Abstract
Aim
To report a case of bilateral papillitis as the initial ophthalmologic presentation in a patient with complex medical history and multisystemic symptoms, eventually revealing a diagnosis of sarcoidosis.
Methods
Retrospective interventional case report.
Report
A 54-year-old Caucasian woman presented with bilateral decreased vision, photophobia and eye pain for a month. She was referred for evaluation of disc edema with questionable history of vitritis. She had a complicated medical history and systemic symptoms, including: multiple tick bites; focal neurologic symptoms including tingling, headache, numbness of fingers, and stiff neck; systemic immune disease with thyroid nodule; and chest strain, mild shortness of breath, and palpitations, leading to a large differential diagnosis. Further workup ruled out infectious diseases and multiple sclerosis. After chest imaging, she was finally diagnosed via biopsy with sarcoidosis. Therapy included combined high dose prednisone taper and ongoing methotrexate. Both ocular and systemic symptoms improved after treatment, but there was limited improvement of scotoma in the left eye.
Conclusion
This report provides a case for ophthalmologists for papillitis as the initial manifestation of sarcoidosis, but with various potential differential diagnoses during work up.
Keywords: Papillitis, Sarcoidosis, Differential diagnosis
This case highlights a 54-year-old woman with papillitis who presented with a complicated history and wide variety of systemic symptoms, creating a large differential diagnosis and challenging work up, ultimately resulting in a diagnosis of sarcoidosis via biopsy. The authors feel that papillitis is an underappreciated feature of ocular sarcoid.
1. Introduction
Optic neuritis (ON) and papillitis may be associated with a range of autoimmune and infectious diseases, including multiple sclerosis (MS).1 Most of the remaining cases are idiopathic.1,2
Sarcoidosis is a granulomatous disease of unknown origin, with pulmonary findings in more than 90% of patients.3 Although the lung is predominantly affected, virtually every organ may be involved, including skin, eye, brain, and abdominal organs.3 Frequently, extrapulmonary manifestations of the disease are the major cause of morbidity.4 Because sarcoidosis can involve any organ system, the clinical presentation is often variable.
Ocular involvement concerns about 25%–60% of patients with systemic sarcoidosis, while optic disc edema has been reported to be a less common event5; it is the opinion of the authors that this is a more common and underappreciated finding, and actually shifts our focus of diagnostic studies toward sarcoid when it is present. Here we report a case of decreased vision in both eyes related to papillitis with multiple systemic symptoms as the initial presentation of sarcoidosis. The purpose of this study is both to showcase a diagnostic approach to a complicated case of papillitis and/or ON when the initial differential diagnosis was vast, and to express our opinion on the underappreciated finding of optic nerve inflammation in ocular sarcoid, even when associated uveitis or retinal vasculitis are not present.
1.1. Case report
A 54-year-old Caucasian woman was referred for evaluation of suddenly decreased vision, light sensitivity and pain OU, but without significant worsening of pain with eye movement. Ocular and systemic complaints and symptoms included: chronic neck pain and stiffness, tension headaches, tingling, numbness of fingers, chest strain, mild shortness breath and heart palpitations for 6 months. She was diagnosed with posterior vitreous detachment OU and there was a question of subtle vitreous hemorrhage OD without other ocular symptoms two months prior, though the initial provider did not communicate certainty of the latter when questioned. One month before presentation, she noticed poor vision OS, extreme photophobia and pain OU and was diagnosed with disc edema OS and possible vitritis in addition to, again, subtle vitreous hemorrhage versus vitritis OD. Symptoms also included waxing and waning flashes and infrequent floaters. Thus, she was referred to our center for further evaluation. No systemic or local treatment had been performed prior to referral.
Magnetic resonance imaging (MRI) of the brain prior to presentation revealed a 2.0 cm extra-axial dural based lesion overlying and indenting the anterior right frontal lobe. The appearance was most suggestive of meningioma, with a differential that included metastatic disease. Degenerative disc disease was also seen. A second MRI was done and dural malignant lesion was ruled out per radiologist report.
