Abstract
Background:
Constrained acetabular components have been used to treat hips that experience recurrent or intra-operative instability after a total hip replacement. We previously reported the results of cementing tripolar constrained acetabular liners into secure, well-positioned acetabular shells in patients with preoperative or intraoperative hip instability at an average 3.9 years of follow-up. In this study, we report the results at an average of 15.4 years of follow-up to determine the long-term durability of the construct.
Methods:
Between 1988 and 2000, thirty-one constrained liners were cemented into well-fixed acetabular shells at three institutions. The average age at the time of the surgery was 72.1 years. The indications for the procedure were recurrent hip instability in 16 hips and intraoperative instability in 15 hips. Patients were evaluated for failure of the device and need for revision. There were 8 patients alive at the time of final follow-up and the average age was 78.2 years (48-102).
Results:
In addition to the two acetabular liners revised and the one removed for infection at the 3.9 year follow-up study, one additional liner was revised for loosening bringing the total revisions for failure to 3/31 (9.7%) and one was incidentally revised at the time of revision for femoral loosening. Thus, total revisions for any reason were 5/31 (16.1%).
Conclusion:
At an average of 15.4 years of follow-up, considering the complexity of cases, the durability of the construct was excellent.
Background
Previously, we reported the results of a retrospective analysis of cementing thirty-one tripolar constrained liners (Osteonics, Allendale, New Jersey) (Fig. 1) into thirty patients undergoing total hip arthroplasty.1 All hips had well-secured acetabular shells and either recurrent instability or intraoperative instability. Patients were followed clinically for a mean of 3.9 years (2-12.7 years) at which time two implants had been revised and one had been removed for infection. The operations were performed by three surgeons (JJC, RCJ, DGL) at three different institutions. The purpose of this current analysis is to present an additional eleven years of follow-up to determine the long-term durability of the construct.
Figure 1.

The constrained tripolar liner (Osteonics, Allendale, New Jersey).
Methods
Between December 1, 1988 and October 30, 2000, patients were identified at the University of Iowa Hospitals and Clinics (Iowa City, IA), Iowa Methodist Medical Center (Des Moines, IA), and Mayo Clinic (Rochester, MN) that were undergoing revision hip arthroplasty and a tripolar constrained liner was cemented into a well-fixed and well-positioned acetabular shell. Thirty patients were identified and 31 liners were inserted (one patient had a bilateral procedure). There were 15 women and 15 men with an average age of 72.1 years at the time of the index procedure. The data was then collected prospectively at all three institutions. At the time of the previous follow-up, 26 patients (27 hips) were being followed, 4 patients (4 hips) died by the time of the follow-up, and none were lost to follow-up. Since the last follow-up, 17 additional patients (17 hips) have died for a total of 21 patients (21 hips) deceased. At this present follow-up, there was 1 patient (1 hip) who had been lost to follow-up since the last study. Eight patients (9 hips) are living. The average age of the living patients at the time of index surgery was 62.8 years (31-86 years). The living patients were followed for an average of 15.4 years (8.2-17 years). The patients who are deceased were followed for an average 8.7 years (0.3-23.75 years).
For the index procedure, the surgical approaches were anterolateral (17 hips), posterolateral (12 hips), transtrochanteric (2 hips). In all cases a tripolar constrained liner was cemented into a secure acetabular shell. The shells were Harris-Galante-I components (Zimmer) in 14 hips, Trilogy prostheses (Zimmer) in 7 hips, Harris-Galante-II components (Zimmer) in 5 hips, PSL cups (Osteonics) in 3 hips, a PCA prosthesis (Howmedica) in 1 hip, and a Duraloc TriSpike shell (DePuy) in 1 hip. The average size of shells was 58 mm in diameter (52-80 mm).
