Abstract
The objective of this review was to investigate the efficacy of dental local anesthetics, as it is well known among clinicians that local anesthesia may be challenging in some circumstances. Therefore, the focus of this review was on the efficacy of the products used in dental local anesthesia.
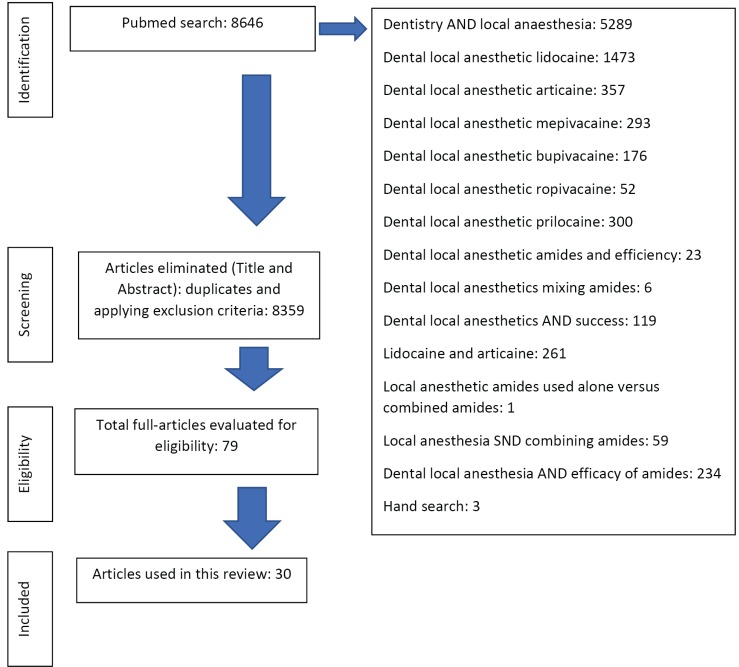
In a Pubmed database literature search conducted, a total of 8646 articles were found to be related to dental local anesthetics. After having applied the inclusion criteria (human research, performed in the last 10 years, written in English language, and focus on dental local anesthetics) and having assessed the quality of the papers, 30 were deemed eligible for inclusion in this review.
The conclusion of this review is that none of the dental local anesthetic amides provide 100% anesthesia. The problem appears to be more pronounced when mandibular teeth are attempted to be anaesthetized and especially if there is irreversible pulpitis involved. The authors conclude that this finding suggest exploration of more efficient techniques to administer dental local anesthesia, especially in the mandible, to establish a 100% efficacy, is needed.
Keywords: Amides, Local Anesthesia
INTRODUCTION
Local anesthesia in dentistry provides comfort for the patient, but also as much comfort for the clinician as the planned procedures can be carried out under the best possible conditions. From clinical experience and from the literature, it is clear that dental local anesthesia is not always as successful as anticipated [1,2,3,4,5,6,7,8]. Especially mandibular block anesthesia can be difficult to achieve or challenging in some patients, even in the absence of a tooth with an acute pulpitis. Mandibular block failure rates differ from study to study and teach us that there is no 100% success [1,2,3,7]. The efficacy of local anesthesia in the maxilla is much higher, based on clinical experience and publications. The main reason is probably the cortical plates of the mandible being thicker and denser and having less porosities that allow for a volume of local anesthetic to be diffused into the cancellous bone in case one attempts a buccal infiltration for instance, explains most of the difference with the maxilla. Another reason is the techniques that are used to achieve local anesthesia. In the maxilla, the most appropriate technique would be a buccal infiltration anesthesia close to the level of the apices of the teeth, while in the mandible, because of the reason mentioned above, local anesthesia is achieved mainly by attempting to deposit a volume of local anesthetic close to the mandibular nerve before it enters the mandible [6,7,9,10]. Because of anatomical variations in localisation of the second branch of the trigeminal nerve with regard to the ramus of the mandible, the efficacy of local anesthesia is not 100% [1,2,3,4,5,6,7,8,9,10,11].
The aim of this current review was to assess the peer-reviewed literature on the topic of dental local anesthetics to see if the efficacy of dental local anesthetics depends on the amide or a combination of amides used.
MATERIAL AND METHODS
Fig. 1 shows which search terms were used in the PubMed® database to identify relevant publications, how many publications were found per search term and how publications were finally triaged to be reviewed by both researchers. The inclusion criteria used, were that studies had to be related to human research, performed in the last 10 years, written in English language, and with a focus on dental local anesthetics. After having identified the search terms, the search was conducted between January 2017 and January 2018 by one researcher (NB). As can be derived from Fig. 1, an initial total of 8646 manuscripts were identified. After applying the selection criteria, 79 papers were subsequently read by both researchers, and then categorised in consensus in an Excel spread sheet (Microsoft®, Redmond, Washington, USA) to identify the type of study (e.g. randomised clinical trial), the amides investigated (e.g. articaine), the number of patients included in the study if it was a clinical trial, the country of origin and the year of publication and finally, the conclusion of the study. Both investigators read all 79 publications, and, in consensus, deemed 30 manuscripts eligible for the study's aim.
Fig. 1. The decision process of the review explained, mentioning the number of papers collected, assessed and reviewed.
RESULTS
A total of 30 publications (Fig. 1) were considered relevant for the study: 7 reviews, and 23 clinical trials.
The details of the different studies and their conclusions can be found in Tables 1 and 2. These tables show data regarding the country of origin, the number of subjects involved, which amides were investigated and in the last column the final conclusions as stated in the respective papers. Table 3 tabulates the number of manuscripts that investigated which type of amide and which amide was found to be more or equally in efficacy to achieve local anesthesia. The numbers in the right hand side column refer to the manuscripts reference list.
Table 1. Review papers included in this current review, indicating reference, year of publication, type of amides involved, type of anesthesia involved and conclusion of the study.