Past medical history included laser in-situ keratomileusis (LASIK) surgery OU in 1995 with enhancement later. She also had a history of multiple tick bites, notably two bites one year prior with bull's eye rash, treated with doxycycline. She had a history of a recent thyroid nodule, without any other known autoimmune disease. Her family history was non-contributory, she had only ever lived in the United States, and owned a cat and a dog.
1.2. Examinations
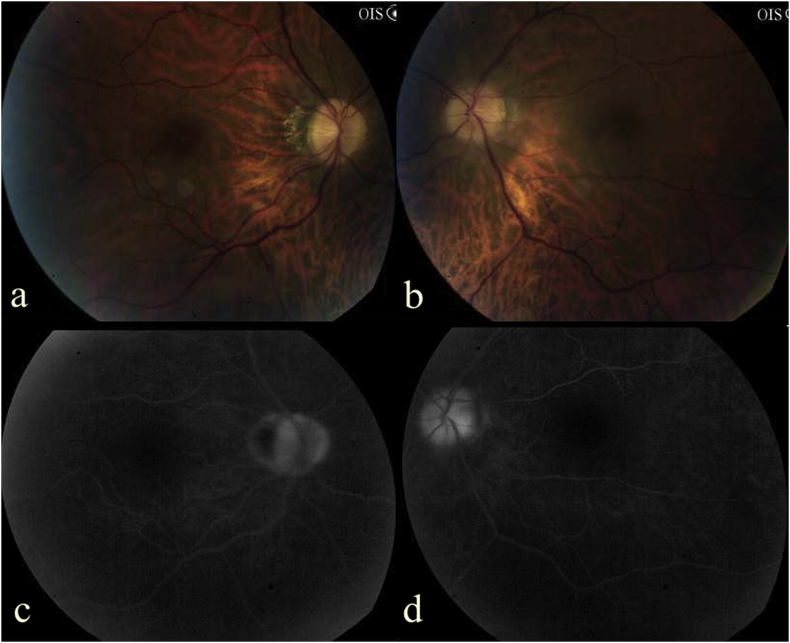
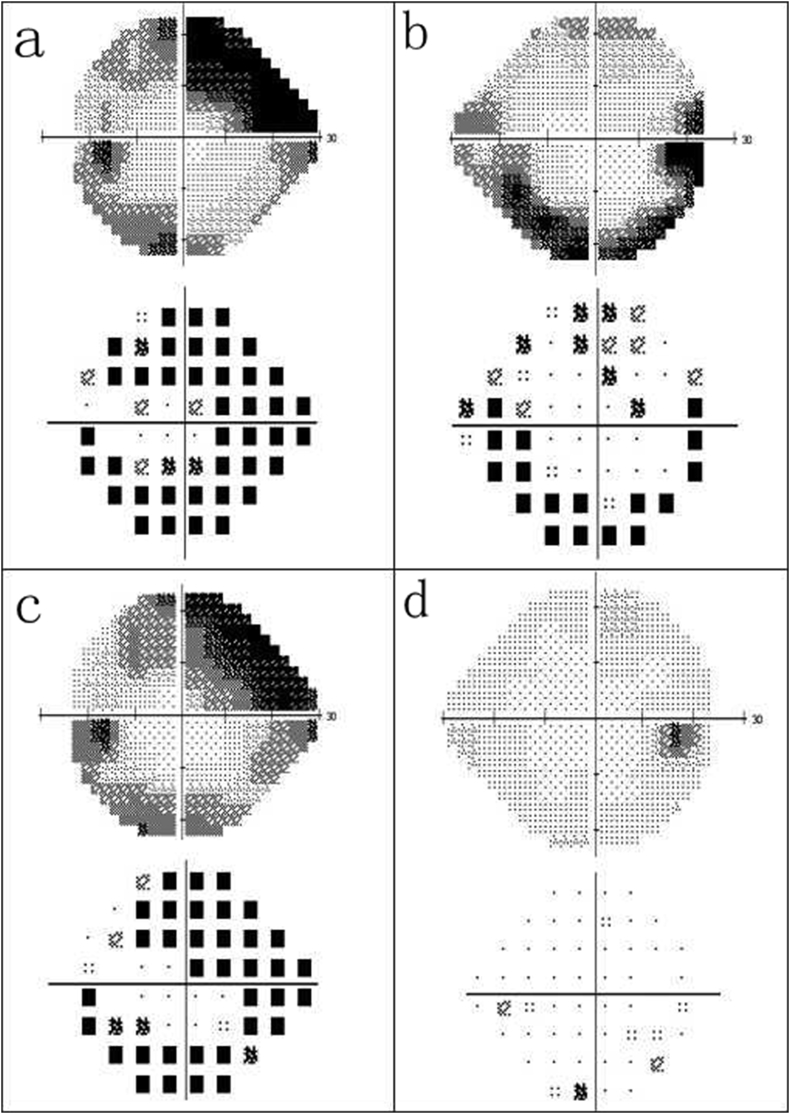
On examination at first presentation in our clinic, her best corrected visual acuity (BCVA) was 20/25 OD, 20/20 OS. Intraocular pressure was 12 mm Hg OU. Relative afferent pupillary defect was present OS. Slit-lamp examination revealed no inflammation of anterior chamber or vitreous bilaterally. No vitreous hemorrhage was noted. Dilated fundus exam revealed disc fullness with peripapillary atrophy OD and 2 + disc edema OS with peripapillary atrophy (Fig. 1 a/b). Fundus fluorescein angiography (FFA) showed leakage and staining of optic disc OU, with no signs of vasculitis (Fig. 1 c/d). Automated perimetry showed arcuate defects OU, left greater than right. (Fig. 3 a/b).
Fig. 1.
Fundus photography (a/b) and fundus fluorescein angiography (c/d) at presentation. (a/b) At first visit, fundus photography shows disc fullness and peripapillary atrophy OD and 2 + disc edema OS with mild peripapillary atrophy. (c/d) Late stage of retinal fundus fluorescein angiography showed leakage and staining of optic disc OU, greater OS. No other significant findings were noted.
Fig. 3.
Humphrey visual field: (a/b) At first visit, perimetry revealed generalized reduction in sensitivity with arcuate defects OS > OD. (c/d) Two months after treatment, automated perimetry showed essential resolution of defects OD, and limited improvement of scotomas and generalized reduction OS.
