Abstract
Traumatic brain injury (TBI) is the most common cause of death and permanent disability in people aged <45, and is associated with secondary brain injury and bleed progression, resulting in increased morbidity and mortality. TBI may also induce innate host defense responses characterized by activation of resident microglia and astrocytes, brain microvascular endothelial cells and peripheral blood monocytes. In the present study, 34 patients with moderate-to-severe traumatic brain injury were randomly divided into two groups, including a 7.5% hypertonic saline (HS) treatment group (4 ml/kg) and 3% HS treatment group (4 ml/kg). The results demonstrated that treatment with 7.5% HS decreased the intracranial pressure and improved coagulofibrinolytic homeostasis. Analysis of the monocyte subsets revealed significant reduction in the proportion of cluster of differentiation (CD)14++CD16+ circulating inflammatory monocytes in the 7.5% HS group. In addition, 7.5% HS treatment downregulated the expression of long non-coding (lnc) RNA2448-11 and lncRNA1403 in the peripheral blood mononuclear cells of patients with TBI. Using reverse transcription-quantitative polymerase chain reaction, it was determined that 7.5% HS regulated the expression of tumor necrosis factor-α, interleukin-1β, transforming growth factor-β and thrombomodulin, which are the target genes of lncRNA2448-11 and lncRNA1403. These results indicated that 7.5% HS improved the intracranial pressure and coagulofibrinolytic homeostasis by modulating the phenotype of monocytes through lncRNA2448-11 and lncRNA1403. These findings provided evidence that initial resuscitation with HS imparts functional changes to inflammatory cells following TBI, thereby reducing potential neuroinflammatory events associated with secondary brain injury.
Keywords: hypertonic saline, coagulofibrinolytic homeostasis, monocyte phenotype, lncRNAs, traumatic brain injury
Introduction
Traumatic brain injury (TBI), also known as craniocerebral trauma, can cause temporary or permanent impairments to cognition, behavior and emotion, and is the main cause of death and disability in people <45 (1). A previous study revealed that the incidence of TBI is three times higher than the increasing population rate and costs >33 billion euros each year to treat (2). The incidence of TBI has increased with the acceleration of urban construction and its associated increase in traffic accidents, and has led to a large consumption of social resources (3).
TBI is a complex pathophysiological process that involves primary and secondary brain injury, which affects the structure and function of the nervous system. The primary injury involves irreversible brain damage, vascular damage and diffuse axonal injury (4), whereas the secondary injury is due to hypoxia, release of inflammatory mediators, and abnormal function of coagulation fibrinolysis and monocyte infiltration (5).
The main characteristics of TBI are cerebral edema, cerebral lesions, a progressively increasing intracranial pressure (ICP) as well as tissue ischemia, hypoxia and necrosis. Irreversible brain damage is mainly caused by microcirculatory disorders, increased vascular permeability and damage to the blood-brain barrier (6,7). The detailed mechanisms are not fully understood, but TBI is closely associated with the release of tissue factor (TF), disseminated intravascular coagulation and dysfunctional platelets (8). Innate immunity can activate coagulation-related signaling pathways via pathogen associated molecular patterns or damage associated molecular patterns. Subsequently, monocytes secrete TF into the peripheral circulation and activate the extrinsic coagulation pathway, which may lead to coagulation disorders, and even coronary syndrome and stroke (9).
Laboratory and clinical studies have demonstrated that hypertonic saline (HS) can inhibit the activation of immune and endothelial cells, and suppress cytokine secretion, thereby reducing damage to nerve function and progression to secondary brain injury (10,11). A previous study also revealed that HS could decrease the expression of TFs and D-dimers following TBI, and maintain a regular expression level of thrombomodulin (12). TF is one of the factors that initiate the extrinsic coagulation pathway, whereas thrombomodulin can activate C-reactive protein and acts as an anticoagulation factor. Monocytes are the only immune cells in the blood that express both TF and thrombomodulin.
Long non-coding RNA (lncRNA) is a type of RNA that is >200 nucleotides in length. lncRNA does not encode for proteins, but instead regulates the expression of specific genes at the transcriptional, post-transcriptional and epigenetic level. lncRNA also serves an important role in maintaining homeostasis of multiple organs and tissues during both normal physiological and pathological states via regulation of prostaglandin-endoperoxide synthase 2 and interferon-stimulated genes (13). lncRNA is a crucial regulator in promoting differentiation and maturation of dendritic cells through activation of the signal transducer and activator of transcription 3 signaling pathway (14). lncRNA can also inhibit inflammatory reactions by providing negative feedback signaling to nuclear factor κ-light-chain-enhancer of activated B cells, resulting in inhibition of the tumor necrosis factor (TNF) signaling pathway (15). A previous study indicated that lncRNA participates in inflammatory reactions, and can initiate a cascade of coagulation reactions as well as cell apoptosis (16). Therefore, it was speculated that HS may regulate coagulation and inflammatory responses in patients with TBI by influencing the activation and phenotype of monocytes, and the expression of lncRNAs. HS may serve a protective role in the pathophysiological process of TBI.
Materials and methods
Materials
Ficoll-Paque PLUS (cat. no. 71-7167-00 AG) was purchased from GE Healthcare (Chicago, IL, USA). Fetal bovine serum (FBS) and high glucose (H)-Dulbecco's modified Eagle's medium (DMEM) were purchased from Invitrogen (Thermo Fisher Scientific, Inc., Waltham, MA, USA). TRIzol® (cat. no. 15596026) was purchased from Invitrogen (Thermo Fisher Scientific, Inc.). The HiFiScript cDNA Synthesis kit (cat. no. CW2569), UltraSYBR One Step RT-qPCR kit (cat. no. CW0659) and AllPure DNA/RNA/Protein kit (cat. no. CW0591) were purchased from CWBiotech (Beijing, China). Fluorescein isothiocyanate (FITC)-labeled CD14 (cat. no. 301804) and phycoerythrin (PE)-labeled CD16 (cat. no. 302008) antibodies were purchased from BioLegend, Inc. (San Diego, CA, USA).
