Abstract
Couples HIV testing and counseling (couple counseling) promotes safer sexual behaviors, increases communication between couples, and decreases HIV transmission. However, the impact of couple counseling on social support, critical for persons living with HIV, has not been examined. Ninety couples with a recently tested HIV-positive pregnant woman (female-positive couples) and 47 couples with a recently tested HIV-negative pregnant woman (female-negative couples) were enrolled in an observational study at an antenatal clinic in Malawi. Each couple member was assessed immediately before and one month after couple counseling for partner, family, and peer social support using the Multidimensional Scale of Perceived Social Support. Before couple counseling, social support was lower among women than men in both female-positive couples (β=−10.00, p <0.01) and female-negative couples (β=−8.43, p<0.01). After couple counseling, social support increased for women in female-positive couples (β=4.01, p<0.01) and female-negative couples (β=4.69, p <0.01) but not for men in either type of couple. couple counseling could be an effective strategy to increase social support for women, including those with recent HIV diagnoses.
Keywords: HIV, pregnancy, couples, social support, counseling
Introduction
Couples HIV testing and counseling (couple counseling) is an opportunity for a couple to learn their HIV status together. Following mutual testing and disclosure, couples have a chance to discuss prevention and treatment options with a counselor(Guidance on Couples HIV Testing and Counselling Including Antiretroviral Therapy for Treatment and Prevention in Serodiscordant Couples: Recommendations for a Public Health Approach, 2012). In Sub-Saharan Africa, couple counseling has been associated with increased communication between couple members, sexual behavior change, and decreased HIV transmission (E. L. Cohen, Scott, White, & Dignan, 2013; Kennedy, Medley, Sweat, & O’Reilly, 2010; Plazy et al., 2013; Rosenberg et al., 2013; van der Straten, King, Grinstead, Serufilira, & Allen, 1995). In 2012, the World Health Organization (WHO) recommended offering couple counseling wherever HIV testing and counseling is available, particularly for HIV-discordant couples and in antenatal settings(Guidance on Couples HIV Testing and Counselling Including Antiretroviral Therapy for Treatment and Prevention in Serodiscordant Couples: Recommendations for a Public Health Approach, 2012).
Despite the WHO’s recommendation, couple counseling is not widespread, and the vast majority of HIV tests are delivered to individuals (Government of Malawi Ministry of Health, 2016, World Health Organization, 2015). This low volume of couple counseling is in part due to concerns about bringing intimate partners together for mutual disclosure and the impact this will have on the relationship itself (Colombini, James, Ndwiga, Integra team, & Mayhew, 2016; Flax et al., 2017; Gielen et al., 2000; Maman, van Rooyen, & Groves, 2014; Obermeyer, Baijal, & Pegurri, 2011), including withdrawal of social support. Social support is the provision of emotional, instrumental, or informational assistance from members of an individual’s social network, such as partners, peers, or family(S. Cohen, 2004). Examining the impact of couple counseling on the relationship, including social support, can offer insight into whether these concerns are warranted.
In this analysis, we assess whether social support differs between female and male couple members in couples with an HIV-infected woman (female-positive couples) and HIV-uninfected woman (female-negative couples). We then assess whether engaging in couple counseling is associated with changes in social support among each couple member and the couple overall. Finally, we examine how these differences and changes are distributed across sources of social support (partners, peers, and family).
Methods
Study Design, Participants, and Procedures
The study was conducted from December 2015 to December 2016 at the antenatal clinic (ANC) at Bwaila District Hospital, a high-volume urban maternity hospital in Lilongwe, Malawi. In 2011, Malawi adopted Option B+, a test-and-treat approach to the prevention of mother to child transmission (PMTCT) of HIV. Under Option B+, women routinely test for HIV during pregnancy, and those who test HIV-positive are eligible to start immediate lifelong antiretroviral therapy (ART). Pregnant women who present to ANC alone are tested and counseled individually and those who present with a partner are offered couple counseling.
The couple counseling process included couple pre-test counseling, simultaneous testing, joint return of test results, and couple post-test counseling. In our study, the female partner had already been tested within the last month. Couple counseling was provided by a trained counselor, and counseling messages were tailored to the couples’ HIV status. Couple counseling counselors aimed to ease tension, diffuse blame, and create a safe environment where couples could talk through difficult HIV-related issues. Couples were urged to focus on the positive aspects of their relationship and focus on the future, rather than the past (Guidance on Couples HIV Testing and Counselling Including Antiretroviral Therapy for Treatment and Prevention in Serodiscordant Couples: Recommendations for a Public Health Approach, 2012).
