Abstract
Background and Objective:
Prostate cancer is considered as one of the most common malignancies in males. Despite the decreasing trend during the past decade, the incidence continues to rise in adolescents worldwide. Recently, new emerging technologies beside TRUS-guided prostate biopsy were introduced and showed high potential in the diagnosis of prostate cancer. The current study aimed at investigating the role of blood cell count and its prognostic value on pathologic findings.
Methods:
The current prospective analysis was conducted on patients with abnormality from January 2013 to January 2016. A total of 168 CBC tests including absolute Neutrophil and lymphocyte counts were performed on males at the Department of Urology, Razi University Hospital (Guilan, Iran). Of these, all males had both CBCs and free:total (F/T) prostate-specific antigen (PSA) ratio.
Results:
Average age of patients was 63.5±7. It was observed that Neutrophil count and Neutrophil percentage was not significantly different among the groups with different pathologies. In comparison to biopsy findings none of the cell count had suitable specificity and sensitivity. In the multivariate analysis to predict malignancy, only age (B=0.1, S.E=0.04, EXP [B]) =1.1 and sig=0.00) and PSA level (B=0.1, S.E=0.04, EXP [B]) =1.1 and sig=0.00) were significant.
Conclusions:
In comparison to biopsy findings, none of the cell counts (absolute or percent) had suitable specificity and sensitivity, and the cell count and percentage before biopsy were not different among the groups with different pathologies. Powerful and long-term studies are required to evaluate prognostic values of cell count on adenocarcinoma.
Key Words: Neutrophil/Lymphocyte Ratio, Prostate, Pathology, Biopsy
Introduction
Prostate cancer is considered as one of the most common malignancies in males (1). About 14% of males are diagnosed with prostate cancer sometime through their lifespan (2). Despite the decreasing trend of the prostate cancer during the last 10 years, there is an increase in incidence of the prostate cancer among adolescents (3).
Up to now the gold standard to detect prostate adenocarcinoma in patients suspected to prostate cancer is systematic standard transrectal ultrasound (TRUS)guided biopsy of the prostate (4).
The current study aimed at finding any relationships between the neutrophil count and neutrophil/lymphocyte ratio to the pathologic reports of the TRUS-guided biopsy of the prostate. The study also sought to find their prognostic values.
Material and method Patients
The current prospective analysis was conducted on patients from January 2013 to January 2016.
After receiving permission from the Research Ethics Board (REB) of our hospital, a total of 168 complete blood count (CBC) tests including absolute neutrophil and lymphocyte counts were performed on males at the Department of Urology, Razi University Hospital (Guilan, Iran). Of these, all males had both CBCs and free: total (F/T) prostate-specific antigen (PSA) ratio. The study also investigated subjects undergoing TRUS-guided biopsy of the prostate with abnormal digital rectal exam or PSA levels in suspicious range. The current study protocol was approved by the Institutional Review Board of Guilan University of Medical sciences, Rasht, Iran.
The exclusion criteria were: known malignancy other than prostate, history of local or systemic infection, any medication related to inflammatory condition of patient such as corticosteroids and hematologic dyspraxia.
Clinical and laboratory assessments
Blood samples were collected one day before biopsy and after antibiotic prophylaxis. Total WBC, neutrophil, and lymphocyte counts were reported by Sysmex XE-2100 Hematology Analyzer (Sysmex Corp., Kobe, Japan). Neutrophil-to-lymphocyte ratio (NLR), absolute neutrophil count was defined by dividing absolute lymphocyte counts. CRP levels were measured by means of automated latex-enhanced turbid metric immunoassay (Dimension; Dade Behring, Newark, NJ, USA; TBA-200FR; Toshiba, Tokyo, Japan) in the first hour after sampling.
Two experienced pathologists with more than five years of experience to diagnose prostate pathology reviewed the specimens to verify the diagnosis. The Gleason score (GS) grading system, 2010 update, was used to grade prostate (5).
Treatment
A urology PGY-4 resident with satisfactory experience in TRUS-biopsy performed all the prostate biopsies in the study. All patients were prepared with spinal anesthetics using a BK ultrasound scanner, end fire transducer, a needle guide, and an 18-G 25-cm biopsy needle; after undergoing ciprofloxacin prophylaxis for three days, the treatment regimens provided to patients remained consistent over the study era.
If pathology was anything other than benign prostatic hyperplasia (BPH) and patient underwent a radical prostatectomy, then the final pathology (and its GS) was considered in the data (13 patients).
