Abstract
We report the first case series of ICI-associated colitis successfully treated with fecal microbiota transplantation (FMT), with reconstitution of the gut microbiome and a relative increase in the proportion of regulatory T cells (Tregs) within the colonic mucosa. These preliminary data provide evidence that modulation of the gut microbiome may abrogate ICI-associated colitis.
Immunotherapy has transformed the field of oncology improving long-term survival in patients across numerous cancer types. Treatments with immune checkpoint inhibitors (ICI) targeting cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), programmed cell death protein 1 (PD-1) and programmed cell death ligand 1 (PD-L1) are associated with increased T cell activation and effective anti-tumor immune responses in a subset of patients, but treatment can be associated with serious immune-related adverse effects (irAEs) in some patients1. One of the most common toxicities is ICI-associated colitis. This can be quite severe and closely resembles colitis associated with autoimmune pathophysiology including inflammatory bowel disease (IBD)2,3. ICI-associated colitis is routinely treated with immunosuppressive therapy, including corticosteroids and/or agents targeting tumor necrosis factor alpha (TNF-alpha), all of which have significant side effects. Recommendations regarding optimal management of ICI-induced colitis continue to evolve4–9. Interestingly, recent randomized clinical studies suggest that other types of colitis, including Clostridium difficile-associated colitis and IBD, can be successfully treated by modulation of the gut microbiome with fecal microbiota transplantation (FMT)10.
Previously, we demonstrated that differential bacterial signatures comprise the gut microbiome of responders versus non-responders to ICI therapy and additionally showed that modulation of the gut microbiome of germ-free mice via FMT from patients could alter anti-tumor immunity and response to ICI therapy in gnotobiotic mice11–13. Other groups have also demonstrated differential bacterial signatures in the gut microbiome of patients who develop ICI-associated colitis14–16 and have shown that targeting specific bacterial taxa may abrogate ICI-related toxicity in pre-clinical models17. However, approaches incorporating modulation of the microbiome to treat ICI-associated colitis have not yet been explored in patients. Herein, we document results from the first reported case series of two patients with refractory ICI-associated colitis successfully treated with FMT and describe changes in the immune microenvironment following FMT, a potential mechanism of action through which modulation of the gut microbiome may impact ICI-associated colitis.
We sought to determine the impact of treatment with FMT from healthy donors in patients with refractory ICI-associated colitis and enrolled two patients onto this treatment protocol between June 2017 and January 2018 (CIND17–0036, CIND17–0058). Clinical courses for both patients are further detailed in Supplemental Figs. 1–3. The first patient was a 50-year-old female with high-grade metastatic urothelial carcinoma refractory to standard chemotherapy who was enrolled onto a trial of combined CTLA-4 and PD-1 blockade (NCT1928394). Two weeks after treatment initiation, she was hospitalized with CTCAE Grade ≥ 2 diarrhea/colitis. An infectious workup including PCR-based multiplex assay for common GI pathogens was negative, and colonoscopy demonstrated severe colitis that endoscopically resembled ulcerative colitis (Fig. 1a and Supplemental Figs. 3a and 4a). She received systemic corticosteroids, followed later by two doses of an anti-TNF-alpha agent (infliximab) as well as one dose of anti-integrin therapy (vedolizumab), but her symptoms persisted. She then received a single dose of FMT (50 grams of donor stool) via colonoscopy. The second patient enrolled was a 78-year-old male with prostate cancer refractory to chemotherapy and hormonal therapy who received two doses of ipilimumab in the context of a clinical trial (NCT02113657). Three months after treatment initiation, he was hospitalized with fever and CTCAE Grade ≥ 2 diarrhea/colitis. Infectious etiologies were excluded and colonoscopy confirmed the diagnosis of ICI-associated colitis, though with a Crohn’s colitis-like presentation (Fig. 1d and Supplemental Figs. 3b and 4b). His symptoms persisted despite systemic corticosteroids, infliximab and vedolizumab. He received two doses of FMT. The source of all three FMT products was from a single healthy unrelated donor, collected at three different time points.
