The rapid fosfomycin/Escherichia coli NP test was developed to detect fosfomycin resistance in E. coli isolates. The test is based on glucose metabolization and the detection of bacterial growth in the presence of fosfomycin at 40 µg/ml.
KEYWORDS: Escherichia coli, fosfomycin, rapid test
ABSTRACT
The rapid fosfomycin/Escherichia coli NP test was developed to detect fosfomycin resistance in E. coli isolates. The test is based on glucose metabolization and the detection of bacterial growth in the presence of fosfomycin at 40 µg/ml. Bacterial growth is visually detectable by an orange-to-yellow color change of red phenol, a pH indicator. A total of 100 E. coli isolates, among which 22 were fosfomycin resistant, were used to evaluate the test performance. The sensitivity and specificity of the test were 100% and 98.7%, respectively. This new test is user friendly, sensitive and specific, and its results are obtained in 1 h 30 min.
INTRODUCTION
Multidrug resistance in Enterobacteriaceae spp. represents a serious threat to public health, since the accumulation of resistance determinants may be the source of difficult-to-treat infections in humans. The increase of multidrug-resistant (MDR) bacteria induced a renewed interest in old antibiotics, such as fosfomycin (1). Because of its broad-spectrum activity and its safety profile, fosfomycin is often used as a first-line antibiotic for treating uncomplicated urinary tract infections (UTIs) (2).
Escherichia coli, which is the bacterial species most frequently responsible for UTIs, exhibits an increased resistance rate to broad-spectrum cephalosporins through the production of extended-spectrum β-lactamases (ESBLs) but often remains susceptible to fosfomycin (3). However, the fosfomycin resistance rate in E. coli might also be increasing due to an increased clinical use and, consequently, an increased selective pressure.
In Gram-negative bacteria, fosfomycin resistance can result from reduced permeability, amino acid mutations in the active site of the MurA target involved in peptidoglycan biosynthesis, and the production of fosfomycin-inactivating enzymes (fos genes) (4). Acquired resistance to fosfomycin in E. coli may be due to metalloenzymes of the FosA type that catalyze the conjugation of glutathione to fosfomycin, thereby inactivating this antibiotic (5). The FosA3 enzyme is the most commonly identified FosA-like determinant found as an acquired mechanism of fosfomycin resistance in E. coli, and it is quite widespread in East Asia (6–8). The fosA3 gene is usually located in conjugative plasmids also carrying CTX-M-type ESBL-encoding genes (9, 10). Consequently, E. coli strains acquiring such plasmids usually exhibit coresistance to both fosfomycin and broad-spectrum cephalosporins. Although less frequently, fosA4, fosA5, and fosA6 genes have also been identified in E. coli (9, 11, 12). In addition, the acquisition of the fosA1 gene has been reported in Serratia marcescens, and a chromosomal fosA2 gene has been identified in Enterobacter cloacae (13, 14).
Since fosfomycin is being used as an empirical treatment for UTIs in the community and also for severe hospital-acquired infections, there was an interest to develop a rapid test to evaluate its efficacy. The standard reference technique for determining susceptibility to fosfomycin is based on agar dilution that is a tedious technique requiring 18 ± 2 h to be performed (15). Other techniques, such as disk diffusion and Etest strips, can also be used, but they also require at least 18 h (16, 17).
In order to rapidly identify fosfomycin-resistant E. coli isolates, we aimed to develop a rapid and cost-effective test that might be used worldwide, regardless of the technical level of the laboratory. Similar to the recently developed Rapid Polymyxin NP test (18), we have developed the rapid fosfomycin/E. coli NP test which is a user-friendly technique based on carbohydrate hydrolysis detecting bacterial growth (or absence of growth) in the presence of a defined concentration of fosfomycin, allowing the rapid detection (1 h 30 min) of fosfomycin-resistant E. coli isolates.
MATERIALS AND METHODS
Isolate collection.
