Abstract
Background
Hybrid decompression has been used to treat patients with cervical spondylotic myelopathy (CSM). However, no published study has investigated the effect of titanium mesh (TM) located cephalad or caudal in hybrid decompression surgery on the graft subsidence in treatment of three-level CSM.
Material/Methods
Forty-eight cases with three-level CSM who underwent the procedure of hybrid decompression from Jan 2014 to Jan 2017 were retrospectively reviewed. Radiological outcomes immediately postoperatively and at the final follow-up were compared between cases from group A (TM located cephalad, n=21) and group B (TM located caudal, n=27).
Results
No differences were observed in the 2 groups in terms of number, sex, or duration of follow-up. The average follow-up was 4.38±0.439 months in group A and 4.81±0.509 months in group B (p>0.05). The index loss of anterior (AIBH), middle (MIBH), and posterior interbody height (PIBH) in group A were 0.857±0.448/1.00±0.525/1.33±0.608, respectively, which were all lower than that in group B (P<0.05), as was the occurrence of TM subsidence. However, there was no significance difference in height loss of adjacent intervertebral space between groups. All angles were decreased at the final follow-up in both groups (p<0.05). More decrease of C2–C7 angle occurred in group B (p>0.05), and segmental angle in group A decreased more than in group B (p>0.05).
Conclusions
TM inferior to intervertebral cage (IC) in hybrid decompression has a higher risk for developing subsidence, and when the choice of the position of TM is available in hybrid decompression surgery, TM located cephalad was recommend to alleviate TM subsidence.
MeSH Keywords: Osteoarthritis, Spine; Periprosthetic Fractures; Spinal Cord Compression; Spine
Background
Cervical spondylotic myelopathy (CSM) is a common age-related degenerative disease characterized by progressive narrowing of the spinal canal, which results in compression of the spinal cord. Due to its insidious onset, patients with CSM frequently require surgical decompression [1]. The objects of surgical technique for CSM are decompression of the nerve roots and spinal cord, stabilization of the spinal column, and maintaining cervical alignment [2]. For patients with CSM, the anterior approach can yield good outcomes by direct decompression of the spine. Both anterior cervical discectomy and fusion (ACDF) and anterior cervical corpectomy and fusion (ACCF) are effective treatments for patients with severe anterior pathogenic structures and cervical kyphosis [3]. ACDF is appropriate for cases with a compressing lesion primarily confined to the disc space region without extending extensively behind the vertebral body [4]. ACCF is used for larger ossified masses beyond the cervical spine interspaces. However, for patients with three-level CSM, the results are far from satisfactory. The long corpectomy for the treatment of multi-level CSM was reported to cause higher occurrence of graft subsidence, delayed union or nonunion, and pseudoarthrosis with increased numbers of decompressed levels [5,6].
The hybrid decompression procedure combining one-vertebra corpectomy and one-level discectomy was first introduced by Ashkenazi et al. for the treatment of three-level CSM, and has been reported to have high effectiveness and safety [7,8]. However, the restoration of cervical lordosis following the HDF is inferior to the ACDF at the final visit, and subsidence of the titanium mesh (TM) may play a pivotal role in loss of lordosis correction [9]. It was reported that the incidence of TM subsidence was approximately 96%, and severe subsidence frequently resulted in neurological deterioration, neck pain, and instrument failures [10,11]. Several factors may contribute to TM subsidence, such as age, sex, fusion level, endplate preparation, and bone mineral density [12]. However, to the best of our knowledge, no uniform standard has been published regarding where the TM should be placed in hybrid decompression surgery to avoid graft subsidence in the treatment of three-level CSM [13].
In this study, we compared the radiological changes in patients with three-level CSM who had hybrid decompression procedure and assessed the effect of the position of TM relative to intervertebral cage (IC) on graft subsidence.
Material and Methods
Patient population
From Jan 2014 to Jan 2017, we retrospectively reviewed 92 consecutive cases with CSM who underwent hybrid decompression procedure using titanium mesh (TM, DePuy, USA) by the same spine surgery team in our Orthopedics Department. We excluded 25 cases who had injury history, previous history of cervical spine surgery, infection, or cancer, and 19 cases were excluded for lack of a lateral radiograph at follow-up. Finally, 48 cases were selected for our study and were divided into group A (TM located cephalad, n=21, Figure 1A, Table 1) and group B (TM located caudal, n=27, Figure 1B, Table 1) according to the level of TM. This study was approved by the Institutional Review Board of our institution, and all patients signed informed consent.