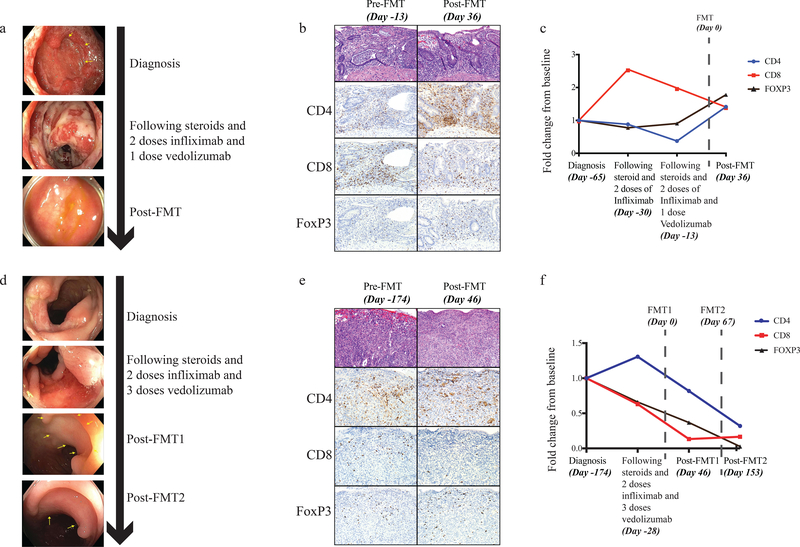
Figure 1:
Endoscopic changes and characterization of colonic mucosal infiltrate throughout clinical course for Patient 1 (a-c) and Patient 2 (d-f). (a) Changes in colonic mucosa as assessed by full colonoscopy. Near the time of diagnosis (row 1), multiple large ulcers and diffuse inflammatory exudate are present (in the distal 40cm of the colon only, with the normal appearing proximal colon) and remain despite months of treatment with steroids and biologic immunosuppressive agents (steroid + 2 doses infliximab + 1 dose vedolizumab) (row 2). Approximately one month after FMT (row 3), colonic mucosa exhibits grossly normal vasculature, minimal patchy erythema, and near-complete healing of prior ulcers. Yellow arrows point to ulcerative lesions. This patient had full colonoscopic evaluations that examined every segment of the colon (ascending, transverse, descending, sigmoid and rectum). Endoscopy was performed once at each time point. Given the qualitative nature of endoscopic data collection and inability to provide true statistical analyses, we chose to include multiple other representative photos from the same colonoscopic evaluations. Additional representative photos are presented in Supplemental Figure 4a. (b) Immunohistochemical analysis of mucosal biopsies of the colon/rectum prior to, and following, FMT. A single slide representative of the endoscopic biopsy specimen as a whole was stained for each patient for each time point. Representative slides from additional time points are included in Supplemental Figure 5a. (c) Analysis of changes in the density immune cell subsets (CD8 red squares, CD4 blue circles, FOXP3 black triangles) over time, expressed as a fold change from baseline based on total densities of cells expressing these markers (absolute densities are presented in Supplemental Figure 6a). Timepoints include time of diagnosis, prior to FMT, following steroids and biologic immunosuppression and following FMT. Date of FMT is represented by dotted vertical line and is designated Day 0. These data represent the average cell density from 4 regions of interest (ROIs) per sample (single slide per patient at each time point) with each ROI measuring 500 μm x 500 μm for a total of 0.25 mm2. We report the mean # IHC-positive cells/mm2 divided by the mean # IHC-positive cells/mm2 at baseline. (d) Changes in colonic mucosa as assessed by full colonoscopy. Near the time of diagnosis (row 1), multiple large ulcers and inflammatory exudate is present (throughout the entire colon) and remains after unsuccessful treatment with steroids and biologic immunosuppressive agents (steroid + 2 doses infliximab + 4 doses vedolizumab) (row 2). There is notable improvement following first FMT (row 3) but residual ulcers remain. Following second FMT (row 4) we note near complete resolution of all ulcerative lesions. Again full endoscopic examinations were performed, once for each time point. Additional representative photos from the colonoscopic evaluation are shown in Supplemental Figure 4b. (e) Immunohistochemical analysis of mucosal biopsies of the colon/rectum taken prior to first FMT and following first FMT. A single slide representative of the endoscopic biopsy specimen was stained for each patient for each time point. Representative slides from additional time points are included in Supplemental Figure 5b. (f) Analysis of changes in the density immune cell subsets (CD8 red squares, CD4 blue circles, FOXP3 black triangles) over time, expressed as a fold change from baseline based on total densities of cells expressing these markers (absolute densities are presented in Supplemental Figure 6b). These data represent the average cell density from 4 regions of interest (ROIs) per sample (single slide per patient at each time point) with each ROI measuring 500 μm x 500 μm for a total of approximately 1 mm2. We report the mean # IHC-positive cells/mm2 divided by the mean # IHC-positive cells/mm2 at baseline. Date of first (Day 0) and second FMT (Day 67) are represented by dotted vertical lines.
