Abstract
Background
Hidradenitis suppurativa (HS) and psoriasis are inflammatory skin diseases associated with obesity. Each disease is likely to impact the quality of life of patients, but the relative impact of each disease is unknown.
Objectives
This study aimed to determine whether skin disease or obesity is more distressing to obese patients who have either psoriasis or HS.
Methods
A cohort of obese patients with psoriasis and HS was surveyed using a time-trade-off utility. T-tests and regression analysis were used to compare differences in impact on quality of life between skin disease and obesity for patients with HS and psoriasis. Further analyses were adjusted for degree of obesity and severity of disease.
Results
A total of 79 subjects completed the survey. Obese patients with HS were heavier than patients with psoriasis (mean body mass index 38.1 kg/m2 vs. 34.9 kg/m2). Obese patients with either HS or psoriasis were both willing to trade a significantly higher proportion of their life to live without skin disease than to live at a normal weight (p = .01). This effect persisted after controlling for disease severity and weight. Patients with HS were willing to trade significantly more years of life to live at a normal weight than obese patients with psoriasis (14 vs. 7; p < .04).
Limitations
This was a small study conducted at an academic institution.
Conclusion
In this study population, obesity was more severe in patients with HS than in those with psoriasis. Even after controlling for relative severity, HS was more problematic for subjects in this study than weight when these conditions existed concomitantly.
Keywords: Hidradenitis suppurativa, obesity, psoriasis, quality of life
Introduction
Hidradenitis suppurativa (HS) and psoriasis are chronic inflammatory dermatologic disorders that are strongly associated with psychosocial and medical morbidity, including metabolic syndrome and obesity (Lebwohl and Callen, 2006, Shalom et al., 2015, Shlyankevich et al., 2014). Obesity is independently associated with prejudice at work and in public and has negative effects on interpersonal relationships. Obese women in particular are reported to have a decreased health-related quality of life (especially in self-esteem, sexual life, and physical functioning) and greater rates of depression compared with obese men (Kolotkin et al., 2008). Given the stigmatization of both obese patients and those with skin disease, obese patients with psoriasis experience more psychosocial comorbidities than their non-obese counterparts (Kim et al., 2014, Rand and Macgregor, 1991). However, the relative impairment caused by skin disease versus obesity in patients with psoriasis or HS has not been characterized.
To address this question, this survey study quantified the relative quality-of-life impairment associated with psoriasis or HS versus obesity through a cross-sectional time trade-off (TTO) utility measurement, which is a tool to assess patients’ willingness to exchange a portion of their future survival for disease-free living (Oppe et al., 2016).
Methods
This study was approved by the institutional review board at Partners for Massachusetts General Hospital. The subjects were recruited among adult patients with psoriasis and HS and with a body mass index (BMI) ≥ 30 who receive dermatological care at the Massachusetts General Hospital. Participants completed a self-administered questionnaire that consisted of a TTO utility, framed in 20- and 50-year remaining life expectancy, as well as symptoms, feelings, and daily activities pertaining to obesity and skin disease (psoriasis or HS).
For the utility analysis, each subject was asked how many of a theoretical 20 or 50 remaining years he or she would be willing to trade in return for disease-free living without HS or psoriasis versus obesity. A higher number of years indicated by the TTO suggested a lower quality of life in those living with HS or psoriasis. Additionally, BMI, Psoriasis Area Severity Index (PASI), and Hurley stage were measured for each subject. T-tests and regression analyses were performed to correlate TTO utility scores with measures of psoriasis or HS, respectively. Variables controlled in the regression analysis included age and sex. A level of statistical significance of p < .05 was chosen for the analysis.
The survey also included a modified six-question Dermatology Life Quality Index (DLQI) questionnaire to assess the psychosocial impact of skin disease and obesity separately in the following domains: personal feelings, daily activities, personal relationships/interactions, leisure, and work/school (Finlay and Khan, 1994). Responses were scored on a five-point Likert scale (possible score range: 1-5), and higher responses correlated with a poorer quality of life for a maximum of 30 points. Individual responses pertaining to each question were compared using T-tests, and a level of statistical significance of p < .05 was chosen for the analysis.
