Abstract
OBJECTIVES:
To evaluate the Pittsburgh Fatigability Scale (PFS) as a predictor of performance and functional decline in mobility-intact older adults.
DESIGN:
Longitudinal analysis of Baltimore Longitudinal Study of Aging data.
SETTING:
National Institute on Aging, Clinical Research Unit, Baltimore, Maryland.
PARTICIPANTS:
Mobility-intact men (46.8%) and women aged 60 to 89 with concurrent PFS administration and performance and functional assessment and follow-up assessment within 1 to 4 years (N=579).
MEASUREMENTS:
The PFS is a self-administered, 1-page assessment of expected physical and mental fatigue with a score ranging from 0 (no) to 5 (extreme) associated with performing 10 activities. Analyses examined associations between each dimension scored continuously (0–50), categorically (0–5), and dichotomously and change in and likelihood of clinically meaningful decline in usual and fast gait speed, chair stand pace, and reported walking ability. Covariates included age, age2, sex, race, visit status, baseline function, and follow-up time. We defined meaningful decline as 0.05 m/s per year for usual gait speed, 0.07 m/s per year for fast gait speed, 0.02 chair stands/s per year and 1 point or more for walking ability index.
RESULTS:
Over a mean 2.2 years, 20.5% to 37.7% of participants experienced meaningful decline across assessments. Independent of covariates, higher PFS physical and mental scores were most consistently associated with greater decline in usual gait speed, chair stand pace, and reported walking ability regardless of scoring approach. For example, higher physical fatigability was associated with twice the likelihood of meaningful decline in gait speed as lower physical fatigability (p=.001). PFS scores were superior to fatigue symptoms such as tiredness and energy level in predicting performance decline, which showed no association.
CONCLUSION:
Routine self-administered perceived fatigability assessment may help identify older persons vulnerable to accelerated mobility decline.
Keywords: fatigability, mobility decline, self-report, aging
Fatigability has recently emerged as an important dimension of aging and health1 and a potential early marker of impending mobility decline in seemingly robust, high-functioning older adults.2 The construct of fatigability has been operationalized as observed deterioration in performance during an endurance-based activity (performance fatigability3,4) and perceived exertion immediately after performance of a standardized task, such as walking a given speed for a set period of time (perceived fatigability3). The fatigability construct has been designed to improve identification of fatigue because unconscious slowing down or reduction in activity to avoid, diminish, or delay fatigue often biases perception of fatigue. We recently demonstrated that perceived fatigability was superior to responses to basic questions about fatigue symptoms (e.g., feeling unusually tired over the past month or experiencing low energy levels) in predicting clinically meaningful decline in usual and fast gait speed and a composite measure of lower extremity performance.2 Perceived fatigability also predicts lower overall objectively assessed physical activity, which may be intermediate to functional decline.5
Performance and perceived fatigability assessment require face-to-face interaction, trained personnel, and ample space and time, which are not often available in clinical settings or possible in longitudinal observation and intervention studies that rely on remote contact. Thus, as an alternative to direct in-person testing, we developed the Pittsburgh Fatigability Scale (PFS),6 a 1-page, self-administered questionnaire that asks about level of exertion on a scale from 0 to 5 on 10 different activities that range in energetic demand from sitting for 2 hours to brisk walking for 30 minutes. Physical and mental fatigability are assessed. Although several fatigue questionnaires have been developed (e.g., Multidimensional Fatigue Inventory, Piper Fatigue Scale, Fatigue Assessment Instrument)7–9 and are widely used in research and clinical settings, none ascertain fatigue symptoms anchored to performance of specific tasks (fatigability). The few exceptions include the Mobility-Tiredness Scale, which assesses presence versus absence of fatigue associated with performing 6 mobility tasks but does not ascertain level of fatigue,10 and the Dutch Exertion Fatigue Scale11 and Situational Fatigue Scale,12 neither of which was developed for use in community-residing older adults. The PFS, in contrast, specifically assesses perceived fatigability, that is, the context in which fatigue might occur and its severity. Details on the development of the PFS and its psychometric properties and construct validity have been published previously.6 In the current work, we examine the predictive validity of the physical and mental subscales of the PFS in identifying risk of performance and functional decline in mobility-intact older adults.