A total of 100 E. coli isolates collected from clinical samples worldwide were used. This collection included 22 fosfomycin-resistant isolates, consisting of 14 isolates with acquired resistance to fosfomycin due to the fosA3 gene and 8 isolates with an unknown mechanism of resistance. The other 78 E. coli isolates were susceptible to fosfomycin (Table 1).
TABLE 1.
Rapid fosfomycin NP/E. coli test results for fosfomycin-resistant and fosfomycin-susceptible E. coli isolates
| Origin | Fosfomycin phenotypea | MIC (µg/ml) | Rapid fosfomycin NP test | Resistance mechanism | No. of isolates |
|---|---|---|---|---|---|
| China | R | >512 | + | fosA3 | 4 |
| Switzerland | R | >512 | + | fosA3 | 5 |
| Nepal | R | >512 | + | fosA3 | 2 |
| France | R | >512 | + | fosA3 | 1 |
| South Africa | R | >512 | + | fosA3 | 2 |
| Switzerland | R | 64 | + | fosA1–6 not detected | 1 |
| Switzerland | R | 128 | + | fosA1–6 not detected | 1 |
| Switzerland | R | >512 | + | fosA1–6 not detected | 6 |
| China | S | 1 | − | NAb | 7 |
| Switzerland | S | 1 | − | NA | 9 |
| Switzerland | S | 1 | + | NA | 1 |
| Switzerland | S | 16 | − | NA | 2 |
| France | S | 1 | − | NA | 53 |
| Lebanon | S | 16 | − | NA | 1 |
| Inde | S | 1 | − | NA | 2 |
| France | S | 16 | − | NA | 1 |
| France | S | 32 | − | NA | 1 |
| Angola | S | 1 | − | NA | 1 |
| Switzerlandc | R | >512 | + | fosA1–6 not detected | 1 |
| Switzerlandd | S | 1 | − | NA | 1 |
R, resistant; S, susceptible.
NA, not applicable. Fosfomycin-susceptible strains were not investigated for the presence of fosA genes.
Positive control isolate N279.
Negative control isolate N6.
MIC determination.
To determine MIC values for fosfomycin, we used the agar dilution method in cation-adjusted Mueller-Hinton agar (MHA-CA, reference 64884; Bio-Rad, Marnes-La-Coquette, France) supplemented with 25 µg/ml of glucose-6-phosphate, as recommended by Clinical and Laboratory Standards Institute (CLSI) guidelines (14). We considered this technique to be the standard for comparison with the results obtained with the rapid fosfomycin/E. coli NP test. Fosfomycin (reference 34089; Sigma-Aldrich, St. Louis, MO, USA) was tested over a range of dilutions (1 to 512 µg/ml). All experiments were repeated in three separate experiments, using daily freshly prepared plates and inoculums.
The breakpoints of the European Committee on Antimicrobial Susceptibility Testing (EUCAST) were used as reference (19). Hence, E. coli isolates with fosfomycin MICs of ≤32 µg/ml were categorized as susceptible, while those with MICs of >32 µg/ml were categorized as resistant.
PCR amplification and sequencing.
DNA of the isolates was recovered using the QIAamp DNA mini kit and the QIAcube workstation (Qiagen, Courtaboeuf, France), according to the manufacturer’s instructions. PCR amplification was performed to detect the plasmid-mediated fosA1 to fosA6 genes with the following primers: fosA1-2_Fw (5′-STAYGACGAGGCGCGCSRKTACGTG-3′), fosA3-4_Fw (5′-CTGGATGMGCAGCGGCGTAAAACG-3′), fosA5-6_Fw (5′-CCGCAGCGGCGCGTTACTCCGCCG-3′), and fosA_Univ_Rv (5′-CRTCVGGRTCGAGRAAATAG-3′). The PCR conditions were 98°C for 1 min; followed by 35 cycles of 98°C for 1 s, 55°C for 30 s, and 72°C for 30 s; with a final extension of 72°C for 10 min. Enterobacter cloacae R2969, Kluyvera georgiana R1108, and Klebsiella pneumoniae R2292 were used as controls for plasmids carrying fosA1 to 2, fosA3 to 4, and fosA5 to 6 genes, respectively. To discriminate between fosA3 and fosA4, positive PCRs were further sequenced by Microsynth (Balgach, Switzerland) and results analyzed with CloneManager Professional (Sci-Ed software, Denver, CO, USA).
