Abstract
Aims/hypothesis
Exercise is recommended for the treatment and prevention of type 2 diabetes. However, the most effective time of day to achieve beneficial effects on health remains unknown. We aimed to determine whether exercise training at two distinct times of day would have differing effects on 24 h blood glucose levels in men with type 2 diabetes.
Methods
Eleven men with type 2 diabetes underwent a randomised crossover trial. Inclusion criteria were 45–68 years of age and BMI between 23 and 33 kg/m2. Exclusion criteria were insulin treatment and presence of another systemic illness. Researchers were not blinded to the group assignment. The trial involved 2 weeks of either morning or afternoon high-intensity interval training (HIIT) (three sessions/week), followed by a 2 week wash-out period and a subsequent period of the opposite training regimen. Continuous glucose monitor (CGM)-based data were obtained.
Results
Morning HIIT increased CGM-based glucose concentration (6.9 ± 0.4 mmol/l; mean ± SEM for the exercise days during week 1) compared with either the pre-training period (6.4 ± 0.3 mmol/l) or afternoon HIIT (6.2 ± 0.3 mmol/l for the exercise days during week 1). Conversely, afternoon HIIT reduced the CGM-based glucose concentration compared with either the pre-training period or morning HIIT. Afternoon HIIT was associated with elevated thyroid-stimulating hormone (TSH; 1.9 ± 0.2 mU/l) and reduced T4 (15.8 ± 0.7 pmol/l) concentrations compared with pre-training (1.4 ± 0.2 mU/l for TSH; 16.8 ± 0.6 pmol/l for T4). TSH was also elevated after morning HIIT (1.7 ± 0.2 mU/l), whereas T4 concentrations were unaltered.
Conclusions/interpretation
Afternoon HIIT was more efficacious than morning HIIT at improving blood glucose in men with type 2 diabetes. Strikingly, morning HIIT had an acute, deleterious effect, increasing blood glucose. However, studies of longer training regimens are warranted to establish the persistence of this adverse effect. Our data highlight the importance of optimising the timing of exercise when prescribing it as treatment for type 2 diabetes.
Keywords: Blood glucose level, Circadian rhythm, Continuous glucose monitoring, Exercise, High-intensity interval training, Type 2 diabetes
Introduction
Exercise is recommended for the prevention and treatment of type 2 diabetes [1]. Low-volume high-intensity interval training (HIIT) remodels skeletal muscle and the cardiorespiratory system to a similar extent as continuous moderate-intensity training, with reduced time commitment and exercise volume [2]. In addition, glucose tolerance, insulin sensitivity and muscle oxidative capacity show circadian oscillations [3, 4]. Interactions between these factors could lead to divergent physiological adaptations to exercise training at different times of day. By determining the effects of morning and afternoon HIIT on 24 h blood glucose in men with type 2 diabetes in ‘free-living’ conditions, we tested the hypothesis that time of day would influence the metabolic response to exercise.
Methods
This trial was approved by the regional ethics board at the Karolinska Institutet, Stockholm, Sweden (2016/1421-31/1). All participants gave their informed consent.
Study design
Eleven men with type 2 diabetes (Table 1) completed a randomised crossover trial. The trial was intended as a pilot to a larger-scale study (ClinicalTrials.gov number NCT03553524). Inclusion criteria were age between 45 and 68 years and a BMI between 23 and 33 kg/m2. Exclusion criteria were insulin treatment, recent history of smoking (<6 months) and presence of cardiovascular, rheumatoid, blood-borne or neoplastic disease. Participants were receiving either dietary treatment (n = 2) or metformin (n = 9; daily dose range 500–3000 mg; n = 2, 3/day; n = 4, 2/day; n = 3, 1/day) and continued their treatment throughout the study. Blood samples were obtained before and after completion of each training regimen (Table 2). Participants kept dietary records for 24 h before blood sampling and were asked to replicate their diet prior to subsequent visits.
Table 1.
Baseline characteristics
| Variable (n = 11) | Baseline data |
|---|---|
| Age (years) | 60 ± 2 |
| Time since diagnosis (years) | 11 ± 3 |
| BMI (kg/m2) | 27.5 ± 0.6 |
| WHR | 0.99 ± 0.01 |
| Body fat (%) | 26.4 ± 0.8 |
| Max heart rate (beats/min) | 158 ± 7 |
| Maximum power (W/kg) | 2.1 ± 0.1 |
Data are mean ± SEM
Table 2.