METHODS
Participants
The study population consisted of 579 men (46.8%) and women aged 60 to 89 participating in the Baltimore Longitudinal Study of Aging (BLSA), a continuous-enrollment cohort study of normative aging established in 1958. At enrollment, participants are free of functional limitations, cognitive impairment, and major chronic conditions. Follow-up visits occur at regular intervals, with persons aged 60 to 79 scheduled biannually and those aged 80 and older scheduled annually for, on average, a 3-day visit to the National Institute on Aging Clinical Research Unit in Baltimore, Maryland.
At their index visit for the current analysis, participants were mobility intact, that is, reported no difficulty walking one-quarter of a mile, did not use a walking aid, and could perform 10 consecutive chair stands. Participants also completed the physical and mental subscales of the PFS and had a performance and functional assessment at their index and a follow-up visit 1 to 4 years later. For participants with multiple follow-up visits, the visit closest to 2 years (730 days) from the index visit was used, yielding a mean follow-up of 2.2 ± 0.5 years. Two hundred two participants out of 781 with a qualifying index visit had no eligible follow-up, 121 of whom were not due or overdue for a follow-up visit, 52 withdrew for health-related reasons or were lost to follow-up, 9 had a telephone follow-up only, 8 were seen more than 4 years later, and 12 had died. These participants did not differ from those included in the study on any measured characteristic. The National Institute of Environmental Health Sciences internal review board approved the BLSA study protocol, and all participants provided written informed consent at each visit.
Data Collection
Pittsburgh Fatigability Scale
The 10-item PFS is a valid, reliable, self-administered, 1-page assessment of perceived fatigability6 that was added to the BLSA in March 2011. The 10 items cover sedentary, social, lifestyle, and physical activities ranging from light to high intensity. The form instructs respondents to indicate the level of “physical and mental fatigue you expect or imagine you would feel immediately after completing each … activity” and to “please circle responses for both physical and mental fatigue between 0 and 5, where “0” equals no fatigue at all and “5” equals extreme fatigue.” Continuous scores for each dimension can range from 0 to 50, with higher scores indicating higher fatigability. Higher physical fatigability has been defined as a PFS-physical score of 15 and greater and higher mental fatigability as a PFS-mental score of 13 and greater.13 For this article, we also evaluated categorical scoring ranging from 0 to 5 for each scale. For the physical scale, 0 was assigned to scores of 0 to 4, 1 to scores of 5 to 9, 2 to scores of 10 to 14, 3 to scores of 15 to 19, 4 to scores of 20 to 24, and 5 to scores of 25 and higher. For the mental scale, 0 was assigned to scores of 0 to 3, 1 to scores of 4 to 7, 2 to scores of 8 to 11, 3 to scores of 12 to 15, 4 to scores of 16 to 19, and 5 to scores of 20 and higher.
Reported Tiredness and Energy Level
Tiredness and energy level were assessed using an interviewer-administered questionnaire. For tiredness, the question (and response code) was, “In the past month, on average how often have you felt unusually tired during the day: all (3), most (2), some (1), or none (0) of the time?” For analyses, responses were dichotomized as none versus some or more, because most and all were rarely endorsed. For energy level, the question was, “During the past month, what category best describes your usual energy level, using a scale from 0 to 10, where 0 is no energy at all, and 10 is the most energy you have ever had? For analyses, energy level was reverse coded to be consistent with PFS and tiredness coding.
Physical Performance and Function
Usual and fast gait speed were assessed over a 6-m course, with participants asked to walk at their “usual walking pace” for 2 trials and then “as fast as you can” for 2 trials. The faster of each trial was used in the analyses. Repeated chair stand pace was derived from time to complete 10 full stands. Reported walking ability was determined from responses to a series of questions beginning with, “Because of a health or physical problem, do you have any difficulty walking one-quarter of a mile, that is, about 2 or 3 blocks, without stopping?” Those reporting difficulty were asked whether they had a little, some, or a lot of difficulty or were unable to walk. Persons denying difficulty were asked how easy it was for them to walk one-quarter of a mile—very, somewhat, or not so easy—followed by whether they had any difficulty walking 1 mile and the ease of walking 1 mile if no difficulty was reported. Responses were combined to create a walking ability index ranging from 0 to 9, with 0 representing unable to walk one-quarter of a mile and 9 indicating that walking 1 mile was very easy.3
Covariates
Covariates included age and age2 to account for accelerated physical and mental decline with increasing age, sex, self-reported race (black vs nonblack, because few nonblack BLSA participants identify as other than Caucasian), whether the index visit was a first BLSA visit, time between functional assessments, and baseline value of the specific function evaluated.