All women newly diagnosed as HIV-positive during their initial ANC visit were approached and screened for eligibility. HIV-uninfected pregnant women were selected from ANC using frequency matching based on age categories of HIV-infected enrolled women (18-19, 20-24, 25-29, 30-34, and 35-39 years) and also approached and screened for eligibility. Among HIV-positive women, 318 were screened and 202 were eligible (64%). Among HIV-positive women, 98 were screened and 92 were eligible (94%). Eligible women provided informed consent. Additional details on recruitment, eligibility, and enrollment have been reported elsewhere (Rosenberg et al., 2017, 2018).
Each woman was provided with an invitation for her male sexual partner. Data were only collected from women who presented as couples. Couples had two visits: on the first day, they presented together and one month later. During the first visit, the two partners participated in separate interviewer-administered questionnaires about demographics, relationship characteristics, social support, and HIV related behaviors. Afterwards, couples received couple counseling. At the second visit, each participant completed a second, similar interviewer-administered questionnaire. Participants who returned without their partners at the second visit were still interviewed (N = 5).
Measures
Social support was measured using the Multidimensional Scale of Perceived Social Support (MSPSS). The MSPSS is a 12-item instrument that evaluates perceptions of social support across three subscales: partner, family, and friends (Zimet, Dahlem, Zimet, & Farley, 1988). The scale’s psychometric properties have been previously validated within an antenatal population in Malawi (Stewart, Umar, Tomenson, & Creed, 2014). Participants were asked how much they agreed or disagreed with each scale item with the five possible responses ranging from “strongly disagree,” to “strongly agree.” Each response was given a score from one to five and then summed (Zimet et al., 1988). The total possible score is 60 points overall with each subscale accounting for 20 points. For analysis, overall support was categorized into three levels: low (<40), medium (40-50), and high (>50) (Knowlden, Hackman, & Sharma, 2016; Kronish, Edmondson, Li, & Cohen, 2012). We also categorized couples by the woman’s HIV status—either “female-positive couples” or “female-negative couples.”
Statistical Methods
First, we compared frequencies of baseline demographic characteristics by couple type and gender using Pearson’s chi-squared tests. When cell counts were <5, we used Fisher’s exact tests. Next, we examined levels of social support (low, medium, high) by couple type and gender. To estimate changes in social support following couple counseling, we conducted analyses at the individual and couple levels.
Individual-level analysis included one record per individual. We estimated the change in average social support before and after couple counseling using generalized estimating equations to account for correlation between the same individual at two time points with an identity link, exchangeable correlation matrix, and robust variance. We estimated changes separately for women and men in female-positive and female-negative couples. Pre- and post-couple counseling individual mean scores and corresponding p-values were also calculated for overall social support, partner support, peer support, and family support across female-positive and female-negative couples.
Couple-level analysis included one record per couple. We first calculated the difference in social support scores between male and female couple members at each time point and then estimated the change in these differences before and after couple counseling. Changes were estimated separately for female-positive and female-negative couples. To account for correlation between the same couple at two time points, generalized estimating equations with an identity link, exchangeable correlation matrix, and robust variance were again used to estimate mean score changes and corresponding p-values. In addition to looking at differences in social support between couples, we looked at means between male and female couple members. Pre- and post-couple counseling differences in overall social support, partner support, peer support, and family support were calculated.
Both unadjusted and adjusted models were run for each set of analyses and included age to account for frequency matching, a design effect. Additional covariates included age category, children with study partner, male HIV status, marital status, and education level. All analyses were performed using Stata version 14 (College Station, Texas, USA).
Ethics
The study received approval from both the National Health Science Research Committee in Malawi and the University of North Carolina at Chapel Hill Institutional Review Board. All participants provided informed consent.
Results
Population
A total of 137 couples were enrolled in the study: 90 female-positive and 47 female-negative couples. The recruitment to participation cascade has been detailed elsewhere (Rosenberg et al., 2017). The mean age for HIV-infected and HIV-uninfected was 26 years for women and 32 years for men. Nearly all women were married (99%) and believed their study partner was responsible for the pregnancy (98%). Most women enrolled during their second trimester (73%) and had previously given birth (77%). Most women (72%) had been tested for HIV previously, but few (9%) had received a prior HIV-positive result. Most men (69%) had also been tested for HIV previously, but 13 (14%) had received a prior HIV-positive result (Table I).