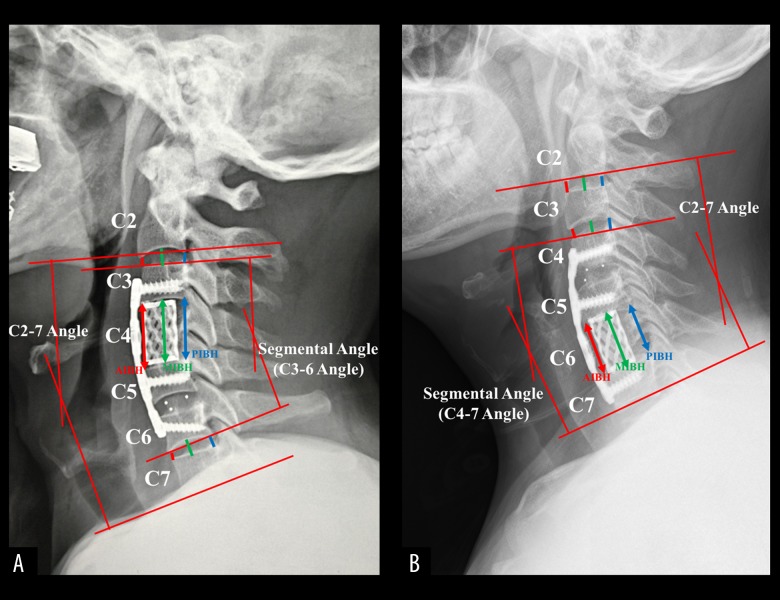
Figure 1.
Radiological measurement of the cervical spine. (A) Measurement of the TM subsidence (AIBH, MIBH, PIBH), HAIS (C2–C3 and C6–C7), C2–C7 angle, and segmental angle (C3–C6 angle). (B) Measurement of the TM subsidence (AIBH, MIBH, PIBH), HAIS (C2–C3 and C3–C4) and the space of vertebrae superior and inferior to TM, C2–C7 angle, and segmental angle (C4–C7 angle). AIBH, MIBH, and PIBH was the length between the anterior, middle, and posterior portions of the adjacent upper and lower endplates, respectively. AIBH is indicated by red arrow, MIBH by green arrow, and PIBH by blue arrow. HAIS was defined as the anterior, middle, and posterior height of the adjacent space, which is indicated by red, green, and blue short lines, respectively.
Table 1.
Comparisons of general demographic data between Group A and Group B. Interobserver reliability.
| Group A | Group B | p Value | |
|---|---|---|---|
| TMC located cephalad | TMC located caudal | ||
| Numbers | 21 | 27 | |
| Sex (Female/Male, n) | 8/13 | 8/19 | 0.537 |
| Age (years) | 53.95±9.877 | 54.11±9.720 | 0.774 |
| Fusion segments (n) | |||
| C3–C6 | 13 | 18 | |
| C4–C7 | 8 | 9 | |
| Follow-up (months) | 4.38±0.439 | 4.81±0.509 | 0.290 |
Surgical techniques
The hybrid decompression operation was performed as previously described [13]. Briefly, after general endotracheal anesthesia, a right-sided Smith-Robinson approach was used to expose cervical vertebral bodies and discs. Discectomy was carried out first. After careful removal of disc, posterior osteophyte, and ossified longitudinal ligament, an appropriately sized intervertebral cage (IC, DePuy, USA) packed with autogenous bone was inserted into the intervertebral space. Of note, more attention should be paid to avoiding excessive damage to the endplate. After adequate adjacent discectomies, corpectomy was conducted by resecting three-fifths of the vertebral body. Then, the posterior longitudinal ligament was resected in each patient to ensure full decompression of the spinal cord. After being packed with autogenous bone, the TM was filled with autologous bone fragments harvested from the excised vertebra, and then implanted under distraction. The distraction was less than 6 mm for two-level corpectomy. The TM was inserted at two-thirds of the vertebral column, usually 2–3 mm to the vertebral anterior border. A semiconstrained cervical plate (Skyline or Slimlock, DePuy, USA) was used to bridge the fusion segments. All patients in this study wore a Philadelphia neck collar for at least 2 months.
Demographic and radiological analysis
Demographic information was collected for all patients, including age, sex, and duration of follow-up. Our study defined a minimum duration of follow-up as 3 months on the basis of previous studies demonstrating that significant changes in construct geometry frequently occurred within about 3 months following surgery [14]. Several radiological parameters were measured immediately postoperatively and at the last follow-up (more than 3 months): anterior (AIBH), middle (MIBH), and posterior interbody height (PIBH), the height of adjacent intervertebral space (HAIS), C2–C7 angel (Cobb angle), and segmental angle (C3–C6 angle, and C4–C7 angle) (Figure 1). These parameters were determined by neutral lateral radiographs taken with the patient in a standing position. Of note, if the lower cervical spine was not visualized on a simple radiograph, we adjusted the contrast ratio of the bony structure and soft tissue on Mimics Research 9.0 to visualized the profile of the C7 vertebral body. Anterior, middle, and posterior subsidence of TM were defined as the loss between the immediately postoperative and final follow-up values in AIBH, MIBH, and PIBH, respectively [15]. The overall TM subsidence was calculated as the average of AIBH, MIBH, and PIBH, which were divided into mild subsidence (1–3 mm) and severe subsidence (>3 mm) [16]. Adjacent segmental changes were defined as the difference between postoperative and final follow-up values in HAIS. C2–C7 angle indicated the angle formed between the lower endplate of C2 and the lower endplate of C7 [17]. Segmental angle was defined as the angle formed between the lines parallel the cranial endplate of the most cranial vertebra and the caudal endplate of the most caudal vertebra at the fusion level. All these measurements were performed by 2 independent observers who were not involved in this study. Measurement values were recorded and interclass coefficients were analyzed.