Statistical Analyses
Analyses examined associations between index visit value of each dimension scored continuously (0–50), categorically (0–5), and dichotomously, with scores of 15 or less defining higher physical fatigability and 13 or less defining higher mental fatigability and change and likelihood of clinically meaningful decline in physical performance represented by usual and fast gait speed and repeated chair stand pace and function represented by reported walking ability. The association between continuous scoring of the physical and mental dimensions of the PFS and change in physical performance and function was examined using linear regression. Logistic regression was used to estimate odds of clinically meaningful decline associated with categorical increments in the PFS physical and mental scales and for the dichotomous measures distinguishing higher fatigability. Categorical scoring was devised to facilitate comparison with a recently validated treadmill walk–based measure of perceived fatigability with a possible score range of 6 to 20 on which scores greater than 12 are rare.2 Clinically meaningful decline—that is, the amount of decline considered clinically important14—was defined as a loss of 0.05 m/s per year for usual gait speed, 0.07 m/s per year for fast gait speed, 0.02 chair stands/s per year, and a loss of 1 or more points on the walking ability index.2,14,15 All analyses controlled for the covariates noted above. For comparison, logistic regression analyses were used to examine associations between two fatigue symptoms unusual tiredness and energy level and likelihood of clinically meaningful decline. Analyses were conducted using SAS version 9.3 (SAS Institute, Inc., Cary, NC).
RESULTS
Table 1 summarizes participant characteristics according to physical and mental fatigability. Mean age was 73.6 and was greater in those with higher physical or mental fatigability. Participants with higher fatigability on either dimension were more likely to report tiredness at least some of the time and to have a lower mean energy level and poorer performance and function. The percentage of men was proportionately lower in those with either higher physical or mental fatigability. The proportion having their first BLSA visit was lower and percentage black race higher in those with higher physical fatigability.
Table 1.
Baseline Characteristics According to Higher and Lower Physical and Mental Fatigability: Pittsburgh Fatigability Scale (N=579)
| Characteristic | Physical | Mental | ||
|---|---|---|---|---|
| Lower, <15, n=341 | Higher, ≥15, n=238 | Lower, <13. n=448 | Higher, ≥13, n=131 | |
| Age, mean±SD | 72.8 ± 7.5 | 74.9 ± 7.8 | 72.9 ± 7.6 | 76.3 ± 7.6 |
| Male, % | 52.5 | 38.7 | 49.3 | 38.2 |
| Black, % | 21.7 | 29.0 | 23.7 | 28.2 |
| First Baltimore Longitudinal Study of Aging visit, % | 25.5 | 17.2 | 22.8 | 19.9 |
| Unusual tiredness, % | 26.7 | 47.5 | 30.4 | 51.5 |
| Energy level, mean±SD | 1.86 ± 1.32 | 2.77 ± 1.54 | 2.03 ± 1.43 | 2.95 ± 1.44 |
| Usual gait speed, m/s, mean±SD | 1.22 ± 0.21 | 1.13 ± 0.19 | 1.21 ± 0.20 | 1.11 ± 0.20 |
| Fast gait speed, m/s, mean±SD | 1.86 ± 0.36 | 1.70 ± 0.32 | 1.84 ± 0.34 | 1.66 ± 0.33 |
| Chair stand pace, seconds, mean±SD | 0.53 ± 0.15 | 0.46 ± 0.13 | 0.52 ± 0.15 | 0.44 ± 0.13 |
| Walking index, mean±SD | 8.73 ± 0.80 | 7.92 ± 1.42 | 8.57 ± 0.97 | 7.79 ± 1.52 |
| Follow-up, years, mean±SD | 2.19 ± 0.43 | 2.16 ± 0.53 | 2.19 ± 0.46 | 2.11 ± 0.50 |
SD = standard deviation
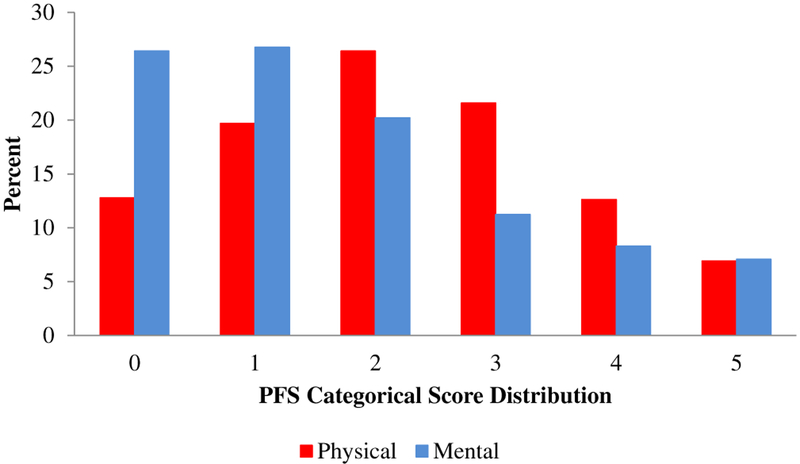
Figure 1 shows the distribution of categorical scoring for the PFS physical and mental scales at the index visit. Using the 0 to 5 categorical scoring, the PFS physical scale exhibits a normal distribution, whereas the PFS mental scale is skewed toward the low fatigability end of the distribution.