Rapid fosfomycin/E. coli NP test.
Reagents and solutions. The rapid fosfomycin/E. coli NP test requires two reagents and solutions, namely the stock solutions of fosfomycin and the rapid fosfomycin NP solution, as described below. For stock solutions of fosfomycin, powder was diluted into Milli-Q water to obtain a concentration of 50 mg/ml. This solution can be stored for 1 month at 4°C. The rapid fosfomycin NP solution was prepared by mixing the culture medium, the pH indicator, and the distilled water. The pH was further adjusted to 7.5 and the solution autoclaved to obtain a final concentration of 2.5% MHB-CA powder, 0.005% phenol red indicator, and 1% d(+)-glucose. This solution can be kept at 4°C for 1 week or at −20°C for 1 year and must be prewarmed at 37°C before use to prevent growth delay and a delayed color change. Before performing the experiment, fosfomycin was added to the rapid fosfomycin NP solution and mixed to obtain a final fosfomycin concentration at 40 µg/ml.
Bacterial inoculum preparation. A standardized E. coli inoculum was prepared by using freshly obtained (overnight) bacterial colonies grown on UriSelect 4 agar plates, as previously described (17). Bacterial colonies were resuspended into 5 ml of sterile NaCl (0.85%) to obtain a 3.0 to 3.5 McFarland standard optical density (∼109 CFU/ml). A bacterial suspension was prepared for each isolate to be tested (Table 1).
Tray inoculation and reading. Inoculation and reading were performed similarly to what is recommended for the optimized Rapid Polymyxin NP test (18). Briefly, a 96-well polystyrene microtest plate (round base with lid, sterile, reference 82.1582.001; Sarstedt, Nümbrecht, Germany) was used to inoculate the bacterial suspension in the presence or absence of fosfomycin, in separate wells. A total of 50 µl of bacterial suspension was added to two wells, the first containing 150 µl of rapid fosfomycin NP solution without fosfomycin, and the second containing 150 µl of rapid fosfomycin NP solution supplemented with 25 µg/ml glucose-6-phosphate and 40 µg/ml fosfomycin. The same procedure was performed using 50 µl NaCl instead of the bacterial suspension, as a negative control. The final concentration of bacteria was ∼108 CFU/ml in each well, and the final concentration of fosfomycin was 40 µg/ml. Each sample was tested in duplicate.
The trays were visually inspected every 30 min. Isolates N6 and N279 were used as negative and positive controls, respectively (Table 1). A test result was considered positive (fosfomycin resistance) if the isolate grew in the presence of fosfomycin, when a color change from orange to yellow was observed in the wells, confirming the metabolism of glucose by the isolate (Fig. 1). Conversely, a test result was considered negative (fosfomycin susceptibility) if the isolate did not grow in the presence of fosfomycin, meaning the color of the wells remained orange.
FIG 1.