To allow for an adequate cement mantle, the liners were 2 to 4 mm smaller than the retained shell. This allowed the liner to be seated in the shell without leaving it proud. The Osteonics constrained liner with an outer diameter of 50 to 56 mm can only accommodate a 22 mm femoral head. If the diameter was ≥56 mm, a fixed or modular head with a diameter of 28 mm was used. When the metal capturing ring could be removed from the liner, the groove was used for cement interdigitation at the periphery of the liner. We also scored the polyethylene in a spiderweb pattern to a depth of 1 to 2 mm. This was performed in all but the first 5 hips. This added more lever-out and torsional strength to the cement liner construct .2 The shell was also scored in this pattern if it didn’t have any screw holes. The cement was then pressurized into the shell and the liner was placed when the cement was still in its doughy state. If the acetabular shell was fixed in 50° abduction, the extended lip of the liner was placed laterally. If the shell was in neutral version, the extended lip was placed posteriorly. Antibiotic powder was only used in 11 hips and at the discretion of the treating surgeon. The other 20 hips did not use antibiotics.
Acetabular and femoral components were also evaluated for position and stability during the index procedure. The orientation of the acetabular shell was adequate in all hips (between 35° and 50° of abduction and 0° to 15° of anteversion). The stability was tested by moving the hip in all directions. We used a constrained liner if the instability occurred in the functional range of motion (flexion of 90°, adduction of 20°, abduction of 30°, and rotation of 15°). In 16 hips, the constrained liner was used due to recurrent instability (three hips had no functioning abductor muscles) and the other 15 hips were due to instability during surgery (nine of which did not have functioning abductor muscles). The patients had an average of 2.7 previous hip operations (1-7 operations).
Ten femoral components were found to be loose or malpositioned and were revised during the index surgery. Other procedures included a femoral head exchange (22 hips), trochanteric advancement (3 hips), and acetabular cancellous bone-grafting (2 hips).
Due to the advanced age of the population at the time of surgery (72 years), as stated, only 8 patients (9 hips) were living at the time of final follow-up. Thus, hip scores were not calculated for the patients. The emphasis of this report will be to evaluate for further failures of the construct at long term follow-up.
Survivorship Analysis
Kaplan-Meier survivorship3 analysis was performed with two end points: (1) revision because of mechanical failure of the device or dislocation and (2) revision for any reason.
Results
Revisions
Since the last follow-up, one more hip has been revised due to mechanical failure for a total of 3 failures (3/31, 9.7%) and one was incidentally revised during revision of the femoral stem (back to a non-constrained device). The constrained construct was stable without mechanical failure at the time of that revision.
Two revisions due to failure of the constrained liner construct were previously described (one for loosening in the case of a liner that was cemented proud and one for loosening of the liner at the time of a patient’s grand mal seizure).1 Since the previous report, one additional revision occurred at an outside institution due to recurrent dislocation of the bipolar out of the tripolar locking mechanism. At the time of revision, a new constrained liner was cemented into the shell and a new head was placed on the stem. This patient has had no further revisions.
At the time of the previous follow-up, one additional hip underwent revision due to infection. This patient had a history of multiple right hip replacements for recurrent dislocation. During her last revision surgery (the index procedure), a cemented constrained liner was placed in the hip, which proceeded to become infected. Approximately eight months after the index procedure, the hip was converted to a resection arthroplasty. Since the previous follow-up, one other hip had undergone a revision for reasons other than acetabular construct failure. The patient had a loose femoral stem which was revised approximately three years after the index procedure. In addition to a loose stem, the patient also had a retrograde nail for a supracondylar fracture. The nail and stem were removed and both hip and knee were revised in the same procedure. The cemented constrained liner was intact at the time of revision, but was converted to a non-constrained device. This brings the total number of revisions due to any reason to 5/31 (16.1%).
Complications
There were no other complications at the time of the previous follow-up. In the time since the earlier follow-up, there have been two complications. One patient was found to have broken the constraining ring of the constrained liner. It is unclear when this was broken, but the patient never had a dislocation and was never revised before passing away. The other patient had debonding of the cement from the shell without the component position changing on final radiographs. The constrained liner has not dissociated and has not been revised.
