Synopsis
Bone morphology is one feature that contributes to knee kinematics. The geometry of the tibia and femur vary across individuals, and these differences can influence the risk of ACL injury and of failure after isolated ACL reconstruction. There has been renewed interest in lateral extra-articular stabilization procedures to supplement an ACL reconstruction, though which patients benefit most from these procedures remains unclear. In this article, we review the impact of bone morphology on knee kinematics, including tibial slope, depth of the medial tibial plateau, intercondylar notch shape, tibial eminence volume, and sphericity of the femoral condyles.
Keywords: Bone morphology, anterior cruciate ligament injuries, knee kinematics, tibial slope, intercondylar notch shape
Introduction
Anterior cruciate ligament (ACL) injuries occur frequently in young, active patients and are a common cause of disability in this group of patients. ACL injuries place patients at risk for the development of post-traumatic osteoarthritis, further contributing to limited function of the injured knee.1 There are approximately 250,000 ACL injuries in the United States alone each year, with 175,000 of these patients electing to undergo surgical reconstruction.2,3
The stability of the knee following an isolated ACL injury can be quite variable, with a subset of patients reporting minimal instability while others face profound limitations from this injury.4,5 Multiple factors contribute to knee stability both after ACL injury and following ACL reconstruction. There has been renewed interest recently in the role of additional extra-articular procedures in the setting of failed reconstruction or patients with increased preoperative knee laxity.6 Clear indications regarding utilization of these procedures remains unclear. One factor that contributes to knee kinematics that determines this spectrum of instability, from patients who may cope with an isolated ACL injury to those who may require a lateral extra-articular reconstruction to eliminate a pivot shift phenomenon, maybe the bony geometry of the knee. There is a need to clarify which patients will benefit most from surgical reconstruction and from supplemental procedures in addition to ACL reconstruction, and there is potential that the anatomic differences with regards to bone shape may be an important factor in determining appropriate treatment recommendations. The purpose of this article will be to review the current evidence on the contribution of tibial and femoral bone morphology to knee kinematics.
Tibial Bone Morphology
The articular geometry of the tibial plateau influences the stability of the knee following ACL injury and changes the forces transmitted through the cruciate ligaments. The lateral plateau is convex, compared to the concave medial plateau with increased congruity with its femoral condyle, which leads to more translational motion at the lateral side of the knee.7,8 The posterior slope of the knee also contributes to the magnitude of the pivot shift, as the femoral condyle can translate more with an increased posterior tibial slope.9 Increased motion at the anterior lateral tibial plateau may be responsible for tibial subluxation at the initiation of knee flexion10 and may be associated with the severity of the pivot shift.11
Marouane et al., investigated the effects of varying the posterior tibial slope on knee kinematics and forces across the ACL.12 The kinematic changes were calculated through finite element modeling of the normal gait cycle. With increases in posterior tibial slope, the anterior tibial translation increased, while decreased anterior tibial translation was observed with a lower tibial slope. The force across the ACL increased from 181 N to 317 N with a 5 degree increase in posterior tibial slope and to 460 N with a 10-degree slope increase. This force decreased to 102 N by decreasing posterior slope by 5 degrees, and the ACL was offloaded completely by decreasing posterior slope by 10 degrees. The observed effects would likely be further increased with greater external loads through larger muscle activation forces. Multiple cadaveric studies have also demonstrated that an increase in the tibial slope results in increasingly anterior resting position of the tibia relative to the femur.13–15
Shelburne et al., reported how posterior tibial slope effected the forces across the cruciate ligaments and knee-joint loading in a finite element model during standing, squatting, and walking.16 For all positions, there was a linear relationship between the posterior tibial slope and cruciate ligament forces, tibial shear force, as well as anterior tibial translation. Tibial shear force, which is determined by the posterior tibial slope, has been shown to determine the forces across the cruciate ligaments.17,18 Therefore, the shape of the proximal tibia is a strong contributor to forces across the ACL and kinematics of the knee.
