Abstract
Background
During critical illness in humans, the effects of caloric restriction on the inflammatory response are not well understood. The aim of this study is to examine the associations of caloric restriction, inflammatory response profiles and outcomes in critically ill patients.
Methods
This is a sub-study of the PermiT trial (Permissive Underfeeding or Standard Enteral Feeding in Critically Ill Adults Trial- ISRCTN68144998). Serum samples were collected on study days 1, 3, 5, 7 and 14 and analyzed for a panel of 29 cytokines. We used principal component analysis to convert possibly correlated variables (cytokine levels) into a limited number of linearly uncorrelated variables (principal components). We constructed repeated measures mixed linear models to assess whether permissive underfeeding compared to standard feeding was associated with difference cytokine levels over time.
Results
A total of 72 critically ill patients were enrolled in this study (permissive underfeeding n = 36 and standard feeding n = 36). Principal component analysis identified 6 components that were responsible for 78% of the total variance. When adjusted to principal components, permissive underfeeding was not associated with 90-day mortality (adjusted odds ratio 1.75, 95% confidence interval 0.44, 6.95, p = 0.43) or with incident renal replacement therapy. The cytokines did not differ with time between permissive underfeeding and standard feeding groups.
Conclusions
The association of permissive underfeeding compared to standard feeding with mortality was not influenced by the inflammatory profile. Permissive underfeeding compared to standard feeding was not associated with differences in the serum levels of cytokines in critically ill patients.
Introduction
The possible effects of caloric and protein intake on inflammatory response have been increasingly recognized. Caloric restriction has been shown to attenuate the inflammatory response associated with diabetes, obesity, cancer, cardiovascular disease and ageing.[1–3] During critical illness, which is typically characterized by an intense pro-inflammatory response, the effects of caloric intake on inflammation are less certain. Animals subjected to caloric restriction mounted less elevation of pro-inflammatory cytokines.[4, 5] During critical illness in humans, the effects of caloric restriction on the inflammatory response are not well understood.
The objective of this sub-study of the PermiT (Permissive Underfeeding versus Target Enteral Feeding in Adult Critically Ill Patients Trial)[6] is to examine the associations of caloric restriction, inflammatory response profiles and outcomes in critically ill patients. We hypothesized that permissive underfeeding attenuates the pro-inflammatory response and that the association of caloric intake with clinical outcomes may differ according to patient inflammatory profile. Some of these findings have been previously presented and published as an abstract.[7]
Materials and methods
Study population
This is a sub-study of the PermiT trial, in which critically ill patients were randomized to permissive underfeeding (40–60% of calculated caloric requirements) or standard feeding (70–100%) for up to 14 days while maintaining similar protein intake in both groups.[8] Eligibility criteria and interventions are detailed in the publication of the main trial.[6, 8] The trial found no difference in the primary endpoint of 90-day mortality between the permissive and standard feeding groups [relative risk 0.94, 95% confidence interval (CI) 0.76, 1.16, p = 0.58]. In this a priori sub-study, consecutive patients enrolled in PermiT trial at King Abdulaziz Medical City, Riyadh, Saudi Arabia between September 2012 and September 2014 and expected to stay for ≥14 days as judged by the treating intensivist were approached for informed consent for participation in this study. The study was approved by the Institutional Board Review of the Ministry of the National Guard Health Affairs, Riyadh, Saudi Arabia and all clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki.
Nutrition
The dietician calculated caloric requirement based on predefined formulae using the Penn State equation for mechanically ventilated patients with BMI <30 kg/m2 and the Ireton-Jones equation for mechanically ventilated patients with BMI ≥30 kg/m2 and for spontaneously breathing patients[6] and then selected the tube feeding formula depending on the patient condition, usually after discussion with the treating ICU team. Protein target was calculated at 1.2 to 1.5 g g/kg according to the clinical practice guidelines.[9] To achieve similar protein delivery to both feeding groups, additional protein (Resource Beneprotein, Nestle Healthcare) was provided if needed.
Clinical data
We documented demographics and nutritional intervention data and clinical outcomes including mortality (at ICU and hospital discharge, 90 days, 28 days, 180 days), incident renal replacement therapy, mechanical ventilation duration, ICU and hospital lengths of stay (LOS), and ICU-associated infections during the ICU stay.
Blood sampling and measurements of cytokines
Blood samples were collected on days 1, 3, 5, 7 and 14 of enrollment in the PermiT trial. Day 1 was the day of randomization, which was within 48 hours of ICU admission. Serum was prepared from the clotted blood samples by centrifugation for 10 minutes at 1000 x g at 4°C, then was stored at −80°C prior to assay. A total of 29 cytokines were measured in duplicates using Milliplex panel (human cytokine/chemokine magnetic bead panel, kit catalog code HCYTMAG-60K-PX29, Merck Millipore, Darmstadt, Germany) with the Luminex 3D platform (Luminex, Austin, TX), according to the manufacturer instructions. The cytokine panel included epidermal growth factor (EGF), eotaxin, granulocyte-colony stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF), interferon (IFN)-α2 and IFN-γ, interleukin (IL)-1α, IL-1β, IL-1ra, IL-2, IL-3, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12 (p40), IL-12 (p70), IL-13, IL-15, IL-17A, inducible protein-10 (IP-10), monocyte chemo-attractant protein (MCP)-1, macrophage inflammatory protein (MIP)-1α, MIP-1β, tumor necrosis factor (TNF)-α, TNF-β, and vascular endothelial growth factor (VEGF).