Both patients had complete resolution of clinical symptoms following treatment with FMT, with eventual return to normal solid daily bowel movements without further bleeding (Supplemental Fig. 3). In the first patient, complete resolution occurred gradually within 2 weeks and she was weaned off steroids in 7 days (Supplemental Fig. 3a), while the second patient experienced partial improvement of GI symptoms but with persistent ulcers on follow-up colonoscopy and recurrent abdominal pain; he experienced complete resolution after a second FMT treatment (Supplemental Fig. 3b).
Endoscopic evaluation demonstrated significant mucosal inflammation and ulceration in both patients near the time of diagnosis of ICI-colitis, without substantial improvement after systemic corticosteroids, anti-TNF and anti-integrin agents. Following FMT, marked improvement was evident on endoscopic evaluation, with reduced inflammation and resolution of ulcerations (Fig. 1a and 1d and Supplemental Figs. 3 and 4). In the first patient, analysis of immune infiltrates in the colonic mucosa demonstrated a dense inflammatory infiltrate prior to FMT with a high density of CD8+ cytotoxic T lymphocytes and a low density of CD4+ FoxP3+ T cells (Fig. 1b-c and Supplemental Figs. 5a and 6a), consistent with findings from reports of autoimmune colitis18,19. Following FMT, there was a substantial reduction in CD8+ T-cell density with a concomitant increase in CD4+ FoxP3+ (Fig. 1b-c and Supplemental Figs. 5a and 6a), offering a potential mechanism through which FMT could abrogate ICI-associated toxicity. In the second patient, the density of all T cell subtypes analyzed decreased following FMT, but the CD4+ T cell population was relatively spared compared to the CD8+ T cell population, with persistence again noted for CD4+ and FoxP3+ cells (Figs. 1e-f and Supplemental Figs. 5b, 6b and 7).