Tibial slope is the most frequently reported bone shape feature implicated in ACL injury and risk of failure following ACL reconstruction. Dejour and Bonnin radiographically measured anterior tibial translation on the lateral standing, bent-knee radiographs of 281 patients with chronic ACL injuries.19 Posterior tibial slope is measured on radiographs, first defining the longitudinal axis of the tibia with two points equidistant between the anterior and posterior tibial cortices just distal to the tibial tubercle and a second 10 cm distal to this first point (Figure 1). A line perpendicular to this is drawn at the joint line, and the angle between this line and a line along the tibial plateau defines the tibial slope. The amount of anterior tibial translation was directly and significantly correlated with the magnitude of the posterior tibial slope, with 6 mm of anterior tibial translation observed for each 10 degrees that tibial slope increased. This study is in agreement with the cadaveric and modeling studies that show the influence of tibial slope on knee kinematics and force across the ACL.
Figure 1.

The posterior tibial slope is defined on the lateral radiograph by measuring the angle between the diaphyseal axis (blue line) of the tibia and the tibial plateau (solid green line). An increased posterior tibial slope (dotted yellow line) is associated with increased anterior tibial translation and increased force across the anterior cruciate ligament.
Multiple clinical case-control studies have found increased posterior tibial slope as a risk factor for sustaining a non-contact ACL injury. Brandon et al., found the posterior tibial slope to be higher for both female (12.6° vs 8.6°; p<0.001) and male (10.8° vs 8.4°; p<0.001) with ACL injuries relative to patients with patellofemoral pain.11 Additionally, among patients with ACL injuries, those with a more severe pivot-shift grade had increased posterior tibial slope relative to those with a lower-grade pivot shift (11.1° vs 9.2°; p=0.03). Other case-control studies have identified increased posterior slope as a risk factor for ACL injury in both male and female patients20 or female patients alone.21
The effects of posterior tibial slope also appear to be different between the medial and lateral sides of the knee, with the lateral side more consistently having a larger impact on knee kinematics. Stijak et al., reported increased lateral tibial slope in patients with ACL injuries relative to control patients (7.5° vs 4.4°) while there was no increase with the slope of the medial plateau (5.2° vs 6.6).22 Other case-control studies have found that both the medial and lateral plateaus23 or just the lateral plateau in men24 showed increased posterior slope in patients with ACL injuries. In a recent meta-analysis of studies evaluating the impact of tibial slope on ACL injury, Zeng et al., found that both the medial and lateral slope appeared to be associated with increasing the risk of ACL injury.25 The evidence for lateral tibial plateau slope as a risk factor for ACL injury was overall stronger and more consistent. These studies suggest the slope, particularly of the lateral tibial plateau, places patients at-risk for ACL injuries, likely through the mechanism of increased translation of the lateral tibia and greater stress across the ACL.
The depth of the medial tibial plateau has also been implicated in contributing to the risk of ACL injury. The medial plateau has a concave shape that allows for inherent congruity with the medial femoral condyle and is more constrained relative to the convex lateral plateau. Hashemi et al., measured the depth of the medial tibial plateau on MRI for 49 patients with ACL injuries and 55 subjects without ACL injury.23 A shallower medial tibial plateau was noted in patients with ACL injuries (Figure 2). This finding suggests that patients with ACL injury may have bone shape features, such as a shallow medial tibial plateau, that predispose to ligamentous injury, which may help to identify patients who may benefit from additional procedures in addition to ACL reconstruction, though this hypothesis would need further clinical and biomechanical testing.
Figure 2.