Statistical analysis
Due to the exploratory nature of the study, there was no sample size calculation performed. Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC). We used principal component analysis (PCA) as a data reduction technique to capture the maximum variation patterns in the 29 cytokine levels measured at day one in few linearly independent components.[10] PCA summarizes variation in data without any prior assumptions about whether the samples come from different treatment groups or have phenotypic differences, thus avoids introducing inherent bias.[10] PCA was carried out on the correlation matrix of the 29 cytokine measures at baseline using the “PRINCOMP” procedure of SAS. The analysis generated principal components with a set of eigenvalues and eigenvectors. Eigenvalues measures the magnitude of the variance captured by each principal component. We have sorted the principal components so that the first principal component accounted for the largest possible variance in the data (reflected by the highest eigenvalue), and each following component accounted for as much of the remaining variance as possible. We have retained the top 6 principal components using the scree plot method. The eigenvectors represent a set of weights that describe the loading of each cytokine on the extracted principal components.
We compared baseline characteristics, interventions and outcomes among patients in the permissive underfeeding and standard feeding. We reported categorical variables as frequencies with percentages and continuous variables as medians with quartiles 1 and 3 (Q1, Q3). We compared categorical variables using the chi-square or Fisher’s exact test, as appropriate and continuous variables using Wilcoxon Mann Whitney test. We assessed the association of permissive underfeeding compared to standard feeding with 90-day mortality and incident renal replacement therapy using logistic regression analysis adjusting for the resulting principal components. To assess whether permissive underfeeding compared to standard feeding was associated with difference cytokine levels over time, we constructed repeated measures mixed linear models. A two-tailed P value <0.05 was considered statistically significant.
Ethics approval and consent to participate
The study was approved by the National Guard Health Affairs Institutional Review Board (IRB), Riyadh, Saudi Arabia. Informed consent was obtained from subjects enrolled in this study.
Results
A total of 72 patients were enrolled in this sub-study with 36 patients receiving permissive underfeeding and 36 standard feeding (S1 Fig). Their baseline characteristics are presented in Table 1. Patients in the permissive underfeeding group received less calories per day for the study period (up to 14 days) compared with the standard feeding group as per the study criteria [911.4 kcal (789.1, 1072.5) vs. 1137.3 kcal (819.2, 1639.0), p = 0.006]. Other aspects of interventions and co-interventions are reported in Table 2. Clinical outcomes, including mortality (at ICU and hospital discharge, 90 days, 28 days, 180 days), incident renal replacement therapy, mechanical ventilation duration, ICU and hospital lengths of stay (LOS), and ICU-associated infections during the ICU stay, were not different between the two groups (Table 3).
Table 1. Baseline characteristics of patients in the permissive underfeeding and standard feeding.
| Variable | Permissive underfeeding N = 36 |
Standard feeding N = 36 |
P value |
|---|---|---|---|
| Age–(yr), median (Q1, Q3) | 46.8 (24.1, 70.4) | 53.5 (33.0, 71.3) | 0.16 |
| Female sex–no. (%) | 9 (25.0) | 12 (33.3) | 0.44 |
| Height–(cm), median (Q1, Q3) | 168 (162, 170) | 165 (155, 170) | 0.57 |
| Weight–(kg), median (Q1, Q3) | 74.5 (57.0, 86.0) | 72.5 (60.0, 95.0) | 0.39 |
| BMI–(kg/m2), median (Q1, Q3) | 26.1 (22.0, 31.2) | 29.3 (23.0, 35.7) | 0.18 |
| BMI ≥ 30 kg/m2, no. (%) | 11 (30.6) | 15 (41.7) | 0.33 |
| Diabetes, no. (%) | 19 (52.8) | 19 (52.8) | 1.00 |
| Inclusion blood glucose–(mmol/L), median (Q1, Q3) | 10.9 (8.3, 13.6) | 8.7 (6.7, 12.5) | 0.12 |
| Admission category, no. (%) | |||
| Medical | 19 (52.8) | 21 (58.3) |
0.88 |
| Surgical | 4 (11.1) | 4 (11.1) | |
| Post-operative trauma | 13 (36.1) | 11 (30.6) | |
| Renal replacement therapy, no. (%) | 1 (2.8) | 1 (2.8) | 1.00 |
| APACHE II–median (Q1, Q3) | 21 (16, 25) | 21 (12, 27) | 0.92 |
| Mechanical ventilation, no. (%) | 33 (91.7) | 35 (97.2) | 0.30 |
