This cohort study of community-recruited women aged 40 to 60 years evaluates the association of a history of sexual harassment and sexual assault with mental and physical health indices.
Key Points
Question
Do women with a history of sexual harassment or sexual assault have higher blood pressure, greater depression and anxiety, and poorer sleep than women without this history?
Findings
Among 304 nonsmoking midlife women recruited from the community to undergo assessment and complete questionnaires for this prospective cohort study, those with a history of workplace sexual harassment had significantly higher odds of hypertension and clinically poor sleep than women without this history, after adjusting for covariates. Women with a history of sexual assault had significantly higher odds of clinically significant depressive symptoms, anxiety, and poor sleep than women without this history, after adjusting for covariates.
Meaning
Sexual harassment and sexual assault have implications for women’s health.
Abstract
Importance
Sexual harassment and sexual assault are prevalent experiences among women. However, their association with health indices is less well understood.
Objective
To investigate the association of history of sexual harassment and sexual assault with blood pressure, mood, anxiety, and sleep among midlife women.
Design, Setting, and Participants
Nonsmoking women without cardiovascular disease were recruited from the community to undergo physical measurements (blood pressure, height, weight), medical history, and questionnaire psychosocial assessments (workplace sexual harassment, sexual assault, depression, anxiety, sleep).
Exposures
Sexual harassment and sexual assault.
Main Outcomes and Measures
Blood pressure, depressive symptoms, anxiety, and sleep characteristics.
Results
Among the 304 nonsmoking women aged 40 to 60 years who participated in the study, all were free of clinical cardiovascular disease, and the mean (SD) age was 54.05 (3.99) years. A total of 19% reported a history of workplace sexual harassment (n = 58), and 22% reported a history of sexual assault (n = 67). Sexual harassment was related to significantly greater odds of stage 1 or 2 hypertension among women not taking antihypertensives (odds ratio [OR], 2.36; 95% CI, 1.10-5.06; P = .03) as well as clinically poor sleep (OR, 1.89; 95% CI, 1.05-3.42; P = .03), after adjusting for covariates. Sexual assault was associated with significantly greater odds of clinically elevated depressive symptoms (OR, 2.86; 95% CI, 1.42-5.77; multivariable P = .003), clinically relevant anxiety (OR, 2.26; 95% CI, 1.26-4.06; P = .006), and clinically poor sleep (OR, 2.15; 95% CI, 1.23-3.77; multivariable P = .007), after adjusting for covariates.
Conclusions and Relevance
Sexual harassment and sexual assault are prevalent experiences among midlife women. Sexual harassment was associated with higher blood pressure and poorer sleep. Sexual assault was associated with poorer mental health and sleep. Efforts to improve women’s health should target sexual harassment and assault prevention.
Introduction
Sexual harassment and sexual assault are common experiences among women. In the United States, an estimated 40% to 75% of women have experienced workplace sexual harassment,1 and over 1 in 3 women (36%) have experienced sexual assault.2 With recent popular movements (eg, MeToo, #TimesUp), there is rising public awareness of sexual harassment and assault and their implications for women’s health.
Both sexual harassment and sexual assault have been linked to poorer self-reported physical and mental health outcomes.3,4,5,6,7,8 While these studies suggest that harassment and assault are associated with adverse outcomes broadly, these findings are limited by several issues. Survey studies, particularly of sexual harassment, largely assess physical health via self-report. These reports can be biased by mood, memory, and reporting of physical symptoms9 and by awareness of health conditions, which can vary by socioeconomic status, health care access, and health literacy.10 Another limitation is incomplete consideration of critical confounding factors, such as socioeconomic position, adiposity, and medication use. Furthermore, self-reported outcomes are often assessed using single-question items rather than full validated measures. Research on sexual harassment and assault using measured health indices, full multidimensional scales, and comprehensive consideration of confounders is warranted.
Among a well-characterized sample of 304 midlife women, we investigated the association of a history of sexual harassment and sexual assault with blood pressure (BP), depressed mood, anxiety, and sleep, important health issues affecting midlife women. Elevated BP is a major risk factor for cardiovascular disease (CVD), the leading cause of death in women,11 and an important indicator of risk among midlife women who typically develop clinical CVD later in life.12 Depression and anxiety show a doubling in rates in women relative to men,13 and up to half of midlife women report problems with sleep.14,15 We hypothesized that sexual harassment and assault would be associated with higher BP, more depressed mood and anxiety, and poorer sleep after accounting for key confounders.