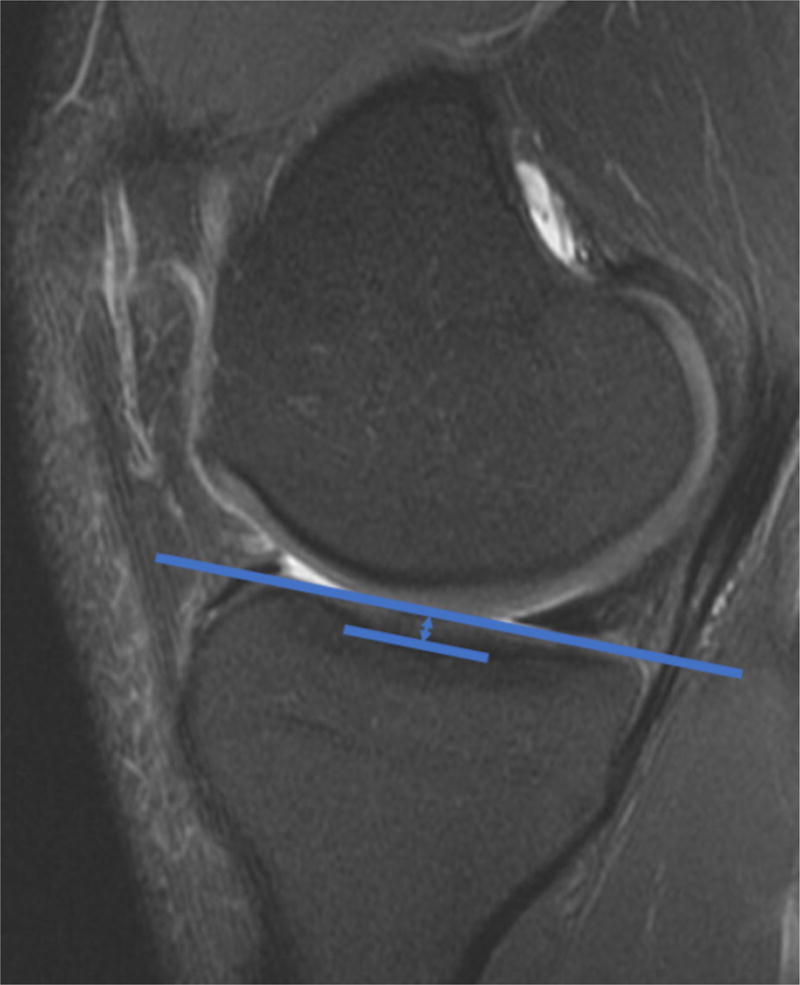
The depth of the medial plateau was shown by Hashemi et al23 to be associated with the risk of ACL injury. A shallow medial tibial plateau, measured as shown here on a sagittal MRI, may be associated with less articular congruity and greater risk of ACL injury.
The volume of the medial tibial spine was identified by Sturnick et al., as a potential risk factor for ACL injury.26 MRI was used to calculate this volume for patients with and without ACL injuries. Among male patients specifically, a lower volume of the medial tibial spine was correlated with an increased risk of ACL injury. Through normal knee range of motion, the tibial spines do have some articulation with the femoral condyles. Motion of the knee may vary with different shapes of the tibial spines, and patients with smaller spines may continue to have abnormal knee kinematics even after ACL reconstruction.
Femoral Bone Morphology
Variations in femoral morphology have also been reported to influenceknee kinematics. Differences in intercondylar notch morphology are the most commonly reported bone feature on the femoral side to be associated with ACL injury. Eggerding et al., followed 257 patients prospectively after ACL injury to determine if morphological features identified on radiographs could predict IKDC knee stability scores.27 Statistical shape modeling, which is an unbiased method for determining unique shape features common within a group of patients, was used to explore bony geometry on lateral and 45-degree, bent-knee PA radiographs. A pyramidal-shaped intercondylar notch was associated with higher IKDC scores 2 years after injury as compared to patients with dome-shaped intercondylar notches (Figure 3). This pyramidal shape of the intercondylar notch was theorized to lead to a more intrinsically stable joint that relies less on ligamentous function. As demonstrated in this study, certain bone features may help in predicting which patients will tolerate an ACL-deficiency state while others may continue to have instability following anatomic ACL reconstruction.
Figure 3.