| Severe sepsis at admission, no. (%) | 7 (19.4) | 11 (30.6) | 0.27 |
| Vasopressor, no. (%) | 23 (63.9) | 25 (69.4) | 0.67 |
| Hemoglobin–(g/L), median (Q1, Q3) | 109 (86, 126) | 111 (97, 131) | 0.38 |
| INR–median (Q1, Q3) | 1.1 (1.0, 1.3) | 1.1 (1.0, 1.3) | 0.88 |
| SOFA Score on Day 1 –median (Q1, Q3) | 10 (9, 12) | 10 (8, 13) | 0.58 |
| PaO2/FiO2 ratio, median (Q1, Q3) | 150.0 (117.0, 269.0) | 125.5 (73.5, 242.0) | 0.44 |
| Platelets–(x 109/L), median (Q1, Q3) | 186.0 (141.5, 277.5) | 187.0 (137.5, 243.0) | 0.55 |
| Bilirubin–(μmol/L), median (Q1, Q3) | 11.7 (8.6, 26.9) | 17.1 (9.7, 27.9) | 0.30 |
| SOFA Hypotension score–median (Q1, Q3) | 3 (3, 4) | 4 (1, 4) | 0.23 |
| GCS–median (Q1, Q3) | 3 (3, 6) | 3 (3, 6) | 0.54 |
| Creatinine–(μmol/L), median (Q1, Q3) | 97.5 (73.0, 118.0) | 84.5 (67.0, 121.0) | 0.49 |
| C-reactive Protein–(mg/L), median (Q1, Q3)) | 120.5 (60.7, 190.5) | 118.1 (55.4, 171.0) | 0.77 |
| 24-hour urinary urea nitrogen–(mmol/L), median (Q1, Q3) | 205 (101, 346) | 255 (183, 371) | 0.21 |
| Serum lipid profile–(mmol/L), median (Q1, Q3) | |||
| Cholesterol | 2.5 (1.9, 3.0) | 2.6 (2.1, 3.3) | 0.36 |
| Triglycerides | 1.1 (0.7, 1.6) | 1.2 (0.9, 1.8) | 0.30 |
| HDL | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.9) | 0.76 |
| LDL | 1.0 (0.6, 1.4) | 1.2 (0.8, 1.7) | 0.23 |
| Albumin–(g/L), median (Q1, Q3) | 29 (25, 32.5) | 28 (27, 31) | 0.68 |
| Prealbumin–(g/L), median (Q1, Q3) | 0.1 (0.1, 0.1) | 0.1 (0.08, 0.1) | 0.60 |
| Hemoglobin A1c, median (Q1, Q3) | 0.06 (0.05, 0.07) | 0.06 (0.05, 0.07) | 0.87 |
| Minute ventilation–(L), median (Q1, Q3) | 9.4 (7.7, 11.3) | 8.6 (7.2, 10.7) | 0.28 |
| Maximum temperature–(0C), median (Q1, Q3) | 37.2 (36.7, 37.7) | 37.0 (36.6, 37.6) | 0.58 |
BMI: body mass index; APACHE II: Acute Physiology and Chronic Health Evaluation II; INR: international normalized ratio; SOFA: Sequential Organ Failure Assessment; GCS: Glasgow coma scale PaO2:FiO2 ratio: the ratio of partial pressure of oxygen to the fraction of inspired oxygen; HDL: High density lipoproteins; LDL: Low density lipoproteins. The denominators for all percentages is the N for each column. Continuous variables are represented as median (quartile 1 and quartile 3)
Table 2. Nutritional and metabolic data in patients in the permissive underfeeding and standard feeding.
| Variable | Permissive underfeeding N = 36 |
Standard feeding N = 36 |
P value |
|---|---|---|---|
| Calculated caloric requirement–(kcal/day), median (Q1, Q3) | 1727 (1613, 2030.5) | 1876 (1586, 2062) | 0.43 |
| Study caloric target–(kcal/day), median (Q1, Q3) | 1074 (962, 1218.5) | 1876 (1586, 2062) | <0.0001 |
| Daily caloric intake for the intervention duration– | |||
| No. of kilocalories, median (Q1, Q3) | 911.4 (789.1, 1072.5) | 1137.3 (819.2, 1639.0) | 0.006 |
| Percent of requirement, median (Q1, Q3) | 54.1 (46.7, 57.3) | 69.8 (47.4, 88.8) | 0.004 |
| Caloric source for the intervention duration–(kcal /day), median (Q1, Q3) | |||
| Enteral | 785.5 (650.0, 1022.5) | 1121.7 (731.1, 1507.9) | 0.004 |
| Propofol | 75.6 (19.1, 129.9) | 73.7 (20.1, 147.6) | 0.83 |
| Intravenous dextrose | 3.6 (0.0, 22.9) | 0.0 (0.0, 32.9) | 0.27 |
| Total parenteral nutrition | 0 (0, 0) | 0 (0, 0) | 0.33 |
| Calculated protein requirement–(g/day), median (Q1, Q3) | 78.5 (68, 90) | 83.0 (70.5, 96.5) | 0.14 |
| Daily protein intake for the intervention duration, median (Q1, Q3) | |||
| No. of grams | 55.3 (42.8, 67.1) | 53.4 (34.0, 66.5) | 0.45 |
| Percent of requirement | 72.6 (63.0, 84.0) | 63.3 (41.6, 83.3) | 0.12 |
| Daily average protein intake/kg (g/day) | 0.77 (0.66, 0.91) | 0.70 (0.40, 0.92) | 0.28 |
| Protein source–(g/day), median (Q1, Q3) | |||
| Main enteral formula | 27.0 (23.4, 37.0) | 50.6 (31.3, 64.1) | <0.0001 |
| Supplemental enteral protein | 23.4 (19.2, 34.0) | 0.0 (0.0, 1.2) | <0.0001 |
| Parenteral protein | 0 (0,0) | 0 (0, 0) | 0.33 |
| Duration of intervention–(days), median (Q1, Q3) | 11 (7, 14) | 13 (5.5, 14.0) | 0.86 |
| Co-interventions during study period | |||
| Insulin | |||
| Use–no. (%) | 21 (58.3) | 24 (66.7) | 0.47 |
| Dose–(units/day), median (Q1, Q3) | 4.6 (0.0, 29.0) | 6.7 (0.0, 31.8) | 0.53 |
| Blood glucose–(mmol/L), median (Q1, Q3) | 7.7 (6.7, 10.3) | 9.0 (6.7, 11.5) | 0.35 |
| Enteral formulae on day 1 –no. (%) | |||
| Disease-non-specific | 16 (44.4) | 15 (41.7) | 0.66 |
| Disease-specific | 20 (55.6) | 21 (58.3) |
Disease-non-specific formula: Osmolite, Jevity, Promote, Ensure plus, Resource, Ensure, Resource plus, Jevity (1.2).