Table I.
Baseline Characteristics
| HIV + Females (N=90) | HIV − Females (N=47) | Chi-Square | F+ Males (N=90) | F− Males (N=46)* | Chi-Square | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | p-value | N | (%) | N | (%) | p-value | |
| HIV Status | ||||||||||
| HIV Positive | 90 | (100.0) | 0 | (0.0) | 67 | (74.4) | 2 | (4.4) | ||
| HIV Negative | 0 | (0.0) | 47 | (100.0) | 22 | (24.4) | 43 | (93.5) | ||
| Unknown | 0 | (0.0) | 0 | (0.0) | < 0.01 | 1 | (1.1) | 1 | (2.2) | < 0.01 |
| Age | ||||||||||
| 18-19 | 4 | (4.4) | 2 | (4.3) | 0 | (0.0) | 0 | (0.0) | ||
| 20-24 | 36 | (40.0) | 19 | (40.4) | 13 | (14.4) | 7 | (15.2) | ||
| 25-29 | 26 | (28.9) | 14 | (29.8) | 22 | (24.4) | 14 | (30.4) | ||
| 30-34 | 20 | (22.2) | 9 | (19.2) | 25 | (27.8) | 9 | (19.6) | ||
| 35-40 | 4 | (4.4) | 3 | (6.4) | 0.98 | 30 | (33.3) | 16 | (34.8) | 0.75 |
| Education | ||||||||||
| Less than secondary | 75 | (83.3) | 37 | (78.7) | 63 | (70.0) | 18 | (39.1) | ||
| Secondary or greater | 15 | (16.7) | 10 | (21.3) | 0.50 | 27 | (30.0) | 28 | (60.9) | < 0.01 |
| Employment | ||||||||||
| Not employed | 76 | (84.4) | 34 | (72.3) | 3 | (3.3) | 1 | (2.2) | ||
| Self-employed | 7 | (7.8) | 6 | (12.8) | 43 | (47.8) | 24 | (52.2) | ||
| Employed | 7 | (7.8) | 7 | (14.9) | 0.22 | 44 | (48.9) | 21 | (45.7) | 0.89 |
| HTC History | ||||||||||
| Never tested | 25 | (27.8) | 14 | (29.8) | 22 | (26.2) | 12 | (26.1) | ||
| Previously negative | 59 | (65.6) | 33 | (70.2) | 51 | (60.7) | 32 | (69.6) | ||
| Previously positive | 6 | (6.7) | 0 | (0.0) | 0.24 | 11 | (13.1) | 32 | (4.4) | 0.30 |
| Unknown or missing | 0 | 0 | 6 | 0 | ||||||
| Trimester | ||||||||||
| 1st trimester | 5 | (5.6) | 2 | (4.3) | ||||||
| 2nd trimester | 69 | (76.7) | 38 | (80.9) | ||||||
| 3rd trimester | 16 | (17.8) | 7 | (14.9) | 0.94 | |||||
| Primiparous | ||||||||||
| No | 15 | (16.7) | 9 | (19.2) | ||||||
| Yes | 75 | (83.3) | 38 | (80.9) | 0.81 | |||||
One record was lost during the uploading process.
When cell counts were less than five, Fisher’s exact tests were used.
Social Support before Couple Counseling
Before couple counseling, 24% of women reported low levels of social support, 51% reported medium levels of social support, and 25% reported high levels of social support. A larger proportion of women in female-positive couples (30%) reported low levels of social support than women in female-negative couples (13%) (Figure I). Women in female-positive couples also reported lower overall social support mean scores than women in female-negative couples (43.0 versus 46.9, p < 0.01) (Table II).
Figure I.