Statistical analysis
Patients` demographics were compared between patients with positive and negative prostate adenocarcinoma. Patient with NLR and neutrophil count were also assessed for differences in different pathologic groups. Statistical tests used for the aforementioned univariate analyses included independent samples t test or the Mann Whitney U test for continuous variables and χ2 or the Fisher exact test for categorical variables, where applicable.
The exploratory variables analyzed in univariate and multivariable survival analyses were assessed as follows: age (continuous), CBC count, NLR ratio, PSA (0.4 to 88 ng/mL), and CRP level.
The cut off points of NLR were determined according to the sensitivity and specificity levels derived from the area under receiver operator characteristics (AUROC) curve plotted using the presence or absence of prostatic carcinoma.
Statistical tests were two sided with α significance level of 0.05. All analyses were performed with SPSS version 20.
Results
Basic characteristics
From October 2013 to march 2016, 168 biopsies were undertaken on 168 patients. The mean age of patients was 63. 5±7 years; their first PSA level was 11.6±10.1 ng/mL in average and after mean four weeks of taking anti-inflammatory by all patients, and antibiotic therapy in 89 patients (53%) PSA reached 10.6±7.4 ng/mL. The mean prostate volume was 56±25.8 mL among the current study patients.
Complete cell count was performed in all patients one day before surgery. Mean WBC count was 7303±1498/µL. Mean±SD percentage of neutrophil was 60.7%±8.01%, lymphocytes 31.9%±8%, eosinophils 4%±1.98%, and monocytes in 3.3%±2.42%, but there was no report of basophil.
Results of CRP tests were negative in 68 patients (40.5%) and positive in 100 patients (59. 5%). Patient’s urinalysis was also examined and it was observed that 113 (67.3%) patients had hematuria (RBC more than 3) and 124 (73.8%) had pyuria; although in no sample bacteria was reported more than 10, all urine cultures were negative.
Pathologic finding
Among the 168 patients undergoing the biopsy, the pathology reports were BPH in 100 patients (59.5%), adenocarcinoma in 59 (35.1%), ASAP in six (3.6%) and active prostatitis in three (1.8. Gleason scorings are shown in Table 1).
Correlations
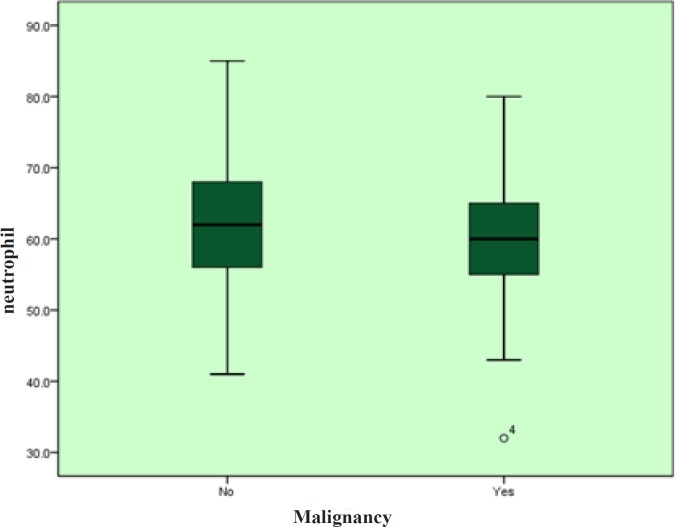
It was observed that neutrophil counts and neutrophil percentage were not different among the groups with different pathologies. After that the pathologies were divided into two benign and malignant groups and previous findings were confirmed, Figure 1 and 4.
NLR was in contrast with GS (P >0.05).
Urinalysis and CRP test had no difference in different cell counts (P >0.05). In comparison to biopsy findings, none of the cell counts (absolute or percent) had suitable specificity and sensitivity (P >0.05).
In multivariate analysis to predict malignancy, only age (B=0.1, S. E=0.04, EXP [B] =1.1 and sig=0.00) and PSA level (B=0.1, S. E=0.04, EXP [B] =1.1 and sig=0.00) were significant.
Figure 1.
Mean Age of Patients in Different Pathology Groups
Figure 2.
Gleason scoring in patients diagnosed with adenocarcinoma in five distinct grade groups based on the modified Gleason score groups. Grade group 1 = Gleason score ≤6, grade group 2 = Gleason score 3 + 4 = 7, grade group 3 = Gleason score 4 + 3 = 7, grade group 4 = Gleason score 8, grade group 5 = Gleason scores 9 and 10.
Figure 3.
ROC curve shows specificity and sensitivity of blood cell counts to diagnose prostate adenocarcinoma
Figure 4.