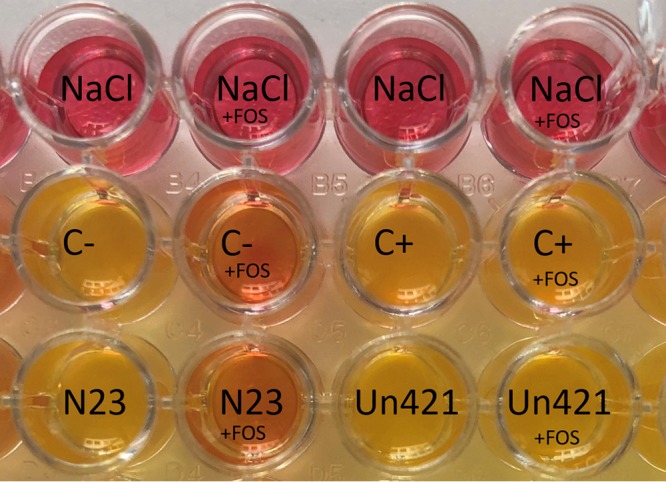
Rapid fosfomycin NP/E. coli test, representative results. The first row shows noninoculated wells, containing the rapid fosfomycin NP solution and NaCl. In columns 2 and 4, the solution was supplemented with fosfomycin (+FOS). The second row shows the negative (C−) and the positive (C+) controls. The third row shows two tested samples, N23 and Un421. As C−, N23 isolate grew (yellow color) in the absence of fosfomycin and did not grow (orange color) in the presence of this antibiotic. Thus, it was thus as fosfomycin susceptible. Isolate Un421 and C+ grew in presence and absence of fosfomycin, and Un421 was reported to be fosfomycin resistant. Note that in the absence of bacterial suspension, the well color is pink, while the inoculated wells exhibit an orange color in the absence of bacterial growth. However, this color difference did not compromise the interpretation of the test results.
RESULTS
A total of 100 E. coli isolates were tested to evaluate the performance of the rapid fosfomycin/E. coli NP test. Among the 22 fosfomycin-resistant isolates, 14 exhibited the acquired mechanism of resistance to fosfomycin FosA3, while 8 were negative for fosA1 to fosA6 gene amplification. Other mechanisms of resistance to fosfomycin were not further investigated.
The 78 fosfomycin-susceptible isolates (MICs of fosfomycin, 1 to 32 µg/ml) gave negative results with the rapid fosfomycin/E. coli NP test, except for a single isolate (isolate N13 showing an MIC value of fosfomycin of 1 µg/ml) which gave a positive result (major error) (Table 1). All the fosfomycin-resistant isolates that carried an acquired fosA3 gene (n = 14; MICs of fosfomycin, >512 µg/ml) or for which the mechanism of resistance remains unknown (n = 8; MICs of fosfomycin, 64 to >512 µg/ml) had a positive test result (Table 1).
There was a strong agreement between the results of the susceptibility test and of the rapid fosfomycin/E. coli NP test, both for susceptible and resistant isolates (Table 1). The sensitivity and specificity were found to be 100% and 98.7%, respectively.
By reading the color change of the wells every 30 min after incubation, we determined that final results could be obtained after 1 h 30 min of incubation at 35 ± 2°C.
Additionally, 10 isolates of K. pneumoniae were evaluated by means of this test, 5 of which were fosfomycin susceptible and 5 of which were fosfomycin resistant. A low correlation between the rapid fosfomycin/E. coli NP test and the agar dilution method was observed. In fact, all samples were found positive with the rapid fosfomycin/E. coli NP test, thereby giving a poor and unacceptable specificity (50%).
DISCUSSION
The rapid fosfomycin/E. coli NP test is a rapid and easy-to-perform test, combining excellent sensitivity and specificity. It detects fosfomycin resistance in E. coli regardless of the molecular mechanism of resistance. This test offers the possibility of detecting fosfomycin resistance from bacterial cultures in 1 h 30 min, which is at least 16 h earlier than with the reference agar dilution method. Even though a discrepancy was observed by using this test (one major error), the sensitivity and specificity remained high, making it a potential useful clinical test.
As for the Rapid Polymyxin NP test, we believe that the rapid fosfomycin/E. coli NP test might be useful for first-step screening, in this case for fosfomycin resistance in E. coli. This use is particularly interesting in a context of increased prevalence of ESBL producers among which resistance to fosfomycin seems to be higher than that observed for non-ESBL producers, with susceptibility rates of 86% and 97%, respectively, as reported in a study from Lebanon (20). Overall, the susceptibility rate of fosfomycin in E. coli (ESBL- and non-ESBL producers) is estimated to be around 90% (21).
Such a test might be useful, considering that the use of molecular-based approaches for the detection of fosfomycin resistance in E. coli is not possible. Indeed, a series of known resistance mechanisms cannot be detected by molecular biology, such as a loss of active transport mechanisms or mutations in the fosfomycin target gene murA (4).