Statistical analysis
Statistical data were analyzed using SPSS (version 18.0, SPSS, Inc. Chicago, IL, USA). Quantitative data were compared by the independent-samples t test, paired t test, and chi-square test. Differences were defined as significant when the p value was less than 0.05.
Results
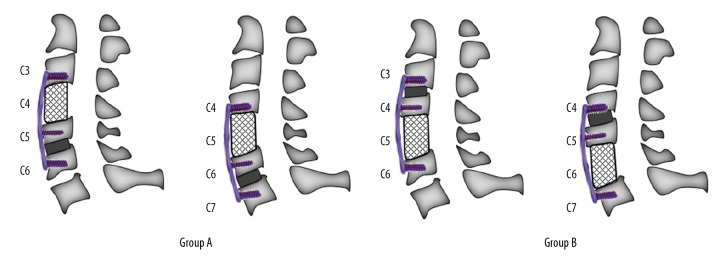
All 48 patients in our study underwent three-level hybrid decompression and fusion, of whom 16 (33%) were female and 32 (67%) were male. The average follow-up was 4.38±0.439 and 4.81±0.509 months in group A and group B, respectively. Among the 31 patients with C3–C6 decompression, TM was implanted superior to the IC in 13 cases, and 18 cases had the TM inferior to the IC. For 17 patients with C4–C7 decompression, TM was superior to the cage in 8 cases and 9 cases had TM inferior to the cage (Figure 2). No significant differences in demographic data were observed between the 2 groups (Table 1).
Figure 2.
Classification of groups based on the relative level of TM to IC.
Interobserver reliability
Interobserver reliability was excellent for all cervical radiographic parameters for the 2 independent observers.
Cervical parameters
Table 2 summarizes the comparison of the TM subsidence among patients who underwent hybrid decompression with different TM levels relative to IC. There were no significant differences in TM subsidence immediately postoperatively between the 2 groups (P>0.05). TM subsidence occurred 85% in group B and 76% in group A. In group A, the AIBH was 28.73±2.541 immediately postoperatively and 27.11±2.619 at the final follow-up, the MIBH was 28.64±2.801 and 26.55±2.823 and the PIBH was 27.06±2.493 and 24.47±2.497. In group B, the AIBH/MIBH/PIBH was 29.34±1.885/29.35±1.947/27.06±2.655 immediately postoperatively and 28.49±2.068/28.35±2.149/ 25.73±2.566 at the final follow-up. The differences in AIBH/MIBH/PIBH between the 2 groups at the final follow-up were significant (p<0.05). The index loss of AIBH/MIBH/PIBH in group A was 0.857±0.448/1 1.33±0.60/8.00±0.525, respectively, all lower than that in group B (P<0.05). In group B, 3 patients had severe TM subsidence at the final follow-up (Figures 3, 4), including 2 cases with fusion of C3–C6 and 1 case with fusion of C4–C7.
Table 2.
Comparisons of the TMC subsidence immediately postoperatively and at the final follow-up.
| Immediately postoperatively | Final follow-up | Index loss | P1 value | |
|---|---|---|---|---|
| AIBH | ||||
| Group A | 28.73±2.541 | 27.11±2.619 | 0.857±0.448 | 0.000 |
| Group B | 29.34±1.885 | 28.49±2.068 | 1.62±0.991 | 0.000 |
| p value | 0.158 | 0.042 | 0.004 | |
| MIBH | ||||
| Group A | 28.64±2.801 | 26.55±2.823 | 1.00±0.525 | 0.000 |
| Group B | 29.35±1.947 | 28.35±2.149 | 2.09±0.792 | 0.000 |
| P2 value | 0.117 | 0.045 | 0.032 | |
| PIBH | ||||
| Group A | 27.06±2.493 | 24.47±2.497 | 1.33±0.608 | 0.000 |
| Group B | 27.06±2.655 | 25.73±2.566 | 2.59±1.167 | 0.000 |
| p value | 0.74 | 0.034 | 0.001 | |
Index loss=value of immediate postoperation – value of final follow-up. P1 indicates the p value of comparison between index value immediately postoperatively and at final follow-up in the same group. P2 value indicates the p value of comparison index value of different groups at the same time point
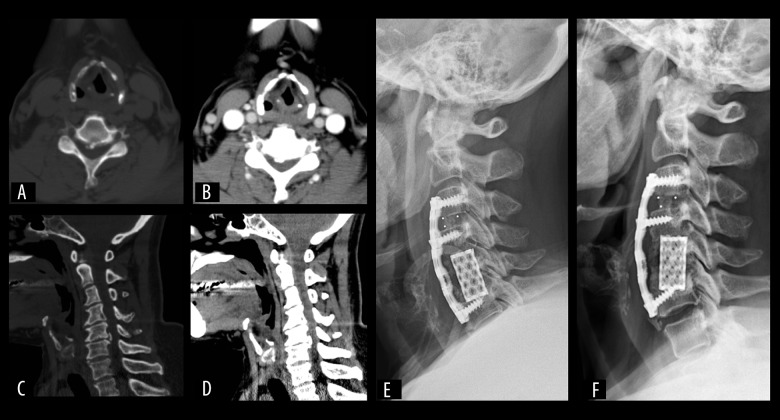
Figure 3.