Methods
Study Participants
A total of 304 nonsmoking women aged 40 to 60 years were recruited from the community (Pittsburgh, Pennsylvania) via advertisements, mailings, and online message boards. The cohort was originally selected for a study designed to examine the association of menopausal hot flashes and subclinical atherosclerosis as assessed by carotid ultrasonography.16 Per the original study design, half of the women reported menopausal hot flashes, and half reported no hot flashes.16 Of the 1929 women who underwent telephone screening, 304 were eligible and enrolled. Exclusions, selected based on their impact on menopausal symptoms and cardiovascular health, included premenopausal status; hysterectomy or oophorectomy; reported history of CVD, arrhythmia, kidney failure, gynecological cancer; current pregnancy; or having used key medications in the past 3 months: oral/transdermal estrogen or progesterone, selective estrogen receptor modulators, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, gabapentin, insulin, β-blockers, calcium channel blockers, and α-2 adrenergic agonists. Procedures were approved by the University of Pittsburgh institutional review board, and all participants provided written informed consent.
Main Outcomes and Measures
Procedures included physical measurements, interviews, and questionnaires. Sexual harassment and assault were assessed from Brief Trauma Questionnaire items developed for the Nurses’ Health Study II17 adapted from the Brief Trauma Interview.18,19 Items assessed workplace sexual harassment (“Have you ever experienced sexual harassment at work that was either physical or verbal?”) and sexual assault (“Have you ever been made or pressured into having some type of unwanted sexual contact? [By sexual contact we mean any contact between someone else and your private parts or between you and someone else’s private parts])?” Response options were yes/no. This measure has high interrater reliability relative to the Diagnostic and Statistical Manual of Mental Disorders (fourth edition) for presence of Criterion A1 trauma exposure (κ = 0.70).17
Seated BP was measured via a Dinamap device after a 10-minute rest. Height and weight were measured via a stadiometer and balance beam scale. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Depressive symptoms were assessed by the Center for Epidemiologic Studies Depression (CESD) scale,20 trait anxiety via the Spielberger State-Trait Anxiety Inventory (STAI),21 and sleep quality via the Pittsburgh Sleep Quality Index (PSQI)22 considered continuously and via clinical cut points (CESD ≥1620; PSQI >522; and STAI ≥4023 and upper quartile of normative samples21). Demographics and medical history were assessed via structured interview. Women reported current medication use (eg, for BP: angiotensin converting enzyme inhibitors, angiotensin receptor blockers, diuretics; for sleep: melatonin, GABA-α agents (γ-aminobutyric acid-α); for anxiety: benzodiazepines; and for depression: bupropion, tricyclic agents). Physical activity was assessed via the International Physical Activity Questionnaire24 and snoring via the Berlin Questionnaire.25
Data Analyses
All PSQI values were natural log–transformed for analysis. Differences between participants by harassment or assault history were tested using linear regression, Wilcoxon rank sum, and χ2 tests. Associations between exposures and outcomes were tested in regression models. Covariates were factors associated with the outcome at P < .15, with select variables selected a priori for inclusion (medications and for sleep models snoring and nightshift work). Residual analysis and diagnostic plots were conducted to verify model assumptions. Analyses were performed with SAS software, version 9.4 (SAS Institute Inc). Models were 2 sided, α = .05.
Results
Participants were on average 54 years old (Table 1). Nineteen percent of women (n = 58) reported a history of workplace sexual harassment, and 22% reported a history of sexual assault (n = 67). Ten percent of women reported both sexual harassment and assault (n = 30). Women with a history of sexual harassment had higher education yet more financial strain. No characteristics varied by sexual assault.
