Abstract
Background/Aims
Adequate bowel preparation is essential for an effective and safe colonoscopy. This study aimed to evaluate the quality of bowel preparation according to waiting times from education to colonoscopy.
Materials and Methods
A prospective, investigator-blinded, randomized study was performed from December 2016 to March 2017. Patients were divided into two groups: within 2 weeks (group A, n=64) or more than 2 weeks (group B, n=66) from education about bowel preparation to colonoscopy. The primary outcome was the quality of bowel preparation as assessed by the Boston Bowel Preparation Scale (BBPS). The secondary outcome was the polyp and adenoma detection rate.
Results
A total of 130 patients were enrolled. The total BBPS score was significantly higher in group A (within 2 weeks from education to colonoscopy) than in group B (more than 2 weeks). Total BBPS scores were 8.25±0.97 in group A and 7.75±1.32 in group B (P=.017). The rate of good preparation (BBPS≥8) was higher in group A than in group B (78.1% vs. 59.1%, P=.020). The rates of polyp and adenoma detection were both slightly higher in group A (polyps, 42.2% vs. 38.5%, P=.667; adenoma, 31.2% vs. 22.7%, P=.275). A numerical trend was observed for the slightly superior polyp and adenoma detection rate in group A, but it was not statistically significant.
Conclusion
This study demonstrated that shorter waiting times from education to colonoscopy can improve the quality of bowel preparation. Ensuring sufficient staff and equipment for endoscopy is one approach to reducing waiting times to colonoscopy. If waiting times can not be reduced, more contact through telephone, e-mail, and text messaging could be used to remind patients about information regarding bowel preparation.
Keywords: Colonoscopy, bowel preparation, waiting times
INTRODUCTION
Colorectal cancer is a major public health concern in developed and developing countries. In 2015, there were an estimated 774.000 deaths due to colorectal cancer worldwide according to the World Health Organization. Colonoscopy is an effective tool for the early detection and prevention of colorectal cancer (1–3). Adequate bowel preparation is essential for an accurate and safe colonoscopy (2–3), and inadequate bowel preparation is a major cause of missed adenoma and cancer (4). Many studies have reported risk factors associated with inadequate bowel preparation (5–9); however, the relationship between the waiting time from education to colonoscopy and risk of inadequate bowel preparation has not been studied in detail. Chan et al (10) reported that appointment waiting times influenced the quality of bowel preparation, and a prolonged appointment waiting time of >16 weeks was associated with poor bowel cleansing (odds ratio: 1.86, P=.035). Another retrospective study (11) in the United States did not identify waiting time as a risk factor for poor bowel cleansing, but in this study the mean waiting time was 4.3 weeks. However, in these previous studies, bowel cleansing was not assessed by a validated scale such as the Ottawa scale or the Boston Bowel Preparation Scale (BBPS). Furthermore, mean waiting times vary across countries because of differences in health insurance, the availability of resources such as endoscopy units and staff, and education level about colonoscopy screening. In South Korea, colonoscopy is widely accessible due to support from the health insurance system and adequate resources, and it is uncommon for waiting times to exceed 8 weeks unless a patient opts to delay the procedure. Therefore, this study aimed to evaluate the quality of bowel preparation according to waiting time to colonoscopy in South Korea. Enrolled patients were divided into those who underwent colonoscopy in fewer or more than 2 weeks from being educated about the bowel preparation procedure.
MATERIALS AND METHODS
Subjects
This prospective, endoscopist-blinded, randomized study was performed at a single university hospital from December 2016 to March 2017. All consecutive outpatients between 20 and 70 years of age who were scheduled to undergo colonoscopy for screening and surveillance were enrolled. The following exclusion criteria were applied: age under 20 years or above 70 years, pregnancy, lactation, bowel obstruction, structural intestinal disorders, congestive heart failure, liver failure, inflammatory bowel disease, or inability to provide informed consent. All participants provided written informed consent. This study was approved by the Institutional Review Board (HPIRB 2016-11-007-002).