To elucidate a possible association between disease severity and the impact of obesity on the quality of life of subjects, a regression analysis of standardized disease severity and years willing to be traded for normal weight was performed. We grouped patients into three categories that corresponded with the average DLQI scores published for each disease (Sartorius et al., 2009, Vinding et al., 2014). The PASI scores were converted on a scale of 1 to 3 to correspond with the Hurley stage. PASI scores < 6 were compared with Hurley stage 1, scores > 6 but < 12 were compared with Hurley stage 2, and PASI scores > 12 were compared with Hurley stage 3.
Results
A total of 79 patients participated in the study: 47 patients with psoriasis (45% female) and 32 patients with HS (72% female). The average age of subjects with psoriasis was 51 years with a mean BMI of 34.9 kg/m2. The average age of patients with HS was 34 years with a mean BMI of 38.1 kg/m2 (Table 1).
Table 1.
Demographic information
| Hidradenitis suppurativa Mean (SD) |
Psoriasis Mean (SD) |
|||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| Number of patients | 9 | 23 | 32 | 26 | 21 | 47 |
| Age (years) | 40 (16) | 31 (7.2) | 34 (11) | 47 (13) | 56 (17) | 51 (16) |
| Body-mass index | 34.8 (6.3) | 39.7 (9.5) | 38.1 (8.8) | 34.9 (4.4) | 34.9 (5) | 34.9 (4.6) |
| Body surface area or areas involved | 4.1 (2.3) | 3.8 (2.7) | 3.9 (2.6) | 15% (17%) | 14% (12%) | 15% (15%) |
| Age at time of onset | 24 (12.5) | 20 (7.5) | 21.3 (9.4) | 29 (13) | 38 (12) | 33 (13) |
| Age at time of diagnosis | 32 (13) | 28 (8) | 28 (10) | 29 (13) | 38 (12) | 33 (13) |
| PASI score | 9.1 (8.7) | 8.4 (7.6) | 8.8 (8.2) | |||
| Clinical severity: Hurley Stage (%)/PASI score converted stage |
1 = 0 | 1 = 4 | 1 = 3 | 1 = 50 | 1 = 52 | 1 = 51 |
| 2 = 44 | 2 = 61 | 2 = 56 | 2 = 27 | 2 = 24 | 2 = 26 | |
| 3 = 56 | 3 = 35 | 3 = 41 | 3 = 23 | 3 = 24 | 3 = 23 | |
PASI, Psoriasis Area Severity Index; SD, standard deviation
Of the participants with HS, 3%, 56%, and 41% were Hurley stages 1, 2, and 3, respectively. The mean PASI score was 8.8, and patients were categorized into severity groups 1, 2, 3 (51%, 26%, 23% in each, respectively).
Twenty-year trade-off
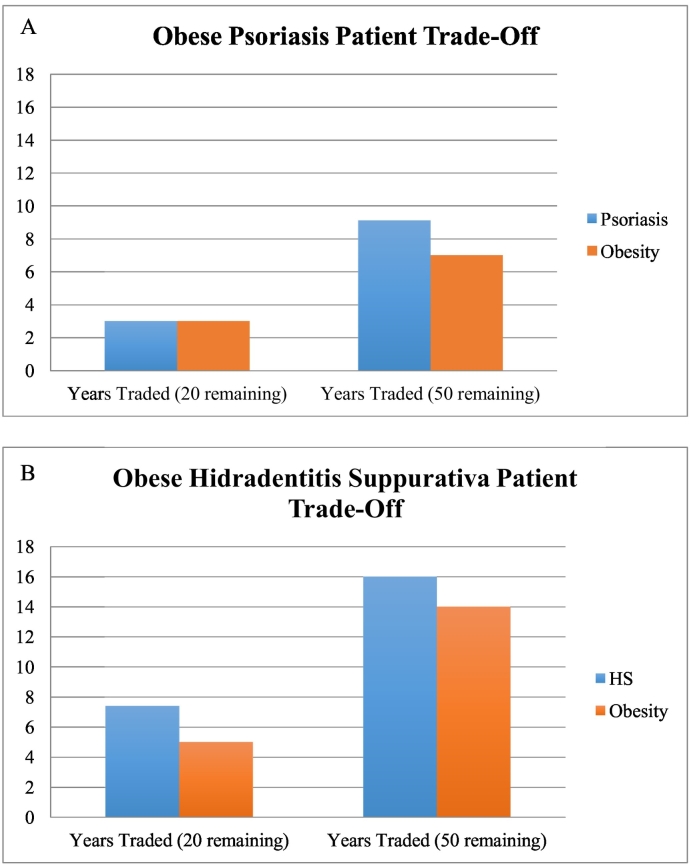
Patients with psoriasis reported that they were willing to trade 3.2 years of a possible remaining 20 years to be without their current level of skin disease. They were similarly willing to trade 2.5 years of a possible remaining 20 years to live at a normal weight (vs. psoriasis: p = .29; Fig. 1A). When only subjects with a PASI score > 6 were included, the figures changed to 4.2 years and 2.7 years, respectively, which is consistent with the higher skin disease burden.