| Authors, Country, Year | Type of study | Amid and Vasoconstrictor Concentrations | Anesthesia Techniques Used | Conclusion of Study |
|---|---|---|---|---|
| Su N et al. China, 2014 [12] | meta-analysis of randomised controlled trials | • 2% lidocaine and 1:100k epinephrine | • Inferior alveolar nerve block | Given the efficacy and safety of the two solutions, 2% mepivacaine with vasoconstrictors is better than 2% lidocaine with vasoconstrictors in dental treatment. Meanwhile, 3% plain mepivacaine is better for patients with cardiac diseases. |
| • 3% mepivacaine plain | • infiltration | |||
| • 2% mepivacaine and 1:100k epinephrine | • Maxillary block | |||
| • 2% mepivacaine and 1:20k levonordefrin | • intraosseous | |||
| • 2% lidocaine and 1:50k epinephrine | • intraligamentary | |||
| Su N et al. China, 2014 [14] | meta-analysis of randomised controlled trials | • 2% lidocaine and 1:100k epinephrine | • Inferior alveolar nerve block | There was no statistical significance in adverse events between two groups. Given the efficacy and safety, the bupivacaine group is better than the lidocaine group in dental operations that take a relatively long time, especially in endodontic treatments or where there is a need for postoperative pain management. |
| • 0.5% bupivacaine and 1:200k epinephrine | • infiltration | |||
| • 2% lidocaine and 1:80k epinephrine | ||||
| • 0.75% bupivacaine and 1:200k epinephrine | ||||
| • 0.75% levobupivacaine plain | ||||
| • 0.5% levobupivacaine plain | ||||
| Katyal V, Australia, 2010 [42] | meta-analysis | • 4% articaine and 1:100k epinephrine | • Inferior alveolar nerve block | Articaine is more likely than lignocaine to achieve an anesthetic success in the posterior fist molar area with a relative risk for success at 1.31. The results of this systematic review provide support for the argument that articaine is more effective than lignocaine in providing anesthetic success in the fist molar region for routine dental procedures. In addition, both drugs appear to have similar adverse effect profies. The clinical impact of articaine's higher post-injection pain scores than lignocaine is negligible. Hence, articaine is a superior anesthetic to lignocaine for use in routine dental procedures. Use in children under 4 years of age is not recommended, since no data exists to support such usage. |
| • 2% lignocaine and 1:100k epinephrine | • infiltrations in maxilla and mandible | |||
| Kung J et al. USA, 2015 [43] | systematic review and meta-analysis | unclear | • Inferior alveolar nerve block | For combined studies, articaine was more likely than lidocaine to achieve successful anesthesia. Maxillary infiltration subgroup analysis showed no significant difference between articaine and lidocaine. For combined mandibular anesthesia studies articaine was superior to lidocaine, with further subgroup analysis showing no difference for mandibular block anesthesia. When used for supplemental infiltration after successful mandibular block anesthesia, articaine was significantly more effective than lidocaine. There were no reports of adverse events. In conclusion, the present meta-analysis showed that in patients with symptomatic irreversible pulpitis, articaine is as effective as lidocaine when used for mandibular block or maxillary infiltration anesthesia. In cases of persistent pulpal pain despite successful mandibular block anesthesia, supplementary infiltration with articaine instead of lidocaine has 3.55 times greater likelihood of achieving successful anesthesia. |
| • infiltration | ||||
| Su N et al. China, 2016 [44] | systematic review and meta-analysis | • 2% lidocaine and 1:100k epinephrine | Not specified | In comparison with 2% lidocaine with 1:100 000 epinephrine, 4% articaine with 1:100 000 epinephrine showed a higher success rate in anesthesia of irreversible pulpitis at either person, lower VAS scores during injection phase and treatment phase, shorter onset time of pulpal anesthesia and lower percentage of patients undergoing adverse events. Given the efficacy and safety of the two solutions, 4% articaine with 1:100 000 epinephrine was superior to 2% lidocaine with 1:100 000 epinephrine in dental treatments in irreversible pulpitis. |
| • 4% articaine and 1:100k epinephrine | ||||
| Hillerup S et al. Denmark, 2011 [39] | review | unclear | • Inferior alveolar nerve block | The significant overrepresentation of neurosensory disturbances associated with articaine 4 percent is related mainly to mandibular blocks. The statistically significant overrepresentation of articaine 4 percent formulations in so-called “double injuries” indicates that properties of the injected substance are the causative agent through neurotoxicity. The prudent approach is to avoid high-concentration anesthetic formulations (that is, 4 percent) for block anesthesia in the trigeminal area. |
| • Infiltrations | ||||
| Garisto GA et al. USA (authors Canadian), 2010 [40] | review | yes, but not specified | Not applicable | The findings of our study confirm that paresthesia arising from a local anesthetic injection alone is a rare event. Nevertheless, the findings we report herein support those published previously and show that the 4 percent anesthetic solutions used in dentistry, namely prilocaine and articaine, are more highly associated with the development of paresthesia than are those of lower concentration. |
Table 2. In vivo and in vitro papers included in this current review, indicating reference, year of publication, type of amides involved, type of anesthesia involved and conclusion of the study.
| Authors, Country, Year | Type of study | Amid and Vasoconstrictor Concentrations | Technique Used: Block or Infiltration? Mandibular or Maxillary? | Number of Subjects in Study | Conclusion of Study |
|---|---|---|---|---|---|
| Colombini BL et al. Brazil, 2006 [45] | randomised double blind cross-over study | • 4% articaine and 1:100k epinephrine | Inferior alveolar nerve block (third molar removal) | 20 | Articaine provides a longer period of analgesic effect and a tendency for a longer period of anesthesia as compared to mepivacaine. The presence of a vasoconstrictor agent in local anesthetic solutions does not seem to influence hemodynamic parameters during lower third molar removal in healthy subjects. |
| • 2% mepivacaine and 1:100k epinephrine | |||||
| Jain NK et al. India, 2016 [31] | comparative prospective | • 4% articaine and 1:100k epinephrine | Inferior alveolar nerve block (third molar surgical removal) | 70 | Results showed that 4% articaine had a significant faster onset and longer duration of action when compared to 2% lignocaine. We concluded that 4% articaine is a safe alternative to 2% lignocaine, which is potent and effective in minor surgical procedures such as removal of mandibular third molars. |
| • 2% lignocaine and 1:80k epinephrine | |||||
| Pellicer-Chover H et al. Spain, 2013 [46] | comparative split mouth | • 4% articaine and 1:100k epinephrine | Inferior alveolar nerve block (third molar surgical removal) | 36 | Articaine showed greater clinical efficacy than bupivacaine, reducing latency time, bleeding, anesthetic duration in the soft tissues and achieving higher anesthetic quality, requiring less reinforcement during surgery than bupivacaine. |
| • 0.5% bupivacaine and 1:200k epinephrine | |||||