Table 1. Study Participant Characteristics.
| Characteristic | Participants, No. (%) (n = 304) | |||
|---|---|---|---|---|
| Workplace Sexual Harassment | Sexual Assault | |||
| Yes (n = 58 [19%]) | No (n = 246 [81%]) | Yes (n = 67 [22%]) | No (n = 237 [78%]) | |
| Age, mean (SD), y | 53.93 (3.53) | 54.08 (4.09) | 53.73 (4.06) | 54.14 (3.97) |
| Race/ethnicity | ||||
| White | 45 (77.59) | 175 (71.14) | 50 (74.63) | 170 (71.73) |
| Nonwhitea | 13 (22.41) | 71 (28.86) | 17 (25.37) | 67 (28.27) |
| Educationb | ||||
| <College | 17 (29.31) | 112 (45.53) | 23 (34.33) | 106 (44.73) |
| ≥College | 41 (70.69) | 134 (54.47) | 44 (65.67) | 131 (55.27) |
| Marital status | ||||
| Married/partnered | 28 (48.28) | 142 (57.72) | 32 (47.76) | 138 (58.23) |
| Divorced/widowed | 14 (24.14) | 64 (26.02) | 17 (25.37) | 61 (25.74) |
| Single | 16 (27.59) | 40 (16.26) | 18 (26.87) | 38 (16.03) |
| Financial strain, yesc | 27 (46.55) | 68 (27.98) | 26 (38.81) | 69 (29.49) |
| BMI, mean (SD) | 27.85 (6.07) | 29.26 (6.89) | 27.80 (6.20) | 29.32 (6.88) |
| Alcohol use | ||||
| <Monthly | 21 (36.21) | 109 (44.31) | 29 (43.28) | 101 (42.62) |
| Monthly but <weekly | 20 (34.48) | 77 (31.30) | 23 (34.33) | 74 (31.22) |
| Weekly | 17 (29.31) | 60 (24.39) | 15 (22.39) | 62 (26.16) |
| Leisure physical activity (IPAQ score), median (IQR)d | 458 (0-1286) | 396 (0-1298) | 297 (0-1188) | 438 (0-1386) |
| Snoring | 27 (46.55) | 109 (44.31) | 31 (46.27) | 105 (44.30) |
| Nightshift work | 3 (5.17) | 17 (6.91) | 5 (7.46) | 15 (6.33) |
| Medication use | ||||
| BP-lowering | 9 (15.52) | 39 (15.85) | 7 (10.45) | 41 (17.30) |
| Sleep | 2 (3.45) | 12 (4.88) | 1 (1.49) | 13 (5.49) |
| Antidepressants | 1 (1.72) | 5 (2.03) | 1 (1.49) | 5 (2.11) |
| Anxiolytics | 1 (1.72) | 4 (1.63) | 1 (1.49) | 4 (1.69) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BP, blood pressure; IPAQ, International Physical Activity Questionnaire24; IQR, interquartile range.
Nonwhite race/ethnicity includes African American, Asian, Hispanic, or biracial.
Education level varied significantly by harassment status (P < .05).
Financial strain was defined as somewhat hard or very hard to pay for basic necessities of life, and it varied significantly by harassment status (P < .05).
Physical activity was square-root transformed for analysis.
Women with a history of sexual harassment had significantly higher systolic BP (SBP), marginally higher diastolic BP (DBP), and significantly poorer sleep quality than women without a history of harassment, after adjusting for covariates (all supporting data provided in Table 2). When considering clinical cut points, harassment was associated with significantly higher likelihood of stage 1 or 2 hypertension among women not taking antihypertensive medications (SBP ≥130 or DBP ≥80 mm Hg; odds ratio [OR], 2.36; 95% CI, 1.10-5.06; multivariable P = .03) and of poor sleep consistent with clinical insomnia (OR, 1.89; 95% CI, 1.05-3.42; multivariable P = .03) (Figure 1).
Table 2. Workplace Sexual Harassment and Sexual Assault Associated With BP, Mental Health, and Sleep Indicesa.
| Characteristic | Sexual Harassment, B (SE) | P Value | Sexual Assault, B (SE) | P Value |
|---|---|---|---|---|
| SBP | 3.96 (1.94) | .04 | 1.55 (1.85) | .40 |
| DBP | 2.40 (1.29) | .06 | 1.49 (1.23) | .23 |
| Depressive symptoms | 2.27 (1.21) | .06 | 4.01 (1.13) | <.001 |
| Anxiety | 1.55 (1.43) | .28 | 3.78 (1.34) | .005 |
| Sleep qualityb | 0.15 (0.07) | .03 | 0.24 (0.06) | <.001 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BP, blood pressure; B (SE), unstandardized beta (standard error); DBP, diastolic blood pressure; SBP, systolic blood pressure.