Figure 1.
Distribution of categorical scoring for Pittsburgh Fatigability Scale physical (0–4 =0, 5–9 =1, 10–14 = 2, 15–19 = 3, 20–24 = 4, ≥25 = 5) and mental (0–3 = 0, 4–7 = 1, 8–12 = 2, 12–15 = 3, 16–19 = 4, ≥20 = 5) scales at index visit (N=579).
Over a mean 2.2 years of follow-up, 20.5% to 37.7% of participants declined on all assessments. Findings reported in Table 2 indicate that higher PFS physical score was associated with greater decline in usual gait speed, chair stand pace, and reported walking ability (all p ≤ .009) and a 15% to 48% greater likelihood of meaningful decline per unit increase in 0 to 5 categorical scoring over all measures (p < .001 to .05). Those with higher physical fatigability at their index visit were 1.8 to 2.4 times as likely to experience meaningful decline in all but fast gait speed as those with lower physical fatigability (all p ≤ .008). Similar but somewhat less robust associations were observed for PFS mental fatigability score, with a 16% to 23% greater likelihood of meaningful decline per unit increase in 0 to 5 categorical scoring for usual gait speed (p=.003), chair stand pace (p=.04), and walking ability index (p=.008). Those with greater mental fatigability were 1.5 times as likely to experience meaningful decline in walking ability index and 2.5 times as likely to experience meaningful decline in usual gait speed as those with lower mental fatigability.
Table 2.
Association Between Pittsburgh Fatigability Scale Physical and Mental Scores, Reported Tiredness and Energy Level, and Change in Performance and Function and Likelihood of Clinically Meaningful Decline
| Assessment | Usual Gait Speed, m/s |
Fast Gait Speed, m/s |
Chair Stand Pace, Stands/s |
Walking Index Points |
|---|---|---|---|---|
| Physical, beta (p-value)1 | −0.003 (.009) | −0.002 (.11) | −0.002 (.003) | −0.042 (<.001) |
| Mental, beta (p-value)1 | −0.002 (.04) | −0.002 (.21) | −0.002 (.02) | −0.039 (<.001) |
| Clinically Meaningful Decline, %2 | 33.2 | 37.7 | 23.7 | 20.5 |
| Physical (range 0–5),3 OR (95% CI) p-value1 |
1.30 (1.12–1.52) <.001 |
1.15 (1.00–1.31) .05 |
1.20 (1.02–1.40) .03 |
1.48 (1.24–1.76) <.001 |
| Mental (range 0–5),4 OR (95% CI) p-value1 |
1.23 (1.07–1.41) .003 |
1.13 (1.00–1.28) .06 |
1.16 (1.01–1.34) .04 |
1.22 (1.05–1.41) .008 |
| Higher physical fatigability ≥ 15, OR (95% CI) p-value1 |
2.03 (1.33–3.09) .001 |
1.43 (0.98–2.09) .07 |
1.82 (1.17–2.83) .008 |
2 39 (1.52–3.78) <.001 |
| Higher mental fatigability ≥ 13, OR (95% CI) p-value1 |
2.54 (1.58–4.10) <.001 |
1.40 (0.90–2.18) .13 |
1.58 (0.97–2.59) .07 |
1.51 (0.93–2.46) .04 |
| Tiredness, OR (95% CI) p-value1 |
1.18 (0.80–1.73) .41 |
1.13 (0.79–1.62) .49 |
1.30 (0.87–1.95) .20 |
1.66 (1.10–2.51) .01 |
| Energy level, OR (95% CI) p-value1 |
1.10 (0.96–1.25) .17 |
1.01 (0.90–1.14) .85 |
1.13 (0.98–1.30) .08 |
1.16 (1.01–1.34) .04 |
Adjusted for age, age2, sex, race, visit status, baseline function, and time between visits.