Disease-specific formula: Glucerna, Nutric hepatic, Nepro, Pulmocare, Novasource Renal, Peptamen (1.0), Peptamen (1.2), Suplena, Oxepa.
Table 3. Outcome data in patients in the permissive underfeeding and standard feeding.
| Variable | Permissive underfeeding N = 36 |
Standard feeding N = 36 |
P value |
|---|---|---|---|
| Death by 28 days–no. (%) | 5 (13.9) | 4 (11.1) | 0.92 |
| Death by 90 days–no. (%) | 7 (19.4) | 5 (13.9) | 0.53 |
| Death by 180 days–no. (%) | 7 (19.4) | 7 (19.4) | 1.00 |
| Death in the ICU–no. (%) | 4 (11.1) | 3 (8.3) | 0.69 |
| Death in the hospital–no. (%) | 5 (13.9) | 5 (13.9) | 1.00 |
| New renal replacement therapy–no. (%) | 3 (6.1) | 9 (25.7) | 0.06 |
| ICU-associated infections–no. (%) | 19 (52.8) | 19 (52.8) | 1.00 |
| ICU length of stay–(days), median (Q1, Q3) | 16 (10, 21) | 15 (10, 21) | 0.76 |
| Hospital length of stay–(days), median (Q1, Q3) | 33 (17, 72) | 40 (22, 86) | 0.23 |
| Duration of mechanical ventilation–(days), median (Q1, Q3) | 10 (7, 16) | 11 (5, 17) | 0.93 |
ICU: intensive care unit
Principal component analysis
PCA reduced the original 29 cytokines to 6 components that could explain 78% of the total variance. The principal component 1 explained 42% of the total variance, while the other principal components 2–6 were responsible for 12%, 10%, 6%, 4% and 4% respectively (S1 Table). S2 Table represents the loading of each of the 29 cytokines on the retained 6 principal components. GM-CSF, IFN-α2, IL-1β, IL-2, IL-3, IL-4, IL-7, IL-12 (p40), IL-12 (p70), IL-13, IL-15, IL-17A,TNF-α and TNF-β had a loading weight value greater than 0.2 on the principal component 1.
Association of permissive underfeeding with outcomes adjusting for baseline cytokine principal components
When adjusted to principal components, permissive underfeeding was not associated with 90-day mortality (adjusted odds ratio (aOR) 1.97, 95% CI 0.47, 7.89, p = 0.34) or with incident renal replacement therapy (aOR 0.36, 95% CI 0.07, 1.96, p = 0.24, Table 4). None of the principal components were generally associated with 90-day mortality or incident renal replacement therapy.
Table 4. The association of permissive underfeeding compared to standard feeding with 90-day mortality and incident renal replacement therapy adjusted for the principal components of the cytokines.
| 90-day mortality | Incident renal replacement therapy | |||
|---|---|---|---|---|
| aOR (95% CI) | P value | aOR (95% CI) | P value | |
| Permissive underfeeding vs Standard feeding | 1.75 (0.44–6.95) | 0.43 | 0.25 (0.04–1.45) | 0.12 |
| Principal component 1 | 1.07 (0.87–1.31) | 0.52 | 4.82 (0.91–25.69) | 0.07 |
| Principal component 2 | 1.14 (0.85–1.53) | 0.39 | 0.71 (0.37–1.37) | 0.31 |
| Principal component 3 | 1.35 (0.84–2.18) | 0.22 | 2.37 (0.43–12.95) | 0.32 |
| Principal component 4 | 1.14 (0.72–1.82) | 0.58 | 1.02 (0.61–1.72) | 0.93 |
| Principal component 5 | 0.76 (0.43–1.33) | 0.33 | 0.70 (0.41–1.22) | 0.21 |
| Principal component 6 | 1.17 (0.62–2.23) | 0.63 | 3.08 (1.26–7.50) | 0.01 |
aOR: adjusted odds ratio, CI: confidence interval
Effect of permissive underfeeding on cytokine levels over time
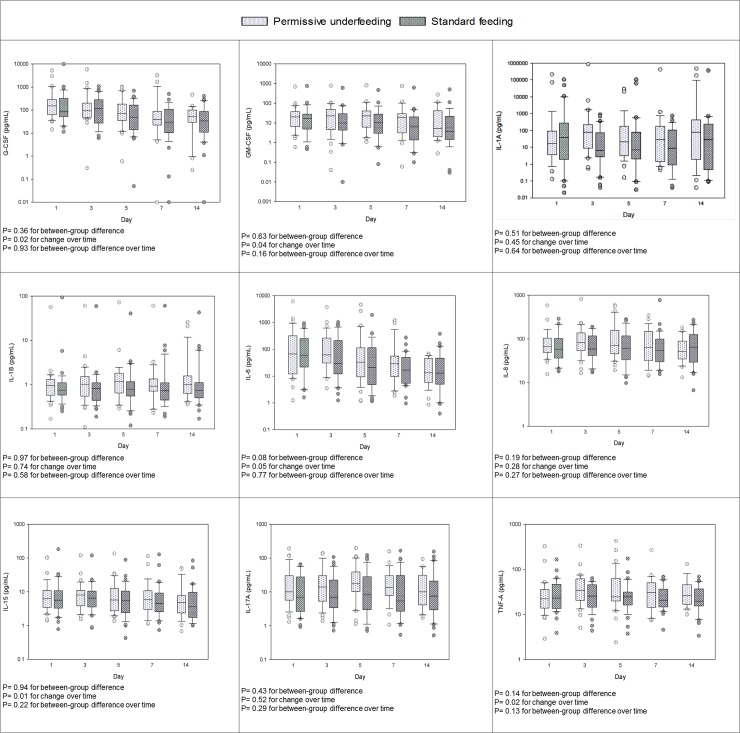
There was no difference in any of the cytokine levels over time between the permissive underfeeding and standard feeding (Fig 1 and S2 Fig).