Blood chemistry analyses
| Blood chemistry | Pre-training | Post-morning | Post-afternoon |
|---|---|---|---|
| Glucose (mmol/l) | 7.3 ± 0.3 | 7.7 ± 0.4 | 7.5 ± 0.3 |
| Insulin (pmol/l) | 56.9 ± 9.3 | 71.4 ± 6.9 | 70.4 ± 11.6 |
| HbA1c (mmol/mol) | 48.3 ± 3.9 | 45.1 ± 2.1 | 46.1 ± 2.7 |
| HbA1c (%) | 6.6 ± 0.4 | 6.3 ± 0.2 | 6.4 ± 0.2 |
| Total cholesterol (mmol/l) | 4.2 ± 0.4 | 4.4 ± 0.3 | 4.2 ± 0.4 |
| HDL-cholesterol (mmol/l) | 1.2 ± 0.1 | 1.3 ± 0.1 | 1.2 ± 0.1 |
| LDL-cholesterol (mmol/l) | 2.4 ± 0.4 | 2.4 ± 0.4 | 2.3 ± 0.4 |
| Triacylglycerol (mmol/l) | 1.2 ± 0.2 | 1.6 ± 0.3 | 1.4 ± 0.2 |
| PTH (pmol/l)†† | 3.9 ± 0.2 | 4.4 ± 0.2 | 4.6 ± 0.3‡ |
| TSH (mU/l)†† | 1.4 ± 0.2 | 1.7 ± 0.2‡ | 1.9 ± 0.2‡ |
| T4 (pmol/l)† | 16.8 ± 0.6 | 16.1 ± 0.7 | 15.8 ± 0.7‡‡ |
| T3 (pmol/l) | 4.7 ± 0.2 | 4.8 ± 0.2 | 4.9 ± 0.1 |
Blood samples were obtained from fasting participants before (Pre-training) and after HIIT training for 2 weeks in the morning (Post-morning) or afternoon (Post-afternoon). Data are mean ± SEM. One-way ANOVA (†p < 0.1, ††p < 0.05), followed by Tukey’s post hoc test (‡p < 0.1, ‡‡p < 0.05 vs pre-training)
Continuous glucose monitors (CGMs; FreeStyle Libre, Abbott Laboratories, Chicago, IL, US) were fitted, and baseline (pre-training) measurements were collected for 2 weeks. Participants were assigned (block randomisation, size = 4 or 5) to either morning (08:00 hours) or afternoon (16:00 hours) training (n = 7 and n = 4, respectively) for 2 weeks; this consisted of supervised exercise sessions on Mondays, Wednesdays and Fridays (Exercise), followed by a rest day (Rest) (giving six exercise sessions in total). Following a 2 week ‘wash-out’ period, participants performed the opposite exercise training regimen. Two participants who completed only three and four afternoon sessions, respectively, were excluded from the week 2 comparisons. Researchers were not blinded to the group assignment.
Exercise intervention
Supervised exercise training was performed at a gym in Stockholm. At a pilot test, each individual cycled at 75 rpm and with a load that forced a rest after 1 min. This was repeated six times with a 1 min rest in between. The load reached for each 1 min pulse was recorded, and a mean of the six pulses was used for all HIIT sessions. HIIT sessions were performed on a cycle ergometer, commencing with a 7 min warm-up, followed by six 1 min pulses at the predetermined load (usually above 220 W, range 180–350 W) and with a pedalling rate of 75 rpm. Each pulse was followed by a 1 min recovery period (75 rpm with minimal load). Participants were instructed to have a light breakfast before (approximately 1 h ahead of) the morning sessions, and a standardised snack (sandwich and juice) was offered ad libitum around 30 min after the exercise. Afternoon sessions took place after lunch (approximately 3 h later) and were followed by dinner around 30 min thereafter.
Statistical analysis
Blood glucose level was determined using CGMs throughout the study, from which hourly means were calculated. The 24 h blood glucose measurements for the first three (week 1) and the last three (week 2) Exercise and Rest days for each trial were compared with each other and with corresponding pre-training days. Pre-training days were matched to corresponding days of the week for Exercise and Rest, respectively. Data were analysed using Prism 7.01 software (GraphPad, San Diego, CA, US) by two-way ANOVA followed by a Tukey’s post hoc test (significance level set at p < 0.05).