The intercondylar notch shape has been implicated as a risk factor for ACL injury. A pyramidal shape notch shape, present in this patient and outlined in blue, may lead to greater bony congruity of the knee and was found to be associated with better knee stability scores at two years after non-operatively treated ACL injuries as compared to a dome-shaped notch, outlined in green.
Friden et al., also investigated for potential bony factors that contribute to subjective instability following ACL injury.28 A series of 100 patients with ACL injuries and limited activity levels were followed for 5 years. There were 16 patients that elected to undergo ACL reconstruction, and a more spherical shape of the femoral condyles was correlated with patients who had failed non-operative treatment. Differences in the shape of the femoral condyles may lead to variability in knee kinematics and differential injury risk and subjective stability.
Three-Dimensional Shape Study
Our group has utilized three-dimensional statistical shape modeling with MRI-based knee kinematics to correlate the relationship between specific bone morphological features and post-surgical knee kinematics after ACL reconstruction.29 There was wide variation in the post-reconstruction anterior tibial translation of the reconstructed knee compared to the patient’s normal, contralateral knee in patients with isolated ACL injuries, and the amount of both post-injury and post-reconstruction anterior tibial translation was associated with morphological features of both the tibia and femur. Greaterslope of the medial tibial plateau (Figure 4A), a more spherical medial femoral condyle (Figure 4B), and increased length of the lateral tibial plateau were all associated with abnormal post-injury and post-surgical knee kinematics. A shorter medial tibial plateau, like that observed by Hashemi et al., was also associated with abnormal post-surgical knee kinematics. The findings in this prospective study with three-dimensional imaging and sophisticated shape determination algorithms corroborate many of the findings identified in previous retrospective studies, given further strength to the relationships proposed between bone morphology and knee kinematics.
Figure 4.

Two shapes identified through statistical shape modeling that were identified to be associated with abnormal post-ACL injury and post-reconstruction knee kinematics were the slope of the medial tibial plateau and the sphericity of the medial femoral condyle. A flatter medial tibial slope (A) was associated with knee kinematics that were more similar to the patient’s contralateral knee, while a steeper medial tibial slope was associated with greater anterior tibial translation. A more ovoid-shaped medial femoral condyle (B) was associated with more similar kinematics compared to the patient’s contralateral knee, while a more spherical-shaped medial femoral condyle was associated with greater anterior tibial translation. S – superior; I – inferior; A – anterior; P – posterior; M – medial; L – lateral.
Surgical Considerations
Posterior tibial slope is one factor that may be altered surgically. Dejour et al., reported on a series of 9 patients who were treated with second-time revision ACL reconstruction. In this series, the patients were also treated with a deflexion tibial osteotomy, decreasing the mean posterior tibial slope of the group from 13.2° to 4.4°.30 With this bony correction, the anterior tibial translation decreased from 11.7 mm prior to surgery to 4.3 mm after reconstruction. These results highlight the importance of considering bone morphology, especially when contemplating revision ACL reconstruction. Correction of an increased posterior tibial slope should be strongly considered in the setting of a failed ACL reconstruction and 13 degrees or more of posterior tibial slope. Many of the other bony features noted here that impact knee kinematics and lead to an increased ACL injury risk may not be modifiable. These findings however, may still have great utility when dealing with patients at risk for ACL injury, after primary ACL injury, or following failed reconstruction and may prove to be important in clarifying indications for extra-articular reconstructive procedures.
Conclusions
Future clinical and biomechanical studies should evaluate how bone morphology may contribute to knee kinematics after isolated ACL reconstruction or combined with lateral extra-articular reconstruction procedures. Further studies using three-dimensional imaging and statistical shape modeling will aide in clarifying the role of various bone features in knee kinematics. Patients with certain tibial and femoral morphological features may remain at-risk for ACL injury even after an anatomic ligament reconstruction due to the articular geometry that may increase anterior tibial translation and stress across the ACL. The patients with the specific bone features described here will benefit from further evaluation as to the optimal surgical reconstructive techniques and methods to achieve a stable and functional knee.