Bowel preparation method and education
All patients ingested a low-volume (2 L) polyethylene glycol solution with 20 g ascorbic acid (PEG-Asc, Coolprep®, Taejun Co., Seoul, South Korea) as a bowel cleansing agent. A split-dose bowel preparation was used in both groups. Patients ingested 1 L of solution in the evening before colonoscopy (up to 21:00) and the remaining 1 L in the early morning at least 2 hours before the procedure. On the day before the colonoscopy, patients had a normal diet for breakfast and lunch and a soft diet for dinner. Patients were told to start a low-fiber diet 3 days before the colonoscopy and received instructions and a list of unacceptable foods. All patients were educated about bowel preparation by a single nurse trained to provide this information and were also provided with written instructions (a brochure) at the time of making the colonoscopy appointment.
Randomization and blinding
All eligible patients were randomly assigned to one of two groups: within 2 weeks or more than 2 weeks from education about bowel preparation to colonoscopy. The patients were randomized in block sizes of two, using a randomization schedule created by the website http://www.randomization.com. After randomization, the precise day for colonoscopy was determined considering both patient preference and the endoscopy room schedule. Participating endoscopists were blinded to patient assignment before and during the procedure and while scoring bowel cleansing.
Assessment of bowel preparation quality and colonoscopy procedure
The Boston Bowel Preparation Scale (BBPS) was used to evaluate the quality of bowel cleansing (Table 1). Cleanliness was assessed for the right colon (cecum and ascending colon), mid-colon (transverse colon, hepatic and splenic flexures), and left colon (descending colon, sigmoid colon, and rectum). Each region of the colon was assigned a segment score from 0 to 3 (excellent: 3, good: 2, fair: 1, poor: 0), and these segment scores were summed to calculate a total BBPS score ranging from 0 to 9. When an endoscopic procedure failed because of inadequate preparation, any non-visualized proximal segments were scored 0. Prior to starting this study, three colonoscopists, one highly experienced staff member and two clinical fellows with experience of more than 200 colonoscopies each, conducted calibration exercises involving 20 colonoscopies. The interclass correlation coefficient k was estimated at 0.89, indicating a high level of inter-rater consistency. All colonoscopy procedures were performed by these three colonoscopists and conducted in the afternoon (started at 14:00).
Table 1.
The Boston Bowel Preparation Scale (BBPS)
| Segment score | Description |
|---|---|
| 0 | Unprepared colon segment with mucosa not seen due to solid stool that cannot be cleared |
| 1 | Portion of mucosa of the colon segment seen, but other areas of the colon segment not well seen due to staining, residual stool, and/or opaque liquid |
| 2 | Minor amount of residual staining, small fragments of stool and/or opaque liquid, but mucosa of the colon segment seen well |
| 3 | Entire mucosa of the colon segment seen well with no residual staining, small fragments of stool or opaque liquid |
Sample size calculation and statistical analysis
The sample size calculation was based on the comparison of bowel cleansing quality between two groups. A sample size of 64 patients for each group was estimated to give 80% power at a two-sided α of 0.05 for the detection of a 1.0-point difference in total BBPS score. Quantitative data were presented as means ± standard deviation and compared by Student’s two-tailed t-test. Qualitative data were presented as percentages and compared by chi-square test. Univariate and multivariate logistic regression analyses were used to determine factors associated with poor bowel preparation. P values < 0.05 were considered statistically significant. Statistical analysis was performed using MedCalc software version 16.2.1 (MedCalc Software, Mariakerke, Belgium).
RESULTS
Patient characteristics
A total of 132 patients were enrolled in this study. Two patients cancelled the procedure, and 130 patients were evaluated (Figure 1). Patients were divided into two groups: within 2 weeks (group A, n=64) or more than 2 weeks (group B, n=66) from education about bowel preparation to colonoscopy. The mean waiting time was 8.07±3.8 days in group A and 29.4±16.1 days in group B. As shown in Table 2, there were no significant differences in patient characteristics between the two groups.
Figure 1.