Cell cultures
Human monocyte leukemia (THP-1; cat. no. TCHu 57), human Burkitt's lymphoma (Raji; cat. no. TCHu 44) and human T lymphoblastic leukemia cell lines (A3; cat. no. TCHu 96) were purchased from the Shanghai Cell Resource Center of Chinese Academy of Sciences (Shanghai, China). Cells were cultured in H-DMEM supplemented with 10% FBS at 37°C and in a 5% CO2 atmosphere.
Ethics statement
The present study was approved by the Medical Ethics and Human Clinical Trial Committee of the Affiliated Hospital of the Logistic University of the Chinese People's Armed Police Force (Tianjin, China) and was carried out in compliance with the Helsinki Declaration. Written informed consent was obtained from all patients prior to recruitment onto the study. The clinical specimens used in the present study were collected from patients at the Neurosurgical Intensive Care Unit of the Affiliated Hospital of the Logistic University of the Chinese People's Armed Police Force (Tianjin, China) between April 2015 and March 2016. All the protocols were carried out in accordance with the approved guidelines.
Patients and treatments
A total of 34 moderate and severe patients with TBI (19 males and 15 females; aged 18–60 years) were recruited. All patients were admitted to the hospital at least 6 h after injury and experienced disturbances of consciousness. Patients were inspected with computed tomography and magnetic resonance imaging scans to clarify diagnosis following admission, and blood samples were collected. The Glasgow Coma Scale (GCS) score (17) was between 9–12 for 12 patients and 3–8 for 22 patients. Only patients with episodes of ICP >20 mm Hg lasting >5 min were included in the study. The exclusion criteria were as follows: i) Pregnancy, ii) severe body damage, iii) open TBI, iv) survival time <3 days, v) history of blood disorder or other diseases affecting coagulation, vi) patients on coagulation therapy and vii) serious systemic diseases prior to or following injury, including cancer, neurodegenerative diseases and congenital developmental disorders. Patients were randomly divided into two treatment groups, including the 7.5% HS and 3% HS treatment group. The basic characteristics of patients in each group are presented in Table I. The ICP, mean arterial pressure (MAP), cerebral perfusion pressure (CPP), heart rate (HR), respiratory rate (RR) and urine volume (UV) of these patients were measured before HS treatment, immediately after receiving HS treatment, and 12 and 24 h post-HS treatment. Prothrombin time (PT), activated partial thromboplastin time (APTT), thrombin time (TT) and fibrinogen (FIB) were measured before HS treatment, immediately following receiving HS treatment, and 6, 12 and 24 h post-HS treatment.
Table I.
Characteristics of the HS treatment groups.
| Treatment groups | ||
|---|---|---|
| Variables | 7.5% HS (n) | 3% HS (n) |
| Sex | ||
| Male | 10 | 9 |
| Female | 8 | 7 |
| Average age (years) | 47.33±16.19 | 46.00±15.03 |
| GCS score | ||
| 9–12 | 6 | 6 |
| 3–8 | 12 | 10 |
GCS, Glasgow Coma Scale; HS, hypertonic saline.
Extraction of peripheral monocyte
EDTA-treated whole blood of patients was centrifuged at 2,000 × g at room temperature for 10 min. Plasma was added to tubes and incubated with Ficoll-Paque PLUS, followed by centrifugation at 400 × g and room temperature for 30 min. The supernatants were then centrifuged at 400 × g at room temperature for 5 min. Peripheral blood mononuclear cells (PBMCs) in the precipitate were collected following centrifugation.
Phenotypic characterization of peripheral monocytes using flow cytometry
PBMCs were washed twice with cold PBS, and incubated with FITC-labeled CD14 and PE-labeled CD16 antibodies for 1 h at 4°C in the dark. After washing with cold PBS, the cells were acquired on a Cytomics FC500 flow cytometer (Beckman Coulter, Inc., Brea, CA, USA). The phenotypes of the monocytes from each group were analyzed using CXP software (version 2.2), which was supplied with the flow cytometer.
