Abstract
Background:
High level of self-efficacy and adherence to self-care activities have a positive impact on the achievement of glycemic goal among diabetic patients. In Sudan, there is a gap in knowledge related to self-efficacy management and its influence on adherence to self-care activities and overall disease control.
Objective:
To identify the influence of management self-efficacy on adherence to self-care activities and treatment outcome among Sudanese patients with type 2 diabetes mellitus.
Methods:
A cross-sectional study was conducted at two health care facilities in Sudan from April to May 2016. Patients with type 2 diabetes mellitus were included. Convenience sampling method was adopted. Diabetes Management Self-Efficacy Scale and the Revised Summary of Diabetes Self-care Activities were used to collect data through a face-to-face interview. Logistic regression analysis was performed. A p value <0.05 was considered to be significant. Data were processed using the software SPPS v 21.0.
Results:
A total of 392 patients were included. Respondents classified with high level of self- efficacy across all domains were 191 (48.7%). Moreover, high level of education [adjusted OR 0.5 (0.3-0.7), (p=0.001)] and formal health education on diabetes [adjusted OR 2.4 (1.6-3.7), (p<0.001)], were found to be significantly associated with high level of diabetes management self-efficacy. Patients who had high level of self-efficacy to manage nutrition, physical exercise activity and medication were found more adherent to general diet, exercise activity, and medication taking, respectively. Patients with controlled disease were 87(22.2%). The only predictor of diabetes control was diabetes management self-efficacy [OR 2.1(1.3- 3.5), (p=0.002)].
Conclusions:
Diabetes management self-efficacy was associated with high level of education and receiving health education. Self-efficacy was significantly associated with adherence to self-care activities and glycemic control. Substantial efforts are still needed to empower the patients with self-efficacy and improving adherence to self-care activities through appropriate interventions.
Keywords: Diabetes Mellitus, Type 2, Self Efficacy, Medication Adherence, Self Care, Healthy Lifestyle, Outcome Assessment (Health Care), Multivariate Analysis, Surveys and Questionnaires, Sudan
INTRODUCTION
Diabetes mellitus (DM) is an important public health problem with a steadily increasing rate globally. In the year 2014, an estimated number of 422 million adults were living with the disease.1 Type 2 diabetes mellitus accounts for more than 90% of all diabetes globally.2
In Sudan, a recent research conducted in urban communities revealed a high rate of diabetes among adult population (19.1%) and impaired glucose tolerance (9.5%).3 Diabetes represent a significant impact in term of adverse social effects and economic burden on Sudanese patients.4
Achievement of the target therapeutic goals requires regular monitoring of blood sugar, strict adherence to both lifestyle measures and medications, and continuous management to prevent complications. Therapeutic goal achievement also needs a high capability to survive with the psychosocial challenges related to living with the disease and dynamically consuming pertinent diabetes support services.5 Multiple factors can influence glycaemic control, which can be related to the patient, the disease and the treatment.6 Studies around different parts of the world documented high prevalence of uncontrolled diabetes with multiple factors implicated in poor blood sugar control.7,8,9,10
Self-care in diabetes is an evolutionary process of developing knowledge or awareness by learning to survive with the complex nature of the disease in a social context.11 Self-care in diabetes include seven important activities, which predict the outcome of treatment, such as eating healthy diets, practicing physical exercise, monitoring of blood sugar, adherence to medications, good problem–solving skills, healthy coping skills, and risk-reduction behavior.12 Self-management is considered as the foundation of diabetes care, and it is assumed that improving patient self-management could be through enhancement of self-efficacy.13
Self-efficacy concerns with the people’s beliefs about their capabilities to produce designated levels of performance that exercise influence over events that affect their lives.14 Self-efficacy can be simplified by the interaction between behavioral, personal, and environmental factors in health and chronic disease.14,15 Self-efficacy has a positive influencing effect on self- management for many chronic health conditions.15,16 High self-efficacy was found to be associated with high self-care behavior among diabetic patients, and both had a direct effect on glycosylated hemoglobin (HbA1c).17,18,19,20 Conversely, in some studies, no significant association was documented between glucose control and self-efficacy or self-care.21,22 Moreover, educational status, employment status, family support, positive mental attitudes and diabetes education were found to have an influence on self-efficacy.