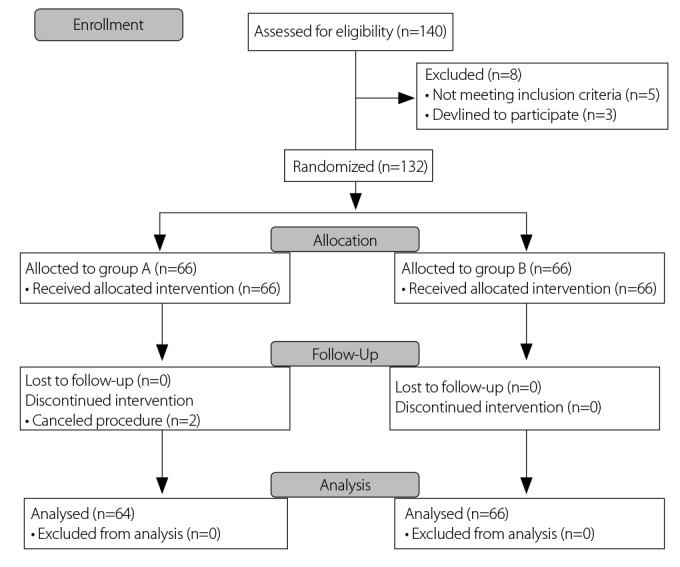
Consort flow diagram. Group A = within 2 weeks, Group B = more than two weeks
Table 2.
Patients’ baseline characteristics
| Waiting time from education to colonoscopy | |||
|---|---|---|---|
|
|
|||
| Characteristics | Within 2 weeks (N=64) | More than 2 weeks (N=66) | p |
| Waiting time (days), mean (SD) | 8.0 (3.8) | 29.4 (16.1) | <0.0001 |
| Age (years), mean (SD) | 53.6 (11.1) | 54.5 (10.2) | 0.642 |
| Sex (female), N (%) | 40 (62.5) | 38 (57.6) | 0.568 |
| Body mass index, mean (SD) | 23.7 (3.5) | 23.3 (3.5) | 0.510 |
| Experience of colonoscopy, N (%) | 48 (75.0) | 48 (72.7) | 0.769 |
| Family history of colon cancer, N (%) | 5 (7.8) | 5 (7.6) | 0.959 |
| Abdominal or pelvic surgery, N (%) | 14 (21.9) | 14 (21.2) | 0.927 |
| Past medical history, N (%) | |||
| Diabetes | 8 (12.5) | 5 (7.6) | |
| Hypertension | 13 (20.3) | 15 (22.7) | |
| Thyroid disease | 3 (4.7) | 1 (1.5) | |
| Hyperlipidemia | 1 (1.6) | 3 (4.5) | |
SD: standard deviation; N: number of patients
Primary outcome: bowel preparation quality
The efficacy of bowel cleansing according to BBPS is shown in Table 3 and Figure 2. Total BBPS scores were 8.25±0.97 in group A and 7.75±1.32 in group B (p=.017). BBPS scores were also separately assessed for the right, mid-, and left colon, and the BBPS score of the right colon was slightly but significantly higher in group A than in group B (2.71±0.45 in group A vs. 2.50±0.53 in group B; p=.013). The rate of good preparation (BBPS≥8) was higher in group A than in group B (78.1% vs. 59.1%, p=.020), while the rate of adequate preparation (BBPS≥6) did not differ significantly (100% vs. 98.5%, p=.324). The mean total BBPS scores for patients who underwent colonoscopy within 1, 2, 3, and ≥4 weeks after education were 8.31±0.99, 8.17±0.96, 7.60±1.52, and 7.86±1.16, respectively (p=.085). There was no significant dose-response relationship between waiting time and quality of bowel cleansing.
Table 3.
Efficacy of bowel cleansing according to BBPS
| Waiting time from education to colonoscopy | |||
|---|---|---|---|
|
|
|||
| Within 2 weeks (N=64) | More than 2 weeks (N=66) | p | |
| Right colon, mean (SD) | 2.71 (0.45) | 2.50 (0.53) | 0.013 |
| Mid-colon, mean (SD) | 2.79 (0.40) | 2.66 (0.50) | 0.108 |
| Left colon, mean (SD) | 2.73 (0.44) | 2.59 (0.52) | 0.096 |
| Total score, mean (SD) | 8.25 (0.97) | 7.75 (1.32) | 0.017 |
| Good bowel cleansing (BBPS≥8), N (%) | 50 (78.1) | 39 (59.1) | 0.020 |
| Adequate bowel cleansing (BBPS≥6), N (%) | 64 (100) | 65 (98.5) | 0.086 |
SD: standard deviation; N: number of patients; BBPS: Boston Bowel Preparation Scale
Figure 2.