| Budharapu A et al. India, 2015 [18] | randomised single blind trial | • 0.5% ropivacaine | Inferior alveolar nerve block (third molar surgical removal) | 78 | We had no adverse effects from 0.5% ropivacaine, which provided efficient anesthesia and excellent residual analgesia with no cardiovascular or central nervous system complications. The addition of adrenaline to ropivacaine has been shown not to improve the anesthetic effect and may cause transient increases in arterial pressure and heart rate. Evaluation of the plasma concentration would give more details about its effects on the cardiovascular system, as we confined ourselves to studying only the haemodynamic changes. |
| • 2% lignocaine | |||||
| Brkovic BM et al. Serbia, 2010 [17] | double blind randomised controlled design | • 0.5% ropivacaine plain | infiltration (third molars maxilla) | 66 | In conclusion, the current data suggest that maxillary infiltration of 0.75 and 1% of ropivacaine offered adequate and safe intraoperative analgesia but not successful postoperative pain control for the surgical removal of upper third molars. |
| • 0.75% ropivacaine plain | |||||
| • 1% ropivacaine plain | |||||
| Christensen J et al. Denmark, 2013 [15] | randomised double blind cross over design | • 2% lidocaine with or without methylprednisolone or placebo | Inferior alveolar nerve block (third molar surgical removal) | 126 | Bupivacaine combined with methylprednisolone reduced the postoperative pain and swelling compared with the use of lidocaine and placebo, lidocaine and methylprednisolone, or bupivacaine and placebo. (two to four supplemental injections were administered sometimes) |
| • 0.5% bupivacaine with or without methylprednisolone or placebo | |||||
| Krzeminski TF et al. Poland, 2011 [25] | randomised parallel group trial | • 0.5% ropivacaine plain | infiltration maxillary incisors and canines | 60 | The efficacy of anesthesia of lateral and central incisors was 100% for both anesthetics. There were insignificant differences in effectiveness of canine pulp anesthesia. Ropivacaine (0.5%) achieved effective and long duration of uninflamed pulp and soft tissue anesthesia. Ropivacaine could be useful for long-lasting operative procedures without the need for a vasoconstrictor. |
| • 4% articaine and 1:100k epinephrine | |||||
| Thakare A et al. India, 2014 [47] | randomised cross-over study | • 4% articaine | infiltration in maxilla (premolar extractions) | 40 | The results showed that 4% articainehad significantly faster onset of action and lower VAS scores when compared with bupivacaine. However, the duration of analgesia and time to first rescue analgesic medication was longer in the bupivacaine group. Articaine seemed to have better potency and efficacy in terms of onset of action and lower pain scores compared to the bupivacaine group. Further studies are required to confirm these results. Moreover, the volume of LA required seemed to be lower in the articaine group, demonstrating better anesthetic potency and efficacy. |
| • 0.5% bupivacaine | |||||
| • [epinephrine concentration unclear] | |||||
| Ashraf H et al. Iran, 2013 [48] | randomised double blind study | • 2% lidocaine and 1:100k epinephrine | • Inferior alveolar nerve block | 125 | Supplementing an incomplete articaine inferior alveolar nerve block with articaine infiltration raises the anesthetic success more effectively compared with lidocaine in mandibular molars with irreversible pulpitis. The success rate after the administration of the infiltration injections after an incomplete inferior alveolar nerve blockby using lidocaine was 29%, whereas by using articaine it was 71%. No statistical differences were detected in the success rates between the 2 anesthetics after the block injections. |
| • 4% articaine and 1:100k epinephrine | • infiltration | ||||
| Brkovic B et al. Serbia, 2008 [49] | randomised double blind | • 2% lidocaine and clonidine (15ug/mL) | infiltration (maxilla) | 40 | The results of this study indicate for the first time in dental anesthesia that the lidocaine + clonidine combination could be a useful and safe alternative to lidocaine + epinephrine for intraoral infiltration anesthesia. |
| • 2% lidocaine and epinephrine (12.5 ug/mL) | |||||
| Piccinni C et al. Italy, 2015 [16] | case-non-cas e study | unclear about concentrations of: | NA | 17246 | In conclusion, among local anesthetics, only articaine and prilocaine generated a signal of paresthesia, especially when used in dentistry. The highest number of reports was found for lidocaine (247 reports), followed by bupivacaine (99 reports), articaine (85 reports), combination of different local anesthetics (45 reports) and prilocaine (30 reports). A significant disproportionality of ‘paresthesias and dysaesthesias’ was found for articaine and prilocaine. Other local anesthetics did not show disproportionality signals according to the defined thresholds. |
| • lidocaine | |||||
| • bupivacaine | |||||
| • articaine | |||||
| • prilocaine | |||||
| Lammers E, et al. USA, 2014 [26] | prospective, randomised, double blind study | • 2% lidocaine with 1:100k epinephrine | Inferior alveolar nerve block | 100 | The combination of 3% mepivacaine plus 2% lidocaine with 1:100,000 epinephrine was equivalent to the combination of 2 cartridges of 2% lidocaine with 1:100,000 epinephrine in terms of injection pain, onset time, and pulpal anesthetic success for the IAN block. |
| • 2% lidocaine with 1:100k epinephrine | |||||
| Visconti RP et al. Brasil, 2016 [13] | double blind randomised clinical trial | • 2% mepivacaine and 1:100k epinephrine | Inferior alveolar nerve block (irreversible pulpitis) | 42 | All patients tested reported lip anesthesia after application of either type of inferior alveolar nerve block. Pulpal anesthesia success rates measured by using the pulp tester were satisfactory for both solutions (86% for mepivacaine and 67% for lidocaine). Success rates according to patient report of no pain or mild pain during pulpectomy were higher for mepivacaine solution (55%) than for lidocaine solution (14%). The differences between mepivacaine and lidocaine were statistically significant. Mepivacaine resulted in effective pain |
| • 2% lidocaine and 1:100k epinephrine | |||||
| Whitcomb M et al. USA, 2010 [32] | prospective, randomised, double blind | • 2% lidocaine and 1:100k epinephrine | Inferior alveolar nerve block | 40 | For the buffered 2% lidocaine with 1: 100,000 epinephrine/sodium bicarbonate formulation, successful pulpal anesthesia ranged from 10 to 71%. For the unbuffered 2% lidocaine with 1: 100,000 epinephrine formulation, successful pulpal anesthesia ranged from 10 to 72%. We concluded that buffering a 2% lidocaine with 1: 100,000 epinephrine with sodium bicarbonate, as was formulated in the current study, did not statistically increase anesthetic success, provide faster onset, or result in less pain of injection when compared with unbuffered 2% lidocaine with 1: 100,000 epinephrine for an IAN block. |
| • 2% lidocaine buffered with sodium bicarbonate | |||||
| Kanaa MD et al. UK, 2012 [28] | randomised, double blind study | • 4% articaine and 1:1000k epinephrine | infiltration (maxilla and irreversible pulpitis) | 100 | There was no significant difference in efficacy between 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1:80,000 epinephrine in achieving anesthesia in maxillary teeth with irreversible pulpitis after buccal infiltration. |