Given a vast array of systemic findings and possible diagnoses, a large serologic panel was ordered. This showed increased total complement and mild anemia, while all other results were normal, including: angiotensin converting enzyme (ACE), C-reactive protein, rheumatoid factor, antinuclear antibodies, anti-neutrophil cytoplasmic antibody, lysozyme, and infectious studies (including for Lyme, tuberculosis, and syphilis). Microscopic urinalysis was also unremarkable.
Imaging was also requested at the initial visit. MRI orbit with and without gadolineum was ordered and revealed there was minimal asymmetric edema and enhancement within the intraconal portion of the left optic nerve with no evidence of associated demyelinating disease. The dural based lesion mentioned above was unchanged on this study.
With a suspicion of sarcoidosis and associated papillitis at the initial visit, a spiral computed tomography (CT) scan of the chest with contrast was also ordered and revealed mildly enlarged pretracheal and subcarinal lymph nodes measuring up to 1.2 cm, as well as borderline enlarged hilar adenopathy measuring up to 1.1 cm. Further evaluation by pulmonology was immediately requested and three months after her initial visit, histopathology of lymph node biopsy by her pulmonologist showed epithelioid histiocytes and multinuclear giant cells, confirming sarcoidosis.
Her palpitations were evaluated by a Holter monitor with reports showing intermittent tachycardia and no true arrhythmic issues. Thoracic CT-scan showed a stable thyroid nodule. This was monitored without further intervention by her endocrinologist and not felt to be involved in her symptoms.