Detection of lncRNA in cultured cells using reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
THP-1, Raji and A3 cells were cultured as described previously. Cultured cells were harvested once they reached 80–90% confluence and RNA were extracted using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. Subsequently, RNA concentration was determined using a NanoDrop™ 2000 spectrophotometer (Thermo Fisher Scientific, Inc.). A total of 500 ng RNA was used for reverse transcript using the HiFiScript cDNA Synthesis kit, according to the manufacturer's protocol. ChIPBase (rna.sysu.edu.cn/chipbase) was used to screen for lncRNAs associated with TBI, including 75 upregulated and 22 downregulated lncRNAs. Among these, transcription factors involved in the inflammatory response were screened, including TLRs, IL-6 and TNF-α. Therefore, the expression levels of the lncRNAs (lncRNA4916, lncRNA1403, lncRNA2448-11, lncRNA7411-1, lncRNA4551-1, and lncRNA5189-2) was detected using UltraSYBR One Step RT-qPCR kit (CWBiotech). The forward and reverse primers were as follows: lncRNA4916, forward, 5′-TCCACTGGCTTGGAAATCCT-3′ and reverse, 5′-TACAGGACAGTGGTGCTTCC-3′; lncRNA1403, forward, 5′-GATTCACAACCGTGGCAGGA-3′ and reverse, 5′-TGTCCGCAGTTGGTCATCG-3′; lncRNA2448-11, forward, 5′-CACAGTGAAGAGTTGGGATTTGA-3′ and reverse, 5′-TCAGTAACGGAGGTGATTTAGACA-3′; lncRNA7411-1, forward, 5′-GGCAAGTCTGTTTGTGTGGG-3′ and reverse, 5′-GCCAATTCCTTAGATGCAGGTC-3′; lncRNA4551-1, forward, 5′-AGTCACACTACCAAAGGCCG-3′ and reverse, 5′-GCAAGAGAGACAGATCGTCCA-3′; lncRNA5189-2, forward, 5′-CTCTGCCTATGCTGGACTTGAA-3′ and reverse, 5′-CAGTGGCTTTGGGTGTTGCT-3′; β-actin, forward, 5′-CATGTACGTTGCTATCCAGGC-3′ and reverse, 5′-CTCCTTAATGTCACGCACGAT-3′. The reaction conditions were set according to the manufacturer's protocol: Initial denaturation at 95°C for 5 min, followed by 45 cycles of denaturation at 95°C for 15 sec, annealing at 60°C for 45 sec and extension at 72°C for 30 sec. Relative gene expression was determined using the 2−ΔΔCq method (18). β-actin was used as an internal control, and each experiment was repeated three times.
The expression of lncRNAs and their target genes involved in the inflammatory response was detected in peripheral monocytes using RT-qPCR. Total RNA was extracted from peripheral monocytes using the AllPure DNA/RNA/Protein kit, according to the manufacturer's protocol. Subsequently, total RNA was reverse transcribed into cDNA, as previously described. cDNA was used in qPCR to detect the expression levels of lncRNA2448-11, lncRNA1403, lncRNA5189-2 and lncRNA-related genes, including TNF-α, interleukin (IL)-6, IL-1β, transforming growth factor-β (TGF-β) and thrombomodulin. The primers were follows: TNF-α, forward, 5′-AGCCCATGTTGTAGCAAACC-3′ and reverse, 5′-TGAGGTACAGGCCCTCTGAT-3′; IL-6, forward, 5′-CACAGACAGCCACTCACCTC-3′ and reverse, 5′-TTTTCTGCCAGTGCCTCTTT-3′; IL-1β, forward, 5′-CCACGGCCACATTTGGTT-3′ and reverse, 5′-AGGGAAGCGGTTGCTCATC-3′; TGF-β: forward, 5′-GGTCACCCGCGTGCTA-3′ and reverse, 5′-TGCTGTGTGTACTCTGCTTGAA-3′; thrombomodulin: Forward, 5′-AGGGGCTGGCACTGGTACTCGCAGT-3′ and reverse, 5′-CATGTGCGAAGACCGGCTCCGGCTG-3′. The reaction conditions were as previously described.
Statistical analysis
Data are presented as the mean ± standard deviation of three independent experiments. Differences between multiple groups were analyzed using one-way analysis of variance followed by Tukey's post-hoc test, and Student's t-test was used to analyze differences between two groups in SPSS 22.0 (IBM Corp., Armonk, NY, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
Basic characteristics of patients with TBI treated with HS
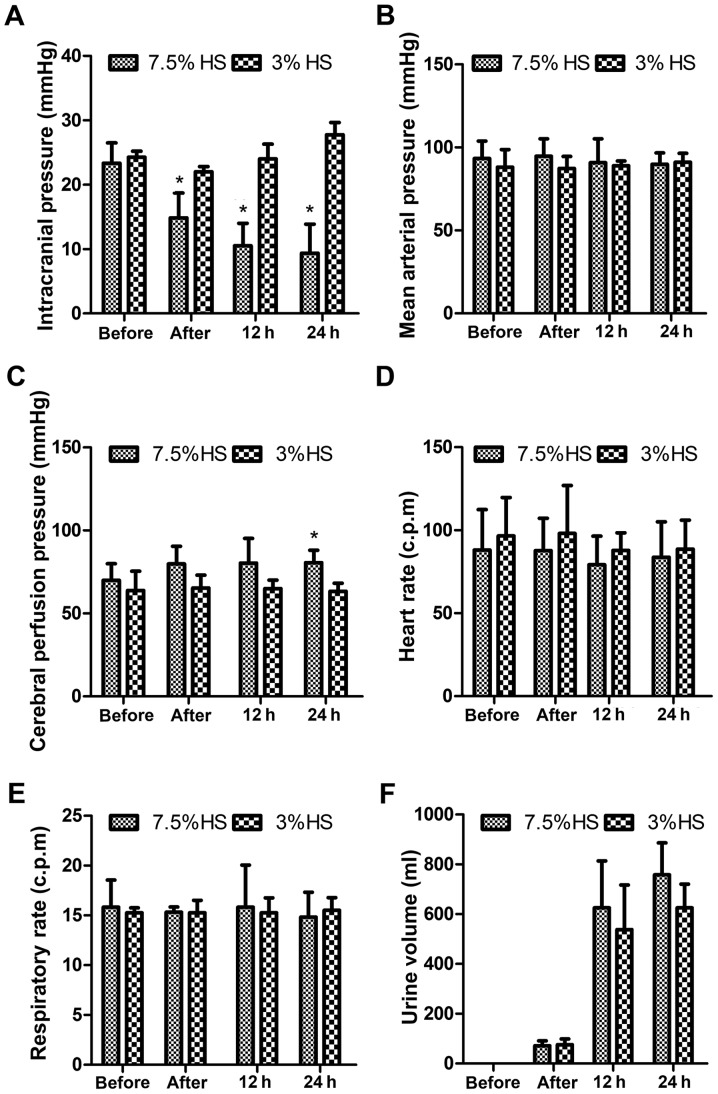
Compared with the 3% HS treatment group, treatment with 7.5% HS treatment significantly decreased the ICP of patients in a time-dependent manner and significantly increased the CPP of patients at 24 h post-treatment (P<0.05; Fig. 1). However, the vital signs of these patients, including MAP, HR, RR and UV, were not significantly different. Indexes associated coagulation function, including PT, APTT, TT and FIB, were also not significantly different.