Table 1.
Bone shape features and their relationship to knee kinematics
| Bone Shape Feature | Correlation with Knee Kinematics |
|---|---|
| Posterior-inferior tibial slope | Increasing posterior-inferior tibial slope is correlated with increased anterior tibial translation and force across ACL |
| Depth of medial tibial plateau | Decreasing depth of medial tibial plateau is associated with decreased bony congruity in the medial compartment |
| Volume of medial tibial eminence | Decreased volume of medial tibial eminence is associated with decreased contact area |
| Notch shape | Pyramidal notch shape may lead to more intrinsically-stable knee while dome-shaped notch may be more dependent on ACL for stability |
| Sphericity of femoral condyles | More spherical femoral condyles, particularly medial, associated with abnormal knee kinematics after surgery and after ACL reconstruction and increased risk of symptomatic instability |
Key Points.
Morphological variations in the tibia and femur influence the kinematics of the knee and contribute to risk of ACL injury, as well as function of the knee after injury and following surgical reconstruction.
Increases in posterior tibial slope result in increased forces across the ACL and increased anterior tibial translation.
A shallow medial tibial plateau and lower volume of the medial tibial eminence lead to less bony congruity and place greater demand on ligamentous restraint in the knee.
A dome-shaped intercondylar notch and spherical femoral condyles have been linked to worse patient-reported knee stability scores after ACL injury.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lohmander LS, Östenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis & Rheumatism. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 2.Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction & prevention of ACL injuries: Cut risk with 3 sharpened & validated tools. Journal of Orthopaedic Research. 2016 doi: 10.1002/jor.23414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spindler KP, Wright RW. Anterior cruciate ligament tear. New England Journal of Medicine. 2008;359(20):2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrance PJ, Williams GN, Snyder-Mackler L, Buchanan TS. Altered knee kinematics in ACL-deficient non-copers: A comparison using dynamic MRI. Journal of Orthopaedic Research. 2006;24(2):132–140. doi: 10.1002/jor.20016. [DOI] [PubMed] [Google Scholar]
- 5.Barrance PJ, Williams GN, Snyder-Mackler L, Buchanan TS. Do ACL-injured Copers Exhibit Differences in Knee Kinematics?: An MRI Study. Clinical Orthopaedics and Related Research. 2007;454:74–80. doi: 10.1097/BLO.0b013e31802bab0d. [DOI] [PubMed] [Google Scholar]
- 6.Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP. Effect of High-Grade Preoperative Knee Laxity on Anterior Cruciate Ligament Reconstruction Outcomes. The American journal of sports medicine. 2016;44(12):3077–3082. doi: 10.1177/0363546516656835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amis AA. Anterolateral knee biomechanics. Knee Surgery, Sports Traumatology, Arthroscopy. 2017:1–9. doi: 10.1007/s00167-017-4494-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahfouz MR, Komistek RD, Dennis DA, Hoff WA. In vivo assessment of the kinematics in normal and anterior cruciate ligament-deficient knees. J Bone Joint Surg Am. 2004;86(suppl 2):56–61. doi: 10.2106/00004623-200412002-00009. [DOI] [PubMed] [Google Scholar]
- 9.østgaard SE, Helmig P, Nielsen S, Hvid I. Anterolateral instability in the anterior cruciate ligament deficient knee: a cadaver study. Acta Orthop Scand. 1991;62(1):4–8. doi: 10.3109/17453679108993082. [DOI] [PubMed] [Google Scholar]
- 10.Bull A, Earnshaw P, Smith A, Katchburian M, Hassan A, Amis A. Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. Bone & Joint Journal. 2002;84(7):1075–1081. doi: 10.1302/0301-620x.84b7.13094. [DOI] [PubMed] [Google Scholar]