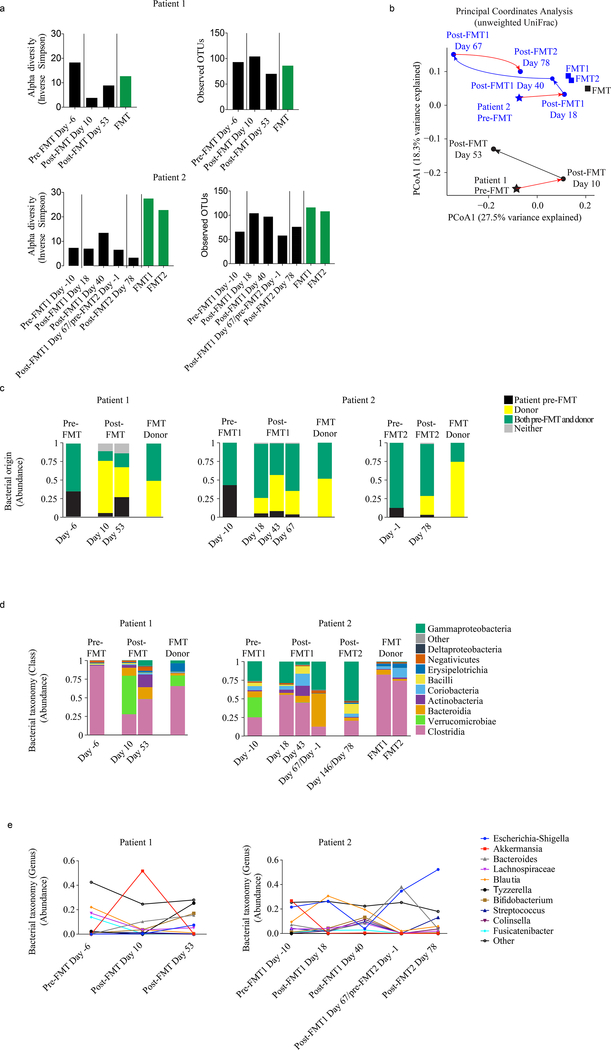
Importantly, stool samples were collected from patients prior to FMT and serially following FMT to assess the diversity and composition of the microbiome before and after intervention via 16S sequencing (Supplemental Figs. 1–2). Results demonstrated variable pre-treatment alpha diversity compared to the healthy FMT donor (Fig. 2a). There was no observable trend in alpha diversity following treatment, measured by the inverse Simpson’s index. Numbers of observed OTUs, however, did consistently rise following each FMT in both patients, though in both cases they would later come back down (Fig. 2a). Principal coordinates analyses of unweighted UniFrac distances demonstrated that the gut microbiome of patients became most similar to the FMT donor immediately following treatment, but, in both cases later deviated away though remaining distinct compared to pre-FMT (Fig. 2b). An evaluation of unique 16S sequences20 detectable in patient pre-FMT baseline samples and FMT products was used to determine probable bacterial origins in longitudinal samples, demonstrating considerable abundances of bacteria of donor origin that stably joined the patient’s intestinal microbiome with each FMT procedure (Fig. 2c).
Figure 2:
Microbiome analysis of patient and donor intestinal bacteria by 16S deep sequencing. The patients’ stool microbiomes were longitudinally sampled at indicated time points before and after FMT, along with samples from the FMT donor. Between 3380 and 42,776 sequences were obtained for each sample (average 10,003). (a) Alpha diversity, quantified by the inverse Simpson index after rarefying to 3000 sequences, as well as total observed OTU numbers, was evaluated for patient and FMT donor samples. (b) Using principal coordinate analysis of unweighted UniFrac distances, microbiome samples from (a) are depicted in space with more similar samples located closer together. (c) Bacterial 16S sequences from samples in (a) were classified by origin (unique to patient baseline, unique to donor, present in both patient baseline and donor, or absent in both patient baseline and donor). (d) Sequences were classified by taxonomy at the Class level. (e) Changes in the abundances of top varying 10 bacterial genera over time.
We next assessed bacterial taxa present at time of colitis in these patients as well as compositional changes in the gut microbiome following treatment with FMT. Bacterial taxa present at time of colitis were quite disparate between the two patients, with a predominance of Clostridia and a notable absence of bacteria shown to be protective against ICI-associated colitis and IBD such as Bacteroidia14,16 and Verrucomicrobiae21 respectively in the first patient and a predominance of Gammaproteobacteria (predominantly Escherichia) in the second patient, which is commonly seen in perturbed intestinal states22. Immediately following FMT in the first patient, donor FMT-derived bacteria had effectively colonized the intestinal tract, with nearly 75% of the sequences uniquely attributable to the FMT donor microbiome and a notably higher abundance of Akkermansia (Fig. 2d-e). By week 7 after FMT, Akkermansia now only accounted for a small portion of her microbiome and there was further expansion of Clostridia which were largely patient-derived in origin (Fig. 2d, left and 2e, left). Of note, the patient also showed an expansion of Bifidobacterium after FMT, which recently was reported to abrogate ICI-related toxicity in a murine model17 (Fig. 2d, left and 2e, left). In the second patient, there was a notable increase in the abundance of Blautia and Bifidobacterium species after FMT, which have been associated with reduced intestinal inflammation (Fig. 2d, right and 2e, right)23,17. In addition to this, he had a decrease in the abundance of potentially pathogenic Escherichia and an increase in potentially beneficial Bacteroides after his first FMT (Fig. 2d, right and 2e, right). After his second FMT, he had a higher abundance of Escherichia and eventual decrease in Bacteroides; however, his gastrointestinal symptoms steadily continued to improve (Fig. 2d, right and 2e, right).