Results
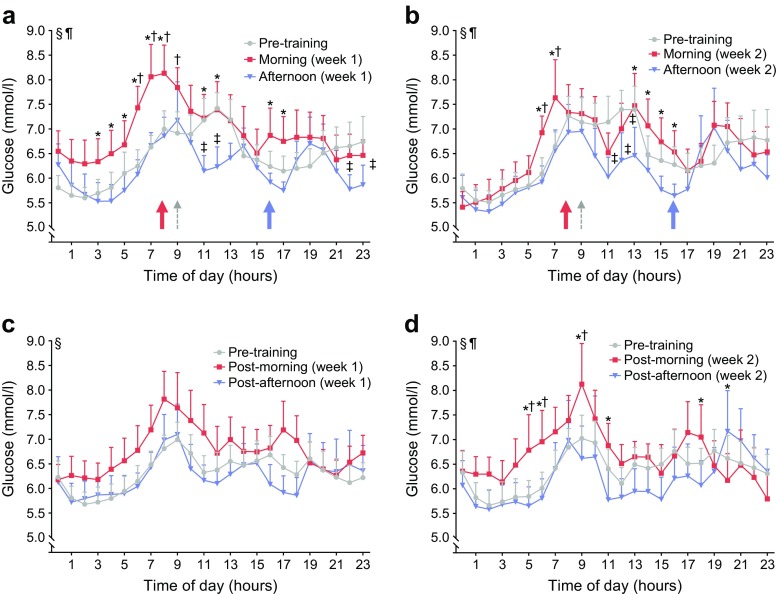
Morning HIIT increased CGM-based glucose concentrations on Exercise days during week 1 (6.9 ± 0.4 mmol/l; mean ± SEM) (Fig. 1a) and week 2 (6.6 ± 0.4 mmol/l) (Fig. 1b) compared with either the pre-training days (6.4 ± 0.3 mmol/l) or afternoon HIIT (6.2 ± 0.3 and 6.1 ± 0.4 mmol/l for week 1 and 2, respectively) at several time points. Conversely, afternoon HIIT reduced CGM-based glucose concentration on Exercise days during week 1 (Fig. 1a) and week 2 (Fig. 1b) of training compared with either pre-training or morning HIIT at several time points. Morning HIIT also increased CGM-based glucose concentrations on Rest days during week 2 (Fig. 1d), but not week 1 (Fig. 1c), compared with pre-training days or afternoon HIIT at several time points. Mean 24 h glucose curves for the pre-training period and the last 3 days of the wash-out period were unaltered (data not shown). Thus, the wash-out period was sufficient to remove the effects of HIIT. Afternoon HIIT elevated parathyroid hormone (PTH) and thyroid-stimulating hormone (TSH) concentrations, and reduced T4 concentration, compared with pre-training concentrations (Table 2). TSH was also elevated after morning HIIT, whereas PTH and T4 concentrations were unaltered.
Fig. 1.
CGM-based glucose levels in response to HIIT. CGM-based glucose levels were assessed during the pre-training period and on exercise days (Exercise) and subsequent days (Rest). Blood glucose readings on Exercise days in (a) week 1 (n = 11) and (b) week 2 (n = 9), and on Rest days in (c) week 1 (n = 11) and (d) week 2 (n = 8). Red lines and symbols, morning exercise; blue lines and symbols, afternoon exercise; grey lines and symbols, matched pre-training days. Red arrows, time of morning exercise; blue arrows, time of afternoon exercise; grey arrows, snack offered. Using two-way ANOVA: §p < 0.05 for the effect of time; ¶p < 0.05 for the interaction between exercise and time. Using Tukey’s multiple comparison test: *p < 0.05 for the difference between exercise trials; †p < 0.05 for the difference between morning exercise trial and pre-training period; ‡p < 0.05 for the difference between afternoon exercise trial and pre-training period. Values are means + SEM
Discussion
To our knowledge, this is the first study performed in a real-life setting that compares the impact of 2 weeks of HIIT at different times of day on blood glucose excursions in people with type 2 diabetes. Afternoon HIIT was more efficacious than morning HIIT in improving blood glucose levels. Unexpectedly, morning HIIT elevated glucose levels at several time points throughout the day compared with the pre-training period and afternoon HIIT. Conversely, afternoon HIIT lowered blood glucose at several time points throughout the day compared with pre-training and morning HIIT. Our results are clinically relevant, showing that timing of exercise affects the glycaemic response to HIIT in men with type 2 diabetes.