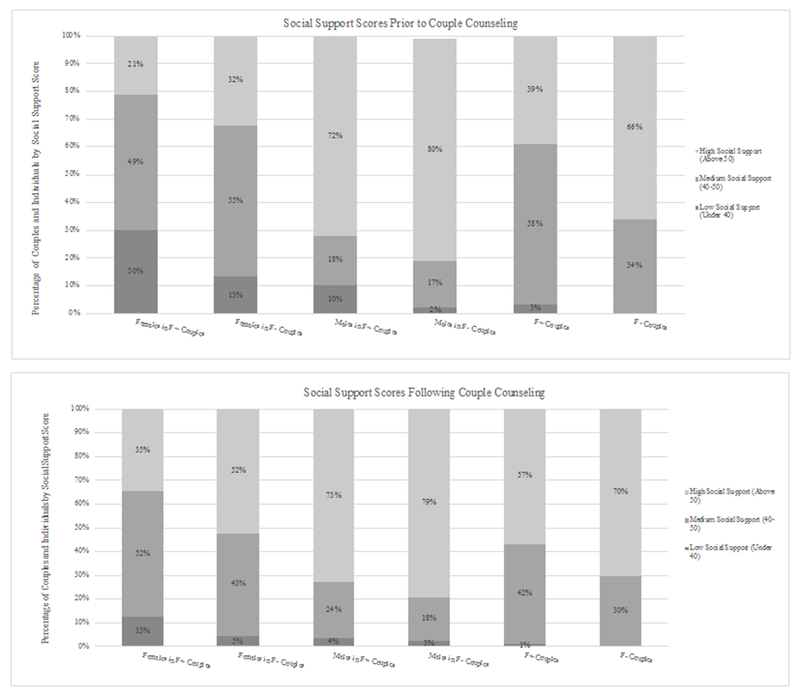
Social support scores before and after couples counseling.
Table II.
Individual and Couple Differences in Social Support by Gender and HIV Status Before & After Couple HIV Testing and Counseling (CC)
| Female + Couples | Female − Couples | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean Score (SE) | Change in Mean Score (P-Value) | Mean Score (SE) | Change in Mean Score (P-Value) | |||||
| Pre-CC | Post-CC | Unadjusted* | Adjusted** | Pre-CC | Post-CC | Unadjusted* | Adjusted** | |
| Women | ||||||||
| Partner Support | 14.3 (0.3) | 15.5 (0.3) | 1.2 (< 0.01) | 1.2 (< 0.01) | 15.5 (0.4) | 17.1 (0.4) | 1.6 (< 0.01) | 1.6 (< 0.01) |
| Peer Support | 14.2 (0.3) | 15.9 (0.4) | 1.7 (< 0.01) | 1.8 (< 0.01) | 15.5 (0.4) | 17.1 (0.4) | 1.6 (0.01) | 1.6 (0.01) |
| Family Support | 14.5 (0.3) | 15.6 (0.3) | 1.0 (< 0.01) | 1.0 (< 0.01) | 15.8 (0.4) | 17.4 (0.4) | 1.5 (< 0.01) | 1.5 (< 0.01) |
| Overall Support | 43.0 (0.9) | 47.1 (0.9) | 4.0 (< 0.01) | 4.0 (< 0.01) | 46.9 (1.0) | 51.5 (1.1) | 4.7 (< 0.01) | 4.7 (< 0.01) |
| Men | ||||||||
| Partner Support | 16.9 (0.4) | 17.0 (0.4) | 0.1 (0.71) | 0.2 (0.58) | 18.3 (0.4) | 17.9 (0.4) | −0.4 (0.35) | −0.4 (0.36) |
| Peer Support | 18.1 (0.3) | 18.4 (0.3) | 0.3 (0.28) | 0.4 (0.21) | 18.8 (0.3) | 19.0 (0.3) | 0.1 (0.74) | 0.1 (0.82) |
| Family Support | 18.0 (0.3) | 17.9 (0.3) | −0.2 (0.64) | 0.0 (0.91) | 18.3 (0.4) | 18.2 (0.4) | 0.0 (0.92) | 0.0 (0.94) |
| Overall Support | 53.0 (0.8) | 53.3 (0.8) | 0.3 (0.58) | 0.4 (0.52) | 55.4 (0.9) | 55.1 (1.0) | −0.3 (0.76) | −0.4 (0.75) |
| Couples Differences | ||||||||
| Partner Support | −2.6 (0.5) | −1.5 (0.5) | 1.14 (0.02) | 1.1 (0.02) | −2.8 (0.5) | −1.0 (0.5) | 1.8 (< 0.01) | 1.9 (< 0.01) |
| Peer Support | −3.9 (0.5) | −2.4 (0.5) | 1.49 (< 0.01) | 1.5 (< 0.01) | −3.3 (0.5) | 1.8 (0.5) | 1.4 (0.03) | 1.5 (0.02) |
| Family Support | −3.5 (0.5) | −2.3 (0.5) | 1.24 (0.01) | 1.2 (0.01) | −2.5 (0.6) | −0.9 (0.6) | 1.5 (< 0.01) | 1.6 (< 0.01) |
| Overall Support | −10 (1.3) | −6.1 (1.3) | 3.9 (< 0.01) | 3.9 (< 0.01) | −8.5 (1.4) | −3.7 (1.4) | 4.8 (< 0.01) | 4.9 (< 0.01) |
Adjusted for age category
Adjusted for age category, male HIV status, marriage, education, and child with study partner
Before couple counseling, 7% of men reported low levels of social support, 18% reported medium levels of social support, and 75% reported high levels of social support. These levels did not differ for men in female-negative or female-positive couples (Fisher’s Exact = 0.27). Men in female-positive couples reported slightly lower overall social support mean scores than men in female negative couples (53.0 versus 55.4, p = 0.07).