Fig 1. Serial measurements for selected acute pro-inflammatory cytokines in patients randomized to permissive underfeeding and standard feeding groups.
The differences between groups, with time and between groups with time (group*time) were tested by repeated measures mixed linear models. Box plots are displayed with medians and quartiles 1 and 3. The error bars refer to 10th and 90th percentiles.
Discussion
Our study showed that the association of permissive underfeeding compared to standard feeding (with similar protein intake provided) with mortality and incident renal replacement therapy was not influenced by the inflammatory profile. Cytokine components were not associated with outcomes. Permissive underfeeding compared to standard feeding (with similar protein intake provided) was not associated with any major differences in the inflammatory response in critically ill patients.
Caloric restriction has been associated with increased life span and protection against diabetes, cardiovascular disease and cancer in animals and non-critically ill humans.[11] There is accumulating evidence that caloric restriction may modulate inflammatory response in these settings. A review of the published data suggests that caloric restriction may protect against aging of the immune system, maintain naive T cells, and modify the host response to infection.[12] A randomized controlled trial in 316 older obese adults showed that diet induced weight-loss led to significant reduction in C-reactive protein (CRP), IL-6, and soluble TNF-α receptor 1.[2] A study evaluated a 15-week lifestyle intervention (hypocaloric diet and daily exercise) in 27 severely obese patients and found that the intervention was associated with significant decrease in IL-6, IL-8, and TNF-α.[13] In a pre-post study, 8-week hypocaloric diet in 41 obese subjects led to reduction in CRP, complement C3 and TNF-α levels compared to baseline.[14]
In animal models of critical illness, caloric intake has been shown to influence the inflammatory response. Mice subjected to 40% energy-restriction for 4 weeks, showed less elevation of IL-1β, IL-6 and TNF-α after lipopolysaccharide injection compared with mice in the control group.[4] In another prospective controlled laboratory experiment in mice, 40% dietary restriction for 3 weeks followed by induction of abdominal sepsis or endotoxemia was associated with significantly reduced visceral fat-derived messenger RNA expression of IL-6, thrombospondin-1, plasminogen activator inhibitor-1, and tissue factor and of serum IL-6 and with improved survival.[5]
In critically ill patients, enteral nutrition (EN) may modulate inflammation through several potential mechanisms including affecting the gastrointestinal microbiome,[15] maintaining the intestinal mucosal barrier function[16] and restoring gut immunity.[17] However, the effect of EN on cytokines has not been universally demonstrated. A randomized controlled trial of EN versus parenteral nutrition in 50 patients with severe pancreatitis showed that EN was not associated with changes in IL-6, IL-8 or CRP.[18] A study randomized 20 ICU patients to either receive EN alone or similar EN feeding with supplemental parenteral nutrition to increase caloric intake for 7 days and found that IL-1, IL-6 and TNF-α measured on days of 0, 3 and 7 did not differ between the two groups.[19]
Data on the effect of caloric intake on cytokines in critically ill patients are scarce. In 103 mechanically ventilated patients, markers of inflammation (TNF-α, IL-1β, IFN-γ, IL-6, IL-8, IL-10, IL-12) were not different at day 6 between patients who were randomized to receive trophic feeds (15±11% of target calories) compared to the full calorie group (75 ±39%).[20, 21] The current study was similar in that both used EN with standard non-immune enhancing formulae. However, it differed in that caloric restriction in our study was moderate but more prolonged (up to 14 days versus up to 6 days) and supplemental protein was provided to the patients in the permissive underfeeding group, so the restriction involved only calories.[6, 20, 21] Nevertheless, the two studies showed no major difference in cytokines with caloric restriction. In addition, our study shows that the association of caloric intake with clinical outcomes was not different even after accounting for cytokine profiles.