Figure 1.
Clinical characteristics of patients prior to and following HS treatment. (A) Intracranial pressure, (B) mean arterial pressure, (C) cerebral perfusion pressure, (D) heart rate, (E) respiratory rate and (F) urine volume were measured in patients with traumatic brain injury prior to HS treatment, immediately following HS treatment, and 12 and 24 h post-HS treatment. Data are presented as the mean ± standard deviation of three individual experiments. P-values were calculated using one-way analysis of variance. *P<0.05 vs. the 3% HS. c.p.m, counts per minute; HS, hypertonic saline.
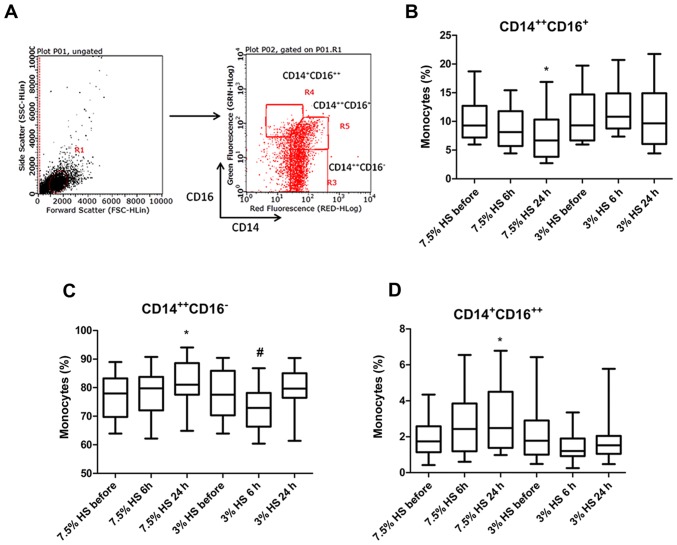
Treatment with 7.5% HS reduces the proportion of CD14++CD16+ inflammatory monocytes
Detection of different peripheral monocyte phenotypes was performed using flow cytometry (Fig. 2A). According to the results, 7.5% HS treatment significantly reduced the proportion of CD14++CD16+ inflammatory monocytes (IMs), which exhibit a pro-inflammatory function at 24 h (P<0.05; Fig. 2B). Following 7.5% HS treatment for 6 and 24 h, the percentage of IMs in total monocytes was 8.83±3.32 and 7.21±3.75%, respectively. Conversely, following 3% HS treatment for 6 and 24 h, the percentage of IMs in total monocytes was 12.06±4.06 and 10.51±4.92%, respectively. However, the frequency of classical monocytes (CMs) exhibited a different trend. Following 7.5% HS treatment for 6 and 24 h, the percentage of CMs in total monocytes was 78.3±7.84 and 82.34±7.41%, whereas following 3% HS treatment for 6 and 24 h, the percentage of IMs in total monocytes was 72.64±8.18 and 79.88±6.57%. The results revealed that 7.5% HS treatment for 24 h significantly increased the proportion of CMs (P<0.05), whilst 3% HS treatment for 6 h significantly decreased the proportion of CMs (P<0.05; Fig. 2C). In addition, the proportion of CD14+CD16++ dendritic cell-like monocytes in total monocytes were significantly increased following 7.5% HS treatment for 24 h (P<0.05; Fig. 2D).
Figure 2.
Phenotypic characterization of peripheral monocytes. (A) Flow cytometry gating strategy for the phenotypic characterization of peripheral monocytes. Percentage (B) CD14++CD16+, (C) CD14++CD16− and (D) CD14+CD16++ monocytes of total PBMCs following 7.5 and 3% HS treatment. Data are presented as the mean ± standard deviation of three individual experiments. P-values were calculated using one-way analysis of variance. *P<0.05 vs. 7.5% HS before. #P<0.05 vs. 3% HS before. CD, cluster of differentiation; HS, hypertonic saline.
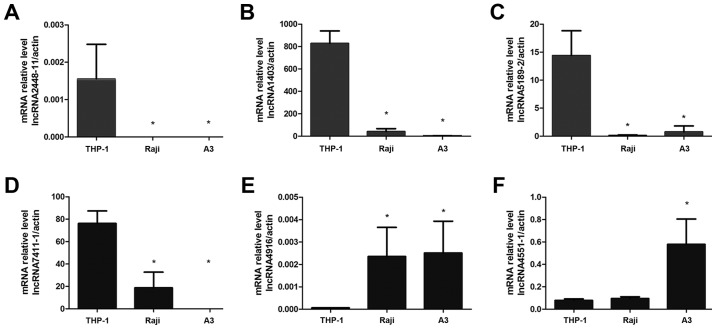
Screening for lncRNAs preferentially expressed in monocytes
To screen for lncRNAs preferentially expressed by monocytes, the expression levels of six lncRNAs, including lncRNA4916, lncRNA1403, lncRNA2448-11, lncRNA7411-1, lncRNA4551-1 and lncRNA5189-2 were detected in the THP-1, Raji and A3 cell lines. The qPCR results indicated that lncRNA2448-11 was only expressed in THP-1 cells and that the expression levels of lncRNA1403 and lncRNA5189-2 were significantly increased in THP-1 cells compared with the other two cell lines (P<0.05; Fig. 3A-C). However, lncRNA7411-1 was expressed in both THP-1 and Raji cells, but not in A3 cells (Fig. 3D). In addition, the expression levels of lncRNA4916 and lncRNA4551-1 were significantly lower in THP-1 compared with in the other two cell lines (P<0.05; Fig. 3E and F). These results demonstrated that lncRNA2448-11, lncRNA1403 and lncRNA5189-2 were preferentially expressed by monocytes.