At the couple level, 2% of the couples reported low levels of social support, 50% reported medium levels of social support, and 48% reported high levels of social support before couple counseling. Female-positive couples reported a larger mean difference in social support than female-negative couples (−10 versus −8.5, p = 0.04).
Social Support after Couple Counseling
Following couple counseling, 10% of women reported low levels, 49% reported medium levels, and 41% report high levels of social support, a trend towards higher social support. Adjusted mean scores increased by 4.0 points in female-positive couples and 4.7 points in female negative couples. These increases were driven by 1-2 point increases in social support across different sources.
Following couple counseling, 3% of men reported low levels, 22% reported medium levels, and 75% report high levels of social support. No substantial changes in overall social support were observed for men following couple counseling, regardless of whether they were in a female-positive or female-negative couples. Examining changes by men’s HIV status, instead of by their female partner’s HIV status, yielded similar results: there were no significant increases in overall social support for HIV-positive men (Adjusted Change in Mean Score = 0.5, p=0.69) or HIV negative men (Adjusted Change in Mean Score = 0.26, p=0.82). Across sources of social support, men in female-positive couples and men in female-negative couples reported a 1-2-point increase or decrease in social support.
Following couple counseling, at the couple level, 1% of the couples reported low levels, 38% reported medium levels, and 61% reported high levels of social support. Both female-positive couples (Adjusted Change in Mean Score Difference = 3.9, p-value < 0.01) and female-negative couples (Adjusted Change in Mean Score Difference = 5.2, p-value < 0.01) reported significant decreases in the differences in overall social support between men and women. This change in differences was driven by increases in female social support rather than decreases in male social support. Across sources of social support, female-positive couples and female negative couples reported similar decreases in the male-female difference for peers, partners, and friends.
Discussion
We conducted an observational study to measure changes in social support before and after CTHC, and how this differed by gender and female HIV status. Social support was lower among women than men both before and after couple counseling. However, the gap in social support between couple members narrowed following couple counseling. This narrowing was driven by increased social support for women, and stable social support scores for men. This trend was observed in both female-positive couples and female-negative couples and was a result of increases in support from a combination of peers, partners, and family members.
Women, regardless of their HIV statuses or their partners’ HIV statuses, experienced increases in social support one month after couple counseling. This finding has important implications for HIV-positive women, who disproportionately bear the burden of disclosure within couples(Anglewicz & Chintsanya, 2011; Hampanda & Rael, 2018; Kalichman, DiMarco, Austin, Luke, & DiFonzo, 2003; Medley, Garcia-Moreno, McGill, & Maman, 2004; Vu et al., 2012). They may be hesitant to disclose due to fears of violence, abandonment, and divorce(Colombini et al., 2016; Gielen et al., 2000; Maman et al., 2014; Obermeyer et al., 2011). Despite these concerns, few social harms have been reported in such situations, (Rosenberg et al., 2015, 2017) and our findings demonstrate that couple counseling may, on average, lead to increased social support, a psychosocial benefit.
The opportunity to enhance social support during the antenatal period is particularly important for HIV-positive pregnant women. In addition to the physical, psychological, and economic demands of pregnancy and preparing for birth, HIV-positive women face the risk of HIV transmission to their infants. In sub-Saharan Africa, social support from one’s partner is associated with increased adherence to PMTCT programs and decreased levels of emotional distress (Antelman et al., 2007; Mepham, Zondi, Mbuyazi, Mkhwanazi, & Newell, 2011; Nassali et al., 2009; Peltzer, Sikwane, & Majaja, 2011; Serovich, Kimberly, Mosack, & Lewis, 2001). Thus, interventions such as couple counseling that increase social support have the potential to help HIV-positive women cope with the burden of HIV infection as they navigate pregnancy, childbirth, and lifelong treatment, and could ultimately have an impact on maternal and child health outcomes.