(A–F) Case 1. A 47-year-old female patient with three-level CSM (C3–C6) complained of degenerative hands numbness and lower limbs instability for more than 2 years. Sagittal and axial CT demonstrated severe disc degeneration and osteophyte at C3/4 and C4/5. Severe TM subsidence and graft migration were found just 7 months postoperatively by lateral plain radiograph.
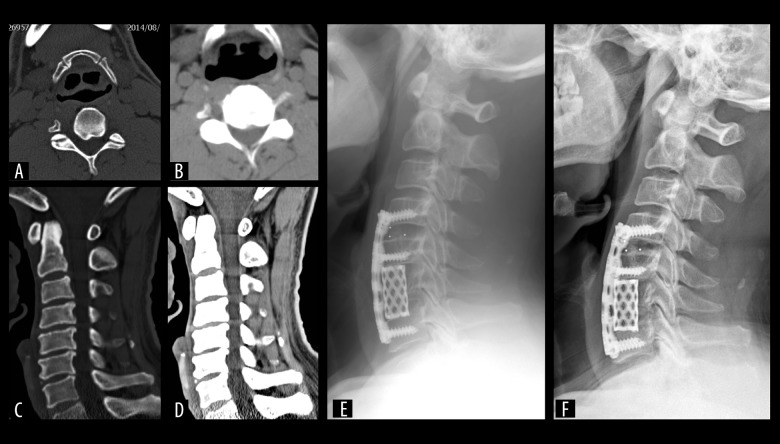
Figure 4.
(A–F) Case 2. A 45-year-old male patient presented with weakness and numbness of his hands and lower limbs for 1 year. Preoperative imaging showed protrusion of multi-level intervertebral disc (C3/4, C4/5, and C5/6) with significant disc degeneration at C5/6 level, and osteophytes located at dorsal part of C3–C6 vertebral body. He underwent the hybrid decompression procedure of C4–C7. Lateral radiograph showed significant TM subsidence at the final follow-up of 6 months.
Table 3 summarizes the height loss of adjacent intervertebral space. Because degeneration at disc C7/T1 was not common [16], we used disc C2–C3 as the adjacent segment instead of disc C7–T1 in cases with fusion segment from C4 to C7. There was no significance difference immediately postoperatively or at the final follow-up in height loss of adjacent intervertebral space in either group (p>0.05).
Table 3.
Comparisons of the height loss of intervertebral space adjacent to the fusion segment postoperatively and at the final follow-up.
| AIBH loss | MIBH loss | PIBH loss | ||
|---|---|---|---|---|
| Fusion segment of C3–C6 | ||||
| C2–C3 | Group A | 0.46±0.487 | 0.43±0.757 | 0.60±0.606 |
| Group B | 0.44±0.373 | 0.47±0.387 | 0.56±0.358 | |
| p value | 0.248 | 0.439 | 0.086 | |
| C6–C7 | Group A | 0.60±0.640 | 0.84±0.937 | 0.72±0.422 |
| Group B | 0.61±0.396 | 0.54±0.386 | 0.66±0.340 | |
| p value | 0.140 | 0.057 | 0.068 | |
| Fusion segment of C4–C7 | ||||
| C2–C3 | Group A | 0.63±0.328 | 0.68±0.599 | 0.65±0.4000 |
| Group B | 0.67±0.436 | 0.53±0.287 | 0.62±1.091 | |
| p value | 0.437 | 0.065 | 0.281 | |
| C3–C4 | Group A | 0.33±0.104 | 0.68±0.587 | 0.61±0.307 |
| Group B | 0.39±0.215 | 0.62±0.593 | 0.64±0.446 | |
| p value | 0.098 | 0.611 | 0.077 | |
Cobb angle (C2–C7 angel), and segmental angles (C3–C6 angle, C4–C7 angle) immediately postoperatively and at the last follow-up are shown in Table 4. All angles were decreased at the final follow-up in both groups (p<0.05). However, no significant differences were observed in angle between the 2 groups (p>0.05).
Table 4.