However, the rapid fosfomycin/E. coli NP test presents some limitations. The interpretation of color changes is made visually. Therefore, despite that resistant isolates show a clear switch from orange to yellow, low-level resistance isolates (MICs, 64 and 128 µg/ml; e.g., isolates N140 or N181) might need a more accurate reading and/or a second reader. In addition, this test does not allow discrimination between chromosomally encoded and acquired fosfomycin resistance mechanisms. Finally, another shortcoming of the test could be that it may only be applied to E. coli so far. Since preliminary results with K. pneumoniae isolates showed a poor specificity of the test, we hypothesize that this might be due to the occurrence of fosfomycin-resistant mutants, perhaps showing mutations in an intrinsic chromosomal gene which is homologous to fosA in that species. This test would benefit from a multicenter evaluation. Finally, since E. coli is responsible for more than 75% of UTIs (22), the test responds to most of the clinical need for rapidly choosing an optimal treatment for this infection as well as for UTI-associated septicemia.
ACKNOWLEDGMENTS
This work was financed by the University of Fribourg, Switzerland. It has also been funded by the Swiss National Science Foundation (project number FNS-407240_177382).
REFERENCES
- 1.Hendlin D, Stapley EO, Jackson M, Wallick H, Miller AK, Wolf FJ, Miller TW, Chaiet L, Kahan FM, Foltz EL, Woodruff HB, Mata JM, Hernandez S, Mochales S. 1969. Phosphonomycin, a new antibiotic produced by strains of Streptomyces. Science 166:122–123. doi: 10.1126/science.166.3901.122. [DOI] [PubMed] [Google Scholar]
- 2.Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE, Infectious Diseases Society of A, European Society for M, Infectious D. 2011. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 52:e103–e120. doi: 10.1093/cid/ciq257. [DOI] [PubMed] [Google Scholar]
- 3.Liu HY, Lin HC, Lin YC, Yu SH, Wu WH, Lee YJ. 2011. Antimicrobial susceptibilities of urinary extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae to fosfomycin and nitrofurantoin in a teaching hospital in Taiwan. J Microbiol Immunol Infect 44:364–368. doi: 10.1016/j.jmii.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Castaneda-Garcia A, Blazquez J, Rodriguez-Rojas A. 2013. Molecular mechanisms and clinical impact of acquired and intrinsic fosfomycin resistance. Antibiotics (Basel) 2:217–236. doi: 10.3390/antibiotics2020217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falagas ME, Vouloumanou EK, Samonis G, Vardakas KZ. 2016. Fosfomycin. Clin Microbiol Rev 29:321–347. doi: 10.1128/CMR.00068-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wachino J, Yamane K, Suzuki S, Kimura K, Arakawa Y. 2010. Prevalence of fosfomycin resistance among CTX-M-producing Escherichia coli clinical isolates in Japan and identification of novel plasmid-mediated fosfomycin-modifying enzymes. Antimicrob Agents Chemother 54:3061–3064. doi: 10.1128/AAC.01834-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho PL, Chan J, Lo WU, Lai EL, Cheung YY, Lau TC, Chow KH. 2013. Prevalence and molecular epidemiology of plasmid-mediated fosfomycin resistance genes among blood and urinary Escherichia coli isolates. J Med Microbiol 62:1707–1713. doi: 10.1099/jmm.0.062653-0. [DOI] [PubMed] [Google Scholar]
- 8.Lee SY, Park YJ, Yu JK, Jung S, Kim Y, Jeong SH, Arakawa Y. 2012. Prevalence of acquired fosfomycin resistance among extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae clinical isolates in Korea and IS26-composite transposon surrounding fosA3. J Antimicrob Chemother 67:2843–2847. doi: 10.1093/jac/dks319. [DOI] [PubMed] [Google Scholar]
