If you fly frequently, there’s a good chance you’ve found yourself “bumped” from an overbooked flight.
Airlines overbook to boost occupancy rates. Higher occupancy rates maximize profits (Figure 1A) because a flight’s costs are generally fixed, based mainly on the price of fuel. An empty seat is a missed opportunity for revenue (1). When a flight is overbooked, many airlines use a “first come, first served” model. The first passengers to check in for the flight are guaranteed seats, while stragglers are vulnerable to bumping.
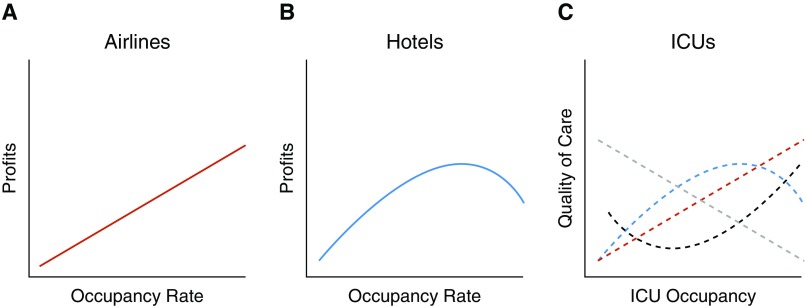
Figure 1.
Occupancy and value among airlines, hotels, and intensive care units (ICUs). (A) Profits increase linearly with occupancy rates for the airline industry. (B) Profits for the hotel industry increase until occupancy rates reach approximately 75% occupancy, at which point more staffing is required and profits decrease. (C) Four hypothesized examples of how ICU occupancy may influence the quality of care delivered to critically ill patients. Red dashed line: if an ICU always provides the highest-quality care in a hospital, then maximizing ICU occupancy improves quality of care. Gray dashed line: increasing ICU occupancy results in less attention for each additional patient. Blue dashed line: at a given point, ICU occupancy becomes overwhelming and quality of care suffers. Black dashed line: in an ICU with flexible staffing, the ICU provides close attention at low occupancy; at high occupancy, the ICU increases staffing to meet demand, but at medium occupancy, the ICU maintains staffing as if occupancy were low, resulting in poor quality of care.
Conversely, the hotel industry believes that 100% occupancy counterintuitively diminishes profits. A hotel’s costs are not as fixed as an airplane’s, as costs are tied directly to the number of rooms used. More rooms used means more staff is needed. Also, a hotel can more easily adjust staffing at times of high or low occupancy than an airline. Research from the hotel industry indicates that, on average, an occupancy rate of 75% is optimal because higher occupancy rates strain efficiency and decrease profits (Figure 1B) (2). Thus, hotels deliberately avoid reaching full capacity and need not be bound by a first come, first served policy, and whether you check into your room early or late makes little difference to them.
For both the airline and hotel industries, the ultimate goal is to maximize profits. Yet, to do so, each follows a different path. An intensive care unit (ICU), like an airplane or hotel, has a finite capacity. But rather than seeking to maximize profits, an ICU’s goal is to provide the best quality of care for critically ill patients. Which model, then, should intensivists use when deciding which patients are “critically ill” enough to receive care? Should ICUs operate like airlines, viewing an empty bed as a missed opportunity and thus maximizing occupancy on a first come, first served basis? Or should ICUs operate like hotels, identifying an inflection point at which too little occupancy is wasteful but too high occupancy strains the system, resulting in poor quality of care for patients and burnout for clinicians (3, 4)?
Several metrics aim to measure this inflection point, which is the balance between ICU bed supply and ICU demand—more technically known as ICU capacity strain (3). The term “capacity strain” sounds as if it was ripped straight from the handbook of a hospital administrator. So why should a clinician care about capacity strain? Numerous studies have demonstrated that capacity strain impacts how we use the ICU and the quality of care we provide (3). What we have lacked is consensus on the best way to measure capacity strain—by the number of available ICU beds, by how sick an ICU’s patients are, etc.