Neutrophill Percentage in Patients With and Without Adenocarcinoma
Discussion
Little data were found about NLR and its prognostic value on histology of prostate biopsies (6-8).
Inflammation’s dark side is a dominant power in cancer growth, where it supports and assists tumor growth and metastasis (9). Neutrophils can have an important influence on the tumor microenvironment via their specific characters to modify tumor cell proliferation, angiogenesis, and metastasis, and due to that some researchers explored tumor-associated neutrophils as a means of antitumor therapy (10).
No relationship was observed between hematologic, inflammatory, and laboratory findings of the blood count and histology of prostate biopsy. Fujita et al.,
(11) showed an elevated neutrophil count that can be an indicator of good prostate biopsy, unlike finding was proposed by Kawahara (12). Although some researchers did not find any differences between NLR and prostate biopsy (6), similar to the results of the current study, data discrepancy may be due to different methods and lack of sufficient data; especially data about NLR were inconsistent, blood sampling was different with respect to time and antibiotic therapy (13, 14), also most of studies investigated NLR on survival (15) and some researchers evaluated its impact on specific PCA groups such as metastatic castration resistant prostate carcinoma (mCRPC) (16).
No association was observed between NLR and PSA. Yuksel (17) also did not find any relationships between PSA and NLR; pretreatment NLR was observed in the majority of studies unrelated to PSA (6, 7, 13), but there was a relationship after treatment (14). Maeda et al., (12) reported that NLR, with or without combination with F/T PSA ratio, may function as a new biomarker to predict prostate cancer in males undergoing prostate needle biopsy. Although some researchers believe that NLR is related to PSA (6, 18), Kawahara (13) reported no significant relationship between NLR and PSA lower than 20 ng/dL, but Sümbül reported that NLR was effective to predict the PSA response in chemotherapy.
As already mentioned, theoretically, systemic inflammation might have an effect on the development and progression of cancer, raised CRP (18), but the current study did not observe such a relationship. McDonald et al. (18), reported that serum CRP to PSA association was not significant after age and multivariable adjustments, similar to the current study findings.
In contrast to the current study findings, Gokce (6) revealed that higher GS was associated with higher NLR. Lee et al., (19) reported that high NLR was significantly related to unfavorable clinicopathological outcomes. Further studies are required to clarify the correlation between NLR and GS.
Gu et al. (15), in a comprehensive meta-analysis, revealed that increased NLR could predict poor overall survival, progression-free survival, and recurrencefree survival. In another recently conducted metaanalysis, increased NLR had a strong relationship with poorer prognosis metastatic castration-resistant prostate cancer (21).
In conclusion, since the results of the current study showed no significant relationship between NLR and PSA, CRP or the pathologic results of the prostate TRUS biopsy, the physicians should reconsider using NLR as a decision making parameter to diagnose and approach the patients suspected to prostate cancer, BPH or inflammatory processes such as prostatitis. Prescription of any kind of medications or antibiotic therapies before prostate biopsy should not be relied on the neutrophil count or the NLR index only.
Weakness: It seems to be crucial to evaluate long term prognostic value of blood cell count.
Conflict of interest
The authors declare that there was no conflict of interest.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Inter- national journal of cancer. 2010;127(12):2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Howlader N NA, Krapcho M, Garshell J, Mill- er D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER Cancer Sta- tistics Review, 1975-2012, National Cancer In- stitute. 2014. [Google Scholar]
- 3.Barr RD, Ries LA, Lewis DR, Harlan LC, Keegan TH, Pollock BH, et al. Incidence and incidence trends of the most frequent cancers in adolescent and young adult Americans, includ- ing “nonmalignant/noninvasive” tumors. Cancer. 2016 doi: 10.1002/cncr.29867. [DOI] [PubMed] [Google Scholar]