All models adjusted for age, race/ethnicity, education, BMI; BP models adjusted for use of BP-lowering medication; depression/anxiety models adjusted for use of antidepressants or anxiolytics; sleep models adjusted for snoring, use of sleep medication, nightshift work.
Sleep quality natural log transformed for analysis.
Figure 1. Association of Sexual Harassment With Prevalence of Hypertension and Poor Sleep.
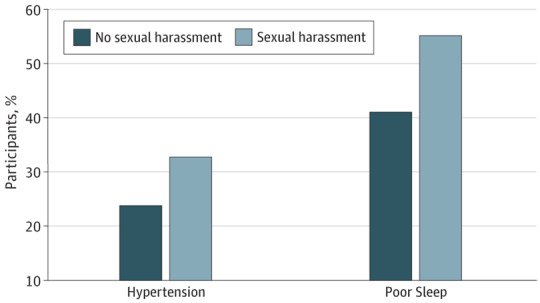
For hypertension, the adjusted odds ratio (aOR) was 2.36 (95% CI, 1.10-5.06) (P = .03); for sleep, aOR, 1.89 (95% CI, 1.05-3.42) (P = .03). Hypertension models were adjusted for age, race/ethnicity, education, and BMI among women not using antihypertensive medications; hypertension stage 1 or 2 was defined as systolic blood pressure of 130 mm Hg or higher or diastolic blood pressure of 80 mm Hg or higher. Sleep models were adjusted for age, race/ethnicity, education, BMI, snoring, use of sleep medication, and nightshift work.
Women with a history of sexual assault had higher depressive symptoms, anxiety, and poorer sleep quality than women without a history of sexual assault (Table 2). Assault was associated with significantly higher odds of clinically elevated depressive symptoms (OR, 2.86; 95% CI, 1.42-5.77; multivariable P = .003), anxiety (OR, 2.26; 95% CI, 1.26-4.06; multivariable P = .006), and poor sleep (OR, 2.15; 95% CI, 1.23-3.77; multivariable P = .007) (Figure 2).
Figure 2. Association of Sexual Assault With Depressed Mood, Anxiety, and Sleep Quality.
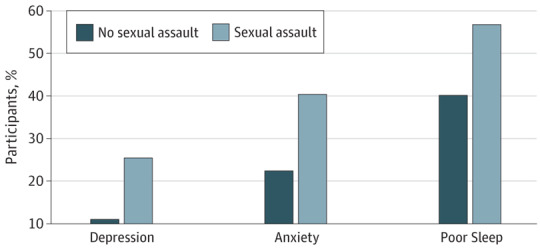
For depressed mood, the adjusted odds ratio (aOR) was 2.86 (95% CI, 1.42-5.77) (P = .003); for anxiety, aOR, 2.26 (95% CI, 1.26-4.06) (P = .006); for sleep, aOR, 2.15 (95% CI, 1.23-3.77) (P = .007). Depression and anxiety models were adjusted for age, race/ethnicity, education, BMI, use of antidepressants, and use of anxiolytics; sleep models were adjusted for age, race/ethnicity, education, BMI, snoring, use of sleep medication, and nightshift work.
Discussion
Among the study participants, 19% reported a history of workplace sexual harassment, and 22% reported a history of sexual assault. Sexual harassment was associated with higher BP and poorer sleep, and sexual assault with depressed mood, anxiety, and poor sleep. Associations persisted after adjusting for demographic and biomedical covariates.