Survivorship Analysis
Figures 2A and 2B are Kaplan-Meier survivorship curves. At 15 years, survivorship (95% confidence intervals) for the end point of revision due to mechanical failure and dislocation was 90% (74.6,97.8). For the endpoint of revision for any reason, survivorship was 82.2% (66,93.9).
Figure 2A and B.
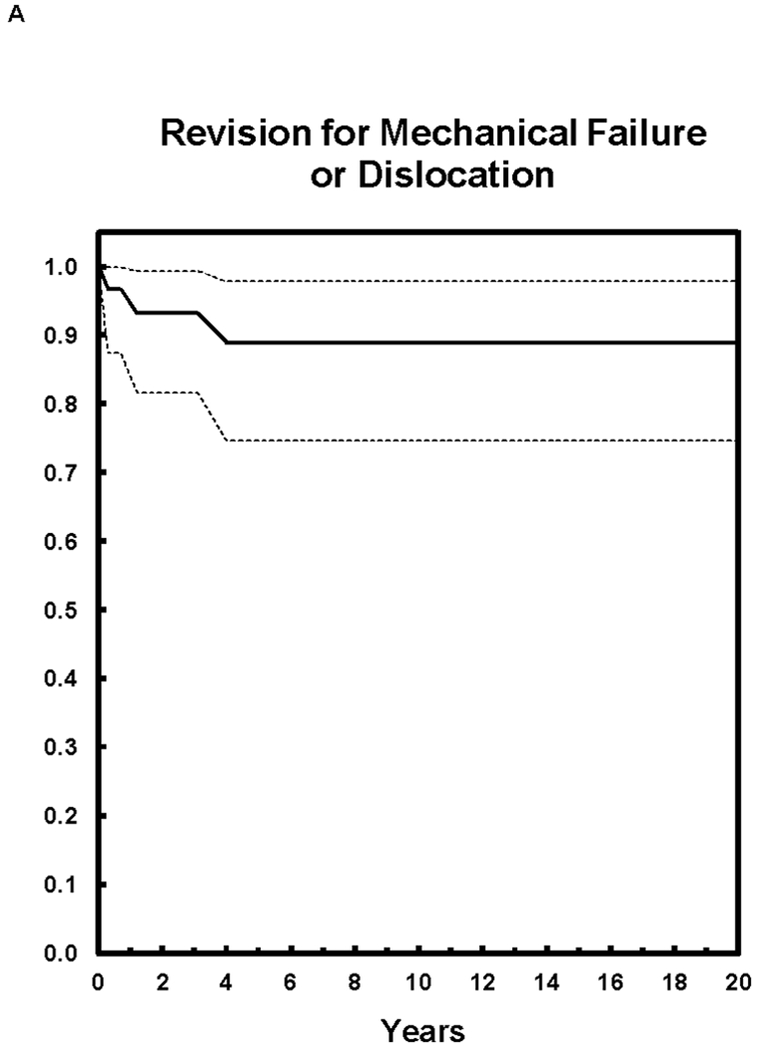
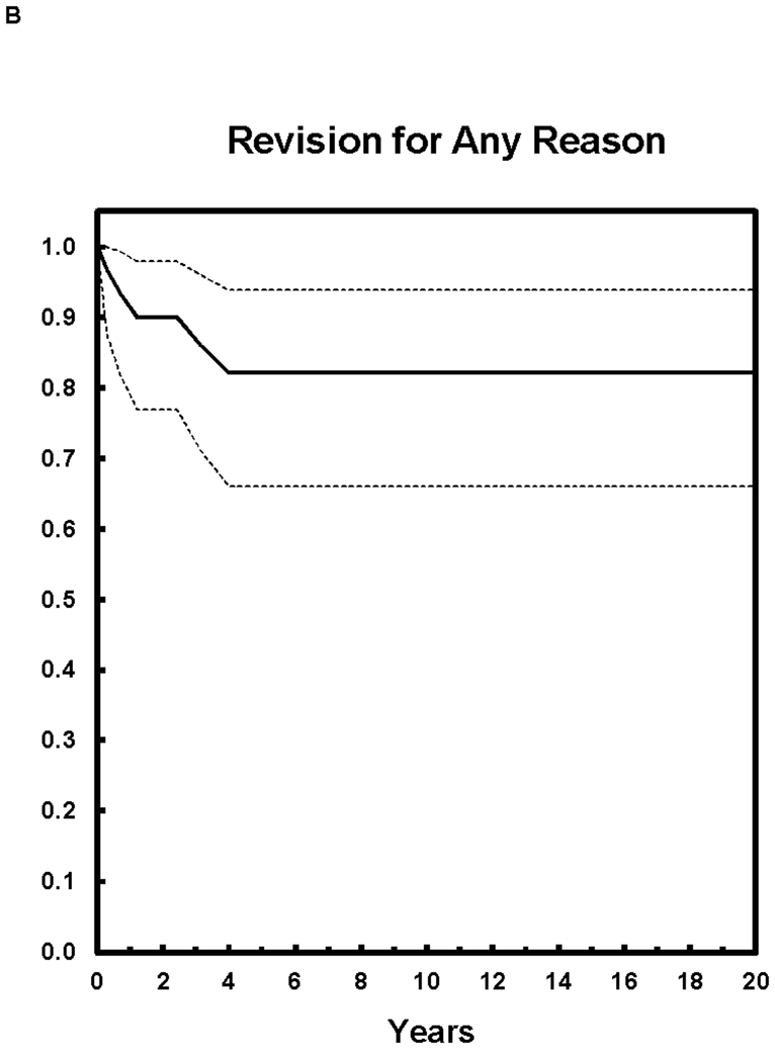
Kaplan-Meier survivorship curves with 95% confidence intervals with the end point of revision for mechanical failure and dislocation (A) and for the end point of revision for any reason (B).
Conclusions
At the time of our reporting the preliminary results of cementing constrained tripolar liners into secure well positioned acetabular shells, there was concern regarding the long term durability of the procedure. Between that initial 3.9 year average follow up and the present 15.4 year average follow up, there has only been one additional acetabular construct failure in addition to the two previously reported (9.7% total, 3 of 31). There has been one additional revision surgery (for femoral loosening) unrelated to the acetabular component, hence including the revision for infection from the previous follow up, there have only been 2 additional surgeries (for a total of 5 of 31 components revised at 15.4 years, 16.1%). Although 21 patients have died and only 8 are living, the decision to use this construct was based on the fact that these were low demand patients that would not require prolonged use (20 plus years) of this device with their relatively limited life expectancies, as the average age of surgery was 72 years. Many patients in this age group who undergo revision are just the group at high risk for dislocation with poor musculature, increased laxity, and balance and cognitive issues. These results compare favorably to the study of revision for instability by Jo et al at 15 year follow up.4 Those authors reported 34.5% re-dislocation and 45.9% re-revision at 15 years. In our study, as stated the average age of the patient at the time of revision was 72 years and most had a relatively low level of activity. The authors still prefer to use this technique more often in relatively low demand patients. The authors also continue to use the same constrained tripolar device utilized in this study. This study should support the intermediate term durability of a cemented tripolar constrained liner into a well-fixed, adequately positioned cementless acetabular shell construct especially in low demand patients (Figure 3). Our data supports continued consideration of this surgical option at the time of revision surgery in patients with recurrent dislocation or intra-operative instability in the low demand patient.
Figure 3A through C.