To the best of our knowledge, no previous study was conducted in Sudan among diabetic patients to correlate self-efficacy with self-management activities and identify the role of self-efficacy on glycemic control. Therefore, this study was conducted to identify the influence of management self-efficacy on adherence to self-care activities and treatment outcome among Sudanese patients with type 2 diabetes mellitus. Secondary objectives were: to measure the level of diabetes management self-efficacy, and to determine its predictors and to determine the level of disease control and to identify its determinants.
METHODS
Design and population
A cross-sectional study was conducted at two healthcare facilities in Khartoum State in Sudan (Jabir Abu Elizz Diabetes Centre and the Outpatient Clinic in Soba Teaching Hospital) from April to May 2016. The Outpatient clinic in Soba Teaching Hospital, which is located in the Southern part of Khartoum State, provides services for approximately 40000 patients per year suffering from chronic diseases. Jabir Abu Elizz Diabetes Centre, located in the central part of Khartoum State, is the only public center for diabetes in the state. The Center provides a broad range of medical services for diabetic patients. The two healthcare facilities were selected as points for data collection due to their potentiality with respect to the number of patients.
The Patients aged over 20 years and diagnosed with type 2 diabetes mellitus, at least one year before commencement of data collection were included. Patients with cognitive impairment, inability to communicate verbally, pregnant or lactating women, and patients had severe concurrent illness that limit lifestyle change were excluded. The patients consented verbally, because the research posed no risk and did not involve procedures for which written consent is normally needed. The convenience sampling method was used, because there were no well-defined registry records in both settings. The sample size was estimated to be 384 patients by using the following equation:
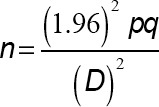
Whereas (p=Probability=0.5), (q=1-p=0.05), (D=Degree of precision=0.05, confidence level (CI)=95%).
Ethical approval for the conduction of the study was obtained from Ministry of Health – Khartoum State on 20 March 2016.
Instruments
The data was collected by the main author through face-to-face interview method using a pre-tested questionnaire. The questionnaire was developed after thoroughly searching the literature for relevant studies. Pertinent clinical parameters were extracted from the relevant patients’ records. Recent HbA1c results were extracted from the patients’ medical records. The second part was designed to collect data on patients’ self-efficacy for the management of diabetes using the Diabetes Management Self-Efficacy Scale (DMSES), which is composed of 20 items.23 DMSES assesses the extent to which a patient is confident that he or she can manage his/her blood glucose level (3 items), foot care (1 item), medication (2 item), diet (10 items), level of physical activity (3 items), and visiting the physician once a year for a checkup (1item). Responses were rated using a scale ranging from 0 (can’t do at all) to 10 (certain to do) with high scores indicating high self-efficacy. High and low general diabetes management self-efficacy and self-efficacy at different domains were measured as follow:
a.The patient was considered as having high level self-efficacy if scored equal or above the mean scores of all the participants.
b.Similarly, high level of self-efficacy at each domain (nutrition, physical exercise and medication) was defined as scores equal or higher than the mean score of all patients.
The third part of the data collection tool included the Revised Summary of Diabetes Self-care Activities (SDSCA).24 In this part, the participant was requested to report the number of days in the last 7 days in which he/she performed each self-care activity. The activities include; diet, exercise, blood glucose testing, medication taking, foot care, and smoking behavior. Adherence to the activities was defined as follows:
a. Adherence to general diet, specific diet, and physical exercise domains was defined as adherence to the determined self-care activity for at least 5 days during the past week.
b. Adherence to medication was defined as full compliance during the past week. If the patient reported less than seven days adherence to medication, he/she was considered as non-adherent.