Approximately 1 in 5 women reported having been sexually harassed or sexually assaulted. Although high, these rates are lower than those of national samples.1,2 Variations in estimates can arise from sample characteristics, assessment methods, and willingness of participants to report these sensitive experiences. Our sample was somewhat lower risk in sociodemographic and physical characteristics than the average population because we excluded women who were smokers, who had undergone hysterectomy, or who were using common antidepressants and certain cardiovascular medications. Few characteristics distinguished between women who had been sexually harassed and those who had been sexually assaulted, with the exception that women who were sexually harassed were more highly educated yet more financially strained. Notably, women who are younger or are in more precarious employment situations are more likely to be harassed, and financially stressed women can lack the financial security to leave abusive work situations.3 Why more highly educated women in the present study were more likely to be harassed is unclear; these women may more often be employed in male-dominated settings, be more knowledgeable about what constitutes sexual harassment, or be perceived as threatening; sexual harassment is an assertion of hierarchical power relations.3,26
This study examines sexual harassment and assault in relation to measured BP, an advance over previous work relying largely on self-reports. An exception is work by Krieger and colleagues,27 who examined workplace hazards in relation to BP among low-income participants, finding that only sexual harassment was associated with SBP among women. Notably, the magnitude of increase in SBP observed in the present study associated with a history of harassment (approximately 4 mm Hg in SBP) is clinically significant (eg, a 20% increased risk for CVD).28 Importantly, harassed women not taking antihypertensive agents had more than 2-fold increased odds of BP consistent with hypertension.
Sexual assault was related to poorer mental health. Assaulted women had almost 3-fold greater odds of symptoms consistent with a major depressive disorder and more than 2-fold greater odds of elevated anxiety. Conversely, sexual assault appeared less related to BP; a relation that may depend on the severity or chronicity of the victimization history.29 Sexual assault and harassment were each associated with a 2-fold increased odds of poor sleep consistent with clinical insomnia. Notably, poor sleep,30,31 depressed mood,32 and anxiety33 are themselves linked adverse physical health outcomes.
Strengths and Limitations
This work has limitations. Study exposures were assessed via 2 questions. Future work should use a full multidimensional scale that measures the severity and chronicity of exposures. Women recalled harassment and assault and reported exclusionary medical conditions that may incorporate reporting biases. The sample had somewhat limited representation of racial/ethnic minority groups and reflected several exclusions; thus, findings may not be generalizable to all women. Future work should include more diverse samples. This work incorporates multiple comparisons. Finally, this study cannot establish the causality or temporality of exposures associated with outcomes.
This study has several strengths. We considered sexual harassment and assault, prevalent yet understudied exposures in women. We considered measured BP and a range of mental health indices assessed with full, validated scales. We adjusted for a range of key covariates. We studied these associations in a well-characterized sample of women.
Conclusions
Among midlife women, workplace sexual harassment was associated with higher BP and poorer sleep, and sexual assault with depressed mood, anxiety, and poorer sleep. Future work should consider whether preventing or mitigating sexual harassment and sexual assault can improve women’s mental and cardiovascular health. Given the high prevalence of sexual harassment and assault, addressing these prevalent and potent social exposures may be critical to promoting health and preventing disease in women.
References
- 1.Willness CR, Steel P, Lee K. A meta-analysis of the antecedents and consequences of workplace sexual harassment. Person Psychol. 2007;60:127-162. doi: 10.1111/j.1744-6570.2007.00067.x [DOI] [Google Scholar]
- 2.Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, Merrick MT. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill Summ. 2014;63(8):1-18. [PMC free article] [PubMed] [Google Scholar]
- 3.McDonald P. Workplace sexual harassment 30 years on: a review of the literature. Int J Manag Rev. 2012;14:1-17. doi: 10.1111/j.1468-2370.2011.00300.x [DOI] [Google Scholar]
- 4.Centers for Disease Control and Prevention . Adverse health conditions and health risk behaviors associated with intimate partner violence—United States, 2005. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5705a1.htm. Accessed September 18, 2018.