Fig. 1.
(A) Trade-off values for life with normal skin versus normal weight in obese patients with psoriasis. (B) Trade-off values for life with normal skin versus normal weight in obese patients with hidradenitis suppurativa.
In comparison, patients with HS reported a willingness to trade 7.4 years of their lives to live without skin disease at their current level of disease severity of a possible 20 years remaining (Fig. 1B). Patients were willing to trade 5 years to live at a normal weight of a possible 20 years remaining (vs. HS; p = .01). Patients with HS were more distressed and willing to trade more years of life than those with psoriasis in this sample (HS vs. psoriasis: p = .001; obesity in HS vs. obesity in psoriasis: p = .01).
Fifty-year trade-off
When the question was framed over a 50-year remaining life span, both groups were willing to trade more of their remaining years to be free of skin disease than free from obesity. Patients with psoriasis reported that they were willing to trade 9.1 years of a possible 50 years remaining to live without skin disease than with their current level of psoriasis and 7 years to live at a normal weight than with their current weight (Fig. 1A; p = .21). Psoriasis subjects with a PASI score > 6 would trade 12.3 and 6.04 years, respectively.
Patients with HS were more distressed (p = .04 and .05) with respect to how they felt about their skin disease and obesity, respectively, and reported that they were willing to trade 16 years of a possible 50 remaining years to live without skin disease than with their current level of HS and 14 years to live at a normal weight than with their current weight (Table 1; Fig. 1B). There was no correlation between BMI and years willing to trade to be free of obesity (r2 = .2 for psoriasis and .01 for HS).
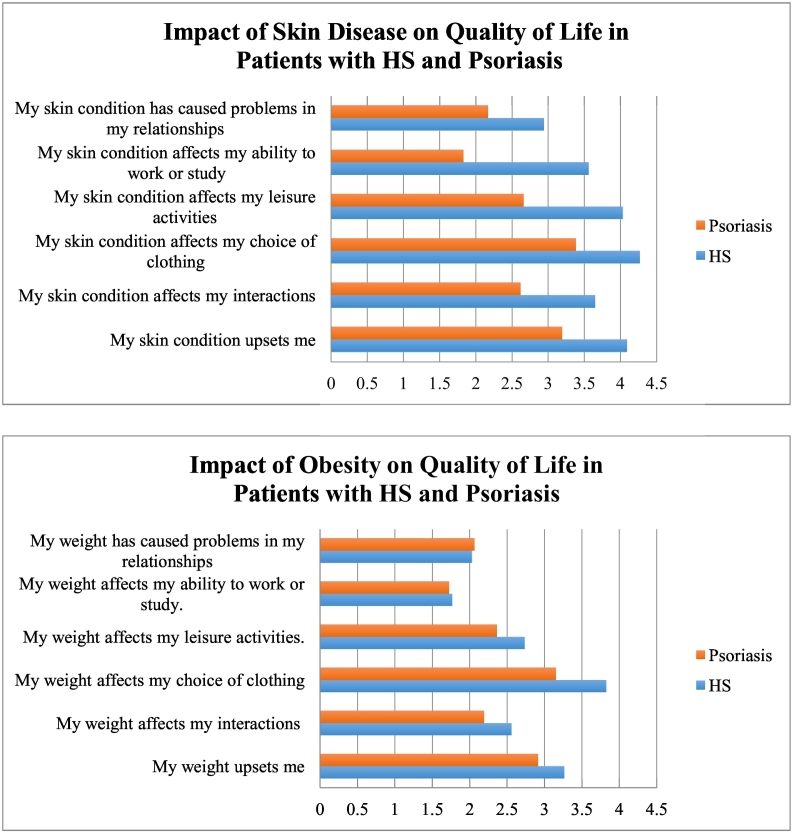
The results of the modified DLQI questionnaire (Fig. 2A) revealed that obese patients with HS had a significantly poorer quality of life than obese patients with psoriasis with respect to feelings (p = .0003), social interactions (p = .0005), clothing choice (p = .002), leisure activities (p < .0001), ability to work or study (p < .0001), and problems in relationships (p = .01). A regression analysis controlled for patient age and disease severity showed similar findings, with all domains maintaining statistical significance (p < .05), except for quality of life with respect to feelings, which trended toward significance (p = .06), and problems in relationships (p = .024).