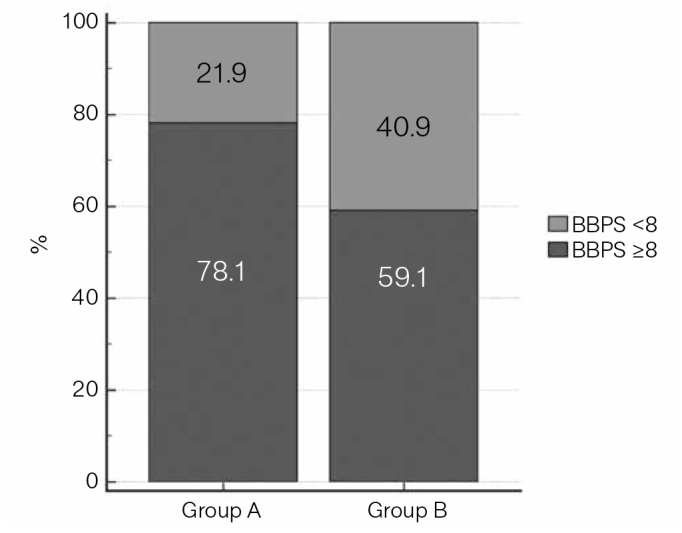
Percentage of patients with adequate preparation quality (p=.020). Group A = within two weeks, Group B = more than two weeks. Good preparation (prep.) is defined as a total BBPS score of ≥8
Secondary outcomes: colonoscopic data
The polyp and adenoma detection rates according to BBPS are shown in Table 4. Both were slightly higher in group A than in group B (polyp detection rate, 42.2% vs. 38.5%, p=.667; adenoma detection rate, 31.2% vs. 22.7%, p=.275). A numerical trend was observed for slightly superior polyp and adenoma detection in group A, but it was not statistically significant. Additionally, cecal intubation rate, cecal intubation time, and colonoscopy withdrawal time did not significantly differ between the two groups.
Table 4.
Secondary outcomes
| Waiting time from education to colonoscopy | |||
|---|---|---|---|
|
|
|||
| Within 2 weeks (N=64) | More than 2 weeks (N=66) | p | |
| Cecal intubation time (min), mean (SD) | 8.33 (3.91) | 8.90 (4.80) | 0.460 |
| Withdrawal time (min), mean (SD) | 11.61 (5.05) | 11.85 (5.88) | 0.817 |
| Cecal intubation rate, N (%) | 64 (100) | 65 (98.5) | 0.086 |
| Adenoma detection rate, N (%) | |||
| Any polyp | 27 (42.2) | 25 (38.5) | 0.667 |
| Multiple polyps (≥3) | 11 (17.2) | 5 (7.6) | 0.096 |
| Any adenoma | 20 (31.2) | 15 (22.7) | 0.275 |
| Multiple adenomas (≥3) | 5 (7.8) | 3 (4.5) | 0.440 |
Min: minute; SD: standard deviation; N: number of patients
DISCUSSION
Adequate bowel cleansing is essential for the diagnostic accuracy and safety of colonoscopy (1–3). The quality of bowel cleansing is affected by many factors including age; failure to follow preparation instructions; inpatient status; choice of bowel-cleansing agents; comorbidities such as diabetes, stroke, and cirrhosis; and abdominopelvic surgery (5–9). Among them, the failure to follow preparation instructions is a modifiable factor related to inadequate bowel cleansing. This factor can be affected by waiting times to colonoscopy because details of the preparation instructions can be forgotten as time passes.