The last part of the questionnaire was designed to record glycated hemoglobin (HbA1c). Diabetes was considered controlled if HBA1c was <7% as per both study sites protocols. The questionnaire was piloted among ten patients to ensure applicability and to estimate the time frame needed for data collection. Minor changes were suggested and finally adopted in the last version.
The questionnaire was delivered to the patients in Arabic language. The Arabic version of DMSES and SDSCA were used after obtaining the permission from Elbur et al.25 The translation was checked further to fit the Sudanese dialect. The research team also checked the questionnaire content validity.
The main outcome measures in the study were: 1) The influence of the level of diabetes management self-efficacy on diabetes self-care activities; and 2) The influence of the level of diabetes management self-efficacy on disease control. Two secondary outcome measures were also considered: 1) The level of diabetes management self-efficacy and its predictors; and 2) The level of disease control and its determinants.
Data analysis
Descriptive statistics were used to characterize the study sample. Percentage and means with standard deviation (SD) were used to describe the variables. Cronbach’s alpha was used to examine the internal consistency of DMSES and SDSCA. Logistic regression analysis was performed to determine the most significant independent variables (demographic and clinical variables) associated with diabetes self-efficacy, management, and diabetes control as dependent variables. Crude logistic regression analysis was performed as initial steps of qualifying covariates to be included in multivariate logistic regression analysis. Covariates with p-value <0.05 were eligible for inclusion in the final model. The association between self-efficacy management and adherence to self-care activities was tested by independent t test or chi-square test. P-values <0.05 were considered statistically significant. The data were processed using the software SPSS v 21.0 (SPSS Inc., Chicago IL, USA).
RESULTS
A total of 392 patients were included, with 335(85.5%) recruited from Jabir Abu Elizz Diabetes Centre and 57 (14.5%) from Soba Teaching Hospital. Male patients were 212 (54.1%) and 250 (63.8%) aged over 50 years. More than half of the participants attained an educational level between 0-9 years and 49.7% attended formal diabetes education sessions. Obese and overweight were 250 (63.8%). Table 1 showed participants characteristics.
Table 1. Patients’ sociodemographic data.
| Demographic variable | N | Percent |
|---|---|---|
| Gender | ||
| Male | 212 | 54.1 |
| Female | 180 | 45.9 |
| Age in years | ||
| <50 Years | 142 | 36.2 |
| >50 Years | 250 | 63.8 |
| Residence | ||
| Khartoum State | 279 | 71.2 |
| Other states | 113 | 28.8 |
| Educational level | ||
| 0-9 Years | 223 | 56.9 |
| >9 Years | 169 | 43.1 |
| Marital status | ||
| Married | 342 | 87.2 |
| Single | 050 | 12.8 |
| Financial support | ||
| Self | 286 | 73.0 |
| Family | 106 | 27.0 |
| Employment | ||
| Employed | 161 | 41.1 |
| Unemployed | 231 | 58.9 |
| Health insurance status | ||
| Covered | 325 | 82.9 |
| Uncovered | 067 | 17.1 |
| Body mass index (Kg/m2) | ||
| Normal | 142 | 36.2 |
| Obese & overweight | 250 | 63.8 |
| Smoking status | ||
| Smoker/Ex-smoker | 97 | 24.8 |
| Non-smoker | 295 | 75.2 |
| Duration of diabetes | ||
| 1-10 years | 209 | 53.3 |
| >10 years | 183 | 46.7 |
| Attending formal diabetes education | ||
| Yes | 195 | 49.7 |
| No | 197 | 50.3 |
| Total | 392 | 100 |
Out of all included patients, 211(53.8%) had other concomitant disease. Patients suffered from hypertension were 140 (35.7%), and 119 (30.4%) had dyslipidemia. Regarding diabetes complications, 111(28.3%) experienced retinopathy, 236 (60.2%) neuropathy, 83(21.2%) diabetic septic foot and 12 (3.1%) nephropathy.