In this issue of AnnalsATS, Anesi and colleagues (pp. 1328–1335) provide key contributions toward identifying the best way to measure capacity strain (5). The investigators took four metrics commonly used to quantify strain—ICU occupancy, ICU turnover, ICU acuity, and ward occupancy—and examined which ones were predictive of ICU admission. For each of the four metrics, greater strain made it less likely that a patient would be admitted to the ICU. This is not surprising, given what we know about how capacity strain influences the way we use the ICU. However, after accounting for patient characteristics, only ICU occupancy was independently predictive of ICU admission.
The authors also sought to evaluate the impact of ICU occupancy on quality of care, as measured by mortality. They found that higher ICU occupancy was predictive of increased mortality among ward patients, but not ICU patients, with sepsis. The authors offered several hypotheses for this finding—most concerningly that perhaps under high-occupancy conditions, patients who might benefit from ICU care are instead triaged to the general ward. As exemplified in Figure 1C, ICU occupancy could impact quality of care in several ways, positively or negatively. This study depicts the association between ICU occupancy and quality of care as replicating the blue or gray lines, suggesting that higher ICU occupancy leads to lower quality of care.
The authors also demonstrated that when the ICU occupancy rate was greater than 70% (or fewer than five open ICU beds), the odds of ICU admission decreased linearly. This finding illustrates how sensitive we intensivists are to ICU bed availability. When several ICU beds are available, we may admit patients to the ICU who are not critically ill—our threshold for ICU admission may be too low. When there are few beds available, we may refuse admission to patients who are critically ill—our threshold may be too high (6). This study highlights that we have yet to determine which patients are particularly vulnerable to these system-level influences on ICU triage. Which patients would be admitted to the ICU under low-strain conditions but refused ICU care under high-strain conditions? Is ICU care best for these patients? Existing studies conflict regarding this so-called “discretionary” use of the ICU, with some revealing no difference in mortality while others suggest a benefit (7, 8).
This study presents several important questions that must be considered. First, how generalizable are these results to other ICUs? Although this was a multicenter study, all three hospitals were part of the same university hospital system, and prior studies have revealed that the prevalence (and likely the effects) of strain can differ substantially based on the clinical environment (9). Even within Anesi and colleagues’s study, ICU admission practices varied among the three hospitals. What, at the hospital or clinician level, motivates these differences remains uncertain. Second, what role should non-ICU care locations or care models play to reduce capacity strain? In this hospital system, intermediate care played a relatively minor role, and the extent to which ward-based critical-care consultations (e.g., involving rapid response teams) were used was unclear. Finally, the authors concluded that ICU occupancy is the most robust strain metric for future use, but the use of a single metric may inadequately capture the concept of strain. For instance, you might imagine situations where even though there are several open ICU beds, one or two extremely sick patients dominate the attention of the ICU clinicians and influence triage decisions regarding potential patients.
This study highlights what is perhaps another key difference between the airline and hotel industries: how unanticipated events are perceived. A customer getting bumped from a flight has become an everyday occurrence, with an expectation that the customer will be compensated and will wait for the next flight. For hotels, however, a customer with an existing reservation having no place to sleep may become a public relations nightmare. Where on this spectrum does refusal of ICU admission lie? For the intensivist, should refusing ICU care to a patient who might benefit be a routine part of the job, and what is an acceptable number of “bumped” patients?
Recent guidelines recommend that ICU triage be based on a patient’s potential to benefit from ICU care (10). This remains difficult to implement, for several reasons. First, there are no good ways to estimate ICU benefit. Second, clinicians are imperfect prognosticators (11). Third, intensivists face great uncertainty related to patient queuing—it is difficult to predict on a given day how many patients will be admitted, when they will arrive, or how critically ill they will be. For these reasons, ICUs tend to fill up like an overbooked airplane, on a first come, first served basis. Yet, this study underscores that the first come, first served model may be particularly prone to influence by factors such as capacity strain.