| • 2% lidocaine and 1:80k epinephrine | |||||
| Mohajeri L et al. Iran, 2015 [36] | randomised, double blind, clinical trial | • 2% lidocaine and 1:100k epinephrine with sterile distilled water | intraligamentary injections | 60 | Within the limitations of the present study, it appears that the addition of meperidine as an opioid to 2% lidocaine with 1 : 100,000 epinephrine will not improve the anesthetic efficacy of a periodontal ligament injection in patients with irreversible pulpitis for whom an inferior alveolar nerve block was ineffective despite lip numbness. |
| • 2% lidocaine and 1:100k epinephrine with 5% meperidine | |||||
| Gazal G, Saudi Arabia, 2017 [50] | randomised, double blind cross over study | • 4% articaine and 1:100k epinephrine | • Inferior alveolar nerve block | 23 | Articaine has better potency, rapid onset of action, earlier lip and teeth numbness compared to the mepivacaine group. Articaine/mepivacaine buccal injection was significantly more comfortable than mepivacaine inferior alveolar nerve block. |
| • 2% mepivacaine and 1:100k epinephrine | • Buccal infiltration | ||||
| Srinivasan N et al. India, 2009 [51] | prospective, randomised, double blind study | • 4% articaine and 1:100k epinephrine | infiltration (maxilla and irreversible pulpitis) | 40 | The success rate for maxillary buccal infiltration to produce pulpal anesthesia using articaine was 100% in first premolar and first molar, and for the lidocaine solution, success rate was 80% in first premolar and 30% in first molar. |
| • 2% lidocaine and 1:100k epinephrine | |||||
| Glenn B et al. USA, 2016 [38] | prospective, randomised, double blind trial | • liposomal bupivacaine | • buccal infiltrations | 100 | The success rate was 29%for the liposomal group and 22% for the bupivacaine group, with no significant difference between the groups. |
| • 0.5% bupivacaine and 1:200k epinephrine | • inferior alveolar nerve block | ||||
| • 2% lidocaine and 1:100 epinephrine | • infiltration (maxilla) | ||||
| Schellenbe rg J et al. USA, 2015 [33] | prospective, randomised, double blind trial | • 4% articaine buffered with sodium bicarbonate and 1:100k epinephrine | Inferior alveolar nerve block | 100 | The success rate for the inferior alveolar nerve block was 32% for the buffered group and 40% for the non buffered group, with no significant difference between the groups. |
| • 4% articaine and 1:100k epinephrine | |||||
| Shurtz R et al. USA, 2015 [34] | prospective, randomised, double blind trial | • 4% articaine buffered with sodium bicarbonate and 1:100k epinephrine | infiltration (mandible) | 80 | Buffered articaine did not provide any advantage over non buffered articaine for anesthetic success, anesthesia onset, or pain of injection for a primary buccal infiltration of the mandibular first molar. |
| • 4% articaine and 1:100k epinephrine | |||||
| Nydegger B et al. USA, 2014 [52] | prospective, randomised, double blind trial | • 4% articaine and 1:100k epinephrine | infiltration (mandible) | 60 | The success rate for the 4% articaine formulation was 55%, 33% for the 4% lidocaine formulation, and 32% for the 4% prilocaine formulation. There was a significant difference between articaine and both lidocaine and prilocaine formulations. |
| • 4% lidocaine and 1:100k epinephrine | |||||
| • 4% prilocaine 1:200k epinephrine | |||||
| Rogers BS et al. USA, 2014 [53] | prospective, randomised, double blind trial | • 4% lidocaine and 1:100k epinephrine | • Inferior alveolar nerve block (irreversible pulpitis) | 100 | Seventy-four patients failed to achieve pulpal anesthesia after inferior alveolar nerve block with 4% articaine, resulting in inferior alveolar nerve block success rate of 26%. Success rates for supplemental buccal infiltrations were 62% for articaine and 37% for lidocaine, which was a significant statistical difference. This effect was most pronounced and significant in second molars. |
| • 2% lidocaine and 1:100k epinephrine | • Buccal infiltration | ||||
| Cohen H et al. USA, 2013 [37] | prospective, randomised, single blind trial | • 1.72 mL 4% lidocaine and 50 ug/mL epinephrine | Inferior alveolar nerve block | 40 | We concluded that adding 0.9 M mannitol to a lidocaine with epinephrine formulation was significantly more effective in achieving a greater percentage of total pulpal anesthesia (as defined in this study) than a lidocaine formulation without mannitol. However, the 0.9 M mannitol/lidocaine formulation would not provide 100% pulpal anesthesia for all the mandibular teeth. |
| • 5 mL 68.8 mg lidocaine with 50 ug epinephrine plus 0.9 M mannitol | |||||
| Martin M et al. USA, 2011 [29] | prospective, randomised, cross-over design | 4% lidocaine and 1:100k epinephrine | infiltration (mandible) | 86 | The anesthetic efficacy of 3.6 mL 4% articaine with 1:100,000 epinephrine is better than 1.8 mL of the same anesthetic solution in a primary mandibular buccal infiltration of the first molar. However, the success rate of 70% is not high enough to support its use as a primary injection technique in the mandibular first molar. |
| McEntire M et al. USA, 2011 [54] | prospective, randomised, double blind cross-over trial | • 4% lidocaine and 1:200k epinephrine | infiltration (mandible) | 86 | The two 4% articaine formulations showed no statistically significant difference when comparing anesthetic success, onset of anesthesia, or incidence of pulpal anesthesia. |
| • 4% lidocaine and 1:100k epinephrine | |||||
| Wali M et al. USA, 2010 [55] | prospective, randomised, single blind trial | • 2% lidocaine and 1:50k epinephrine | Inferior alveolar nerve block | 30 | Increasing the epinephrine concentration to 1:50,000 epinephrine or increasing the volume to 3.6 mL of 2% lidocaine with 1:50,000 epinephrine did not result in more successful pulpal anesthesia when compared with 1.8 mL of 2% lidocaine with 1:100,000 epinephrine by using the inferior alveolar nerve block. |
| • 2% lidocaine and 1:100k epinephrine | |||||
| Goodman A et al. USA, 2006 [35] | prospective, randomised, single blind cross-over trial | • 4% lidocaine and 18 ug/ 1.8 mL epinephrine | Inferior alveolar nerve block | 52 | We conclude that the addition of meperidine to a standard lidocaine solution does not increase the success of the inferior alveolar nerve block. |
| • 4% lidocaine and 36 ug/3.6 mL epinephrine and 36 mg meperidine | |||||
| Brunetto PC et al. Brasil, 2008 [30] | randomised, double blind cross-over study | 2% lidocaine and 1:100k epinephrine | infiltration (maxilla) | 25 | It is concluded that maxillary infiltration anesthesia with lidocaine and epinephrine has a faster onset, a greater success rate, and a longer duration when a volume of 1.2 mL is used than when volumes less than 1.0 mL are used. |
| Poorni S et al. India, 2011 [20] | prospective randomised double blind clinical trial | • 4% articaine and 1:100k epinephrine | • Inferior alveolar nerve block | 156 | To summarize, on the basis of the results of the present study, it can be concluded that there is no statistically significant difference among inferior alveolar nerve block and infiltration of articaine when compared with inferior alveolar nerve block of lidocaine in mandibular molars with irreversible pulpitis. Hence compared with inferior alveolar block, buccal infiltration can be considered a viable alternative to secure pulpal anesthesia for endodontic therapy. |