The internal consistency of DMSES was alpha=0.9. The mean scores of self-efficacy to manage nutrition, physical exercise and weight control and medication were 67.8 (SD 17.0), 18.6 (SD 7.3) and 18.0 (SD 3.4), respectively. The mean score of diabetes management self-efficacy across all domains was 136.8 (SD 29.7). Out of all interviewed patients, 191 (48.7%) were classified as having high self-efficacy across all domains to manage diabetes. Participants with high level of self-efficacy in nutrition management, physical exercise and weight control, and medical treatments were 188 (48.0%), 199 (50.8%) and 281(71.7%), respectively.
Table 2 shows the determinants of diabetes management self-efficacy. Multivariate analysis showed that, education over 9 years, and receiving formal health educational sessions on diabetes were significantly associated with high level of diabetes management self-efficacy.
Table 2. Determinants of diabetes management self-efficacy.
| Covariates | self-efficacy | Univariate analysis | Multivariable analysis | |||
|---|---|---|---|---|---|---|
| % | n | crude OR (95% CL) | p-value | adjusted OR (95% CL) | p-value | |
| Gender | ||||||
| Female | 51.7 | 180 | 1 | |||
| Male | 46.2 | 212 | 0.8 (0.5-1.2) | 0.283 | ||
| Age group in year | ||||||
| ≤50 | 44.8 | 142 | 1 | |||
| >50 | 55.6 | 250 | 1.5 (1.0-2.3 | 0.040 | ||
| Residence | ||||||
| Other states | 42.5 | 113 | 1 | |||
| Khartoum | 51.3 | 279 | 1.4 (0.9-2.2) | 0.116 | ||
| Educational level | 0.001 | |||||
| > 9 years | 60.9 | 169 | 1 | 1 | ||
| 0-9 years | 39.5 | 223 | 0.4 (0.3-0.6) | <0.001 | 0.5 (0.3-0.7) | |
| Marital status | ||||||
| Others | 52.0 | 50 | 1 | |||
| Married | 48.2 | 342 | 0.9 (0.5-1.6) | 0.620 | ||
| Employment status | ||||||
| Unemployed | 47.2 | 231 | 1 | |||
| Employed | 50.9 | 161 | 1.2 (0.8-1.7) | 0.466 | ||
| Duration with diabetes | ||||||
| > 10 years | 48.1 | 183 | 1 | |||
| 1-10 years | 49.3 | 209 | 1.0 (0.7-1.6) | 0.813 | ||
| Attending formal diabetes education | <0.001 | |||||
| No | 36.5 | 197 | 1 | 1 | ||
| Yes | 61.0 | 195 | 2.7 (1.8-4.1) | <0.001 | 2.4 (1.6-3.7) | |
| Diabetes complication | ||||||
| No | 56.9 | 109 | 1 | |||
| Yes | 45.6 | 283 | 0.6 (0.4-1.0) | 0.046 | ||
| Total | 392 | |||||
Among the participants, 253 (64.5%), 121 (30.9%), 69 (17.6%) and 272 (69.4%) were classified as adherent to general diet, specific diet, physical exercise and treatment plan, respectively. Table 3 shows the mean number of days and the level of adherence to diabetes self-care activities.
Table 3. Mean number of days and adherence to diabetes self-care activities.
| Diabetes self-care activities | Days/adherence. Mean (SD) | Adherent |
|---|---|---|
| General diet | 5.1 (1.9) | 253 (64.5%) |
| Specific diet | 3.9 (1.9) | 121 (30.9%) |
| Physical exercise | 2.2 (2.3) | 69 (17.6%) |
| Medication taking | 6.1 (1.8) | 272 (69.4%) |
| Blood glucose testing | 1.7 (3.6) | 0 (0%) |
| Foot exams | 4.1 (3.0) | 0 (0%) |
As shown in Table 4, patients with high self-efficacy to manage nutrition, physical exercise activity and medication were found to be more adherent to general diet, exercise activity and medication taking, respectively, compared to those with low efficacy to manage these domains.