Cobber angle and segmental angle in fusion segment of C3–C6 and C4–C7 postoperatively and at the final follow-up. Immediately postoperatively.
| Immediately postoperatively | Final follow-up | P1 value | Index loss | P2 value | ||
|---|---|---|---|---|---|---|
| Fusion segment of C3–C6 | ||||||
| Group A | C2–C7 | 20.87±9.990 | 20.42±10.713 | 0.000 | 0.45±6.800 | 0.640* |
| C3–C6 | 13.97±6.386 | 13.62±6.167 | 0.000 | 0.35±4.371 | ||
| Group B | C2–C7 | 18.72±8.142 | 18.30±9.057 | 0.044 | 0.52±8.062 | 0.379** |
| C3–C6 | 14.48±6.512 | 14.24±5.013 | 0.032 | 0.24±5.362 | ||
| Fusion segment of C4–C7 | ||||||
| Group A | C2–C7 | 15.86±6.163 | 14.89±7.323 | 0.040 | 0.97±4.639 | 0.348* |
| C4–C7 | 17.19±3.586 | 15.23±5.549 | 0.011 | 1.96±3.008 | ||
| Group B | C2–C7 | 17.67±7.959 | 15.96±5.038 | 0.017 | 1.71±6.987 | 0.070** |
| C4–C7 | 16.19±7.787 | 15.37±8.605 | 0.016 | 0.82±5.629 | ||
Index loss=value of immediate postoperation – value of final follow-up. P1 – comparison between postoperatively and the final follow-up. P2 – comparison of index loss between group A and group B.
Indicates comparison of C2–C7 between group A and group B.
Indicates comparison of segmental angles (C3–C6 and C4–C7) between group A and group B.
Discussion
Patients diagnosed with CSM frequently require decompression surgery to prevent further deterioration [18]. The ACDF technique is only appropriate for cases whose lesions are primarily confined to the disc space region, which limits its clinical application for complete decompression through intervertebral spaces in some cases [19]. Additionally, surgery-related complications such as nonunion are another issue which needs attention, especially in multi-level ACDF [20]. The ACCF procedure is optional for multi-level CSM. However, it has more bleeding, lower fusion rate, and higher incidences of postoperative complications compared with the ACDF, and the improvement of the cervical and segmental lordosis was significantly less than with ACDF [4].
Hybrid decompression combined one-vertebrae corpectomy and one-level discectomy is an alternative to treat multi-level CSM. When treating multi-level CSM, hybrid decompression can address mild stenosis in intervertebral space by adjacent discectomy and provide simultaneous decompression in the vertebral segments with significant lesion of the intervertebral disc space and large osteophytes behind the vertebral bodies by corpectomy, which can achieve full decompression and less insult to the spinal cord and nerve roots [21]. A biomechanical study by Singh revealed that hybrid decompression can avoid the long fused segments and maintain better stability and cervical alignment of the operated levels and less occurrence of plate migration by segmental plate fixation compared to end-construct plate fixation [22].
Although hybrid decompression has several advantages over ACCF and ACDF, such as less bleeding, higher fusion rate, more accurate insertion of the implants, and better maintenance of the cervical lordosis, the advantages may be offset by the higher rate of TM subsidence, which may cause buckling of the cervical ligament flavum, foraminal stenosis, and consequent recompression of spinal cord and nerve roots [4,23]. Subsided TM occurred in up to 80% of patients in the early postoperative period, which may damage the inherent stability of the fusion segments and increase the mechanical load on the screw-plate structure [24]. A study by Daubs et al. reported on 7 patients (30%) who had reconstruction failure before 12 weeks following surgery, especially in cases with multi-level corpectomy [25]. In addition, Nakase reported that subsidence-related complications such as kyphotic deformity, instrument failure, and neurological deterioration can develop and possibly need revision surgery [26].
Many risk factors can contribute to TM subsidence. Older people, especially females after menopause, are commonly considered to have higher risk for developing TM subsidence because of decreased bone density of the vertebrae and the thickness of the endplates [27]. In addition, aggressive cleaning and resection of the endplates, over-distraction of the intervertebral space, and the sharp edge of the cage can also trigger occurrence of TM. Therefore, during the operation, we paid more attention to surgical details. Chen et al. demonstrated TM subsidence occurred in 239 (79.7%) patients, and two-level ACCF with TM was more susceptible to developing severe subsidence (1–3 mm) [16]. Furthermore, several reports suggested that incidence of TM subsidence was higher than that of the IC, and segmental subsidence may be higher after hybrid decompression procedure [28,29]. Thus, more attention should also be paid to the TM subsidence after hybrid decompression procedure.