| • 2% lidocaine and 1:100k epinephrine | • infiltration (mandible) | ||||
| Evans G et al. USA, 2008 [56] | prospective, randomised double blind study | • 4% articaine and 1:100k epinephrine | infiltrations (maxilla) | 80 | In conclusion, a maxillary infiltration of 4% articaine with 1:100,000 epinephrine statistically improved anesthetic success when compared with 2% lidocaine with 1:100,000 epinephrine in the lateral incisor but not in the first molar. Neither solution provided pulpal anesthesia for 1 hour. |
| • 2% lidocaine and 1:100k epinephrine | |||||
| Sreekumar K et al. India, 2011 [27] | randomised double blind cross over study | 4% articaine and 1:100k epinephrine | infiltration (maxilla) | 10 | Maxillary infiltration anesthesia with articaine and epinephrine has a faster onset, a greater success rate, and a longer duration when a volume of 1.2 mL is used than when volumes less than 1.0 mL are used. Palatal tissues were anesthetized with the highest concentration (1.2 mL) in our study (30% of cases). |
| Sampaio RM et al. Brasil, 2012 [21] | randomised double blind study | • 0.5% bupivacaine and 1:200k epinephrine | Inferior alveolar nerve block | 70 | Neither of the solutions resulted in an effective pain control during irreversible pulpitis treatments of mandibular molars. Before initiation of the pulpectomy procedure, 15 patients (42.9%) in the lidocaine group and 7 patients (20%) in the bupivacaine group exhibited pulpal anesthesia (ie, a negative response to electrical stimuli generated with an electric pulp tester). A significant difference between the 2 experimental groups for the pulpal anesthesia was observed, with more individuals in the lidocaine group presenting a negative response to electrical stimuli. During the pulpectomy, 7 patients in the bupivacaine group (20%) and 13 in the lidocaine group (37.1%) reported pain, however this difference was not statistically significant. |
| • 2% lidocaine and 1:100k epinephrine | |||||
| Mason R et al. USA, 2009 [22] | prospective, randomised, double-blind study | • 2% lidocaine and 1:100 epinephrine | infiltrations (maxilla) | 60 | Anesthetic success and the onset of pulpal anesthesia were not significantly different between 2% lidocaine with either 1:100,000 or 1:50,000 epinephrine and 3% mepivacaine for the lateral incisor and first molar. Increasing the epinephrine concentration from 1:100,000 to 1:50,000 in a 2% lidocaine formulation significantly decreased pulpal anesthesia of short duration for the lateral incisor but not the first molar. For both the lateral incisor and first molar, 3% mepivacaine significantly increased pulpal anesthesia of short duration compared with 2% lidocaine with either 1:100,000 or 1:50,000 epinephrine. |
| • 2% lidocaine and 1:50k epinephrine | |||||
| • 3% mepivacaine plain | |||||
| Forloine A et al. USA, 2010 [23] | prospective, randomised, double-blind study | • 2% lidocaine and 1:100 epinephrine | Maxillary block | 50 | The high tuberosity approach to the maxillary second division nerve block with both anesthetic formulations resulted in a high success rate (92%–98%) for the first and second molars. Approximately 76%–78% of the second premolars were anesthetized with both anesthetic formulations. Both anesthetic formulations were ineffective for the anterior teeth and first premolars. The use of 3% mepivacaine provided a significantly shorter duration of pulpal anesthesia than 2% lidocaine with 1:100,000 epinephrine in the molars and premolars. |
| • 3% mepivacaine plain | |||||
| Lawaty I et al. USA, 2010 [24] | prospective, randomised, double-blind study | • 2% mepivacaine and 1:20k levonordefrin | infiltration (maxilla) | 60 | Anesthetic success (obtaining 2 consecutive 80 readings with the electric pulp tester within 10 minutes ) was not significantly different between 2% mepivacaine with 1 : 20,000 levonordefrin and 2% lidocaine with 1 : 100,000 epinephrine for the central incisor and first molar. However, neither anesthetic agent provided an hour of pulpal anesthesia. |
| • 2% lidocaine and 1:100k epinephrine | |||||
| Berberich G et al. USA, 2009 [19] | prospective, randomised, double-blind study | • 2% lidocaine and 1:100k epinephrine | intraoral, infraorbital nerve block | 40 | The intraoral, infraorbital nerve block was ineffective in providing profound pulpal anesthesia of the maxillary central incisor, lateral incisor, and first molar. Successful pulpal anesthesia of the canine and first and second premolars ranged from 75%–92% by using 2% lidocaine with 1:100,000 and 1:50,000 epinephrine. However, pulpal anesthesia did not last for 60 minutes. The use of 3% mepivacaine provided a shorter duration of anesthesia than the lidocaine formulations with epinephrine in the canines and premolars. |
| • 2% lidocaine and 1:50k epinephrine | |||||
| • 3% mepivacaine plain | |||||
| Boonsiriseth K et al. Thailand, 2017 [57] | randomised single blind comparative split mouth design | • 4% lidocaine and 1:100k epinephrine | Inferior alveolar nerve block | 22 | The use of 4% articaine for the inferior alveolar nerve block was clinically more effective in the onset of subjective and objective anesthesiaas compared with the use of 4% lidocaine. |
| • 4% articaine and 1:100k epinephrine |
Table 3. Efficacy comparisons of amides in the literature (“>” indicating a higher efficacy and “=” indicating an equal efficacy).
| Comparing efficacy | Literature list reference |
|---|---|
| Articaine > Mepivacaine | [45], [50] |
| Articaine > Lidocaine | [31], [42], [43], [48], [16], [44], [32], [52], [53], [56], [57] |
| Articaine > Bupivacaine | [46], [47], [16] |
| Articaine > Prilocaine | [51] |
| Articaine = Lidocaine | [20] |
| Lidocaine > Mepivacaine | [19] |
| Mepivacaine > Lidocaine | [12], [13] |
| Mepivacaine = Lidocaine | [22], [23], [24] |
| Bupivacaine > Lidocaine | [14], [15] |
| Bupivacaine = Lidocaine | [21] |
| Ropivacaine no comparison | [18], [17] |
| Ropivacaine = Articaine | [25] |
| Prilocaine > Lidocaine | [16] |
| Prilocaine > Bupivacaine | [16] |
| Mepivacaine + Lidocaine = Lidocaine + Lidocaine | [26] |
| Articaine volume comparison | [27] |
Of the six amide products used in dental local anesthesia, 13 in vivo studies and 4 reviews found that articaine was the amide with the highest efficacy when compared to either lidocaine, mepivacaine, prilocaine or bupivacaine (see Table 1). Mepivacaine [12,13] and bupivacaine [14,15] as opposed to lidocaine, appeared to have a higher efficacy in one review [12,14] and one in vivo study [13,15], each.
Prilocaine, as opposed to lidocaine and bupivacaine, was found to have a higher efficacy in only one in vivo study [16]. Two in vivo studies claimed that ropivacaine had a high efficacy under different concentrations [17], without comparing it to another amide or when comparing it to lignocaine [18].
However, when duration of the local anesthetic effect was taken into account, mepivacaine was shown to work for a shorter duration compared to lidocaine [19].
Eleven studies [20,21,22,23,24,25,26,27,28,29,30] either found no significant differences between two types of amides or studied the volume of anesthetic and found its efficacy was significantly greater if higher volumes (more than one cartridge) were administered.