Figure 3.
Screening of preferentially expressed lncRNAs in a monocyte cell line. The expression levels of (A) lncRNA2448-11, (B) lncRNA1403, (C) lncRNA5189-2, (D) lncRNA7411-1, (E) lncRNA4916, and (F) lncRNA4551-1 were detected in THP-1, Raji and A3 cell lines using reverse transcription-quantitative polymerase chain reaction. Data are presented as the mean ± standard deviation of three individual experiments. P-values were calculated using one-way analysis of variance. *P<0.05 vs. THP-1. lncRNA, long non-coding RNA.
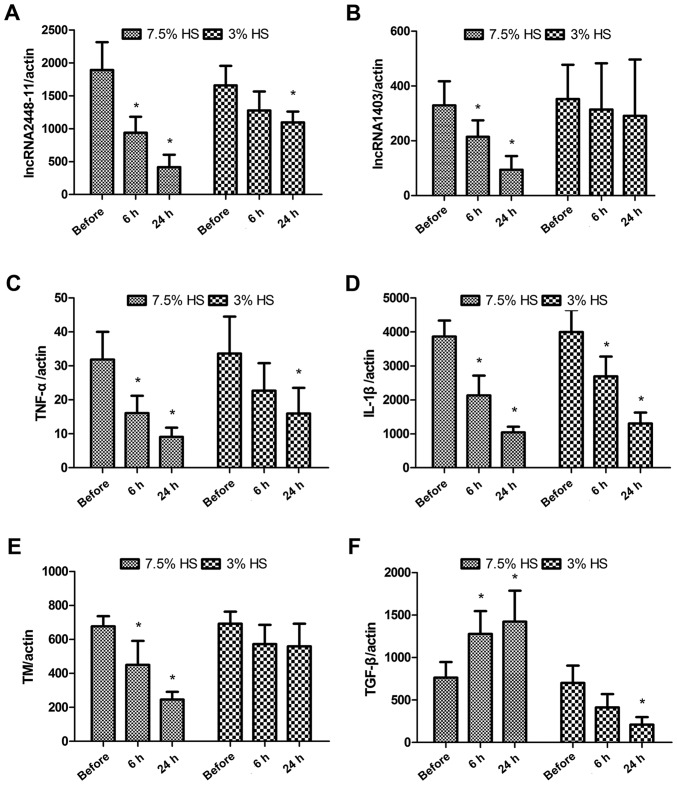
Treatment with 7.5% HS inhibits the expression of lncRNA2448-11, lncRNA1403 and associated genes in peripheral monocytes
As presented in Fig. 4A and B, both 7.5 and 3% HS treatment decreased the expression levels of lncRNA2448-11 and lncRNA1403. However, the expression levels of both lncRNA2448-11 and lncRNA1403 were significantly reduced in the 7.5% HS treatment group, whereas only the expression levels of lncRNA2448-11 were significantly decreased in the 3% HS treatment group at 24 h (P<0.05). The expression levels of lncRNA5189-2 were not significantly different following HS treatment (data not shown). The expression levels of lncRNA-related genes were also measured. Both 7.5 and 3% HS treatment significantly inhibited the expression levels of TNF-α and IL-1β (P<0.05; Fig. 4C and D). Compared with the before group, 7.5% HS treatment significantly decreased the expression levels of thrombomodulin (P<0.05), whereas 3% HS treatment did not affect the expression levels of thrombomodulin (Fig. 4E). For TGF-β, 7.5% HS treatment significantly increased its expression levels compared with the before group (P<0.05), while 3% HS treatment significantly decreased its expression at 24 h (P<0.05; Fig. 4F).
Figure 4.
Treatment with 7.5% HS inhibits the expression of lncRNA2448-11, lncRNA1403 and associated genes in peripheral monocytes. Expression levels of (A) lncRNA2448-11, (B) lncRNA1403, (C) TNF-α, (D) IL-1β, (E) TM and (F) TGF-β in peripheral monocytes were measured before and after HS treatment using reverse transcription-quantitative polymerase chain reaction. Data are presented as the mean ± standard deviation of three individual experiments. P-values were calculated using one-way analysis of variance. *P<0.05 vs. Before. HS, hypertonic saline; IL-, interleukin; lncRNA, long non-coding RNA; TGF-β, transforming growth factor-β; TM, thrombomodulin; TNF-α, tumor necrosis factor-α.
Discussion
The outcome of neuropathological changes induced by TBI is determined by the interaction between inflammations in the central nervous system, systemic inflammatory responses and the coagulation cascade (19). TBI can trigger innate immune responses and host defense responses, by activating microglia and astrocytes (20), cerebral microvascular endothelial cells (21) and peripheral blood leucocytes, including neutrophils and monocytes (22,23). These activated peripheral blood leucocytes can cause secondary brain injury through the release of free radicals, granule proteases and inflammatory cytokines, which can accelerate structural damage to endothelial cells and lead to the formation of a thrombus, ultimately causing terminal organ failure (24). The present study indicated that lncRNAs may serve an important role in the development of TBI. The results demonstrated that 7.5% HS treatment was more effective than 3% HS treatment for TBI. HS 7.5% was able to regulate the phenotype and cytokine secretion of monocytes through the expression of lncRNA 2448-11 and lncRNA 1403, resulting in reduced ICP in patients with TBI.