Table 4. Diabetes management self-efficacy and self-care management practice.
| Domain | Self-efficacy | Adherent | p-value | |
|---|---|---|---|---|
| High | Low | |||
| Nutrition-general diet | 143 (76.1%) | 110 (53.9%) | 253 | <0.001 |
| Nutrition- specific diet | 64 (34.0%) | 57 (27.9%) | 121 | 0.150 |
| Physical exercise | 55 (27.6%) | 14 (7.3%) | 69 | <0.001 |
| Medication taking | 242 (74.2%) | 30 (45.5%) | 272 | <0.001 |
Out of all interviewees, 87 (22.2%) achieved the target therapeutic goal and considered with controlled disease. Univariate analysis showed that the only predictor of diabetes control was diabetes management self-efficacy, as shown in Table 5. The 55 patients (28.8%) who had high self-efficacy, presented more frequently the disease controlled, compared to 32 (15.9%) with low self-efficacy, [OR 2.1 (1.3- 3.5), p=0.002).
Table 5. Determinants of diabetes control (univariate analysis).
| Disease control | crude OR (95%CI) | p-value | ||
|---|---|---|---|---|
| % | n | |||
| Gender | ||||
| Female | 20.6 | 180 | 1 | |
| Male | 33.6 | 212 | 1.2 (0.7-1.9) | 0.472 |
| Age group in year | ||||
| > 50 | 23.6 | 250 | 1 | |
| < 50 | 19.7 | 142 | 0.8 (0.5-1.3) | 0.375 |
| Residence | ||||
| Other states | 19.5 | 113 | 1 | |
| Khartoum | 23.3 | 279 | 1.2 ((0.7-2.1) | 0.409 |
| Educational level | ||||
| > 9 years | 18.3 | 169 | 1 | |
| 0-9 years | 25.1 | 223 | 1.5(0.9-2.4) | 0.111 |
| Marital status | ||||
| Others | 24.0 | 50 | 1 | |
| Married | 21.9 | 342 | 0.9 (0.4-1.8) | 0.742 |
| Employment status | ||||
| Unemployed | 22.1 | 231 | 1 | |
| Employed | 22.4 | 161 | 1.0 (0.6-1.6) | 0.947 |
| Duration with diabetes | ||||
| > 10 years | 21.3 | 183 | 1 | |
| 1-10 years | 23.0 | 209 | 1.1 (0.7-1.8) | 0.694 |
| Diabetes complication | ||||
| No | 24.8 | 109 | 1 | |
| Yes | 21.2 | 283 | 0.8 (0.5-1.4) | 0.447 |
| Self-efficacy | ||||
| Low | 15.9 | 191 | 1 | |
| No | 28.8 | 201 | 2.1 (1.3-3.5) | 0.002 |
| Total | 392 | |||
DISCUSSION
The current study is the first one of its type to investigate the influence of self-efficacy management and its influence on adherence to self-care activities and disease control among diabetic Sudanese patients. Previous studies around the world demonstrated this association, but the documentation of this association at the level of Sudanese patients might convince healthcare authorities and institutions and adopt the concept in health education aiming to change patient behavior.