However, to the best of our knowledge, few studies have been published to determine the optimal location of TM in hybrid decompression surgery to avoid graft subsidence in the treatment of three-level CSM. In the present study, both groups revealed the occurrence of TM subsidence following hybrid decompression in the early stage, which agrees with a previous study [13]. In our study, we defined the TM subsidence as loss of the segmental height (AIBH, MIBH, and PIBH) between vertebral body inferior and superior to the TM to avoid the influence induced by the subsidence of IC. AIBH, MIBH, and PIBH in both groups were comparable, with occurrence of 76% in group A and 85% in group B, and the subsidence on TM was the most severe at the posterior border of the inferior endplate with the largest loss of PIBH, which is consistent with previous studies [13,30]. Most of the inferior cage-endplate contact area is limited to the anterior two-thirds portion of the vertebral body, which frequently results in weak contact between the posterior rim of the TM and endplate [31]. In case of more removal or damage of the endplate, the connection between TM and cancellous portion of the vertebral body would be weaker, and thus the center of stress would act on the posterior portion of TM due to cervical lordosis. In addition, Wu et al. suggested the orientation of endplates at different levels may be also be responsible for this tendency due to disordered stress distribution [15].
Of note, the value of TM subsidence (AIBH, MIBH, and PIBH) in group B was 1.62±0.991, 2.09±0.792, and 2.59±1.167, respectively, which is higher than that in group A (P<0.05), indicating that hybrid decompression with TM inferior to the IC had more tendency to subsidence than that with TM superior to the IC. A study by Liu et al. revealed more height loss with TM inferior to the IC, but this was not emphasized in the study [13]. There are several factors that may explain the results. Firstly, compared with discectomy construct, the corpectomy construct has higher stress acting on the bone grafts and endplates because of the limited contact area between the TM and endplates. Secondly, previous biomechanical studies suggested that the lever arm at the distal end of the plate increased with the length of the plate and the long fixed-moment arm constructs tend to exert far more load on the caudal screw-bone interface than the rostral, which frequently resulted in high construct failure at the caudal ends of the construct [32,33]. Therefore, the skip technique with intermediate vertebral body intact was reported by Dalbayrak to be an alternative for standard multi-level ACCF in the treatment of CSM, which may acquire a favorable load distribution [34]. However, biomechanics of the “skip” corpectomy did not evaluate the axial forces acting on the caudal plate [35]. Additionally, in hybrid decompression procedure with TM located caudal, inferior TM-vertebral surface may be loaded with more stress, and thus TM located caudal may have a higher risk for developing subsidence. Thirdly, TM subsidence seems to occur more commonly at the inferior TM-endplate contact than at the superior portion of the TM [12]. Although hybrid decompression procedure consists of one IC and one TM, the application of anterior cervical plate makes the IC and TM unified. Therefore, the larger subsidence of TM at its lower rim may be explained by the higher rate of subsidence at the lower rim of TM after ACCF only.
Intervertebral space superior and inferior to the index segments was measured in this study. No significant difference of the height loss in adjacent segments was observed in either group. This may be explained by the relatively short follow-up period of this study, and a longer follow-up period may more accurately reveal the effect of the relative level of TM to IC on the adjacent intervertebral space. Guo et al. reported that the hybrid decompression procedure was superior to ACCF in terms of segmental angle and C2–C7 angle improvement [10]. In the present study, we evaluated Cobb angle (C2–C7 angle) and segmental angle immediately postoperatively and at the final follow-up. Normal values of Cobb angle (C2–C7 angle) have been reported to be about 24° (range from 10° to 34°) [15]. In our study, the C2–C7 angle was corrected following the surgery, but more decrease of C2–C7 angle occurred in group B at the final follow-up (p>0.05), which may be associated with more severe TM subsidence in group B. In addition, all patients had decreased segmental angle at the final follow-up of 3 months (p<0.05). Interestingly, segmental angle in group A decreased more than that in group B (p>0.05), but the reason for this is unclear. Finite element analysis of the change in cervical alignment would be required to accurately determine the relationship between the position of TM and cervical angles following hybrid decompression surgery in the future.
The present study has several limitations. Firstly, this study included 48 cases in total and only 17 patients with fusion segments of C4–C7. This is because the study was retrospective, and many patients did not have normal follow-up, and the lateral radiological images were unavailable, which resulted in fewer cases in our study. Therefore, a randomized controlled trial with more cases will be needed to evaluate these results in the future. Secondly, although the TM subsidence were more significant in patients with TM inferior to IC, few cases of severe subsidence was observed in the 2 groups. We think that the cases in our study had relatively short duration of follow-up. Several studies have reported TM subsidence after ACCF occurred in up to 80% of patients in the early postoperative period (at least 6 months) [24]. Therefore, a longer follow-up period is required to adequately evaluate if TM inferior to IC has higher risk for developing severe subsidence. Thirdly, we did not evaluate the relationship between the subsidence and clinical outcomes. Chen et al. reported that mild subsidence did not cause significant clinical results, but severe subsidence was correlated with bad neurologic outcome and subsidence-related complications, owing to the greater loss of height of the fusion segments [16]. However, a meta-analysis by Karikari et al. suggested subsidence has no impact on successful fusion and/or good clinical outcomes [12].