Monocytes account for 5–10% of PBMCs, but studies have not fully elucidated the effect of TBI on the biological characteristics of monocytes. A previous study revealed that the number of monocytes was significantly reduced a few hours following TBI in a mouse model (25), but clinical observations demonstrated that TBI increased the number of peripheral monocytes (11,24) and that the number of peripheral blood mononuclear cells was 2.7 times more compared with the control group. Using a closed TBI mouse model, Schwulst et al (24) demonstrated that 60 days following trauma, the number of peripheral Ly6C− anti-inflammatory monocytes in the TBI group was significantly increased compared with in the sham group and the expression levels of IL-10 were increased in peripheral monocytes, indicating that the differentiation of monocytes into an anti-inflammatory phenotype was activated following TBI (26). The results in the present study indicated that 7.5% HS treatment significantly reduced the proportion of CD14++CD16+ IMs as well as downregulated the expression of genes encoding for proinflammatory cytokines, including TNF-α and IL-1β.
The interaction between inflammation and coagulation following TBI is mediated by vascular endothelial cells. Injured or cytokine-activated endothelial cells participate in the regulation of coagulation and fibrinolysis via TF and thrombomodulin. TF is a molecule with a coagulant function, whereas thrombomodulin is a molecule with anticoagulant function. The balance between TF and thrombomodulin is important for the maintenance of the coagulation system. Dysfunction of the coagulation system is mostly mediated by TF accumulation in the brain tissue of patients with TBI. TNF-α secreted from endothelial cells and monocytes is a strong inducer of TF, and inhibits the expression of thrombomodulin on the surface of the cell membrane (27). Monocytes infiltrating injured tissues in the acute stage of TBI can release pro- and anti-inflammatory factors into cerebral spinal fluid and peripheral blood (28,29). In vivo experiments and clinical research on closed TBI demonstrated that the expression levels of TNF-α and IL-1β in the PBMCs of patients were increased 3 to 8 h following TBI, followed by an increase in the expression levels of IL-6 and IL-10 (30).
In addition to inducing the expression of TF, TNF-α can also induce capillary percolation and cerebral edema, upregulate the expression of intercellular adhesion molecule-1 and vascular cell adhesion molecule-1, and aggravate craniocerebral circulatory disturbances (31). In vivo and in vitro experiments indicated that HS treatment inhibited the innate immune response and the production of cytokines, thereby protecting nerve cells following TBI (32). In the acute stage of central nervous system injury, increased expression of TNF-α can aggravate tissue injury, but moderate expression of TNF-α is necessary for tissue recovery (33).
The results from the present study demonstrated that compared with 3% HS treatment, 7.5% HS treatment significantly inhibited the expression of TNF-α and IL-1β, whilst it increased the expression of TGF-β. These effects are expected to reduce the immune response, promote synthesis of collagen and fiber-bound proteins, and serve an important role in the repair process of injured tissue. In addition, 7.5% HS treatment significantly inhibited the expression of thrombomodulin, downregulated the expression of TNF-α and IL-1β, indicating that HS may have prevented the occurrence of disseminated intravascular coagulation induced coagulation and fibrinolysis system imbalance, through regulation of thrombomodulin.
lncRNA is a type of functional RNA that contains >200 nucleotides. lncRNA rarely participates in protein synthesis but is important in the regulation of transcription, post-transcription and epigenetics. lncRNA can affect the entire process of gene expression, including transcription initiation, transcription prolongation, RNA synthesis, RNA stability and translation. The regulatory effect of lncRNA on the innate immune system has also been revealed (34). Previous studies have indicated that knockdown of lncRNA can inhibit the expression of numerous inflammatory genes, including IL-1β and TNF-α (35,36). TBI can induce the secretion of cytokines, activate astrocytes and microglia, and recruit blood immune cells to the brain (37). A previous study indicated that the recruitment of cytokines following TBI is associated with lncRNAs (38). The findings indicated that the expression of lncRNAs and their target mRNAs may be critical for the development of TBI. Microarray experiments in the hippocampus and pericontusion cortex of mice revealed that following TBI, the expression of numerous microRNAs and lncRNAs is significantly altered (39). It was also identified that lncRNA may serve an important role in the regulation of neural damage and repair. In the present study, preferential expression of lncRNAs in cultured monocytes was screened and the results were verified in peripheral monocytes, in order to investigate the association between altered lncRNA expression and coagulation function.
In conclusion, the present study demonstrated that 7.5% HS treatment altered the expression of lncRNA2448-11 and lncRNA1403, therefore affecting the phenotype of peripheral monocytes and expression levels of cytokines, maintaining balance of the fibrinolytic system in patients with TBI, decreasing ICP, and ultimately reducing secondary injury to the brain. However, the findings are preliminary, and further experiments are required to investigate the clinical significance of lncRNAs and to confirm whether lncRNAs can be utilized therapeutically for TBI. One of the limitations of the present study is it was only a single-center study, In addition, maintenance of coagulofibrinolytic homeostasis is complex; therefore, other immune cells may also participate in this process apart from monocytes. The present study was an exploratory research and additional key factors involved in the inflammatory response, including platelet activating factor (PAF) and cyclooxygenase will be taken into consideration in future studies.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Scientific Fund of Logistic University of Chinese People's Armed Police Force (grant no. WHJ2015021).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
XY, YC and JL performed the experiment and wrote the manuscript. YL and XZ designed the experiment, and check and revised the manuscript. LC and HR collected the blood samples and measured the physiological indexes of TBI patients.