Together, these cases provide provocative and novel evidence that modulation of the gut microbiome via FMT can be associated with significant and rapid improvement of refractory ICI-associated colitis with early insights into potential mechanisms; however, significant limitations exist with this very small cohort and additional studies are needed to assess the utility of this approach as well as to provide further mechanistic insight. Given the widespread application of ICI with expanding indications across cancer types, it is anticipated that there will be an increased incidence in ICI-associated colitis and other irAEs. Thus, further investigations building on this approach are critically needed.
Supplementary Material
Acknowledgements of Funding Support:
Andrew Sabin Family Fellows Program (private donation): J.A.W.
MD Anderson Cancer Center’s Melanoma Moon Shot Program (710499-80-111538-19): J.A.W.
American Association for Cancer Research Stand Up to Cancer (SU2C-AACR-IRG-19-17): J.A.W.
National Institutes of Health (R01 CA219896-01A1): J.A.W.
National Institutes of Health (R01 HL124112): R.R.J.
Cancer Prevention and Research Institute of Texas Grant (RR160089): R.R.J.
Footnotes
Competing Interests Declaration:
J.A.W and V.G. are inventors on a US patent application (PCT/US17/53,717) submitted by The University of Texas MD Anderson Cancer Center that covers methods to enhance checkpoint blockade therapy by the microbiome. J.A.W. is a clinical and scientific advisor at Microbiome DX and a consultant at Biothera Pharma, Merck Sharp, and Dohme. J.A.W. has honoraria from speakers’ bureau of Dava Oncology, Bristol-Myers Squibb, Gilead, Illumina, Omniprex, Imedex and is an advisory board member for GlaxoSmithKline, Novartis, and Roche/Genentech, Astra-Zeneca. V.G. is a consultant at Microbiome DX, and reports honoraria from ExpertConnect. R.R.J. is on the scientific advisory board for Seres Therapeutics, Inc., has consulted for Ziopharm Oncology and Microbiome Dx, and holds patents licensed to Seres Therapeutics, Inc. M.T.T. serves on the advisory board for Novartis, Seattle Genetics and Myriad Genetics. J.A.W., P.S., and J.P.A. are members of the Parker Institute for Cancer Immunotherapy at MD Anderson Cancer Center. P.S. is a consultant for Bristol-Myers Squibb, Jounce Therapeutics, Helsinn, and GlaxoSmithKline and is also a stockholder from Jounce Therapeutics. J.P.A. is a consultant and stockholder for Jounce Therapeutics, receives royalties from Bristol-Myers Squibb, and has intellectual property with Bristol-Myers Squibb and Merck. The other authors declare no competing interests.
Data Availability Statement:
Patient-related data not included in the paper were generated as part of clinical trials and may be subject to patient confidentiality. Any data and materials that can be shared will be released via a Material Transfer Agreement. Sequence data has been deposited at the European Genome-phenome Archive (EGA), which is hosted by the EBI and the CRG, under accession number EGAS00001003217.