This study demonstrated that short waiting times from education to colonoscopy can improve the quality of bowel preparation. The total BBPS score was 8.25±0.97 in group A and 7.75±1.32 in group B (p=.017). However, the difference between the means of the two groups was only 0.5, and the total BBPS scores of both groups were over 6. The rate of good preparation (BBPS≥8) was also higher in group A than in group B (78.1% vs. 59.1%, p=.002). However, the rate of adequate preparation (BBPS≥6) did not differ significantly (100% vs. 98.5%, p=.324). In other studies (12,13), a total BBPS score≥6 and/or all segment scores ≥2 have been considered a standardized definition of adequate bowel preparation, and higher BBPS scores (≥5 vs. <5) were associated with higher polyp detection rates. The United States Multi-Society Task Force on Colorectal Cancer (USMSTF-CRC) proposed “adequate” to be the ability to detect polyps >5 mm in size, and a score of 6 is generally considered the cut-off value for adequate bowel cleansing (13). Although our study revealed a higher total BBPS score in group A than in group B, there was no significant difference in the polyp or adenoma detection rates between the two groups, possibly because the total BBPS scores of both groups were higher than 6 and the rates of BBPS≥6 did not differ. This result may also be attributable to the study design, which primarily assessed total BBPS scores, and hence, further large-scale studies are needed to clarify this issue.
A segment score of 3 may be a more helpful indicator of effective and safe colonoscopy than a score of 2. Consistent with the high total BBPS score in this study, most segment scores were 2 or 3. In a recent prospective study (14), the rate of missed adenoma (≥5 mm) was non-inferior for segments with a BBPS score of 2 compared to those with a score of 3. However, the rate of missed adenoma (≤5 mm) in segments with BBPS scores of 2 and 3 has not been studied in detail. Another study (15) reported that higher BBPS scores (≥8 vs. <8) were associated with a higher polyp detection rate (44.9% vs. 33.0%, p=.042). Thus, higher BBPS scores are indicative of a more effective colonoscopy with regard to the likelihood of a prolonged procedure time due to liquid fluid suction, greater difficulty for the colonoscopist, and patient discomfort.
The mean total BBPS score in this study was slightly higher than those reported in several previous studies (16,17). In South Korea, colonoscopy is widely accessible because of health insurance coverage and patient awareness of colonoscopy screening. Therefore, the interval between colonoscopies is generally shorter than in other countries, and people typically undergo more colonoscopy procedures. Because of their greater experience with colonoscopy and education about bowel preparation, patients in South Korea may be more aware of the importance of bowel preparation. This difference could underlie the high quality of bowel cleansing observed in South Korea and in this study.
In this study, total BBPS scores for patients who underwent colonoscopy within 1, 2, 3, and ≥4 weeks after education were 8.31±0.99, 8.17±0.96, 7.60±1.52, and 7.86±1.16, respectively (p=.085). There was no significant dose-response relationship between waiting time and the quality of bowel cleansing. However, a numerical trend was observed for declining BBPS scores from week 1 to week 3, and the total BBPS score and the rate of good preparation were significantly higher in patients who had a colonoscopy within 2 weeks from education. Bowel preparation instructions are often provided in the outpatient clinic when patients make an appointment for colonoscopy, and sometimes 1 or 2 months pass before the scheduled colonoscopy is performed. Preparation instructions include many components such as the type of diet, dietary restrictions, and timing and method of administering bowel cleansing agents, and having a clear understanding of the process and adherence to instructions are important. However, patients may forget important components of the bowel cleansing process, which may result in inadequate bowel cleansing, especially after an extended waiting time to colonoscopy. Thus, the present study suggests that shorter waiting times from education to colonoscopy can improve the quality of bowel preparation.
The availability of sufficient staff and equipment for endoscopy screening is one factor that can reduce waiting times to colonoscopy. However, health insurance systems, costs of colonoscopy, and resources such as staff and equipment vary across countries. Therefore, if waiting times to colonoscopy can not be reduced, more contact such as via telephone, e-mail, and short message service (SMS) may be useful to remind patients about the bowel preparation process. Liu et al. (18) reported that telephone-based re-education the day before colonoscopy improved the quality of bowel preparation and the polyp detection rate. Several previous studies found that telephone and SMS reminders were associated with an improvement in outpatient attendance (19–23). Therefore, in patients with prolonged waiting times to colonoscopy, reminders may also be helpful for improving the quality of bowel preparation.