Social support for men remained relatively high and constant before and after CTHC. Among other couples-based studies in Sub-Saharan Africa, men, compared to women, were more likely to evaluate relationship characteristics in a positive light (Conroy et al., 2016; Cox, Hindin, Otupiri, & Larsen-Reindorf, 2013). It may be that men are more prone to socially desirable responses (Conroy et al., 2016) or that men with low perceptions of social support were less likely to participate in our study. A third possible explanation may relate to the order in which partners learned their HIV statuses. All women in our study knew their HIV status prior to couple counseling. Specifically, they received their test results during ANC and then again when they returned with their partner. Most men, however, learned their status during couple counseling. This variability between events could affect the amount of time men and women had to process and accept their HIV status for themselves, disclose their status to their social network, and experience changes in social support from partners, friends, and family.
We found partner-specific social support to be a modifiable relationship dynamic among couples. Lewis’ interdependence model and Karney’s dyadic framework both suggest that positive relationship dynamics have the potential to help couples coordinate and engage in HIV risk-reduction behaviors (Karney et al., 2010; Lewis et al., 2006). The association between relationship dynamics and HIV risk-reduction behaviors has been observed among men who have sex with men, with higher perceptions of HIV-specific social support from partners being associated with less extra-partnership sexual activity (Darbes, Chakravarty, Beougher, Neilands, & Hoff, 2012). Perceptions of support from one’s intimate partner might indicate the presence of communication about HIV-related topics and a higher concordance in agreement about safe sexual behaviors (Darbes, Chakravarty, Neilands, Beougher, & Hoff, 2014). We previously examined the impact of couple counseling on relationship dynamics and consistent condom use using these data and found substantial increases in trust, HIV communication, and relationship power after couple counseling. However, no significant associations between these three relationship factors pre-couple counseling and safe sex post-couple counseling were found (Rosenberg et al., 2017). Given couple counseling’s potential to modify perceptions of social support, we believe that an important next step is to understand the relationship between this psychosocial outcome and sexual behaviors in HIV-affected heterosexual couples.
As couple counseling is an intervention for couples, we hypothesized that partner social support would increase but unexpectedly substantial positive changes in peer and family social support were also observed. It is possible that partner disclosure during couple counseling might function as a gateway for women to discuss their HIV statuses with others in their social networks, which in turn enhances the support they receive from them (Kalichman et al., 2003; Maman et al., 2014; Ssali et al., 2010). Alternatively, the act of HIV testing and counseling, irrespective of the couple component, might embolden women to discuss their status with individuals beyond their intimate partner. The pathways through which couple counseling increase social support from friends and family members is an important area for future research.
Given the non-randomized, observational nature of this study, we cannot eliminate the possibility of secular trends or processes outside of couple counseling influencing our results. For example, disclosure of HIV status or engagement in HIV care have the potential to impact how women and men perceive support and assistance from those around them. However, we believe that the prospective assessment of the same women and men before and after couple counseling still suggests that the intervention had a substantial impact on perceptions of social support.
Existing differences in relationship dynamics and individual characteristics also could have influenced the type of couples who did or did not present for the study. Partners who agreed to be part of the study may have had different backgrounds than those who did not present. Similarly, the quality of the couple’s relationships may have independently led to increases in social support rather than couple counseling itself. Our analysis attempted to adjust for these possible differences by including a number of potential confounding factors, whose selection was informed by a review of relevant literature.
Conclusion
With global public health organizations (WHO) and large-scale donors (PEPFAR) recommending couple counseling scale-up wherever possible, there is a growing need to ensure that couple counseling, is an environment where couples can learn one another’s HIV statuses in a supportive environment. Our results suggest that couple counseling does not result in the loss of social support, but rather enhances it.
Acknowledgments
Sources of Funding: NLB was supported by the National Institutes of Health Fogarty International Center (R25TW009340). The parent study and NER were supported by the National Institute of Mental Health (K99MH104154-01A1).
Footnotes
Ethics: The study received approval from both the National Health Science Research Committee in Malawi and the University of North Carolina at Chapel Hill Institutional Review Board. All participants provided informed consent.
