10.4314/ijmu.v10i1.3. [DOI] [Google Scholar]
- 123.Yokota T., Oritani K., Takahashi I., Ishikawa J., Matsuyama A., Ouchi N., Kihara S., Funahashi T., Tenner A.J., Tomiyama Y., et al. Adiponectin, a New Member of the Family of Soluble Defense Collagens, Negatively Regulates the Growth of Myelomonocytic Progenitors and the Functions of Macrophages. Blood. 2000;96:1723–1732. [PubMed] [Google Scholar]
- 124.Racke M.K., Drew P.D. Ppars in Neuroinflammation. PPAR Res. 2008;2008:638356. doi: 10.1155/2008/638356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kim H.I., Ahn Y.H. Role of Peroxisome Proliferator-Activated Receptor-gamma in the Glucose-Sensing Apparatus of Liver and Β-Cells. Diabetes. 2004;53:S60–S65. doi: 10.2337/diabetes.53.2007.S60. [DOI] [PubMed] [Google Scholar]