References
- 1.Michot JM, et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer 54, 139–148 (2016). [DOI] [PubMed] [Google Scholar]
- 2.Cramer P & Bresalier RS Gastrointestinal and Hepatic Complications of Immune Checkpoint Inhibitors. Curr Gastroenterol Rep 19, 3 (2017). [DOI] [PubMed] [Google Scholar]
- 3.Chen JH, Pezhouh MK, Lauwers GY & Masia R Histopathologic Features of Colitis Due to Immunotherapy With Anti-PD-1 Antibodies. Am J Surg Pathol 41, 643–654 (2017). [DOI] [PubMed] [Google Scholar]
- 4.Dadu R, Zobniw C & Diab A Managing Adverse Events With Immune Checkpoint Agents. Cancer J 22, 121–129 (2016). [DOI] [PubMed] [Google Scholar]
- 5.Bertrand A, Kostine M, Barnetche T, Truchetet ME & Schaeverbeke T Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med 13, 211 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horvat TZ, et al. Immune-Related Adverse Events, Need for Systemic Immunosuppression, and Effects on Survival and Time to Treatment Failure in Patients With Melanoma Treated With Ipilimumab at Memorial Sloan Kettering Cancer Center. J Clin Oncol 33, 3193–3198 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck KE, et al. Enterocolitis in patients with cancer after antibody blockade of cytotoxic T-lymphocyte-associated antigen 4. J Clin Oncol 24, 2283–2289 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnston RL, Lutzky J, Chodhry A & Barkin JS Cytotoxic T-lymphocyte-associated antigen 4 antibody-induced colitis and its management with infliximab. Dig Dis Sci 54, 2538–2540 (2009). [DOI] [PubMed] [Google Scholar]
- 9.Minor DR, Chin K & Kashani-Sabet M Infliximab in the treatment of anti-CTLA4 antibody (ipilimumab) induced immune-related colitis. Cancer Biother Radiopharm 24, 321–325 (2009). [DOI] [PubMed] [Google Scholar]
- 10.Borody TJ & Khoruts A Fecal microbiota transplantation and emerging applications. Nat Rev Gastroenterol Hepatol 9, 88–96 (2011). [DOI] [PubMed] [Google Scholar]
- 11.Gopalakrishnan V, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359, 97–103 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matson V, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science 359, 104–108 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Routy B, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 359, 91–97 (2018). [DOI] [PubMed] [Google Scholar]
- 14.Dubin K, et al. Intestinal microbiome analyses identify melanoma patients at risk for checkpoint-blockade-induced colitis. Nat Commun 7, 10391 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vetizou M, et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science 350, 1079–1084 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaput N, et al. Baseline gut microbiota predicts clinical response and colitis in metastatic melanoma patients treated with ipilimumab. Ann Oncol 28, 1368–1379 (2017). [DOI] [PubMed] [Google Scholar]
- 17.Wang F, Yin Q, Chen L & Davis MM Bifidobacterium can mitigate intestinal immunopathology in the context of CTLA-4 blockade. Proc Natl Acad Sci U S A 115, 157–161 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kappeler A & Mueller C The role of activated cytotoxic T cells in inflammatory bowel disease. Histol Histopathol 15, 167–172 (2000). [DOI] [PubMed] [Google Scholar]
- 19.Nancey S, et al. CD8+ cytotoxic T cells induce relapsing colitis in normal mice. Gastroenterology 131, 485–496 (2006). [DOI] [PubMed] [Google Scholar]
- 20.Edgar RC UNOISE2: Improved error-correction for Illumina 16S and ITS amplicon reads. (2016). [Google Scholar]
- 21.Png CW, et al. Mucolytic bacteria with increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria. Am J Gastroenterol 105, 2420–2428 (2010). [DOI] [PubMed] [Google Scholar]
- 22.Litvak Y, Byndloss MX, Tsolis RM & Baumler AJ Dysbiotic Proteobacteria expansion: a microbial signature of epithelial dysfunction. Curr Opin Microbiol 39, 1–6 (2017). [DOI] [PubMed] [Google Scholar]
- 23.Jenq RR, et al. Intestinal Blautia Is Associated with Reduced Death from Graft-versus-Host Disease. Biol Blood Marrow Transplant 21, 1373–1383 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.