The circadian clock is a key homeostatic regulator that is synchronised by photic and non-photic stimuli (food intake, temperature and physical activity), and controls many genomic and physiological responses in virtually all cells [1]. We reasoned that if the timing of exercise could be optimised to coincide with these responses, its potency as a therapeutic tool might be augmented. Several lines of evidence suggest that the timing of exercise alters physiological responses diversely. In healthy young men, parasympathetic and sympathetic activity during the next nocturnal sleep is differentially enhanced by morning and evening exercise, as evidenced by changes in body temperature, heart rate and heart rate variability [5]. Moreover, human skeletal muscular strength and mitochondrial function peak in late afternoon [4, 6], suggesting a circadian rhythm of oxidative metabolism.
Here we report that the time of day affects the blood glucose response to exercise in people with type 2 diabetes, with improvements in daily glucose excursions observed in conjunction with afternoon HIIT. Our results are compatible with a previous report that a session of moderate-intensity exercise performed in the morning vs the afternoon conferred a lower risk of late-onset hypoglycaemia and improved metabolic control on the subsequent day in young individuals with type 1 diabetes [7]. We report that morning HIIT increased CGM-based glucose concentration acutely as well as on the subsequent rest day during week 2 of training. Collectively, these results imply that the timing of exercise impacts blood glucose excursions over the day. Aligning exercise bouts with the systemic circadian rhythm appears to confer a differential glycaemic response in people with diabetes.
Optimising the timing of an exercise session with defined eating patterns may interact with the circadian clock signal to prevent disease pathogenesis [1]. Morning HIIT has been shown to improve blood glucose levels in individuals with type 2 diabetes when performed under controlled conditions with standardised meals provided 1.5 h before the exercise session [8]. In our study, morning HIIT had an acute deleterious effect on blood glucose. Conceivably, individuals participating in an exercise programme in a real-life setting may consume meals closer to or directly after the morning exercise session. Such a scenario, potentiated by the suppressive effects of high-intensity exercise on gastric emptying [9], may partially account for deleterious effects of morning HIIT on blood glucose in our study. Thus, timing is also important in respect to food intake, with a better glycaemic response achieved with postprandial exercise in people with type 2 diabetes [10].
Exercise at different times of day may coincide with fuel utilisation preferences on the part of the working muscles. Moreover, HIIT has a preference for carbohydrate oxidation when compared with moderate-intensity exercise [11]. Thus, differential fuel utilisation patterns during morning vs afternoon exercise may partly explain the changes in blood glucose regulation between trials. Morning HIIT-induced increases in blood glucose levels were predominately observed in week 1. An acute dysregulation of diurnal hormonal rhythms could account for this phenomenon. Supporting this assertion, afternoon HIIT potentiated the TSH and T4 responses. In week 2 of the morning HIIT, we observed an apparent improvement in glucose levels, as the participants become better acclimated to the training regimen. Studies of longer training periods are thus warranted to establish the persistence of these adverse effects.
We conducted a field-based study in ‘free-living’ individuals, so specific factors responsible for differing blood glucose levels between morning and afternoon HIIT trials remain to be elucidated. Due to the randomised crossover design and paired nature of the data, putative individual differences in the sleep/wake cycle and sleep architecture are mostly accounted for. Future studies are warranted to characterise the underlying hormonal and metabolic changes to exercise training at different times of day in healthy and diseased populations.
Although HIIT is promising for the management of type 2 diabetes, our data indicate that the timing of exercise should be considered. This concern may be modality and population dependent. In light of diverse hormonal responses and fuel utilisation preference [11], less intense forms of exercise may have differing effects on blood glucose and associated metabolic responses. Conversely, individuals prone to nocturnal hypoglycaemia or who are receiving insulin treatment might respond differently to the same training regimen. In conclusion, our data highlight the importance of optimising the timing of exercise sessions to improve glycaemic control in people with type 2 diabetes.