With regard to addition of vasoconstrictors epinephrine and clonidine, one in vivo study concluded that clonidine increased efficacy better than epinephrine, combined with lidocaine [31], while increasing the concentration of epinephrine, with articaine and lidocaine, did not significantly impact the anesthetic efficacy [14,15]. Three in vivo studies showed that adding a sodium bicarbonate buffer to lidocaine [32,33] and articaine [34], yielded no improvement in efficacy for either. One study [24] investigated the difference between mepivacaine combined with levonordefrin and lidocaine with epinephrine, and concluded that there were no significant differences between them with regard to efficacy.
Other in vivo studies incorporated drugs such as meperidine [35,36] and mannitol [37] to lidocaine, and neither appeared to have a significant influence on anesthetic efficacy. Also, liposomal bupivacaine was assessed, but did not improve the efficacy either [38].
DISCUSSION
The authors noticed that the terms efficiency and efficacy are sometimes incorrectly interchanged. Efficacy is the correct term to be used when assessing the outcome of a product, for instance, or the ability to produce a desired result (e.g. 100% pulpal anesthesia), while efficiency is to be used to assess a process (e.g. how successful is mandibular block anesthesia?) or the state or the quality of being efficient. The mix up is understandable if English is not the native language of the authors, but it should be avoided at all times as it makes the search for papers for a review more complicated.
Based on this review, which covers the past 10 years, the findings suggest that articaine has been researched the most and that it also has the highest efficacy of the amides used in dental local anesthesia. The fact that articaine received so much attention is probably attributable to the fact that before the year 2000, articaine was not available in the USA, whereas in Europe it was already marketed in 1976. As can be derived from tables 1 and 2, 20 of the 31 papers included in our study were conducted in the USA. Although, it was not within the scope of this review paper, nevertheless, the authors are aware of the dubious reputation of articaine with regard to post-operative paresthesia and the discussion about it being manufactured as a 4% solution instead of 2% like lidocaine for dental local anesthesia [16,39,40]. It deserves to be emphasized, however, that in vitro laboratory studies on cell lines have shown that articaine is not the most neurotoxic amide used in dental local anesthesia. One in vitro study, conducted by Mallet et al., tested the toxicity of 6 local anesthetic products on human neuroblastoma cells and found that articaine is the least toxic amide [40], while another in vitro study, by Perez-Castro et al., conducted on a neuronal cell-line, concluded that bupivacaine is the most toxic amide [41]. These findings are in contrast to the reported potential adverse effects, published in two review articles, stating that articaine is harmful in high concentrations, such as 4% [39], and may cause paresthesia [40]. It has to be emphasized that in the latter review, it was found that also prilocaine can potentially cause paresthesia [40]. It is noteworthy that the clinical reports about paresthesia and apparent toxicity almost always involve mandibular block anesthesia. However, it seems strange to us that articaine, for instance, would have a high neurotoxic preference for the second branch of the trigeminal nerve only. Since that was not the aim of the present study, this issue will not be discussed further here, but it definitely deserves further in depth attention.
It is our impression that, after having read the papers regarding efficacy of dental local anesthetics, none of the amides studied and used in dentistry guarantee a 100% success, especially not in the mandible. Therefore, one could conclude that perhaps the technique of administration is inefficient and therefore the efficacy is poor. Intraosseous anesthesia could be the key to increase the efficacy of local anesthetics in the mandible.
CONCLUSIONS
From the consulted literature, it is clear that local anesthetics used in dentistry do not show a 100% efficacy, especially not if administered in the mandible or in cases of inflammation (acute irreversible pulpitis). The authors suggest that this opens perspectives to explore more successful ways of administering local anesthesia, in order for the local anesthetic to be more efficacious.
Footnotes
CONFLICT OF INTEREST: One of the authors (JA) is a key opinion leader for Dental Hi Tec®, the French manufacturer of SleeperOne® and Quicksleeper®.
References
- 1.Nakai Y, Milgrom P, Mancl L, Coldwell SE, Domoto PK, Ramsay DS. Effectiveness of local anesthesia in pediatric dental practice. J Am Dent Assoc. 2000;131:1699–1705. doi: 10.14219/jada.archive.2000.0115. [DOI] [PubMed] [Google Scholar]
- 2.Milles M. The missed inferior alveolar block: A new look at an old problem. Anesth Prog. 1984;31:87–90. [PMC free article] [PubMed] [Google Scholar]
- 3.AlHindi M, Rashed B, AlOtaibi N. Failure rate of inferior alveolar nerve block among dental students and interns. Saudi Med J. 2016;37:84–89. doi: 10.15537/smj.2016.1.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanchis JM, Penarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofac Surg. 2003;61:422–424. doi: 10.1053/joms.2003.50004. [DOI] [PubMed] [Google Scholar]
- 5.Davoudi A, Rismanchian M, Akhavan A, Nosouhian S, Bajoghli F, Haghighat A, et al. A brief review on the efficacy of different possible and nonpharmacological techniques in eliminating discomfort of local anesthesia injection during dental procedures. Anesth Essays Res. 2016;10:13–16. doi: 10.4103/0259-1162.167846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malamed SF. Techniques of maxillary anesthesia. In: Malamed SF, editor. Handbook of local anesthesia. 5th ed. St Louis, Missouri: Elsevier Mosby; 2004. pp. 189–225. [Google Scholar]
- 7.Malamed SF. Techniques of maxillary anesthesia. In: Malamed SF, editor. Handbook of local anesthesia. 5th ed. St Louis, Missouri: Elsevier Mosby; 2004. pp. 227–253. [Google Scholar]
- 8.van den Akker HP. Local complications. In: Baart JA, Brand HS, editors. Local anesthesia in dentistry. 1st ed. Oxford: Wiley-Blackwell; 2009. pp. 117–125. [Google Scholar]
- 9.Baart JA. Local anesthesia in the upper jaw. In: Baart JA, Brand HS, editors. Local anesthesia in dentistry. 1st ed. Oxford: Wiley-Blackwell; 2009. pp. 57–69. [Google Scholar]
- 10.Pogrel AM, Stevens RL, Bosack RC, Orr T. Complications with the use of local anesthetics. In: Bosack RC, Lieblich S, editors. Anesthesia complications in the dental office. 1st ed. Oxford: Wiley-Blackwell; 2014. pp. 207–218. [Google Scholar]
- 11.Baart JA. Local anesthesia in the upper jaw. In: Baart JA, Brand HS, editors. Local anesthesia in dentistry. 1st ed. Oxford: Wiley-Blackwell; 2009. pp. 71–86. [Google Scholar]