Our study has several limitations. First, it did not assess patients’ socioeconomic status or education level, which are also potential factors affecting the quality of bowel preparation (10,11,24). Second, since we evaluated bowel preparation for afternoon colonoscopy, these results may not apply to morning colonoscopy. Third, this study was conducted in a single tertiary center, and, therefore, the participants do not represent the general population. The results of this study need further confirmation through large-scale randomized trials.
In conclusion, this study demonstrated that short waiting times from education to colonoscopy could improve the quality of bowel preparation. While most endoscopy units try to shorten the waiting time to colonoscopy, the demand for colonoscopy is increasing because of increased colorectal cancer screening. Ensuring sufficient staff and equipment for endoscopy in order to reduce waiting times and increasing contacts by telephone, e-mail, and SMS to reinforce bowel preparation education when waiting times cannot be changed may be useful approaches for improving bowel preparation outcomes.
Footnotes
“See Editorial 4–6”
Ethics Committee Approval: Ethics committee approval was received for this study from the Institutional Review Board of Haeundae Paik Hospital (Decision Date: 21.12.2016/Decision No: 2016-11-007-002).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - T.O.K.; Design - J.L., T.O.K.; Supervision - T.O.K.; Resource - J.H.C.; Materials - J.H.P., S.Y.Y.; Data Collection and/or Processing - J.L., J.W.S.; Analysis and/or Interpretation - J.L., S.H.P., J.H.C.; Literature Search - J.L., J.W.S.; Writing - J.L., J.W.S.; Critical Reviews - T.O.K., Y.S.M.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2014;109:1528–45. doi: 10.1038/ajg.2014.272. https://doi.org/10.1038/ajg.2014.272 [DOI] [PubMed] [Google Scholar]
- 2.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162–8. doi: 10.1056/NEJM200007203430301. https://doi.org/10.1056/NEJM200007203430301 [DOI] [PubMed] [Google Scholar]
- 3.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–81. doi: 10.1056/NEJM199312303292701. https://doi.org/10.1056/NEJM199312303292701 [DOI] [PubMed] [Google Scholar]
- 4.Chokshi RV, Hovis CE, Hollander T, Early DS, Wang JS. Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest Endosc. 2012;75:1197–203. doi: 10.1016/j.gie.2012.01.005. https://doi.org/10.1016/j.gie.2012.01.005 [DOI] [PubMed] [Google Scholar]
- 5.Romero RV, Mahadeva S. Factors influencing quality of bowel preparation for colonoscopy. World J Gastrointest Endosc. 2013;5:39–46. doi: 10.4253/wjge.v5.i2.39. https://doi.org/10.4253/wjge.v5.i2.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2014;80:543–62. doi: 10.1016/j.gie.2014.08.002. https://doi.org/10.1016/j.gie.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 7.Park HJ, Chae MH, Kim HS, et al. Colon transit time may predict inadequate bowel preparation in patients with chronic constipation. Intest Res. 2015;13:339. doi: 10.5217/ir.2015.13.4.339. https://doi.org/10.5217/ir.2015.13.4.339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ness RM, Manam R, Hoen H, Chalasani N. Predictors of inadequate bowel preparation for colonoscopy. Am J Gastroenterol. 2001;96:1797–802. doi: 10.1111/j.1572-0241.2001.03874.x. https://doi.org/10.1111/j.1572-0241.2001.03874.x [DOI] [PubMed] [Google Scholar]
- 9.Yoon JH, Park D, Il, Shin JE, et al. Comparison of bowel preparation depending on completion time of polyethylene glycol ingestion and start time of colonoscopy. Intest Res. 2010;8:24–9. https://doi.org/10.5217/ir.2010.8.1.24 [Google Scholar]
- 10.Chan W, Saravanan A, Manikam J, Goh K, Mahadeva S. Appointment waiting times and education level influence the quality of bowel preparation in adult patients undergoing colonoscopy. BMC Gastroenterol. 2011;11:86. doi: 10.1186/1471-230X-11-86. https://doi.org/10.1186/1471-230X-11-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen DL, Wieland M. Risk factors predictive of poor quality preparation during average risk colonoscopy screening: the importance of health literacy. J Gastrointest Liver Dis. 2010;19:369–72. [PubMed] [Google Scholar]