Acknowledgements
Some of the data were presented as an abstract at the 54th annual meeting of the European Association for Study of Diabetes in 2018. The authors wish to thank J. Larsson and K. Mattsson (SATS Sports Club Sweden AB, Stockholm, Sweden) for assistance with exercise supervision and for access to the training facilities, D. Fiuza-Sanches (Clinical Physiology, Karolinska University Hospital, Stockholm, Sweden) for exercise testing, and P. Odenblad (Clinical Physiology, Karolinska University Hospital, Stockholm, Sweden) for assistance with study coordination.
Data availability
The data analysed during the current study are available from the corresponding author on reasonable request.
Funding
The authors are supported by grants from Novo Nordisk Foundation (NNF14OC0011493 and NNF14OC0009941), Swedish Diabetes Foundation (DIA2015-052), Wenner-Gren Foundation, Swedish Research Council (2015-00165), Strategic Research Program in Diabetes at Karolinska Institutet (2009-1068), Stockholm County Council (SLL20150517 and SLL20170159) and Swedish Heart Lung Foundation (20150423).
Abbreviations
- CGM
Continuous glucose monitor
- HIIT
High-intensity interval training
- PTH
Parathyroid hormone
- TSH
Thyroid-stimulating hormone
Contribution statement
MS and BMG designed the study, collected and analysed the data and wrote the manuscript. JS and TF collected and analysed the data and critically revised the manuscript. MB, KC and PSA designed the study, collected the data and critically revised the manuscript. AK, JRZ and HWH designed the study, analysed the data and critically revised the manuscript. All authors approved the final version of the manuscript for publication. HWH is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
References
- 1.Gabriel BM, Zierath JR. The limits of exercise physiology: from performance to health. Cell Metab. 2017;25(5):1000–1011. doi: 10.1016/j.cmet.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. 2012;590(5):1077–1084. doi: 10.1113/jphysiol.2011.224725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qian J, Scheer F. Circadian system and glucose metabolism: implications for physiology and disease. Trends Endocrinol Metab. 2016;27(5):282–293. doi: 10.1016/j.tem.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Moorsel D, Hansen J, Havekes B, et al. Demonstration of a day-night rhythm in human skeletal muscle oxidative capacity. Mol Metab. 2016;5(8):635–645. doi: 10.1016/j.molmet.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamanaka Y, Hashimoto S, Takasu NN, et al. Morning and evening physical exercise differentially regulate the autonomic nervous system during nocturnal sleep in humans. Am J Physiol Regul Integr Comp Physiol. 2015;309(9):R1112–R1121. doi: 10.1152/ajpregu.00127.2015. [DOI] [PubMed] [Google Scholar]
- 6.Deschenes MR, Kraemer WJ, Bush JA, et al. Biorhythmic influences on functional capacity of human muscle and physiological responses. Med Sci Sports Exerc. 1998;30(9):1399–1407. doi: 10.1097/00005768-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Gomez AM, Gomez C, Aschner P, et al. Effects of performing morning versus afternoon exercise on glycemic control and hypoglycemia frequency in type 1 diabetes patients on sensor-augmented insulin pump therapy. J Diabetes Sci Technol. 2015;9(3):619–624. doi: 10.1177/1932296814566233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillen JB, Little JP, Punthakee Z, Tarnopolsky MA, Riddell MC, Gibala MJ. Acute high-intensity interval exercise reduces the postprandial glucose response and prevalence of hyperglycaemia in patients with type 2 diabetes. Diabetes Obes Metab. 2012;14(6):575–577. doi: 10.1111/j.1463-1326.2012.01564.x. [DOI] [PubMed] [Google Scholar]
- 9.Leiper JB, Broad NP, Maughan RJ. Effect of intermittent high-intensity exercise on gastric emptying in man. Med Sci Sports Exerc. 2001;33(8):1270–1278. doi: 10.1097/00005768-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Nygaard H, Rønnestad BR, Hammarström D, Holmboe-Ottesen G, Høstmark AT. Effects of exercise in the fasted and postprandial state on interstitial glucose in hyperglycemic individuals. J Sports Sci Med. 2017;16(2):254–263. [PMC free article] [PubMed] [Google Scholar]
- 11.Peake JM, Tan SJ, Markworth JF, Broadbent JA, Skinner TL, Cameron-Smith D. Metabolic and hormonal responses to isoenergetic high-intensity interval exercise and continuous moderate-intensity exercise. Am J Phys Endocrinol Metab. 2014;307(7):E539–E552. doi: 10.1152/ajpendo.00276.2014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analysed during the current study are available from the corresponding author on reasonable request.