Ethics approval and consent to participate
The present study was approved by the Medical Ethics and Human Clinical Trial Committee of the Affiliated Hospital of the Logistic University of the Chinese People's Armed Police Force (Tianjin, China) and was carried out in compliance with the Helsinki Declaration. Written informed consent was obtained from all patients prior to recruitment onto the study.
Patient consent for publication
Written informed consent was obtained from all patients prior to recruitment onto the study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Stein SC, Georgoff P, Meghan S, Mizra K, Sonnad SS. 150 years of treating severe traumatic brain injury: A systematic review of progress in mortality. J Neurotrauma. 2010;27:1343–1353. doi: 10.1089/neu.2009.1206. [DOI] [PubMed] [Google Scholar]
- 2.Olesen J, Gustavsson A, Svensson M, Wittchen HU, Jönsson B. The economic cost of brain disorders in Europe. Eur J Neurol. 2012;19:155–162. doi: 10.1111/j.1468-1331.2011.03590.x. [DOI] [PubMed] [Google Scholar]
- 3.Joseph B, Haider A, Rhee P. Traumatic brain injury advancements. Curr Opin Crit Care. 2015;21:506–511. doi: 10.1097/MCC.0000000000000247. [DOI] [PubMed] [Google Scholar]
- 4.Algattas H, Huang JH. Traumatic brain injury pathophysiology and treatments: Early, intermediate, and late phases post-injury. Int J Mol Sci. 2013;15:309–341. doi: 10.3390/ijms15010309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zink BJ, Szmydynger-Chodobska J, Chodobski A. Emerging concepts in the pathophysiology of traumatic brain injury. Psychiatr Clin North Am. 2010;33:741–756. doi: 10.1016/j.psc.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Kumar A, Loane DJ. Neuroinflammation after traumatic brain injury: Opportunities for therapeutic intervention. Brain Behav Immun. 2012;26:1191–1201. doi: 10.1016/j.bbi.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Alali AS, Vavrek D, Barber J, Dikmen S, Nathens AB, Temkin NR. Comparative study of outcome measures and analysis methods for traumatic brain injury trials. J Neurotrauma. 2015;32:581–589. doi: 10.1089/neu.2014.3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy after traumatic brain injury. Neurosurgery. 2012;70:1334–1345. doi: 10.1227/NEU.0b013e31824d179b. [DOI] [PubMed] [Google Scholar]
- 9.Stojkovic S, Thulin Å, Hell L, Thaler B, Rauscher S, Baumgartner J, Gröger M, Ay C, Demyanets S, Neumayer C, et al. IL-33 stimulates the release of procoagulant microvesicles from human monocytes and differentially increases tissue factor in human monocyte subsets. Thromb Haemost. 2017;117:1379–1390. doi: 10.1160/TH16-10-0784. [DOI] [PubMed] [Google Scholar]
- 10.Junger WG, Rhind SG, Rizoli SB, Cuschieri J, Baker AJ, Shek PN, Hoyt DB, Bulger EM. Prehospital hypertonic saline resuscitation attenuates the activation and promotes apoptosis of neutrophils in patients with severe traumatic brain injury. Shock. 2013;40:366–374. doi: 10.1097/SHK.0000000000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rasslan R, Utiyama EM, Marques GM, Ferreira TC, da Costa VA, de Victo NC, Rasslan S, Montero EF. Inflammatory activity modulation by hypertonic saline and pentoxifylline in a rat model of strangulated closed loop small bowel obstruction. Int J Surg. 2014;12:594–600. doi: 10.1016/j.ijsu.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Rhind SG, Crnko NT, Baker AJ, Morrison LJ, Shek PN, Scarpelini S, Rizoli SB. Prehospital resuscitation with hypertonic saline-dextran modulates inflammatory, coagulation and endothelial activation marker profiles in severe traumatic brain injured patients. J Neuroinflammation. 2010;7:5. doi: 10.1186/1742-2094-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carpenter S, Aiello D, Atianand MK, Ricci EP, Gandhi P, Hall LL, Byron M, Monks B, Henry-Bezy M, Lawrence JB, et al. A long noncoding RNA mediates both activation and repression of immune response genes. Science. 2013;341:789–792. doi: 10.1126/science.1240925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang P, Xue Y, Han Y, Lin L, Wu C, Xu S, Jiang Z, Xu J, Liu Q, Cao X. The STAT3-binding long noncoding RNA lnc-DC controls human dendritic cell differentiation. Science. 2014;344:310–313. doi: 10.1126/science.1251456. [DOI] [PubMed] [Google Scholar]
- 15.Rapicavoli NA, Qu K, Zhang J, Mikhail M, Laberge RM, Chang HY. A mammalian pseudogene lncRNA at the interface of inflammation and anti-inflammatory therapeutics. Elife. 2013;2:e00762. doi: 10.7554/eLife.00762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Costa FF. Non-coding RNAs: Meet thy masters. Bioessays. 2010;32:599–608. doi: 10.1002/bies.200900112. [DOI] [PubMed] [Google Scholar]
- 17.Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The Glasgow Coma Scale at 40 years: Standing the test of time. Lancet Neurol. 2014;13:844–854. doi: 10.1016/S1474-4422(14)70120-6. [DOI] [PubMed] [Google Scholar]