- 5.Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162(10):1157-1163. doi: 10.1001/archinte.162.10.1157 [DOI] [PubMed] [Google Scholar]
- 6.Vives-Cases C, Ruiz-Cantero MT, Escribà-Agüir V, Miralles JJ. The effect of intimate partner violence and other forms of violence against women on health. J Public Health (Oxf). 2011;33(1):15-21. doi: 10.1093/pubmed/fdq101 [DOI] [PubMed] [Google Scholar]
- 7.Mason SM, Wright RJ, Hibert EN, et al. Intimate partner violence and incidence of type 2 diabetes in women. Diabetes Care. 2013;36(5):1159-1165. doi: 10.2337/dc12-1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mason SM, Wright RJ, Hibert EN, Spiegelman D, Forman JP, Rich-Edwards JW. Intimate partner violence and incidence of hypertension in women. Ann Epidemiol. 2012;22(8):562-567. doi: 10.1016/j.annepidem.2012.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bower GH. Mood and memory. Am Psychol. 1981;36(2):129-148. doi: 10.1037/0003-066X.36.2.129 [DOI] [PubMed] [Google Scholar]
- 10.Lillie-Blanton M, Rushing O, Ruiz S, Mayberry R, Boone L. Racial/Ethnic Differences in Cardiac Care: The Weight of the Evidence. Menlo Park, California: The Henry J. Kaiser Family Foundation and American College of Cardiology; 2002. [Google Scholar]
- 11.Benjamin EJ, Virani SS, Callaway CW, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 12.Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American heart association. Circulation. 2011;123(11):1243-1262. doi: 10.1161/CIR.0b013e31820faaf8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hankin BL, Young JF, Abela JR, et al. Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. J Abnorm Psychol. 2015;124(4):803-816. doi: 10.1037/abn0000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause. 2003;10(1):19-28. [DOI] [PubMed] [Google Scholar]
- 15.Shaver JL, Woods NF. Sleep and menopause: a narrative review. Menopause. 2015;22(8):899-915. doi: 10.1097/GME.0000000000000499 [DOI] [PubMed] [Google Scholar]
- 16.Thurston RC, Chang Y, Barinas-Mitchell E, et al. Menopausal hot flashes and carotid intima media thickness among midlife women. Stroke. 2016;47(12):2910-2915. doi: 10.1161/STROKEAHA.116.014674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koenen KC, De Vivo I, Rich-Edwards J, Smoller JW, Wright RJ, Purcell SM. Protocol for investigating genetic determinants of posttraumatic stress disorder in women from the Nurses’ Health Study II. BMC Psychiatry. 2009;9:29. doi: 10.1186/1471-244X-9-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schnurr P, Spiro A, Vielhauer M, Findler M, Hamblen J. Trauma in the lives of older men: findings from the Normative Aging Study. J Clin Geropsychol. 2002;8:175-187. doi: 10.1023/A:1015992110544 [DOI] [Google Scholar]
- 19.Schnurr PP, Lunney CA, Sengupta A, Spiro A III. A longitudinal study of retirement in older male veterans. J Consult Clin Psychol. 2005;73(3):561-566. doi: 10.1037/0022-006X.73.3.561 [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385-401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 21.Spielberger CD. Manual for the State-Trait Anxiety Inventory. Palo Alto, California: Consulting Psychologists Press; 1983. [Google Scholar]
- 22.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 23.Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63(11)(suppl 11):S467-S472. doi: 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381-1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 25.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485-491. doi: 10.7326/0003-4819-131-7-199910050-00002 [DOI] [PubMed] [Google Scholar]
- 26.Schweinle W, Cofer C, Schatz S. Men’s empathic bias, empathic inaccuracy, and sexual harassment. Sex Roles. 2008;60(1):142-150. [Google Scholar]
- 27.Krieger N, Chen JT, Waterman PD, et al. The inverse hazard law: blood pressure, sexual harassment, racial discrimination, workplace abuse and occupational exposures in US low-income black, white and Latino workers. Soc Sci Med. 2008;67(12):1970-1981. doi: 10.1016/j.socscimed.2008.09.039 [DOI] [PubMed] [Google Scholar]
- 28.Jones DW, Hall JE. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and evidence from new hypertension trials. Hypertension. 2004;43(1):1-3. doi: 10.1161/01.HYP.0000110061.06674.ca [DOI] [PubMed] [Google Scholar]
- 29.Renner LM, Spencer RA, Morrissette J, et al. Implications of severe polyvictimization for cardiovascular disease risk among female survivors of violence. J Interpers Violence. 2017:886260517728688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484-1492. doi: 10.1093/eurheartj/ehr007 [DOI] [PubMed] [Google Scholar]
- 31.Buysse DJ. Insomnia. JAMA. 2013;309(7):706-716. doi: 10.1001/jama.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305-315. [DOI] [PubMed] [Google Scholar]
- 33.Thurston RC, Rewak M, Kubzansky LD. An anxious heart: anxiety and the onset of cardiovascular diseases. Prog Cardiovasc Dis. 2013;55(6):524-537. doi: 10.1016/j.pcad.2013.03.007 [DOI] [PubMed] [Google Scholar]