Fig. 2.
(A) Impact of skin disease on quality of life in patients with hidradenitis suppurativa and psoriasis: Modified Dermatology Life Quality Index scored as 0 = never; 1 = occasionally; 2 = sometimes; 3 = often; 4 = regularly; and 5 = always. (B) Impact of obesity on quality of life in patients with hidradenitis suppurativa and psoriasis: Modified Dermatology Life Quality Index scored as 0 = never; 1 = occasionally; 2 = sometimes; 4 = regularly; and 5 = always.
When considering the impact of obesity on quality of life (Fig. 2B), clothing choice was the only category where patients with HS reported a significantly worse quality of life than patients with psoriasis (p = .03). Overall, skin disease conferred a greater impact on quality of life than obesity according to the modified DLQI portion of the questionnaire (mean total scores of 22.5 vs. 16.3 for patients with HS, and 15.9 vs. 14.3 for patients with psoriasis, respectively).
Discussion
Obesity has been associated with both disease severity and poorer quality of life in patients with inflammatory skin diseases such as psoriasis and HS. In this study of obese patients, we demonstrate that that the psychological burden of skin disease outweighed the burden of obesity.
A multivariate regression controlled for age, BMI, and sex showed no difference in time trade-off for obesity-free living in obese patients with HS (p = .13). Despite the lack of statistical significance, female patients were willing to trade more years of life than were men for remaining years at a normal weight, regardless of dermatological disease. This finding is consistent with the results from previous studies that showed a greater decrease in quality of life in obese women compared with their male counterparts.
The results of this study indicate that obesity is more bothersome to obese patients with HS than to obese patients with psoriasis. Patients with HS would give up significantly more years of their life to live without skin disease than they would to live at a normal weight, which emphasizes that skin disease may outweigh obesity in terms of morbidity. A previous study found that obese patients would rather incur handicaps such as blindness, deafness, dyslexia, severe acne, heart disease, or amputation than to live at their current weight (Rand and Macgregor, 1991).
Our study did not find that disease severity correlated with the years of life patients were willing to trade to live at a normal weight, which suggests that even clinically mild disease may impose significant quality of life impairments to patients with HS. The difference in significance for time traded off for living with obesity versus HS in the 20- and 50-year periods may be due to patient-assumed life expectancy for these respondents. Our findings suggest that patients with HS may benefit from multidisciplinary clinics that focus on weight loss in addition to managing the skin disease. This model has been used with dermatology clinics that care for patients with rheumatologic diseases and has led to improved quality of care (Velez et al., 2012).
The results of the modified DLQI questionnaire support previous trade-off data that emphasize obese patients’ high burden of skin disease and that obese patients with HS have a poorer quality of life than obese patients with psoriasis. Interestingly, obesity affected clothing choice to a greater extent for patients with HS than those with psoriasis. This difference may be due to the higher weight of these patients and/or the predilection of HS for inguinal areas, which incur friction and moisture and are factors compounded by obesity. Therefore, obese patients with HS may be considering the technical capabilities of clothing, such as wicking fabric, rather than merely choosing clothing to hide or cover obesity.