Analysis of the demographic variables of the patients recruited in this study showed that approximately 30% of them were living in rural areas, where it is difficult to reach the vital services. This reflects the centralization of health services for important chronic illness like diabetes. To the best of our knowledge, there are no specialized centers to provide care for diabetic patients in other states of Sudan. This might partially explain a late diagnosis, poor diseases control, and development of complications. More than half of the respondents had education between 0-9 years, which could affect the understanding of important health education messages. Unemployed participants represented 59%, which in agreement with Von Arx et al.5 study, where most of the population was unemployed because of diabetes complications. The major observed comorbid conditions were hypertension and dyslipidemia, which might increase the microvascular and macrovascular risk in patients with diabetes, but also might increase the financial burden, which inversely could affect the adherence to medication and self-care activities.26 In our study, nearly half (48.7%) of all interviewees participated in this study were classified as having high self-efficacy across all domains to manage their diabetes, and 48.0%, 50.8% and 71.7% were classified as having a high level of self-efficacy to manage nutrition, physical exercise and weight control, and medical treatment, respectively. Comparatively, in a recent published study conducted among Saudi diabetic patients, self-efficacy was found to be moderately low.27
The most important predictors of high level of self-efficacy in our study were the participation in diabetic health education sessions and a high educational level (over 9 years). Both factors are deemed important for understanding of all aspects related to the disease, complications, medical management and the importance of adherence to lifestyle recommendations. Diabetes management self-efficacy was reported as the single most important determinant of the disease control and influenced by educational status.21 Participation in diabetes education programs was also found to be a key factor in diabetes control.28 The results of our study identified the role of self-efficacy on adherence to diabetes self-care activities across important domains of lifestyle changes. This finding was in concordance with the results of other studies conducted in China20, India21, and Native Americans and Alaska Natives.29
Our results also showed that adherence to medication was higher compared to other self-care activities (diet and exercises). In another Sudanese study also conducted in Khartoum state, the authors quoted a deficiency in knowledge about the role of adherence to both domains in the control of the disease (diet 62.3% and physical exercise 51.2%).30
Only 22% of the respondents attained the target therapeutic goal for the control of diabetes. This high percentage of uncontrolled diabetes justifies the prevalence of disease complications observed among the interviewees. The only predictor of diabetes control was self-efficacy for the management of the disease. In fact, several studies had linked high self-efficacy with performing diabetes self-care behaviors, which directly linked to glycemic control.1,17,22,31-33 Self-efficacy is commonly presented as a contribute to the adjustment of the disease and good glycemic control in the long term.20 However, the literature is not be free from controversial results, with some authors supporting that adherence to self-care management behaviors are related to poor glycemic control9 and found no significant association between social support, self-efficacy, self-care behaviors and glycemic control.34
Overall, the findings of our study reflected the importance of self-efficacy as an important determinant of adherence to self-care activities and ultimately to glycemic control. Health care facilities caring for diabetic patients in Sudan should adopt educational intervention programs to increase the level of self-efficacy and to empower patients to better participate in the management of the disease. These goals could be achieved by incorporating self-efficacy in the ongoing education process and through social support.
Limitations
Our study presented some limitations. First, the study was conducted in two settings in one state, so the results cannot be generalized to all diabetic patients at the national level. Second, the study adopted convenience sampling. And third, the self-report method was used to collect data on adherence to self-care management activities, which imply the obtained results may suffer from any bias.
CONCLUSIONS
The level of self-efficacy and adherence to self-care management were high in about half of the respondents, and there was a significant association between self-efficacy and adherence to self-care activities and level of glycemic control. Educational level and formal diabetes education were found to be significantly associated with high level of diabetes management self-efficacy. Enhancing self-efficacy and adherence to self-care activities through continuous patient education must be taken in consideration in diabetes management plan.
ACKNOWLEDGEMENT
The authors would like to thank all staff members of Jabir Abu Elizz Diabetes Centre and Soba Teaching Hospital for their unlimited helps.
Footnotes
CONFLICT OF INTEREST
None to be declared.
FUNDING
None.