1.3. Treatment
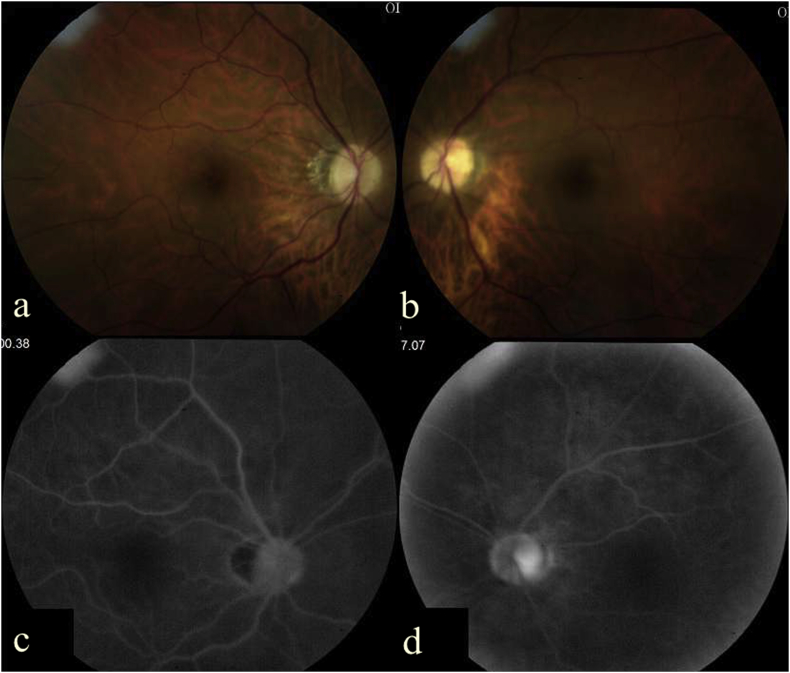
At the initial visit, because of concern of severe optic nerve inflammation, vision loss, and suspicion for sarcoid, the patient was promptly offered intravenous methylprednisolone 1g for 3 consecutive days, followed by oral prednisone 60 mg daily with weekly tapering. Close monitoring of her response following initial intravenous steroid showed there was no initial worsening of her optic neuropathy, so therapy was continued as planned. After steroid initiation, light sensitivity and pain OU improved progressively. Two months after treatment, BCVA was 20/20 OU, fundus examination revealed disc edema OU was resolved (Fig. 2 a/b). FFA showed no remaining leakage, but there was optic disc staining OS > OD in later frames (Fig. 2 c/d). Automated perimetry showed essential resolution of her scotoma OD and improved but persistent scotomas OS (Fig. 3 c/d).
Fig. 2.
Fundus photography (a/b) and fundus fluorescein angiography (c/d) two months after treatment. (a/b) Fundus photography revealed clear vitreous with disc pallor and resolved edema OU. (c/d) Late stage of retinal fundus fluorescein angiography showed no leakage but temporal optic disc staining OS.
Upon biopsy confirmation of sarcoidosis, she was started on weekly oral methotrexate 15 mg weekly with a folic acid supplement by her rheumatologist. Ocular symptoms had completely resolved except for residual visual defect OS. There was no active inflammation seen in both the anterior or vitreous chamber and no further signs of disc edema OU. Disc atrophy and pallor OU were later noted. During a 6 month follow-up, her eyes remained quiet on the above regimen.
2. Discussion
We feel this case of papillitis, which initially presented with several potential etiologies culminating in a final diagnosis of sarcoid, is extremely valuable to the ophthalmic community. It showcases how a complicated and severe presentation can be approached and managed successfully, also highlighting sarcoid as a potential diagnosis for these findings. In the case of our patient, our initial management approach was valuable not only in helping her maintain vision and prevent further loss of this, but also in improving the very concerning systemic features of disease. Given the large differential, presenting history, and findings, she may not have undergone the imaging necessary to solidify the diagnosis (spiral chest CT scan is not always pursued, rather chest radiography is typically recommended which we find to be much less helpful in evaluating for pulmonary sarcoid) nor received the initial care with intravenous steroid, and thus vision may not have been restored to the extent it was.