- 9.Benzerara Y, Gallah S, Hommeril B, Genel N, Decre D, Rottman M, Arlet G. 2017. Emergence of plasmid-mediated fosfomycin-resistance genes among Escherichia coli isolates, France. Emerg Infect Dis 23:1564–1567. doi: 10.3201/eid2309.170560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X, Liu W, Liu Y, Wang J, Lv L, Chen X, He D, Yang T, Hou J, Tan Y, Xing L, Zeng Z, Liu JH. 2014. F33: A-: B-, IncHI2/ST3, and IncI1/ST71 plasmids drive the dissemination of fosA3 and blaCTX-M-55/-14/-65 in Escherichia coli from chickens in China. Front Microbiol 5:688. doi: 10.3389/fmicb.2014.00688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakamura G, Wachino J, Sato N, Kimura K, Yamada K, Jin W, Shibayama K, Yagi T, Kawamura K, Arakawa Y. 2014. Practical agar-based disk potentiation test for detection of fosfomycin-nonsusceptible Escherichia coli clinical isolates producing glutathione S-transferases. J Clin Microbiol 52:3175–3179. doi: 10.1128/JCM.01094-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo Q, Tomich AD, McElheny CL, Cooper VS, Stoesser N, Wang M, Sluis-Cremer N, Doi Y. 2016. Glutathione-S-transferase FosA6 of Klebsiella pneumoniae origin conferring fosfomycin resistance in ESBL-producing Escherichia coli. J Antimicrob Chemother 71:2460–2465. doi: 10.1093/jac/dkw177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ito RMM, Tomich AD, Callaghan JD, McElheny CL, Mettus RT, Shanks RMQ, Sluis-Cremer N, Doi Y. 2017. Widespread fosfomycin resistance in Gram-negative bacteria attributable to the chromosomal fosA gene. mBio 8:e00749-17. doi: 10.1128/mBio.00749-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu H, Miao V, Kwong W, Xia R, Davies J. 2011. Identification of a novel fosfomycin resistance gene (fosA2) in Enterobacter cloacae from the Salmon River, Canada. Lett Appl Microbiol 52:427–429. doi: 10.1111/j.1472-765X.2011.03016.x. [DOI] [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute. 2018. Performance standards for antimicrobial susceptibility testing; 28th informational supplement. CLSI document M100-S28. Clinical Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 16.Hirsch EB, Raux BR, Zucchi PC, Kim Y, McCoy C, Kirby JE, Wright SB, Eliopoulos GM. 2015. Activity of fosfomycin and comparison of several susceptibility testing methods against contemporary urine isolates. Int J Antimicrob Agents 46:642–647. doi: 10.1016/j.ijantimicag.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 17.de Cueto M, Lopez L, Hernandez JR, Morillo C, Pascual A. 2006. In vitro activity of fosfomycin against extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae: comparison of susceptibility testing procedures. Antimicrob Agents Chemother 50:368–370. doi: 10.1128/AAC.50.1.368-370.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nordmann P, Jayol A, Poirel L. 2016. Rapid detection of polymyxin resistance in Enterobacteriaceae. Emerg Infect Dis 22:1038–1043. doi: 10.3201/eid2206.151840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.European Committee on Antimicrobial Susceptibility Testing. 2018. Breakpoint tables for interpretation of MICs and zone diameters, version 8.1. European Committee on Antimicrobial Susceptibility Testing, Växjö, Sweden. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_8.1_Breakpoint_Tables.pdf.
- 20.Araj GF, Jaber FA. 2012. In vitro activity of fosfomycin and other antimicrobials against uropathogenic Escherichia coli and Klebsiella pnuemoniae at a tertiary care center in Lebanon. Lebanese Medical J 60:142–147. [PubMed] [Google Scholar]
- 21.Falagas ME, Kastoris AC, Kapaskelis AM, Karageorgopoulos DE. 2010. Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum β-lactamase producing, Enterobacteriaceae infections: a systematic review. Lancet Infect Dis 10:43–50. doi: 10.1016/S1473-3099(09)70325-1. [DOI] [PubMed] [Google Scholar]
- 22.Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. 2015. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Micro 13:269–284. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]