Another striking finding from the study was the 7-year average difference between age at the time of skin disease development and age at the time of diagnosis for obese patients with HS compared with obese patients with psoriasis, who, on average, were diagnosed with their skin disease within the year of development (Table 1). A delay in diagnosis likely leads to a poorer quality of life for obese patients with HS.
Limitations of this study include the small sample size and the severity assignments. Hurley staging has a static component, and PASI is a dynamic scoring system. This study did not answer how many years obese patients with skin disease would trade to have neither condition.
Conclusions
Skin disease continues to move toward universal acceptance as an entity and contributes to significant patient morbidity. The severity of skin disease in obese patients should include the effect of obesity on quality of life in addition to objective clinical severity. An integrative approach to skin disease and obesity may help immensely to relieve suffering and improve the overall health of these patients.
Footnotes
Funding sources: None.
Conflicts of interest: Dr. Kimball is a consultant for Abbvie, Janssen, Merck, Sun, Lilly, and Novartis and an investigator for Abbvie and Janssen. She also has fellowship funding from Janssen.
References
- Finlay A.Y., Khan G.K. Dermatology Life Quality Index (DLQI) – A simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210–216. doi: 10.1111/j.1365-2230.1994.tb01167.x. [DOI] [PubMed] [Google Scholar]
- Kim G.E., Seidler E., Kimball A.B. The relative impact of psoriasis and obesity on socioeconomic and medical outcomes in psoriasis patients. J Eur Acad Dermatol Venereol. 2014;28(2):216–221. doi: 10.1111/jdv.12089. [DOI] [PubMed] [Google Scholar]
- Kolotkin R.L., Crosby R.D., Gress R.E., Hunt S.C., Engel S.G., Adams T.D. Health and health-related quality of life: Differences between men and women who seek gastric bypass surgery. Surg Obes Relat Dis. 2008;4(5):651–659. doi: 10.1016/j.soard.2008.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebwohl M., Callen J.P. Obesity, smoking, and psoriasis. JAMA. 2006;295(2):208–210. doi: 10.1001/jama.295.2.208. [DOI] [PubMed] [Google Scholar]
- Oppe M., Rand-Hendriksen K., Shah K., Ramos-Goni J.M., Luo N. EuroQol protocols for time trade-off valuation of health outcomes. PharmacoEconomics. 2016;34(10):993–1004. doi: 10.1007/s40273-016-0404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand C.S., Macgregor A.M. Successful weight loss following obesity surgery and the perceived liability of morbid obesity. Int J Obes. 1991;15(9):577–579. [PubMed] [Google Scholar]
- Sartorius K., Emtestam L., Jemec G.B.E., Lapins J. Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol. 2009;4(161):831–839. doi: 10.1111/j.1365-2133.2009.09198.x. [DOI] [PubMed] [Google Scholar]
- Shalom G., Freud T., Harman-Boehm I., Polishchuk I., Cohen A.D. Hidradenitis suppurativa and metabolic syndrome: A comparative cross-sectional study of 3207 patients. Br J Dermatol. 2015;173(2):464–470. doi: 10.1111/bjd.13777. [DOI] [PubMed] [Google Scholar]
- Shlyankevich J., Chen A.J., Kim G.E., Kimball A.B. Hidradenitis suppurativa is a systemic disease with substantial comorbidity burden: a chart-verified case-control analysis. J Am Acad Dermatol. 2014;71(6):1144–1150. doi: 10.1016/j.jaad.2014.09.012. [DOI] [PubMed] [Google Scholar]
- Velez N.F., Wei-Passanese E.X., Husni M.E., Mody E.A., Qureshi A.A. Management of psoriasis and psoriatic arthritis in a combined dermatology and rheumatology clinic. Arch Dermatol Res. 2012;304(1):7–13. doi: 10.1007/s00403-011-1172-6. [DOI] [PubMed] [Google Scholar]
- Vinding G.R., Knudsen K.M., Ellervik C., Olesen A.B., Jemec G.B. Self-reported skin morbidities and health-related quality of life: A population-based nested case-control study. Dermatology. 2014;228(3):261–268. doi: 10.1159/000358009. [DOI] [PubMed] [Google Scholar]