Loss of ≥ 0.05 m/s per year for usual gait speed, ≥0.07 m/s per year for fast gait speed, ≥0.02 chair stands/s per year, and ≥1 points on walking ability index.2,14,15
0–4 =0, 5–9 =1, 10–14 =2, 15–19 =3, 20–24 =4, ≥25 =5.
0–3 =0, 4–7 =1, 8–12 =2, 12–15 =3, 16–19 =4, ≥20 =5.
OR=odds ratio; CI=confidence interval.
In contrast, neither reported tiredness nor energy level predicted likelihood of meaningful decline in any performance measure, although both were associated with decline in reported walking ability (p=.01 and p=.04, respectively).
Discussion
In mobility-intact adults aged 60 to 89, responses to a 1-page self-administered assessment of expected physical and mental fatigue associated with 10 common activities ranging from 2 hours sitting to 30 minutes of brisk walking predicted amount of decline and likelihood of clinically meaningful decline over an average of 2.2 years in lower extremity performance and reported walking ability. Associations were most consistent for usual gait speed, chair stand pace, and reported walking ability and were independent of scoring approach—continuous, categorical, or dichotomous. The PFS was also found to be superior to assessment of global fatigue symptoms such as tiredness and energy level in predicting performance decline; global fatigue measures were not predictive of change in any performance measure.
The odds of clinically meaningful decline associated with one increment in the 0-to-5 categorical scoring of the PFS physical and mental scales were comparable with those for one increment in the Borg Rating of Perceived Exertion16 used in the assessment of perceived fatigability.2 In previously published findings from the BLSA, the odds of meaningful decline associated with one Borg Rating of Perceived Exertion increment were 1.19 for usual gait speed, 1.13 for fast gait speed, and 1.14 for reported walking ability. In contrast, in the current study, the odds of meaningful decline associated with one increment in categorical PFS physical and mental score were 1.30 and 1.23 for usual gait speed, 1.15 and 1.13 for fast gait speed, and 1.48 and 1.22 for reported walking ability.
These findings extend the initial validation work6 to predictive validity of performance and functional decline independent of initial physical performance or reported walking ability and demonstrate the added value of the PFS for evaluating likelihood of mobility decline. The findings with respect to gait speed are similar to those using the Mobility-Tiredness Scale, which found more marked decline in gait speed with increasing mobility-related fatigue over 5 years in men but not in women.17 In contrast, in the current study, the association between PFS physical score and gait speed decline in women was robust (per point increase: odds ratio=1.39, 95% confidence interval=1.15–1.69, p<.001) using the 0-to-5 categorical scoring (data not shown). To our knowledge, neither the Dutch Exertion Fatigue Scale11 nor the Situational Fatigue Scale12 has been studied for its predictive validity for mobility decline.
The nonsignificant predictive associations between physical and mental PFS score and fast gait speed warrant some comment. It would appear that fatigability assessment is most valuable as a stand-alone assessment or an adjunct to minimal challenge tests such as usual gait speed over a short course. The beta coefficients associated with the index visit value in adjusted models of follow-up visit value were 0.75 for fast gait speed, in contrast to 0.57 for usual gait speed and 0.54 for reported walking ability (data not shown), suggesting that performance on more-challenging assessments such as fast gait speed provides more insight into future decline than less-challenging walking tests (e.g., usual gait speed) and self-assessment of walking ability. Thus, the PFS may be especially useful in clinical settings or telephone or mail follow-up of cohort study participants when more-intense testing is impractical because of time, space, or venue-related concerns.