Why the effects of caloric restriction on cytokines in obesity and in animal models were not observed in critically ill patients in our study? There may be multiple reasons. First, the population was different: our patients were severely ill with a mean APACHE II score of 21.2±10.1, 68 (94.4%) ventilated and 48 (66.7%) on vasopressors, so data on patients who are less severely ill may not be generalizable to ICU patients. Second, the inflammatory response during critical illness is different from that observed in chronic conditions like obesity: our patients had a predominantly acute pro-inflammatory profile, characteristic of critical illness and may correlate with evolution of acute organ dysfunction.[22–26] This was observed in our study by the predominance of pro-inflammatory cytokines loading on principal component 1. Furthermore in mice the plasma levels of IL-6 were significantly reduced by dietary restriction and correlated with adipose IL-6 messenger RNA levels and fat mass suggesting that the action of dietary restriction on suppressing IL-6 production was mediated by its effect on resident adipose cells.[5] Whether similar effect on adipose cells occurs with moderate short-term caloric restriction, like in our trial, remains unknown. Third, the intensity of the intervention is different: caloric differences in our study were less intense and were for shorter period (14 days) than in many other studies in non-critically ill patients or in animal models. Unlike what has been achieved in animal models but similar to other randomized clinical controlled trials of normocaloric versus hypocaloric enteral nutrition, the permissive underfeeding feeding in our study was not very hypocaloric and the standard feeding did not achieve full caloric target.[27, 28] Although we achieved a significant difference in caloric intake between the two groups, the target caloric intake was not reached in the standard- group, and as such, the differences in caloric intake were moderate. This was most likely due to feeding intolerance and feeding interruptions which are common in critically ill patients. This may have reduced the chance of identifying an effect on cytokine levels. Feeding at 100% or more of the energy target during the acute phase of critical illness may be harmful compared to lower caloric levels that are comparable to what we achieved in both study arms.[29–31] Therefore, the results may not be generalizable to patients being fed at full energy target; and our findings cannot exclude that full feeding during the acute phase of critical illness may elicit an inflammatory response. Fourth, the timing of the intervention is different: in animal studies, animals were “pre-conditioned” with several weeks of caloric restriction before inducing critical illness, while in critically ill patients the nutritional interventions follow the critical illness. Fifth, we provided similar protein intake to both groups. There is accumulating evidence suggesting that meeting protein goals and not caloric goals is associated with improved outcomes.[31–34] Therefore, it is possible that an effect of caloric restriction on cytokines in our study might have been “masked” by different effects of protein. Sixth, given the results of the recent NUTRIREA-2 trial, one may question whether a potential beneficial effect of EN on reducing inflammatory response might have been masked by an effect of EN triggering subclinical intestinal ischemia (resulting in increased cytokine levels) in patients with hemodynamic failure, who constituted two thirds of the study population. In the NUTRIREA-2 trial, ventilated patients who were in shock were randomized to receive early EN or early parenteral nutrition within 24 hours after endotracheal intubation aiming to achieve nutritional goals on day 1.[35] The study found no difference in the primary endpoint of all-cause mortality at 28 days. However, early EN was associated with a 4-fold increase in ischemic bowel and colonic pseudo-obstruction.[35] Sixth, the large variation of cytokine levels in critically ill patients, which is reflected in the wide interquartile ranges for all cytokines might have precluded detecting differences in cytokines with the current sample size. Seventh, circulating cytokines may not reflect local inflammatory processes. For example, extracorporeal blood purification therapies in septic patients have been shown to be effective in clearing inflammatory mediators from the plasma, but there effect on mortality has not been demonstrated.[36] Finally, nutrition might also influence the inflammatory response by modulating autophagy, a pathway that may not be reflected in cytokine profiles.[37]
The study should be interpreted in the light of its strengths and weaknesses. The strengths include that it was sub-study of a randomized controlled trial; therefore, the assignment to permissive and standard feeding was randomized. We tested for 29 cytokines to obtain a comprehensive picture about the inflammatory response. Serial serum samples at 5 time points were obtained. We used PCA as a data reduction technique, so the variance from all 29 cytokines can be accounted for in the multivariate analysis. The study limitations include being single centered study. Because of the large variability in cytokines and the sample size, the study may have been underpowered to detect differences in cytokine levels. Additionally, the differences in calories achieved in the clinical setting of the trial were moderate and it remains unclear whether more profound differences would affect cytokines. The study was also not sufficiently powered to perform subgroup analyses.
Conclusion
In conclusion, the association of permissive underfeeding compared to standard feeding (with similar protein intake provided) with mortality was not influenced by the inflammatory profile. Permissive underfeeding compared to standard feeding was not associated with differences in the serum levels of cytokines in critically ill patients. Whether delivering more restricted caloric intake (lower than what we have achieved in the permissive underfeeding group) reduces inflammatory response or alternatively whether delivering full caloric intake (higher than what we have achieved in the standard feeding group) elicits an inflammatory response with or without full protein supplementation remains to be studied.
Supporting information
(DOCX)
The differences between groups, with time and between groups with time (group*time) were tested by repeated measures mixed linear models. Box plots are displayed with medians and quartiles 1 and 3. The error bars refer to10th and 90th percentiles.
(DOCX)
(DOCX)
(DOCX)
Excel sheet with data related to the baseline characteristic Table 1, nutritional data Table 2, outcome data Table 3 and data related to the Fig 1.
(XLSX)
Acknowledgments
We wish to thank the following coordinators who made valuable suggestions or who have otherwise contributed to study: Turki Almoammar, Muhammad Rafique Sohail, Shihab Mundekkadan and Aron Toledo.