- 11.Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2006;22(8):894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 12.Marouane H, Shirazi-Adl A, Hashemi J. Quantification of the role of tibial posterior slope in knee joint mechanics and ACL force in simulated gait. Journal of biomechanics. 2015;48(10):1899–1905. doi: 10.1016/j.jbiomech.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Agneskirchner J, Hurschler C, Stukenborg-Colsman C, Imhoff A, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Archives of orthopaedic and trauma surgery. 2004;124(9):575–584. doi: 10.1007/s00402-004-0728-8. [DOI] [PubMed] [Google Scholar]
- 14.Rodner CM, Adams DJ, Diaz-Doran V, et al. Medial opening wedge tibial osteotomy and the sagittal plane the effect of increasing tibial slope on tibiofemoral contact pressure. The American journal of sports medicine. 2006;34(9):1431–1441. doi: 10.1177/0363546506287297. [DOI] [PubMed] [Google Scholar]
- 15.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. The American journal of sports medicine. 2004;32(2):376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 16.Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. Journal of Orthopaedic Research. 2011;29(2):223–231. doi: 10.1002/jor.21242. [DOI] [PubMed] [Google Scholar]
- 17.Pandy MG, Shelburne KB. Dependence of cruciate-ligament loading on muscle forces and external load. Journal of biomechanics. 1997;30(10):1015–1024. doi: 10.1016/s0021-9290(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 18.Shelburne KB, Pandy MG, Anderson FC, Torry MR. Pattern of anterior cruciate ligament force in normal walking. Journal of biomechanics. 2004;37(6):797–805. doi: 10.1016/j.jbiomech.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. Journal of Bone & Joint Surgery, British Volume. 1994;76-B(5):745–749. [PubMed] [Google Scholar]
- 20.Todd MS, Lalliss S, Garcia ES. The Relationship Between Posterior Tibial Slope and Anterior Cruciate Ligament Injuries. The American Journal of Sports Medicine. 2010;38(1):63–67. doi: 10.1177/0363546509343198. [DOI] [PubMed] [Google Scholar]
- 21.Hohmann E, Bryant A, Reaburn P, Tetsworth K. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19(1):109–114. doi: 10.1007/s00167-011-1547-4. [DOI] [PubMed] [Google Scholar]
- 22.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? Knee surgery, sports traumatology, arthroscopy. 2008;16(2):112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 23.Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes new risk factors for anterior cruciate ligament injuries. The American journal of sports medicine. 2010;38(1):54–62. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 24.Bisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2010;26(7):901–906. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Zeng C, Cheng L, Wei J, et al. The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: a meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(1):53–65. doi: 10.1007/s00167-012-2277-y. [DOI] [PubMed] [Google Scholar]
- 26.Sturnick DR, Argentieri EC, Vacek PM, et al. A decreased volume of the medial tibial spine is associated with an increased risk of suffering an anterior cruciate ligament injury for males but not females. Journal of orthopaedic research. 2014;32(11):1451–1457. doi: 10.1002/jor.22670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eggerding V, van Kuijk K, van Meer B, et al. Knee shape might predict clinical outcome after an anterior cruciate ligament rupture. Bone Joint J. 2014;96(6):737–742. doi: 10.1302/0301-620X.96B6.32975. [DOI] [PubMed] [Google Scholar]
- 28.Fridén T, Jonsson A, Erlandsson T, Jonsson K, Lindstrand A. Effect of femoral condyle configuration on disability after an anterior cruciate ligament rupture: 100 patients followed for 5 years. Acta Orthop Scand. 1993;64(5):571–574. doi: 10.3109/17453679308993695. [DOI] [PubMed] [Google Scholar]
- 29.Lansdown DA, Pedoia V, Zaid M, et al. Variations in Knee Kinematics After ACL Injury and After Reconstruction Are Correlated With Bone Shape Differences. Clin Orthop Relat Res. 2017 doi: 10.1007/s11999-017-5368-8. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surgery, Sports Traumatology, Arthroscopy. 2015;23(10):2846–2852. doi: 10.1007/s00167-015-3758-6. [DOI] [PubMed] [Google Scholar]