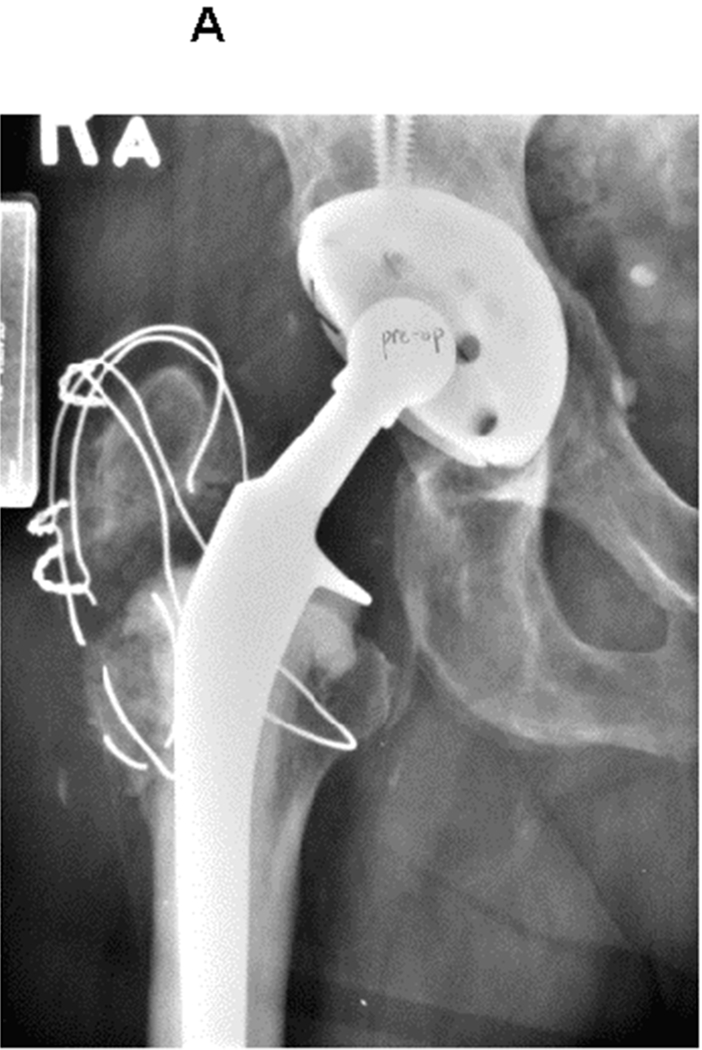
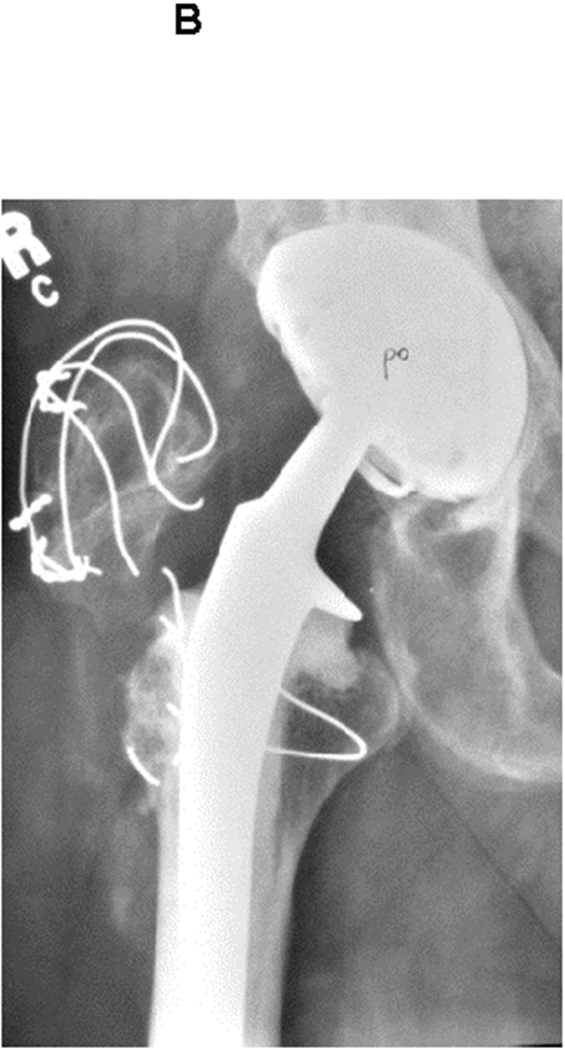
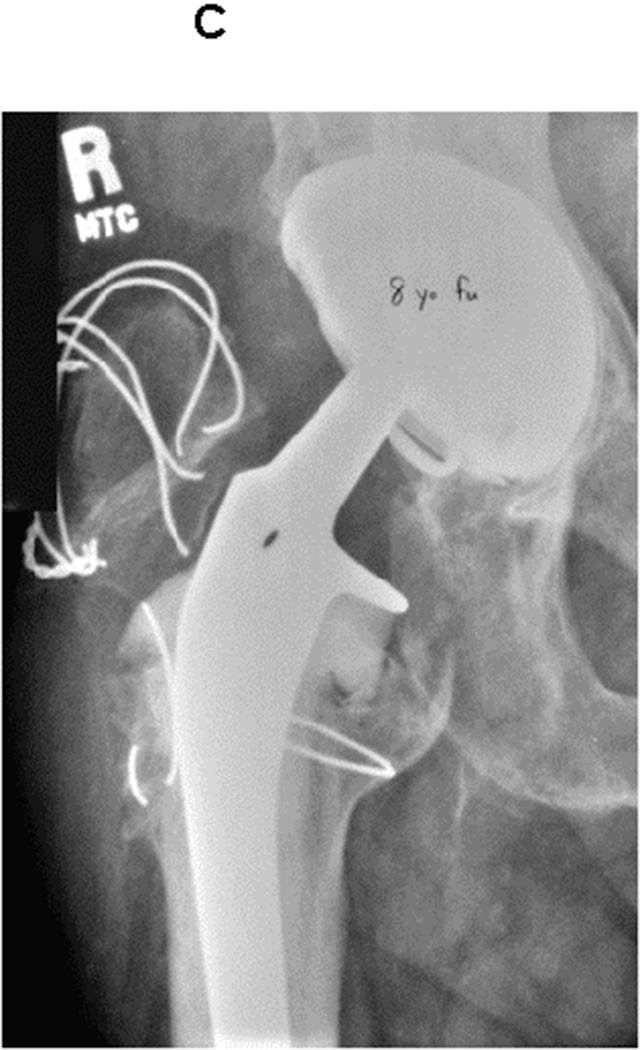
Preoperative (A), postoperative (B), and 8 year follow-up (C) radiographs of cemented constrained liner construct. The patient was an 80 year old male with recurrent dislocations (A). The constrained liner was cemented into a secure shell (note the greater trochanter non-union and escape) (B). Final follow up radiographs demonstrate a secure construct (within a year of his death) (C).
Acknowledgement
The authors would like to acknowledge Richard C. Johnston, MD for his contribution to the study in terms of performing the index revision surgery on a number of the study patients.
References
- 1.Callaghan JJ, Parvizi J, Novak CC, Bremner B, Shrader W, Lewallen DG, Johnston RC, Goetz DD. A constrained liner cemented into a secure cementless acetabular shell. J Bone Joint Surg Am. 2004;86:2206–2211. [DOI] [PubMed] [Google Scholar]
- 2.Haft GF, Heiner AD, Dorr LD, Brown TD, Callaghan JJ. A biomechanical analysis of polyethylene liner cementation into a fixed metal acetabular shell. J Bone Joint Surg Am. 2003. June:85-A(6):1100–10. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81. [Google Scholar]
- 4.Jo S, Jimenez Almonte JH, Sierra RJ. The cumulative risk of re-dislocation after revision THA performed for instability increases close to 35% at 15 years. J Arthroplasty.2015;30(7):1177–82. [DOI] [PubMed] [Google Scholar]