Conclusions
TM inferior to IC in hybrid decompression procedure has a higher risk for developing subsidence. The relative position of TM to IC has no significant effect on adjacent intervertebral space. Considering that TM subsided more than IC, our results suggest that TM located cephalad is the best choice for the position of TM in hybrid decompression surgery.
Footnotes
Source of support: Departmetnal sources
References
- 1.Luo J, Cao K, Huang S, et al. Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J. 2015;24:1621–30. doi: 10.1007/s00586-015-3911-4. [DOI] [PubMed] [Google Scholar]
- 2.Matsunaga S, Komiya S, Toyama Y. Risk factors for development of myelopathy in patients with cervical spondylotic cord compression. Eur Spine J. 2015;24:142–49. doi: 10.1007/s00586-013-2839-9. [DOI] [PubMed] [Google Scholar]
- 3.Liu T, Xu W, Cheng T, et al. Anterior versus posterior surgery for multilevel cervical myelopathy, which one is better? A systematic review. Eur Spine J. 2011;20:224–35. doi: 10.1007/s00586-010-1486-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y, Hou Y, Yang L, et al. Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine. 2012;37:1450–58. doi: 10.1097/BRS.0b013e31826c72b4. [DOI] [PubMed] [Google Scholar]
- 5.Xiao SW, Jiang H, Yang LJ, et al. Anterior cervical discectomy versus corpectomy for multilevel cervical spondylotic myelopathy: A meta-analysis. Eur Spine J. 2015;24:31–39. doi: 10.1007/s00586-014-3607-1. [DOI] [PubMed] [Google Scholar]
- 6.Dan H, Du X, Liang H, et al. Anterior corpectomy versus posterior laminoplasty for the treatment of multilevel cervical myelopathy: A meta-analysis. Int J Surg. 2016;5:21–27. doi: 10.1016/j.ijsu.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Záratekalfopulos B, Araossilva W, Reyessánchez A, et al. Hybrid decompression and fixation technique for the treatment of multisegmental cervical spondylotic myelopathy. Int J Spine Surg. 2016;10:30. doi: 10.14444/3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu JM, Peng HW, Liu ZL, et al. Hybrid decompression technique versus anterior cervical corpectomy and fusion for treating multilevel cervical spondylotic myelopathy: Which one is better? World Neurosurg. 2015;84:2022–29. doi: 10.1016/j.wneu.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 9.Guo Q, Bi X, Ni B, et al. Outcomes of three anterior decompression and fusion techniques in the treatment of three-level cervical spondylosis. Eur Spine J. 2011;20:1539–44. doi: 10.1007/s00586-011-1735-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y, Chen D, Guo Y, et al. Subsidence of titanium mesh cage: A study based on 300 cases. J Spinal Disord Tech. 2008;21:489–92. doi: 10.1097/BSD.0b013e318158de22. [DOI] [PubMed] [Google Scholar]
- 11.Kabir SM, Alabi J, Rezajooi K, et al. Anterior cervical corpectomy: Review and comparison of results using titanium mesh cages and carbon fibre reinforced polymer cages. Br J Neurosurg. 2010;24:542–46. doi: 10.3109/02688697.2010.503819. [DOI] [PubMed] [Google Scholar]
- 12.Karikari IO, Jain D, Owens TR, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: A systematic review. J Spinal Disord Tech. 2014;27(1):1–10. doi: 10.1097/BSD.0b013e31825bd26d. [DOI] [PubMed] [Google Scholar]
- 13.Liu X, Chen Y, Yang H, et al. The application of a new type of titanium mesh cage in hybrid anterior decompression and fusion technique for the treatment of continuously three-level cervical spondylotic myelopathy. Eur Spine J. 2017;26:122–30. doi: 10.1007/s00586-016-4888-3. [DOI] [PubMed] [Google Scholar]
- 14.Koller H, Hempfing A, Ferraris L, et al. 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J. 2007;16:2055–71. doi: 10.1007/s00586-007-0398-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu J, Luo D, Ye X, et al. Anatomy-related risk factors for the subsidence of titanium mesh cage in cervical reconstruction after one-level corpectomy. Int J Clin Exp Med. 2015;8:7405–11. [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y, Chen D, Guo Y, et al. Subsidence of titanium mesh cage: A study based on 300 cases. J Spinal Disord Tech. 2008;21:489–92. doi: 10.1097/BSD.0b013e318158de22. [DOI] [PubMed] [Google Scholar]
- 17.Lee SE, Jahng TA, Kim HJ. Correlation between cervical lordosis and adjacent segment pathology after anterior cervical spinal surgery. Eur Spine J. 2015;24:2899–909. doi: 10.1007/s00586-015-4132-6. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Liu H, Yang H, et al. Anterior cervical corpectomy and fusion versus discectomy and fusion for the treatment of two-level cervical spondylotic myelopathy: Aanalysis of sagittal balance and axial symptoms. Int Orthop. 2018;42:1877–82. doi: 10.1007/s00264-018-3804-3. [DOI] [PubMed] [Google Scholar]