- 12.Su N, Liu Y, Yang X, Shi Z, Huang Y. Efficacy and safety of mepivacaine compared with lidocaine in local anaesthesia in dentistry: A meta-analysis of randomised controlled trials. Int Dent J. 2014;64:96–107. doi: 10.1111/idj.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Visconti RP, Tortamano IP, Buscariolo IA. Comparison of the anesthetic efficacy of mepivacaine and lidocaine in patients with irreversible pulpitis: A double-blind randomized clinical trial. J Endod. 2016;42:1314–1319. doi: 10.1016/j.joen.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 14.Su N, Wang H, Zhang S, Liao S, Yang S, Huang Y. Efficacy and safety of bupivacaine versus lidocaine in dental treatments: A meta-analysis of randomised controlled trials. Int Dent J. 2014;64:34–45. doi: 10.1111/idj.12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christensen J, Matzen LH, Vaeth M, Wenzel A, Schou S. Efficiency of bupivacaine versus lidocaine and methylprednisolone versus placebo to reduce postoperative pain and swelling after surgical removal of mandibular third molars: A randomized, double-blinded, crossover clinical trial. J Oral Maxillofac Surg. 2013;71:1490–1499. doi: 10.1016/j.joms.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Piccinni C, Gissi DB, Gabusi A, Montebugnoli L, Poluzzi E. Paraesthesia after local anaesthetics: An analysis of reports to the fda adverse event reporting system. Basic Clin Pharmacol Toxicol. 2015;117:52–56. doi: 10.1111/bcpt.12357. [DOI] [PubMed] [Google Scholar]
- 17.Brkovic BM, Zlatkovic M, Jovanovic D, Stojic D. Maxillary infiltration anaesthesia by ropivacaine for upper third molar surgery. Int J Oral Maxillofac Surg. 2010;39:36–41. doi: 10.1016/j.ijom.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Budharapu A, Sinha R, Uppada UK, Subramanya Kumar AV. Ropivacaine: A new local anaesthetic agent in maxillofacial surgery. Br J Oral Maxillofac Surg. 2015;53:451–454. doi: 10.1016/j.bjoms.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 19.Berberich G, Reader A, Drum M, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of the anesthetic efficacy of two percent lidocaine with 1:100,000 and 1:50,000 epinephrine and three percent mepivacaine in the intraoral, infraorbital nerve block. J Endod. 2009;35:1498–1504. doi: 10.1016/j.joen.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Poorni S, Veniashok B, Senthilkumar AD, Indira R, Ramachandran S. Anesthetic efficacy of four percent articaine for pulpal anesthesia by using inferior alveolar nerve block and buccal infiltration techniques in patients with irreversible pulpitis: A prospective randomized double-blind clinical trial. J Endod. 2011;37:1603–1607. doi: 10.1016/j.joen.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Sampaio RM, Carnaval TG, Lanfredi CB, Horliana AC, Rocha RG, Tortamano IP. Comparison of the anesthetic efficacy between bupivacaine and lidocaine in patients with irreversible pulpitis of mandibular molar. J Endod. 2012;38:594–597. doi: 10.1016/j.joen.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Mason R, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine and 3% mepivacaine for maxillary infiltrations. J Endod. 2009;35:1173–1177. doi: 10.1016/j.joen.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 23.Forloine A, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of the anesthetic efficacy of two percent lidocaine with 1:100,000 epinephrine and three percent mepivacaine in the maxillary high tuberosity second division nerve block. J Endod. 2010;36:1770–1777. doi: 10.1016/j.joen.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Lawaty I, Drum M, Reader A, Nusstein J. A prospective, randomized, double-blind comparison of 2% mepivacaine with 1 : 20,000 levonordefrin versus 2% lidocaine with 1 : 100,000 epinephrine for maxillary infiltrations. Anesth Prog. 2010;57:139–144. doi: 10.2344/0003-3006-57.4.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krzeminski TF, Gilowski L, Wiench R, Plocica I, Kondzielnik P, Sielanczyk A. Comparison of ropivacaine and articaine with epinephrine for infiltration anaesthesia in dentistry - a randomized study. Int Endod J. 2011;44:746–751. doi: 10.1111/j.1365-2591.2011.01881.x. [DOI] [PubMed] [Google Scholar]
- 26.Lammers E, Nusstein J, Reader A, Drum M, Beck M, Fowler S. Does the combination of 3% mepivacaine plain plus 2% lidocaine with epinephrine improve anesthesia and reduce the pain of anesthetic injection for the inferior alveolar nerve block? A prospective, randomized, double-blind study. J Endod. 2014;40:1287–1292. doi: 10.1016/j.joen.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 27.Sreekumar K, Bhargava D. Comparison of onset and duration of action of soft tissue and pulpal anesthesia with three volumes of 4% articaine with 1:100,000 epinephrine in maxillary infiltration anesthesia. Oral Maxillofac Surg. 2011;15:195–199. doi: 10.1007/s10006-011-0275-8. [DOI] [PubMed] [Google Scholar]
- 28.Kanaa MD, Whitworth JM, Meechan JG. A comparison of the efficacy of 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1:80,000 epinephrine in achieving pulpal anesthesia in maxillary teeth with irreversible pulpitis. J Endod. 2012;38:279–282. doi: 10.1016/j.joen.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 29.Martin M, Nusstein J, Drum M, Reader A, Beck M. Anesthetic efficacy of 1.8 ml versus 3.6 ml of 4% articaine with 1:100,000 epinephrine as a primary buccal infiltration of the mandibular first molar. J Endod. 2011;37:588–592. doi: 10.1016/j.joen.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Brunetto PC, Ranali J, Ambrosano GM, de Oliveira PC, Groppo FC, Meechan JG, et al. Anesthetic efficacy of 3 volumes of lidocaine with epinephrine in maxillary infiltration anesthesia. Anesth Prog. 2008;55:29–34. doi: 10.2344/0003-3006(2008)55[29:AEOVOL]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jain NK, John RR. Anesthetic efficacy of 4% articaine versus 2% lignocaine during the surgical removal of the third molar: A comparative prospective study. Anesth Essays Res. 2016;10:356–361. doi: 10.4103/0259-1162.171445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitcomb M, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind study of the anesthetic efficacy of sodium bicarbonate buffered 2% lidocaine with 1:100,000 epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2010;57:59–66. doi: 10.2344/0003-3006-57.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schellenberg J, Drum M, Reader A, Nusstein J, Fowler S, Beck M. Effect of buffered 4% lidocaine on the success of the inferior alveolar nerve block in patients with symptomatic irreversible pulpitis: A prospective, randomized, double-blind study. J Endod. 2015;41:791–796. doi: 10.1016/j.joen.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 34.Shurtz R, Nusstein J, Reader A, Drum M, Fowler S, Beck M. Buffered 4% articaine as a primary buccal infiltration of the mandibular first molar: A prospective, randomized, double-blind study. J Endod. 