Contributor Information
Fathi A. Amer, Department of Clinical Pharmacy, Faculty of Pharmacy, University of Khartoum, Khartoum, (Sudan). bakarelbu@yahoo.co.uk
Malik S. Mohamed, Department of Pharmaceutics, Faculty of Pharmacy, University of Khartoum, Khartoum, (Sudan). msmohammed@uofk.edu
Abubaker I. Elbur, Department of Pharmacy Practice, College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University. Dammam (Saudi Arabia). aisaeed@iau.edu.sa
Sulafa I. Abdelaziz, Department of medicine, Faculty of Medicine, University of Khartoum. Khartoum (Sudan). sulafibrahim1@gmail.com
Zeinab A. Elrayah, Jabir Abu Elizz Diabetes Centre. Khartoum (Sudan). znab12@gmail.com
References
- 1.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dipiro JT. Pharmacotherapy: A Pathophysiologic Approach. Ninth Edition. New York: Mc Graw Hill; 2014. Diabetes Mellitus 2014. [Google Scholar]
- 3.Elmadhoun WM, Noor SK, Ibrahim AA, Bushara SO, Ahmed MH. Prevalence of diabetes mellitus and its risk factors in urban communities of north Sudan: Population-based study. J Diabetes. 2016;8(6):839–846. doi: 10.1111/1753-0407.12364. [DOI] [PubMed] [Google Scholar]
- 4.Elrayah-Eliadarous HA, Östenson CG, Eltom M, Johansson P, Sparring V, Wahlström R. Economic and social impact of diabetes mellitus in a low-income country: A case-control study in Sudan. J Diabetes. 2017;9(12):1082–1090. doi: 10.1111/1753-0407.12540. [DOI] [PubMed] [Google Scholar]
- 5.von Arx LB, Gydesen H, Skovlund S. Treatment beliefs, health behaviors and their association with treatment outcome in type 2 diabetes. BMJ Open Diabetes Res Care. 2016;4(1):e000166. doi: 10.1136/bmjdrc-2015-000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanal T, Nair N, Adhikari P. Factors associated with poor control of type 2 diabetes mellitus: a systematic review and meta-analysis. J Diabetol. 2011;3(1):1–10. [Google Scholar]
- 7.Quah JH, Liu YP, Luo N, How CH, Tay EG. Younger adult type 2 diabetic patients have poorer glycaemic control: a cross-sectional study in a primary care setting in Singapore. BMC Endocr Disord. 2013;13:18. doi: 10.1186/1472-6823-13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghazanfari Z, Niknami S, Ghofranipour F, Larijani B, Agha-Alinejad H, Montazeri A. Determinants of glycemic control in female diabetic patients: a study from Iran. Lipids Health Dis. 2010;9:83. doi: 10.1186/1476-511X-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complications. 2010;24(2):84–89. doi: 10.1016/j.jdiacomp.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 10.Siddiqui FJ, Avan BI, Mahmud S, Nanan DJ, Jabbar A, Assam PN. Uncontrolled diabetes mellitus: prevalence and risk factors among people with type 2 diabetes mellitus in an urban district of Karachi, Pakistan. Diabetes Res Clin Pract. 2015;107(1):148–156. doi: 10.1016/j.diabres.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 11.Paterson B, Thorne S. Developmental evolution of expertise in diabetes self-management. Clin Nurs Res. 2000;9(4):402–419. doi: 10.1177/10547730022158663. [DOI] [PubMed] [Google Scholar]
- 12.American Association of Diabetes Educators. AADE7 Self-Care Behaviors. Diabetes Educ. 2008;34(3):445–449. doi: 10.1177/0145721708316625. [DOI] [PubMed] [Google Scholar]
- 13.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Self-efficacy: The Exercise of Control. New York: Prentice-Hall; 1994. [Google Scholar]
- 15.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 16.Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 17.Beckerle CM, Lavin MA. Association of self-efficacy and self-care with glycemic control in diabetes. Diabetes Spectrum. 2013;26(3):172–178. doi: 10.2337/diaspect.26.3.172. [DOI] [Google Scholar]
- 18.Fortmann AL, Gallo LC, Walker C, Philis-Tsimikas A. Support for disease management, depression, self-care, and clinical indicators among Hispanics with type 2 diabetes in San Diego County, United States of America. Rev Panam Salud Publica. 2010;28(3):230–234. doi: 10.1590/s1020-49892010000900014. [DOI] [PubMed] [Google Scholar]