Abbreviations
- PCA
Principal component analysis
- ICU
Intensive care unit
- AOR
Adjusted odds ratio
- EN
Enteral nutrition
- APACHE II
Acute Physiology and Chronic Health Evaluation
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The study was funded from King Abdulaziz City for Science and Technology (KACST), Riyadh, Saudi Arabia under Grant Number - AT 32-25 KACST to Y.A. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, et al. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA. 2003;289(14):1799–804. Epub 2003/04/10. 10.1001/jama.289.14.1799 289/14/1799 [pii]. . [DOI] [PubMed] [Google Scholar]
- 2.Nicklas BJ, Ambrosius W, Messier SP, Miller GD, Penninx BW, Loeser RF, et al. Diet-induced weight loss, exercise, and chronic inflammation in older, obese adults: a randomized controlled clinical trial. Am J Clin Nutr. 2004;79(4):544–51. Epub 2004/03/31. 10.1093/ajcn/79.4.544 . [DOI] [PubMed] [Google Scholar]
- 3.Moller K, Ostermann AI, Rund K, Thoms S, Blume C, Stahl F, et al. Influence of weight reduction on blood levels of C-reactive protein, tumor necrosis factor-alpha, interleukin-6, and oxylipins in obese subjects. Prostaglandins Leukot Essent Fatty Acids. 2016;106:39–49. 10.1016/j.plefa.2015.12.001 . [DOI] [PubMed] [Google Scholar]
- 4.Matsuzaki J, Kuwamura M, Yamaji R, Inui H, Nakano Y. Inflammatory responses to lipopolysaccharide are suppressed in 40% energy-restricted mice. J Nutr. 2001;131(8):2139–44. 10.1093/jn/131.8.2139 . [DOI] [PubMed] [Google Scholar]
- 5.Starr ME, Steele AM, Cohen DA, Saito H. Short-Term Dietary Restriction Rescues Mice From Lethal Abdominal Sepsis and Endotoxemia and Reduces the Inflammatory/Coagulant Potential of Adipose Tissue. Crit Care Med. 2016;44(7):e509–19. 10.1097/CCM.0000000000001475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arabi YM, Aldawood AS, Haddad SH, Al-Dorzi HM, Tamim HM, Jones G, et al. Permissive Underfeeding or Standard Enteral Feeding in Critically Ill Adults. N Engl J Med. 2015;372(25):2398–408. 10.1056/NEJMoa1502826 . [DOI] [PubMed] [Google Scholar]
- 7.Arabi YM, Jawdat D, Aldawood AS, Tamim HM, Tamimi W, Al-Balwi M, Al Dorzi HM, Al-Qahtani S, Sadat M, Afesh L, Al Dlamy M, Mashaqbeh W, Sakhija M, Elobeid A, Al-Abdulkareem I, Toledo AC, Sohail MR, Almoammar T, Bouchama A. The Effect of Permissive Underfeeding Compared to Standard Feeding on the Inflammatory Response. Am J Res Crit Care Med 2017;195:A7132. [Google Scholar]
- 8.Arabi YM, Haddad SH, Aldawood AS, Al-Dorzi HM, Tamim HM, Sakkijha M, et al. Permissive underfeeding versus target enteral feeding in adult critically ill patients (PermiT Trial): a study protocol of a multicenter randomized controlled trial. Trials. 2012;13:191 10.1186/1745-6215-13-191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Dietetic Association. Nutritional Assessments of Adults. Manual of Clinical Dietetics. Sixth Edition. 2000;pp 1–66.
- 10.Lever J, Krzywinski M, Altman N. Principal component analysis. Nature Methods. 2017;14:641 10.1038/nmeth.4346 [DOI] [Google Scholar]
- 11.Fontana L, Partridge L, Longo VD. Extending healthy life span—from yeast to humans. science. 2010;328(5976):321–6. 10.1126/science.1172539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nikolich-Žugich J, Messaoudi I. Mice and flies and monkeys too: caloric restriction rejuvenates the aging immune system of non-human primates. Experimental gerontology. 2005;40(11):884–93. 10.1016/j.exger.2005.06.007 [DOI] [PubMed] [Google Scholar]
- 13.Bruun JM, Helge JW, Richelsen B, Stallknecht B. Diet and exercise reduce low-grade inflammation and macrophage infiltration in adipose tissue but not in skeletal muscle in severely obese subjects. American Journal of Physiology-Endocrinology and Metabolism. 2006;290(5):E961–E7. 10.1152/ajpendo.00506.2005 [DOI] [PubMed] [Google Scholar]
- 14.Hermsdorff HH, Zulet MA, Abete I, Martinez JA. Discriminated benefits of a Mediterranean dietary pattern within a hypocaloric diet program on plasma RBP4 concentrations and other inflammatory markers in obese subjects. Endocrine. 2009;36(3):445–51. 10.1007/s12020-009-9248-1 . [DOI] [PubMed] [Google Scholar]
- 15.Smith AR, Macfarlane S, Furrie E, Ahmed S, Bahrami B, Reynolds N, et al. Microbiological and immunological effects of enteral feeding on the upper gastrointestinal tract. J Med Microbiol. 2011;60(Pt 3):359–65. 10.1099/jmm.0.026401-0 . [DOI] [PubMed] [Google Scholar]
- 16.Guzy C, Schirbel A, Paclik D, Wiedenmann B, Dignass A, Sturm A. Enteral and parenteral nutrition distinctively modulate intestinal permeability and T cell function in vitro. Eur J Nutr. 2009;48(1):12–21. 10.1007/s00394-008-0754-3 . [DOI] [PubMed] [Google Scholar]