2015;41:1403–1407. doi: 10.1016/j.joen.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 35.Goodman A, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks. Anesth Prog. 2006;53:131–139. doi: 10.2344/0003-3006(2006)53[131:AEOMFI]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohajeri L, Salehi F, Mehrvarzfar P, Arfaee H, Bohluli B, Hamedy R. Anesthetic efficacy of meperidine in teeth with symptomatic irreversible pulpitis. Anesth Prog. 2015;62:14–19. doi: 10.2344/0003-3006-62.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohen H, Reader A, Drum M, Nusstein J, Beck M. Anesthetic efficacy of a combination of 0.9 m mannitol plus 68.8 mg of lidocaine with 50 mug epinephrine in inferior alveolar nerve blocks: A prospective randomized, single blind study. Anesth Prog. 2013;60:145–152. doi: 10.2344/0003-3006-60.4.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Glenn B, Drum M, Reader A, Fowler S, Nusstein J, Beck M. Does liposomal bupivacaine (exparel) significantly reduce postoperative pain/numbness in symptomatic teeth with a diagnosis of necrosis? A prospective, randomized, double-blind trial. J Endod. 2016;42:1301–1306. doi: 10.1016/j.joen.2016.05.018. [DOI] [PubMed] [Google Scholar]
- 39.Hillerup S, Jensen RH, Ersboll BK. Trigeminal nerve injury associated with injection of local anesthetics: Needle lesion or neurotoxicity? J Am Dent Assoc. 2011;142:531–539. doi: 10.14219/jada.archive.2011.0223. [DOI] [PubMed] [Google Scholar]
- 40.Garisto GA, Gaffen AS, Lawrence HP, Tenenbaum HC, Haas DA. Occurrence of paresthesia after dental local anesthetic administration in the united states. J Am Dent Assoc. 2010;141:836–844. doi: 10.14219/jada.archive.2010.0281. [DOI] [PubMed] [Google Scholar]
- 41.Perez-Castro R, Patel S, Garavito-Aguilar ZV, Rosenberg A, Recio-Pinto E, Zhang J, et al. Cytotoxicity of local anesthetics in human neuronal cells. Anesth Analg. 2009;108:997–1007. doi: 10.1213/ane.0b013e31819385e1. [DOI] [PubMed] [Google Scholar]
- 42.Katyal V. The efficacy and safety of articaine versus lignocaine in dental treatments: A meta-analysis. J Dent. 2010;38:307–317. doi: 10.1016/j.jdent.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 43.Kung J, McDonagh M, Sedgley CM. Does articaine provide an advantage over lidocaine in patients with symptomatic irreversible pulpitis? A systematic review and meta-analysis. J Endod. 2015;41:1784–1794. doi: 10.1016/j.joen.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 44.Su N, Li C, Wang H, Shen J, Liu W, Kou L. Efficacy and safety of articaine versus lidocaine for irreversible pulpitis treatment: A systematic review and meta-analysis of randomised controlled trials. Aust Endod J. 2016;42:4–15. doi: 10.1111/aej.12125. [DOI] [PubMed] [Google Scholar]
- 45.Colombini BL, Modena KC, Calvo AM, Sakai VT, Giglio FP, Dionisio TJ, et al. Articaine and mepivacaine efficacy in postoperative analgesia for lower third molar removal: A double-blind, randomized, crossover study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:169–174. doi: 10.1016/j.tripleo.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Pellicer-Chover H, Cervera-Ballester J, Sanchis-Bielsa JM, Penarrocha-Diago MA, Penarrocha-Diago M, Garcia-Mira B. Comparative split-mouth study of the anesthetic efficacy of 4% articaine versus 0.5% bupivacaine in impacted mandibular third molar extraction. J Clin Exp Dent. 2013;5:e66–e71. doi: 10.4317/jced.50869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thakare A, Bhate K, Kathariya R. Comparison of 4% articaine and 0.5% bupivacaine anesthetic efficacy in orthodontic extractions: Prospective, randomized crossover study. Acta Anaesthesiol Taiwan. 2014;52:59–63. doi: 10.1016/j.aat.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 48.Ashraf H, Kazem M, Dianat O, Noghrehkar F. Efficacy of articaine versus lidocaine in block and infiltration anesthesia administered in teeth with irreversible pulpitis: A prospective, randomized, double-blind study. J Endod. 2013;39:6–10. doi: 10.1016/j.joen.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 49.Brkovic B, Gardasevic M, Roganovic J, Jovic N, Todorovic L, Stojic D. Lidocaine+clonidine for maxillary infiltration anaesthesia: Parameters of anaesthesia and vascular effects. Int J Oral Maxillofac Surg. 2008;37:149–155. doi: 10.1016/j.ijom.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 50.Gazal G. Comparison of speed of action and injection discomfort of 4% articaine and 2% mepivacaine for pulpal anesthesia in mandibular teeth: A randomized, double-blind cross-over trial. Eur J Dent. 2015;9:201–206. doi: 10.4103/1305-7456.156811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Srinivasan N, Kavitha M, Loganathan CS, Padmini G. Comparison of anesthetic efficacy of 4% articaine and 2% lidocaine for maxillary buccal infiltration in patients with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:133–136. doi: 10.1016/j.tripleo.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 52.Nydegger B, Nusstein J, Reader A, Drum M, Beck M. Anesthetic comparisons of 4% concentrations of articaine, lidocaine, and prilocaine as primary buccal infiltrations of the mandibular first molar: A prospective randomized, double-blind study. J Endod. 2014;40:1912–1916. doi: 10.1016/j.joen.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 53.Rogers BS, Botero TM, McDonald NJ, Gardner RJ, Peters MC. Efficacy of articaine versus lidocaine as a supplemental buccal infiltration in mandibular molars with irreversible pulpitis: A prospective, randomized, double-blind study. J Endod. 2014;40:753–758. doi: 10.1016/j.joen.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 54.McEntire M, Nusstein J, Drum M, Reader A, Beck M. Anesthetic efficacy of 4% articaine with 1:100,000 epinephrine versus 4% articaine with 1:200,000 epinephrine as a primary buccal infiltration in the mandibular first molar. J Endod. 2011;37:450–454. doi: 10.1016/j.joen.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 55.Wali M, Drum M, Reader A, Nusstein J. Prospective, randomized single-blind study of the anesthetic efficacy of 1.8 and 3.6 milliliters of 2% lidocaine with 1:50,000 epinephrine for inferior alveolar nerve block. J Endod. 2010;36:1459–1462. doi: 10.1016/j.joen.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 56.Evans G, Nusstein J, Drum M, Reader A, Beck M. A prospective, randomized, double-blind comparison of articaine and lidocaine for maxillary infiltrations. J Endod. 2008;34:389–393. doi: 10.1016/j.joen.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 57.Boonsiriseth K, Chaimanakarn S, Chewpreecha P, Nonpassopon N, Khanijou M, Ping B, et al. 4% lidocaine versus 4% articaine for inferior alveolar nerve block in impacted lower third molar surgery. J Dent Anesth Pain Med. 2017;17:29–35. doi: 10.17245/jdapm.2017.17.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]