- 18.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 19.Hinson HE, Rowell S, Schreiber M. Clinical evidence of inflammation driving secondary brain injury: A systematic review. J Trauma Acute Care Surg. 2015;78:184–191. doi: 10.1097/TA.0000000000000468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lehnardt S. Innate immunity and neuroinflammation in the CNS: The role of microglia in Toll-like receptor-mediated neuronal injury. Glia. 2010;58:253–263. doi: 10.1002/glia.20928. [DOI] [PubMed] [Google Scholar]
- 21.Balabanov R, Goldman H, Murphy S, Pellizon G, Owen C, Rafols J, Dore-Duffy P. Endothelial cell activation following moderate traumatic brain injury. Neurol Res. 2001;23:175–182. doi: 10.1179/016164101101198514. [DOI] [PubMed] [Google Scholar]
- 22.Carson MJ, Thrash JC, Walter B. The cellular response in neuroinflammation: The role of leukocytes, microglia and astrocytes in neuronal death and survival. Clin Neurosci Res. 2006;6:237–245. doi: 10.1016/j.cnr.2006.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nguyen HX, O'Barr TJ, Anderson AJ. Polymorphonuclear leukocytes promote neurotoxicity through release of matrix metalloproteinases, reactive oxygen species, and TNF-alpha. J Neurochem. 2007;102:900–912. doi: 10.1111/j.1471-4159.2007.04643.x. [DOI] [PubMed] [Google Scholar]
- 24.Schwulst SJ, Trahanas DM, Saber R, Perlman H. Traumatic brain injury-induced alterations in peripheral immunity. J Trauma Acute Care Surg. 2013;75:780–788. doi: 10.1097/TA.0b013e318299616a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liao Y, Liu P, Guo F, Zhang ZY, Zhang Z. Oxidative burst of circulating neutrophils following traumatic brain injury in human. PLoS One. 2013;8:e68963. doi: 10.1371/annotation/73ce45d3-4478-4c06-a4d2-3274b6222bae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chu AJ. Tissue factor, blood coagulation, and beyond: An overview. Int J Inflam. 2011;2011:367284. doi: 10.4061/2011/367284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lu J, Goh SJ, Tng PY, Deng YY, Ling EA, Moochhala S. Systemic inflammatory response following acute traumatic brain injury. Front Biosci (Landmark Ed) 2009;14:3795–3813. doi: 10.2741/3489. [DOI] [PubMed] [Google Scholar]
- 28.D'Mello C, Le T, Swain MG. Cerebral microglia recruits monocytes into the brain in response to tumor necrosis factoralpha signaling during peripheral organ inflammation. J Neurosci. 2009;29:2089–2102. doi: 10.1523/JNEUROSCI.3567-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maier B, Schwerdtfeger K, Mautes A, Holanda M, Müller M, Steudel WI, Marzi I. Differential release of interleukines 6, 8, and 10 in cerebrospinal fluid and plasma after traumatic brain injury. Shock. 2001;15:421–426. doi: 10.1097/00024382-200115060-00002. [DOI] [PubMed] [Google Scholar]
- 30.Kadhim HJ, Duchateau J, Sébire G. Cytokines and brain injury: Invited review. J Intensive Care Med. 2008;23:236–249. doi: 10.1177/0885066608318458. [DOI] [PubMed] [Google Scholar]
- 31.Summy-Long JY, Hu S. Peripheral osmotic stimulation inhibits the brain's innate immune response to microdialysis of acidic perfusion fluid adjacent to supraoptic nucleus. Am J Physiol Regul Integr Comp Physiol. 2009;297:R1532–R1545. doi: 10.1152/ajpregu.00340.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woodcock T, Morganti-Kossmann MC. The role of markers of inflammation in traumatic brain injury. Front Neurol. 2013;4:18. doi: 10.3389/fneur.2013.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carpenter S. Long noncoding RNA: Novel links between gene expression and innate immunity. Virus Res. 2016;212:137–145. doi: 10.1016/j.virusres.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 34.Cui H, Xie N, Tan Z, Banerjee S, Thannickal VJ, Abraham E, Liu G. The human long noncoding RNA lnc-IL7R regulates the inflammatory response. Eur J Immunol. 2014;44:2085–2095. doi: 10.1002/eji.201344126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Z, Chao TC, Chang KY, Lin N, Patil VS, Shimizu C, Head SR, Burns JC, Rana TM. The long noncoding RNA THRIL regulates TNFα expression through its interaction with hnRNPL. Proc Natl Acad Sci USA. 2014;111:1002–1007. doi: 10.1073/pnas.1313768111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gyoneva S, Ransohoff RM. Inflammatory reaction after traumatic brain injury: Therapeutic potential of targeting cell-cell communication by chemokines. Trends Pharmacol Sci. 2015;36:471–480. doi: 10.1016/j.tips.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang CF, Zhao CC, Weng WJ, Lei J, Lin Y, Mao Q, Gao GY, Feng JF, Jiang JY. Alteration in long non-coding RNA expression after traumatic brain injury in rats. J Neurotrauma. 2017;34:2100–2108. doi: 10.1089/neu.2016.4642. [DOI] [PubMed] [Google Scholar]
- 38.Sordillo PP, Sordillo LA, Helson L. Bifunctional role of pro-inflammatory cytokines after traumatic brain injury. Brain Inj. 2016;30:1043–1053. doi: 10.3109/02699052.2016.1163618. [DOI] [PubMed] [Google Scholar]
- 39.Liu L, Sun T, Liu Z, Chen X, Zhao L, Qu G, Li Q. Traumatic brain injury dysregulates microRNAs to modulate cell signaling in rat hippocampus. PLoS One. 2014;9:e103948. doi: 10.1371/journal.pone.0103948. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.