- 19.Shamji MF, Massicotte EM, Traynelis VC, et al. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: A systematic review. Spine. 2013;38:195–209. doi: 10.1097/BRS.0b013e3182a7eb27. [DOI] [PubMed] [Google Scholar]
- 20.Del GR, Bydon A. Erratum: Long-term clinical outcomes following 3- and 4-level anterior cervical discectomy and fusion. J Neurosurg Spine. 2016;24:885–91. doi: 10.3171/2015.10.SPINE15795. [DOI] [PubMed] [Google Scholar]
- 21.Odate S, Shikata K, Kimura H, Soeda T, et al. Hybrid decompression and fixation technique versus plated 3-vertebra corpectomy for 4-segment cervical myelopathy: Analysis of 81 cases with a minimum 2-year follow-up. Clin Spine Surg. 2016;29:226–33. doi: 10.1097/BSD.0b013e31827ada34. [DOI] [PubMed] [Google Scholar]
- 22.Singh K, Vaccaro AR, Kim J, et al. Enhancement of stability following anterior cervical corpectomy: A biomechanical study. Spine. 2004;29:845–49. doi: 10.1097/00007632-200404150-00005. [DOI] [PubMed] [Google Scholar]
- 23.Jang JW, Lee JK, Lee JH, et al. Effect of posterior subsidence on cervical alignment after anterior cervical corpectomy and reconstruction using titanium mesh cages in degenerative cervical disease. J Clin Neurosci. 2014;21:1779–85. doi: 10.1016/j.jocn.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 24.Fengbin Y, Jinhao M, Xinyuan L, et al. Evaluation of a new type of titanium mesh cage versus the traditional titanium mesh cage for single-level, anterior cervical corpectomy and fusion. Eur Spine J. 2013;22:2891–96. doi: 10.1007/s00586-013-2976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daubs MD. Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine J. 2005;30:1402–6. doi: 10.1097/01.brs.0000166526.78058.3c. [DOI] [PubMed] [Google Scholar]
- 26.Nakase H, Park YS, Kimura H, et al. Complications and long-term follow-up results in titanium mesh cage reconstruction after cervical corpectomy. J Spinal Disord Tech. 2006;19:353–57. doi: 10.1097/01.bsd.0000210113.09521.aa. [DOI] [PubMed] [Google Scholar]
- 27.Hasegawa K, Abe M, Washio T, et al. An experimental study on the interface strength between titanium mesh cage and vertebra in reference to vertebral bone mineral density. Spine. 2001;26:957–63. doi: 10.1097/00007632-200104150-00022. [DOI] [PubMed] [Google Scholar]
- 28.Park Y, Maeda T, Cho W, et al. Comparison of anterior cervical fusion after two-level discectomy or single-level corpectomy: Sagittal alignment, cervical lordosis, graft collapse, and adjacent-level ossification. Spine J. 2010;10:193–99. doi: 10.1016/j.spinee.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 29.Karikari IO, Jain D, Owens TR, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: A systematic review. J Spinal Disord Tech. 2014;27:1–10. doi: 10.1097/BSD.0b013e31825bd26d. [DOI] [PubMed] [Google Scholar]
- 30.van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW. Anterior cervical interbody fusion with a titanium box cage: Early radiological assessment of fusion and subsidence. Spine J. 2005;5:645–49. doi: 10.1016/j.spinee.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 31.Cheng CC, Ordway NR, Zhang X, et al. Loss of cervical endplate integrity following minimal surface preparation. Spine. 2007;32:1852–55. doi: 10.1097/BRS.0b013e31811ece5a. [DOI] [PubMed] [Google Scholar]
- 32.Schlenk RP, Stewart T, Benzel EC. The biomechanics of iatrogenic spinal destabilization and implant failure. Neurosurg Focus. 2003;15:E2. doi: 10.3171/foc.2003.15.3.2. [DOI] [PubMed] [Google Scholar]
- 33.Zhang B, Li S, Miao D. Risk factors of cage subsidence in patients with ossification of posterior longitudinal ligament (OPLL) after anterior cervical discectomy and fusion. Med Sci Monit. 2018;24:4753–59. doi: 10.12659/MSM.910964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dalbayrak S, Yilmaz M, Naderi S. “Skip” corpectomy in the treatment of multilevel cervical spondylotic myelopathy and ossified posterior longitudinal ligament”. J Neurosurg Spine. 2010;12:33–38. doi: 10.3171/2009.7.SPINE08965. [DOI] [PubMed] [Google Scholar]
- 35.Yilmaz M, Yüksel KZ, Baek S, et al. Biomechanics of cervical “skip” corpectomy versus standard multilevel corpectomy. J Spinal Disord Tech. 2017;30:E152–61. doi: 10.1097/BSD.0b013e318268d30a. [DOI] [PMC free article] [PubMed] [Google Scholar]