Evidence continues to accrue supporting the added value of physical and mental fatigability assessment in identifying apparently well-functioning individuals at risk of performance and functional decline,2 as well as other debilitating health conditions. Including a 1-page self-administered fatigability scale as part of a medical history may help identify the often covert and insidious development of mobility limitations that frequently occurs with aging when options for remediation or delay still exist.
ACKNOWLEDGMENTS
Preliminary findings were presented at the American College of Sports Medicine Annual Meeting, San Diego, California, May 2015.
Financial Disclosure:
The BLSA is supported by the Intramural Research Program of the National Institute on Aging. JAS is supported by R21AG053198, P30AG021334, and U01AG057545. This research was also supported by Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant (NWG), National Institutes of Health P30 AG024826 and P30 AG024827.
Sponsor’s Role: None.
Footnotes
Conflict of Interest: All authors report no financial or personal conflicts of interest.
REFERENCES
- 1.Eldadah BA. Fatigue and fatigability in older adults. PM R 2010;2:406–413. [DOI] [PubMed] [Google Scholar]
- 2.Simonsick EM, Glynn NW, Jerome GJ et al. Fatigued but not frail: Perceived fatigability as a marker of impending decline in mobility-intact older adults. J Am Geriatr Soc 2016;64:1287–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simonsick EM, Schrack JA, Glynn NW et al. Assessing fatigability in mobility-intact older adults. J Am Geriatr Soc 2014;62:347–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnelle JF, Buchowski MS, Ikizler TA et al. Evaluation of two fatigability severity measures in elderly adults. J Am Geriatr Soc 2012;60:1527–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wanigatunga AA, Simonsick EM, Zipunnikov V et al. Perceived fatigability and objective physical activity in mid- to late-life. J Gerontol A Biol Sci Med Sci 2018;73:630–635.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glynn NW, Santanasto AJ, Simonsick EM et al. The Pittsburgh Fatigability Scale for older adults: Development and validation. J Am Geriatr Soc 2015; 63:130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smets EMA, Garssen B, Bonke B et al. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychometric Res 1995;39:315–325. [DOI] [PubMed] [Google Scholar]
- 8.Piper BF, Dibble SL, Dodd MJ et al. The revised Piper Fatigue Scale: Psycho-metric evaluation in women with breast cancer. Oncology Nurs Forum 1998;24:677–684. [PubMed] [Google Scholar]
- 9.Schwartz JE, Jandorf L, Krupp LB. The measurement of fatigue: A new instrument. J Psychosomatic Res 1993;37:753–762. [DOI] [PubMed] [Google Scholar]
- 10.Fieo RA, Mortensen EL, Rantanen T et al. Improving a measure of mobility-related fatigue (the Mobility-Tiredness Scale) by establishing item intensity. J Am Geriatr Soc 2013;61:429–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tiesinga LJ, Dassen TWN, Halfens RJG. DUFS and DEFS: Development, reliability and validity of the Dutch Fatigue Scale and the Dutch Exertion Fatigue Scale. Int J Nurs Stud 1998;35:115–123. [DOI] [PubMed] [Google Scholar]
- 12.Yang C-M, Wu C-H. The Situational Fatigue Scale: A different approach to measuring fatigue. Qual Life Res 2005;14:1357–1362. [DOI] [PubMed] [Google Scholar]
- 13.Cooper R, Popham M, Santanasto AJ et al. Are BMI and inflammatory markers independently associated with physical fatigability in old age? Int J Obes (Lond) 2018. May 24. doi: 10.1038/s41366-018-0087-0. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perera S, Mody SH, Woodman RC et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–749. [DOI] [PubMed] [Google Scholar]
- 15.Perera S, Studenski S, Newman A et al. Are estimates of meaningful decline in mobility performance consistent among clinically important subgroups? J Gerontol A Biol Sci Med Sci 2014;69A:1260–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borg G Psychophysical scaling with applications in physical work and the perception of exertion. Scan DJ Work Environ Health 1990;16(Suppl 1): 55–58. [DOI] [PubMed] [Google Scholar]
- 17.Mänty M, Mendes de Leon CF, Rantanen T et al. Mobility-related fatigue, walking speed and muscle strength in older people. J Gerontol A Biol Sci Med Sci 2012;67A:523–529. [DOI] [PubMed] [Google Scholar]