References
- Anglewicz P, & Chintsanya J (2011). Disclosure of HIV status between spouses in rural Malawi. AIDS Care, 23(8), 998–1005. 10.1080/09540121.2010.542130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, Fawzi WW, & Fawzi MCS (2007). Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. JAIDS Journal of Acquired Immune Deficiency Syndromes, 44(4), 470–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen EL, Scott AM, White CR, & Dignan MB (2013). Evaluation of Patient Needs and Patient Navigator Communication about Cervical Cancer Prevention in Appalachian Kentucky. J Commun, 63(1), 72–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S (2004). Social relationships and health. American Psychologist, 59(8), 676. [DOI] [PubMed] [Google Scholar]
- Colombini M, James C, Ndwiga C, Integra team, & Mayhew SH (2016). The risks of partner violence following HIV status disclosure, and health service responses: narratives of women attending reproductive health services in Kenya. Journal of the International AIDS Society, 19(1), 20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy AA, McGrath N, van Rooyen H, Hosegood V, Johnson MO, Fritz K, Darbes LA (2016). Power and the Association with Relationship Quality in South African Couples: Implications for HIV/AIDS Interventions. Social Science & Medicine, 153, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox CM, Hindin MJ, Otupiri E, & Larsen-Reindorf R (2013). Understanding couples’ relationship quality and contraceptive use in Kumasi, Ghana. International Perspectives on Sexual and Reproductive Health, 39(4), 185–194. [DOI] [PubMed] [Google Scholar]
- Darbes LA, Chakravarty D, Beougher SC, Neilands TB, & Hoff CC (2012). Partner-provided social support influences choice of risk reduction strategies in gay male couples. AIDS and Behavior, 16(1), 159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbes LA, Chakravarty D, Neilands TB, Beougher SC, & Hoff CC (2014). Sexual Risk for HIV among Gay Male Couples: A Longitudinal Study of the Impact of Relationship Dynamics. Archives of Sexual Behavior, 43(1), 47–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flax VL, Yourkavitch J, Okello ES, Kadzandira J, Katahoire AR, & Munthali AC (2017). “If my husband leaves me, I will go home and suffer, so better cling to him and hide this thing”: The influence of gender on Option B+ prevention of mother-to-child transmission participation in Malawi and Uganda. PLOS ONE, 12(6), e0178298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, Fogarty L, O’Campo P, Anderson J, Keller J, & Faden R (2000). Women living with HIV: disclosure, violence, and social support. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 77(3), 480–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Malawi Ministry of Health. (2016). Integrated HIV Program Report January-March 2016. [Google Scholar]
- Guidance on Couples HIV Testing and Counselling Including Antiretroviral Therapy for Treatment and Prevention in Serodiscordant Couples: Recommendations for a Public Health Approach. (2012). Geneva: World Health Organization. [PubMed] [Google Scholar]
- Hampanda KM, & Rael CT (2018). HIV Status Disclosure Among Postpartum Women in Zambia with Varied Intimate Partner Violence Experiences. AIDS and Behavior, 22(5), 1652–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, DiMarco M, Austin J, Luke W, & DiFonzo K (2003). Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine, 26(4), 315–332. [DOI] [PubMed] [Google Scholar]
- Karney BR, Hops H, Redding CA, Reis HT, Rothman AJ, & Simpson JA (2010). A Framework for Incorporating Dyads in Models of HIV-Prevention. AIDS and Behavior, 14(0 2), 189–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy CE, Medley AM, Sweat MD, & O’Reilly KR (2010). Behavioural interventions for HIV positive prevention in developing countries: a systematic review and meta-analysis. Bulletin of the World Health Organization, 88(8), 615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlden AP, Hackman CL, & Sharma M (2016). Lifestyle and mental health correlates of psychological distress in college students. Health Education Journal, 75(3), 370–382. [Google Scholar]
- Kronish IM, Edmondson D, Li Y, & Cohen BE (2012). Post-traumatic stress disorder and medication adherence: results from the Mind Your Heart study. Journal of Psychiatric Research, 46(12), 1595–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, & Emmons KM (2006). Understanding health behavior change among couples: an interdependence and communal coping approach. Social Science & Medicine, 62(6), 1369–1380. [DOI] [PubMed] [Google Scholar]