Sarcoidosis is a multisystemic disease, so suspicion is heightened by concomitant involvement of lungs, skin, lymph nodes, spleen, or eye. Uveitis is the most common manifestation of ocular sarcoidosis.6 Sarcoidosis reportedly contributes to a small amount of papillitis and ON patients in the experience of some.7 Another case series of 422 patients with histologically confirmed sarcoidosis, 112 (26%) had ocular and 31 (7%) neurological involvement, while four had “papilloedema” (1%).5 There are limited case reports on sarcoidosis with papillitis as the initial ophthalmologic presentation for sarcoidosis, and, in our experience, although optic nerve inflammation is often seen in sarcoid, it is very unusual to see ocular sarcoid involving optic nerve alone without uveitis or retinal vasculitis, although this has also been reported.5,6 A recent case was reported of inflammatory disc edema with anterior uveitis in a patient mimicking malignant hypertension, that was later attributed to sarcoidosis after transbronchial lung biopsy, which, again, highlights how this disease may present in a way that the provider may be drawn to other diagnoses first, but with correct suspicion and approach to work up, the final diagnosis can be made and proper management can be employed.8
Often times classic testing for sarcoid is unremarkable, as in this patient who had normal ACE and lysozyme levels. Clinical confirmation of sarcoidosis is most easily obtained by evidence of multisystem involvement, full examinations of the eyes, chest/brain radiography or MRI, histologic evidence of sarcoid in tissue, and response to corticosteroid challenge.5 Sarcoid was only confirmed after initial suspicion and request for chest CT scan, that then led to hilar lymph node biopsy. Response to therapy with corticosteroid and immunomodulatory therapy helped solidify our resolve that her papillitis was, in fact, secondary to systemic sarcoid.
This case also illustrates the importance of distinguishing the etiology of optic disc edema, although the diagnosis can be quite challenging, especially early in the disease or with limited organ involvement, or atypical disease. Despite her remaining visual field defect in the left eye, her other ocular and systemic symptoms, which caused significant distress to the patient and were of large concern to her primary care provider, improved or resolved completely without progression and have since remained in remission without dependence on high dose corticosteroid therapy.
In conclusion, this report provides an example where optic disc inflammation in the form of papillitis may present as the initial ophthalmologic presentation of sarcoidosis, and may help to finally diagnose multisystemic disease, despite prior clinical history suggesting a very wide differential diagnosis. Because of the potential for serious permanent vision loss, causes of optic disc edema should be aggressively evaluated with imaging, laboratories, prompt referral to appropriate specialists when needed, and quick initiation of therapy if possible. As a multisystem granulomatous disease, sarcoidosis has a wide range of presenting manifestations in different organs and tissues. Ophthalmologists should be mindful of this when forming a differential diagnosis for all forms of ocular inflammation, including papillitis, to aid the early diagnosis and management of these patients in an effort to prevent significant ocular complications.
Conflicts of interest
The authors have no conflicts of interest to report. Authorship: All authors attest that they meet the current ICMJE criteria for authorship.
Acknowledgements and disclosures
Funding: The authors have no proprietary or commercial interest in any materials discussed in this article. No funding sources exist for this original manuscript.
References
- 1.Optic Neuritis Study Group Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Arch Neurol. 2008;65(6):727–732. doi: 10.1001/archneur.65.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hickman S.J., Dalton C.M., Miller D.H., Plant G.T. Management of acute optic neuritis. Lancet. 2002;360(9349):1953–1962. doi: 10.1016/s0140-6736(02)11919-2. [DOI] [PubMed] [Google Scholar]
- 3.Wu J.J., Schiff K.R. Sarcoidosis. Am Fam Physician. 2004;70(2):312–322. [PubMed] [Google Scholar]
- 4.Judson M.A. Extrapulmonary sarcoidosis. Semin Respir Crit Care Med. 2007;28(1):83–101. doi: 10.1055/s-2007-970335. [DOI] [PubMed] [Google Scholar]
- 5.James D.G., Zatouroff M.A., Trowell J., Rose F.C. Papilloedema in sarcoidosis. Br J Ophthalmol. 1967;51(8):526–529. doi: 10.1136/bjo.51.8.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Austin A.L., Day L.T., Bishop F.M. Acute vision loss: a fuzzy presentation of sarcoidosis. J Emerg Med. 2013;44(4):e325–328. doi: 10.1016/j.jemermed.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Horwitz H., Friis T., Modvig S. Differential diagnoses to MS: experiences from an optic neuritis Clinic. J Neurol. 2014;261(1):98–105. doi: 10.1007/s00415-013-7166-x. [DOI] [PubMed] [Google Scholar]
- 8.Sharma A., Sagar V., Singla V. Inflammatory optic disc edema due to Sarcoidosis mimicking malignant hypertension. Int J Rheum Dis. 2013;21(4):895–899. doi: 10.1111/1756-185X.12507. [DOI] [PubMed] [Google Scholar]