- 17.Goldberg RF, Austen WG Jr., Zhang X, Munene G, Mostafa G, Biswas S, et al. Intestinal alkaline phosphatase is a gut mucosal defense factor maintained by enteral nutrition. Proc Natl Acad Sci U S A. 2008;105(9):3551–6. 10.1073/pnas.0712140105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eckerwall GE, Axelsson JB, Andersson RG. Early nasogastric feeding in predicted severe acute pancreatitis: A clinical, randomized study. Ann Surg. 2006;244(6):959–65; discussion 65–7. 10.1097/01.sla.0000246866.01930.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abrishami R, Ahmadi A, Abdollahi M, Moosivand A, Khalili H, Najafi A, et al. Comparison the inflammatory effects of early supplemental parenteral nutrition plus enteral nutrition versus enteral nutrition alone in critically ill patients. Daru. 2010;18(2):103–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Bastarache JA, Ware LB, Girard TD, Wheeler AP, Rice TW. Markers of inflammation and coagulation may be modulated by enteral feeding strategy. JPEN J Parenter Enteral Nutr. 2012;36(6):732–40. 10.1177/0148607111433054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rice TW, Mogan S, Hays MA, Bernard GR, Jensen GL, Wheeler AP. Randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit Care Med. 2011;39(5):967–74. 10.1097/CCM.0b013e31820a905a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bozza FA, Salluh JI, Japiassu AM, Soares M, Assis EF, Gomes RN, et al. Cytokine profiles as markers of disease severity in sepsis: a multiplex analysis. Critical care. 2007;11(2):R49 10.1186/cc5783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fjell CD, Thair S, Hsu JL, Walley KR, Russell JA, Boyd J. Cytokines and signaling molecules predict clinical outcomes in sepsis. PLoS One. 2013;8(11):e79207 10.1371/journal.pone.0079207 ; PubMed Central PMCID: PMCPMC3828333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pene F, Vincent JL, Martin-Loeches I. On the verge of using an immune toolbox in the intensive care unit? Intensive Care Med. 2017;43(8):1154–6. 10.1007/s00134-017-4840-y . [DOI] [PubMed] [Google Scholar]
- 25.Darmon M, Bagshaw SM, Forni LG. Balancing the "humors" in severe sepsis: still a role for extracorporeal therapies? Intensive Care Med. 2015;41(6):1132–4. 10.1007/s00134-015-3801-6 . [DOI] [PubMed] [Google Scholar]
- 26.Blanch L, Quintel M. Lung-brain cross talk in the critically ill. Intensive Care Med. 2017;43(4):557–9. 10.1007/s00134-016-4583-1 . [DOI] [PubMed] [Google Scholar]
- 27.Marik PE, Hooper MH. Normocaloric versus hypocaloric feeding on the outcomes of ICU patients: a systematic review and meta-analysis. Intensive Care Med. 2016;42(3):316–23. 10.1007/s00134-015-4131-4 . [DOI] [PubMed] [Google Scholar]
- 28.Allingstrup MJ, Kondrup J, Wiis J, Claudius C, Pedersen UG, Hein-Rasmussen R, et al. Early goal-directed nutrition versus standard of care in adult intensive care patients: the single-centre, randomised, outcome assessor-blinded EAT-ICU trial. Intensive Care Med. 2017;43(11):1637–47. 10.1007/s00134-017-4880-3 . [DOI] [PubMed] [Google Scholar]
- 29.Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care. 2016;20(1):367 10.1186/s13054-016-1538-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casaer MP, Reignier J, Doig G. Optimal guidance for early nutrition therapy in critical illness? Intensive Care Med. 2017;43(11):1720–2. 10.1007/s00134-017-4881-2 . [DOI] [PubMed] [Google Scholar]
- 31.Weijs PJ, Looijaard WG, Beishuizen A, Girbes AR, Oudemans-van Straaten HM. Early high protein intake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients. Crit Care. 2014;18(6):701 10.1186/s13054-014-0701-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicolo M, Heyland DK, Chittams J, Sammarco T, Compher C. Clinical Outcomes Related to Protein Delivery in a Critically Ill Population: A Multicenter, Multinational Observation Study. JPEN J Parenter Enteral Nutr. 2016;40(1):45–51. 10.1177/0148607115583675 . [DOI] [PubMed] [Google Scholar]
- 33.Rugeles SJ, Rueda JD, Diaz CE, Rosselli D. Hyperproteic hypocaloric enteral nutrition in the critically ill patient: A randomized controlled clinical trial. Indian J Crit Care Med. 2013;17(6):343–9. 10.4103/0972-5229.123438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arabi YM, Casaer MP, Chapman M, Heyland DK, Ichai C, Marik PE, et al. The intensive care medicine research agenda in nutrition and metabolism. Intensive Care Med. 2017. 10.1007/s00134-017-4711-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reignier J, Boisrame-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, Anguel N, et al. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet. 2018;391(10116):133–43. 10.1016/S0140-6736(17)32146-3 . [DOI] [PubMed] [Google Scholar]
- 36.Rimmele T, Kellum JA. Clinical review: blood purification for sepsis. Crit Care. 2011;15(1):205 Epub 2011/03/05. 10.1186/cc9411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Dyck L, Casaer MP, Gunst J. Autophagy and Its Implications Against Early Full Nutrition Support in Critical Illness. Nutrition in clinical practice: official publication of the American Society for Parenteral and Enteral Nutrition. 2018. 10.1002/ncp.10084 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
The differences between groups, with time and between groups with time (group*time) were tested by repeated measures mixed linear models. Box plots are displayed with medians and quartiles 1 and 3. The error bars refer to10th and 90th percentiles.
(DOCX)
(DOCX)
(DOCX)
Excel sheet with data related to the baseline characteristic Table 1, nutritional data Table 2, outcome data Table 3 and data related to the Fig 1.
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.