- Maman S, van Rooyen H, & Groves AK (2014). HIV Status Disclosure to Families for Social Support in South Africa (NIMH Project Accept/HPTN 043). AIDS Care, 26(2), 226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, & Maman S (2004). Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bulletin of the World Health Organization, 82(4), 299–307. [PMC free article] [PubMed] [Google Scholar]
- Mepham S, Zondi Z, Mbuyazi A, Mkhwanazi N, & Newell ML (2011). Challenges in PMTCT antiretroviral adherence in northern KwaZulu-Natal, South Africa. AIDS Care, 23(6), 741–747. [DOI] [PubMed] [Google Scholar]
- Nassali M, Nakanjako D, Kyabayinze D, Beyeza J, Okoth A, & Mutyaba T (2009). Access to HIV/AIDS care for mothers and children in sub-Saharan Africa: adherence to the postnatal PMTCT program. AIDS Care, 21(9), 1124–1131. [DOI] [PubMed] [Google Scholar]
- Obermeyer CM, Baijal P, & Pegurri E (2011). Facilitating HIV Disclosure Across Diverse Settings: A Review. American Journal of Public Health, 101(6), 1011–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Sikwane E, & Majaja M (2011). Factors associated with short-course antiretroviral prophylaxis (dual therapy) adherence for PMTCT in Nkangala district, South Africa. Acta Paediatrica, 100(9), 1253–1257. [DOI] [PubMed] [Google Scholar]
- Plazy M, Orne-Gliemann J, Balestre E, Miric M, Darak S, Butsashvili M, Desgrées du Loû A (2013). [Enhanced prenatal HIV couple oriented counselling session and couple communication about HIV (ANRS 12127 Prenahtest Trial)]. Revue D’epidemiologie Et De Sante Publique, 61(4), 319–327. [DOI] [PubMed] [Google Scholar]
- Rosenberg NE, Graybill LA, Wesevich A, McGrath N, Golin CE, Maman S, Hoffman IF (2017). The impact of couple HIV testing and counseling on consistent condom use among pregnant women and their male partners: an observational study. JAIDS Journal of Acquired Immune Deficiency Syndromes, 75(4), 417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg NE, Graybill LA, Wesevich A, McGrath N, Golin CE, Maman S, Hosseinipour MC (2018). Individual, Partner, and Couple Predictors of HIV Infection among Pregnant Women in Malawi: A Case–Control Study. AIDS and Behavior, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg NE, Mtande TK, Saidi F, Stanley C, Jere E, Paile L, Hosseinipour M (2015). Recruiting male partners for couple HIV testing and counselling in Malawi’s option B+ programme: an unblinded randomised controlled trial. The Lancet. HIV, 2(11), e483–e491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg NE, Pettifor AE, De Bruyn G, Westreich D, Delany-Moretlwe S, Behets F, Miller WC (2013). HIV testing and counseling leads to immediate consistent condom use among South African stable HIV-discordant couples. Journal of Acquired Immune Deficiency Syndromes (1999), 62(2), 226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serovich JM, Kimberly JA, Mosack KE, & Lewis TL (2001). The role of family and friend social support in reducing emotional distress among HIV-positive women. Aids Care, 13(3), 335–341. [DOI] [PubMed] [Google Scholar]
- Ssali SN, Atuyambe L, Tumwine C, Segujja E, Nekesa N, Nannungi A, Wagner G (2010). Reasons for disclosure of HIV status by people living with HIV/AIDS and in HIV care in Uganda: an exploratory study. AIDS Patient Care and STDs, 24(10), 675–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart RC, Umar E, Tomenson B, & Creed F (2014). Validation of the multi-dimensional scale of perceived social support (MSPSS) and the relationship between social support, intimate partner violence and antenatal depression in Malawi. BMC Psychiatry, 14, 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Straten A, King R, Grinstead O, Serufilira A, & Allen S (1995). Couple communication, sexual coercion and HIV risk reduction in Kigali, Rwanda. AIDS (London, England), 9(8), 935–944. [DOI] [PubMed] [Google Scholar]
- Vu L, Andrinopoulos K, Mathews C, Chopra M, Kendall C, & Eisele TP (2012). Disclosure of HIV Status to Sex Partners Among HIV-Infected Men and Women in Cape Town, South Africa. AIDS and Behavior, 16(1), 132–138. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2015). WHO Consolidated Guidelines on HIV Testing Services Factsheet. [PubMed]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]