- 12.Calderwood AH, Schroy PC, Lieberman DA, Logan JR, Zurfluh M, Jacobson BC. Boston Bowel Preparation Scale scores provide a standardized definition of adequate for describing bowel cleanliness. Gastrointest Endosc. 2014;80:269–76. doi: 10.1016/j.gie.2014.01.031. https://doi.org/10.1016/j.gie.2014.01.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lieberman D, Nadel M, Smith RA, et al. Standardized colonoscopy reporting and data system: report of the Quality Assurance Task Group of the National Colorectal Cancer Roundtable. Gastrointest Endosc. 2007;65:757–66. doi: 10.1016/j.gie.2006.12.055. https://doi.org/10.1016/j.gie.2006.12.055 [DOI] [PubMed] [Google Scholar]
- 14.Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150:396–405. doi: 10.1053/j.gastro.2015.09.041. https://doi.org/10.1053/j.gastro.2015.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim EJ, Park YI, Kim YS, et al. A Korean experience of the use of Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Saudi J Gastroenterol. 2014;20:219–24. doi: 10.4103/1319-3767.136950. https://doi.org/10.4103/1319-3767.136950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Samarasena JB, Muthusamy VR, Jamal MM. Split-dosed Mira-LAX/Gatorade is an effective, safe, and tolerable option for bowel preparation in low-risk patients: a randomized controlled study. Am J Gastroenterol. 2012;107:1036–42. doi: 10.1038/ajg.2012.115. https://doi.org/10.1038/ajg.2012.115 [DOI] [PubMed] [Google Scholar]
- 17.Calderwood AH, Lai EJ, Fix OK, Jacobson BC. An endoscopist- blinded, randomized, controlled trial of a simple visual aid to improve bowel preparation for screening colonoscopy. Gastrointest Endosc. 2011;73:307–14. doi: 10.1016/j.gie.2010.10.013. https://doi.org/10.1016/j.gie.2010.10.013 [DOI] [PubMed] [Google Scholar]
- 18.Liu X, Luo H, Zhang L, et al. Telephone-based re-education on the day before colonoscopy improves the quality of bowel preparation and the polyp detection rate: a prospective, colonoscopist-blinded, randomised, controlled study. Gut. 2014;63:125–30. doi: 10.1136/gutjnl-2012-304292. https://doi.org/10.1136/gutjnl-2012-304292 [DOI] [PubMed] [Google Scholar]
- 19.Geraghty M, Glynn F, Amin M, Kinsella J. Patient mobile telephone ‘text’ reminder: a novel way to reduce non-attendance at the ENT out-patient clinic. J Laryngol Otol. 2008;122:296–8. doi: 10.1017/S0022215107007906. https://doi.org/10.1017/S0022215107007906 [DOI] [PubMed] [Google Scholar]
- 20.Downer SR, Meara JG, Da Costa AC. Use of SMS text messaging to improve outpatient attendance. Med J Aust. 2005;183:366–8. doi: 10.5694/j.1326-5377.2005.tb07085.x. [DOI] [PubMed] [Google Scholar]
- 21.Koshy E, Car J, Majeed A. Effectiveness of mobile-phone short message service (SMS) reminders for ophthalmology outpatient appointments: observational study. BMC Ophthalmol. 2008;8:9. doi: 10.1186/1471-2415-8-9. https://doi.org/10.1186/1471-2415-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare. 2011;17:358–64. doi: 10.1258/jtt.2011.110707. https://doi.org/10.1258/jtt.2011.110707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park J, Kim TO, Lee NY, et al. The effectiveness of short message service to assure the preparation-to-colonoscopy interval before bowel preparation for colonoscopy. Gastroenterol Res Pract. 2015;2015:628049. doi: 10.1155/2015/628049. https://doi.org/10.1155/2015/628049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenfeld G, Krygier D, Enns RA, Singham J, Wiesinger H, Bressler B. The impact of patient education on the quality of inpatient bowel preparation for colonoscopy. Can J Gastroenterol. 2010;24:543–6. doi: 10.1155/2010/718628. https://doi.org/10.1155/2010/718628 [DOI] [PMC free article] [PubMed] [Google Scholar]