- 19.Gao J, Wang J, Zheng P, Haardorfer R, Kegler MC, Zhu Y, Fu H. Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC Fam Pract. 2013;14:66. doi: 10.1186/1471-2296-14-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cosansu G, Erdogan S. Influence of psychosocial factors on self-care behaviors and glycemic control in Turkish patients with type 2 diabetes mellitus. J Transcult Nurs. 2014;25(1):51–59. doi: 10.1177/1043659613504112. [DOI] [PubMed] [Google Scholar]
- 21.Venkataraman K, Kannan AT, Kalra OP, Gambhir JK, Sharma AK, Sundaram KR, Mohan V. Diabetes self-efficacy strongly influences actual control of diabetes in patients attending a tertiary hospital in India. J Community Health. 2012;37(3):653–662. doi: 10.1007/s10900-011-9496-x. [DOI] [PubMed] [Google Scholar]
- 22.Reisi M, Mostafavi F, Javadzade H, Mahaki B, Tavassoli E, Sharifirad G. Impact of health literacy, self-efficacy, and outcome expectations on adherence to self-care behaviors in Iranians with type 2 diabetes. Oman Med J. 2016;31(1):52–59. doi: 10.5001/omj.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bijl JV, Poelgeest-Eeltink AV, Shortridge-Baggett L. The psychometric properties of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus. J Adv Nurs. 1999;30(2):352–359. doi: 10.1046/j.1365-2648.1999.01077.x. [DOI] [PubMed] [Google Scholar]
- 24.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 25.Elbur AI, AlMalk IAS, Alharthi SA. Self-efficacy, self-care activities management and treatment outcome among type 2 diabetes Saudi patients: across-sectional study. J Pharm Nutrit Sci. 2017;7:48–54. [Google Scholar]
- 26.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317(7160):703–713. doi: 10.1136/bmj.317.7160.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ALAboudi IS, Hassali MA, Shafie AA, Saleem F. Self-efficacy, self-care behaviours and glycaemic control in type 2 diabetic patients in Riyadh, Saudi Arabia. J Public Health. 2016;24(4):281–291. doi: 10.1007/s10389-016-0723-x. [DOI] [Google Scholar]
- 28.Al-Khawaldeh OA, Al-Hassan MA, Froelicher ES. Self-efficacy, self- management, and glycemic control in adults with type 2 diabetes mellitus. J Diabetes Complications. 2012;26(1):10–16. doi: 10.1016/j.jdiacomp.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 29.DePalma MT, Trahan LH, Eliza JM, Wagner AE. The Relationship between Diabetes Self-efficacy and Diabetes Self-care in American Indians and Alaska Natives. Am Indian Alsk Native Ment Health Res. 2015;22(2):1–22. doi: 10.5820/aian.2202.2015.1. [DOI] [PubMed] [Google Scholar]
- 30.Taha HA. Assessment of knowledge about the role of diet regime and physical exercise to control diabetes among type 2 Diabetic Patients in Khartoum State, Sudan. Int J Med Sci Public Health. 2014;3:916–921. doi: 10.5455/ijmsph.2014.090520141. [DOI] [Google Scholar]
- 31.Wynn Nyunt S, Howteerakul N, Suwannapong N, Rajatanun T. Self-efficacy, self-care behaviors and glycemic control among type-2 diabetes patients attending two private clinics in Yangon, Myanmar. Southeast Asian J Trop Med Public Health. 2010;41(4):943–951. [PubMed] [Google Scholar]
- 32.Lee YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns. 2016;99(2):287–294. doi: 10.1016/j.pec.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 33.Walker RJ, Smalls BL, Hernandez-Tejada MA, Campbell JA, Egede LE. Effect of diabetes self-efficacy on glycemic control, medication adherence, self-care behaviors, and quality of life in a predominantly low-income, minority population. Ethn Dis. 2014;24(3):349–355. [PMC free article] [PubMed] [Google Scholar]
- 34.Chlebowy DO, Garvin BJ. Social support, self-efficacy, and outcome expectations: impact on self-care behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. Diabetes Educ. 2006;32(5):777–786. doi: 10.1177/0145721706291760. [DOI] [PubMed] [Google Scholar]