The search for the optimal ICU triage model continues. This model must take into account the relative value that we intensivists place on maintaining an empty bed (sometimes casually referred to as a “code bed”) versus providing ICU care to a patient who may or may not benefit from it (12). Perhaps the optimal ICU triage model could help us avoid “bumping” the wrong patient.
Supplementary Material
Acknowledgments
Acknowledgment
The author thanks Jack Iwashyna, Angie Fagerlin, Bob Dickson, and the Multidisciplinary Intensive Care Research Workgroup (MICReW) for their invaluable feedback on this manuscript.
Footnotes
Supported by National Institutes of Health (NIH) grant K23 HL140165.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Mack R, Jiang H, Peterson RM. Chicago, IL: The Boeing Company; 2013. A discussion of the capacity supply-demand balance within the global commercial air transport industry. [accessed 2018 Sep 11]. Available from: https://www.boeing.com/resources/boeingdotcom/commercial/about-our-market/assets/downloads/AirTransportCapacitySupplyDemandBalance.pdf. [Google Scholar]
- 2.Hotel News Now. Rael J. Maximizing hotel profitability potential; 2016 [accessed 2018 August 15]. Available from: http://hotelnewsnow.com/articles/88558/research-maximizing-hotel-profitability-potential.
- 3.Rewa OG, Stelfox HT, Ingolfsson A, Zygun DA, Featherstone R, Opgenorth D, et al. Indicators of intensive care unit capacity strain: a systematic review. Crit Care. 2018;22:86. doi: 10.1186/s13054-018-1975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akman O, Ozturk C, Bektas M, Ayar D, Armstrong MA. Job satisfaction and burnout among paediatric nurses. J Nurs Manag. 2016;24:923–933. doi: 10.1111/jonm.12399. [DOI] [PubMed] [Google Scholar]
- 5.Anesi GL, Liu VX, Gabler NB, Delgado MK, Kohn R, Weissman GE, et al. Associations of intensive care unit capacity strain with disposition and outcomes of patients with sepsis presenting to the emergency department. Ann Am Thorac Soc. 2018;15:1328–1335. doi: 10.1513/AnnalsATS.201804-241OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gooch RA, Kahn JM. ICU bed supply, utilization, and health care spending: an example of demand elasticity. JAMA. 2014;311:567–568. doi: 10.1001/jama.2013.283800. [DOI] [PubMed] [Google Scholar]
- 7.Stelfox HT, Hemmelgarn BR, Bagshaw SM, Gao S, Doig CJ, Nijssen-Jordan C, et al. Intensive care unit bed availability and outcomes for hospitalized patients with sudden clinical deterioration. Arch Intern Med. 2012;172:467–474. doi: 10.1001/archinternmed.2011.2315. [DOI] [PubMed] [Google Scholar]
- 8.Valley TS, Sjoding MW, Ryan AM, Iwashyna TJ, Cooke CR. Association of intensive care unit admission with mortality among older patients with pneumonia. JAMA. 2015;314:1272–1279. doi: 10.1001/jama.2015.11068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagshaw SM, Wang X, Zygun DA, Zuege D, Dodek P, Garland A, et al. Association between strained capacity and mortality among patients admitted to intensive care: a path-analysis modeling strategy. J Crit Care. 2018;43:81–87. doi: 10.1016/j.jcrc.2017.08.032. [DOI] [PubMed] [Google Scholar]
- 10.Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44:1553–1602. doi: 10.1097/CCM.0000000000001856. [DOI] [PubMed] [Google Scholar]
- 11.Detsky ME, Harhay MO, Bayard DF, Delman AM, Buehler AE, Kent SA, et al. Discriminative accuracy of physician and nurse predictions for survival and functional outcomes 6 months after an ICU admission. JAMA. 2017;317:2187–2195. doi: 10.1001/jama.2017.4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorunescu F, McClean SI, Millard PH. A queueing model for bed-occupancy management and planning of hospitals. J Oper Res Soc. 2002;53:19–24. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.