- 4.Kongnyuy M, George AK, Rastinehad AR, Pinto PA. Magnetic Resonance Imaging- Ultrasound Fusion-Guided Prostate Biopsy: Review of Technology, Techniques, and Out- comes. Current urology reports. 2016;17(4):32. doi: 10.1007/s11934-016-0589-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein JI. An update of the Gleason grading sys- tem. The Journal of urology. 2010;183(2):433–40. doi: 10.1016/j.juro.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 6.Gokce MI, Hamidi N, Suer E, Tangal S, Husey- nov A, Ibis A. Evaluation of neutrophil-to-lym- phocyte ratio prior to prostate biopsy to predict biopsy histology: Results of 1836 patients. Canadian Urological Association journal = Jour- nal de l’Association des urologues du Canada. 2015;9(11-12):E761–5. doi: 10.5489/cuaj.3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minardi D, Scartozzi M, Montesi L, Santoni M, Burattini L, Bianconi M, et al. Neutrophil-to- lymphocyte ratio may be associated with the outcome in patients with prostate cancer. Spring- erPlus. 2015;4:255. doi: 10.1186/s40064-015-1036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langsenlehner T, Thurner EM, Krenn-Pilko S, Langsenlehner U, Stojakovic T, Gerger A, et al. Validation of the neutrophil-to-lym- phocyte ratio as a prognostic factor in a co- hort of European prostate cancer patients. World journal of urology. 2015;33(11):1661–7. doi: 10.1007/s00345-015-1494-7. [DOI] [PubMed] [Google Scholar]
- 9.Rakoff-Nahoum S. Why cancer and inflamma- tion? The Yale journal of biology and medicine. 2006;79(3-4):123–30. [PMC free article] [PubMed] [Google Scholar]
- 10.Gregory AD, Houghton AM. Tumor-associated neutrophils: new targets for cancer therapy. Cancer research. 2011;71(7):2411–6. doi: 10.1158/0008-5472.CAN-10-2583. [DOI] [PubMed] [Google Scholar]
- 11.Fujita K, Imamura R, Tanigawa G, Nakagawa M, Hayashi T, Kishimoto N, et al. Low serum neutrophil count predicts a positive prostate biopsy. Prostate cancer and prostatic diseases. 2012;15(4):386–90. doi: 10.1038/pcan.2012.27. [DOI] [PubMed] [Google Scholar]
- 12.Maeda Y, Kawahara T, Kumano Y, Ohtaka M, Kondo T, Mochizuki T, et al. The neutrophil-to- lymphocyte ratio before repeat prostate needle biopsy for predicting prostate cancer. Urologia Internationalis. 2016 Jan;96(1):123–124. doi: 10.1159/000442895. [DOI] [PubMed] [Google Scholar]
- 13.Kawahara T, Furuya K, Nakamura M, Sakamaki K, Osaka K, Ito H, et al. Neutrophil-to-lympho- cyte ratio is a prognostic marker in bladder can- cer patients after radical cystectomy. BMC cancer. 2016;16(1):185. doi: 10.1186/s12885-016-2219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sümbül AT, Sezer A, Abalı H, Köse F, Gül- tepe I, Mertsoylu H, Muallaoğlu S, Özyılkan Ö. Neutrophil-to-lymphocyte ratio predicts PSA response, but not outcomes in patients with castration-resistant prostate cancer treated with docetaxel. International urology and ne- phrology. 2014;46(8):1531–5. doi: 10.1007/s11255-014-0664-7. [DOI] [PubMed] [Google Scholar]
- 15.Gu X, Gao X, Li X, Qi X, Ma M, Qin S, et al. Prog- nostic significance of neutrophil-to-lymphocyte ratio inprostatecancer: evidencefrom 16,266 pa- tients. Scientific reports. 2016;6:22089. doi: 10.1038/srep22089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Soest RJ, Templeton AJ, Vera-Badillo FE, Mercier F, Sonpavde G, Amir E, et al. Neu- trophil-to-lymphocyte ratio as a prognostic biomarker for men with metastatic castration- resistant prostate cancer receiving first-line che- motherapy: data from two randomized phase III trials. Annals of Oncology. 2015;26(1):743–749. doi: 10.1093/annonc/mdu569. [DOI] [PubMed] [Google Scholar]
- 17.Yuksel OH, Urkmez A, Akan S, Yldirim C, Verit A. Predictive Value of the Platelet-To- Lymphocyte Ratio in Diagnosis of Prostate Cancer. Asian Pacific journal of cancer preven- tion : APJCP. 2015;16(15):6407–12. doi: 10.7314/apjcp.2015.16.15.6407. [DOI] [PubMed] [Google Scholar]
- 18.McDonald AC, Vira MA, Vidal AC, Gan W, Freedland SJ, Taioli E. Association be- tween systemic inflammatory markers and serum prostate-specific antigen in men with- out prostatic disease - the 2001-2008 National Health and Nutrition Examination Sur- vey. The Prostate. 2014;74(5):561–7. doi: 10.1002/pros.22782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee H, Jeong SJ, Hong SK, Byun SS, Lee SE, Oh JJ. High preoperative neutrophil-lym- phocyte ratio predicts biochemical recurrence in patients with localized prostate cancer af- ter radical prostatectomy. World J Urol. 2016 Jun;34(6):821–7. doi: 10.1007/s00345-015-1701-6. [DOI] [PubMed] [Google Scholar]