Abstract
Lambert-Eaton myasthenic syndrome (LEMS) is a representative paraneoplastic neurological syndrome. Recently, nivolumab, an anti-programmed cell death 1 inhibitor, has been approved for advanced non-small-cell lung cancer. Careful attention should be paid to immune-related adverse events (irAEs), including neurotoxicity. We herein report a 73-year-old woman with LEMS that occurred during nivolumab treatment for pulmonary squamous cell carcinoma. After the 20th week of nivolumab, she experienced various neurological symptoms such as ptosis, lower limb weakness, and photophobia. Findings from a nerve conduction study and a positive anti-P/Q-type voltage-gated calcium channel antibody made a diagnosis of LEMS. Pyridostigmine and 3,4-diaminopyridine temporarily improved her symptoms. This was the first case of LEMS as a neurological irAE. LEMS should be considered as a possible neurological irAE.
Keywords: Lambert-Eaton myasthenic syndrome, Squamous cell carcinoma, Nivolumab, Immune checkpoint inhibitor, Immune-related neurological adverse events
Introduction
Lambert-Eaton myasthenic syndrome (LEMS) is a neuromuscular autoimmune disorder characterized by muscle weakness and autonomic dysfunction, and is a representative paraneoplastic neurological syndrome (PNS). Approximately 50–60% of patients with LEMS are associated with malignant tumor [1]. Although most patients with LEMS are associated with small-cell lung cancer (SCLC), several reports have described associations of LEMS with other malignant tumors, such as stomach adenocarcinoma, lymphoproliferative disorders, malignant thymoma, and colonic adenocarcinoma [2, 3, 4]. Anti-P/Q-type voltage-gated calcium channel (VGCC) antibody is detected in approximately 85–90% of patients [5]. When LEMS is observed with malignant tumor, cancer-directed therapies should be prioritized. Regardless of the coexistence of a malignant tumor, symptomatic treatment for LEMS is acetylcholine esterase inhibitor or 3,4-diaminopyridine (DAP). In particular, 3,4-DAP acts directly on the neuromuscular junction.
Currently, there are several immune checkpoint inhibitors (ICIs) that have revolutionized the treatment strategy for various types of cancers. In Japan, as programmed cell death 1 (PD-1) inhibitors, nivolumab and pembrolizumab have been approved for advanced non-small-cell lung cancer (NSCLC). ICI has a wide spectrum of adverse effects, which are quite different from conventional cytotoxic and molecular-targeted chemotherapy. Previously, various types of neurological immune-related adverse events (irAEs), such as encephalopathies, meningoradiculoneuritis, Guillain-Barré-like syndromes, and myasthenic syndromes, have been reported [6]. In particular, myasthenia gravis is well-known as a neurological irAE. The overall incidence of neurological irAE has been reported to be 6.1% with anti-PD1 antibodies [6]. We herein report a case of LEMS caused by nivolumab for pulmonary squamous cell carcinoma.
Case
A 73-year-old woman had been diagnosed with advanced squamous cell lung cancer with multiple bone metastases (c-stage IV, cT2bN0M1b in the 7th TNM classification) 2 years prior to this study. She started nivolumab (2 mg/kg, biweekly) as fourth-line regimen after carboplatin plus nanoparticle albumin-bound paclitaxel, docetaxel, and S-1. Nivolumab successfully provided partial response (PR). However, she was diagnosed with hypothyroidism in the 12th week after the initiation of nivolumab.
In the 20th week of nivolumab, she was found to have ptosis and lower limb weakness. Moreover, she experienced photophobia in the 36th week. Thereafter, these symptoms gradually deteriorated. She could not walk without a cane in the 48th week. Myasthenia gravis was suspected as nivolumab-induced irAE, and then she was referred to neurologists. She was admitted to our hospital for the purpose of diagnosis and treatment of these neurological symptoms in the 51st week of nivolumab.
A physical examination revealed that her body temperature, pulse rate, and blood pressure were 36.2°C, regular at 81 beats/min, and 132/79 mm Hg, respectively. Laboratory analyses showed that blood cell count, biochemical profile, and carcinoembryonic antigen were within the normal range. Anti-thyroglobulin antibody was positive, suggesting a possible irAE of hypothyroidism. Chest computed tomography (CT) showed right hilar lymphadenopathy and the primary tumor in the right lower lobe. The tumor kept providing PR even after the 19th cycle of nivolumab (Fig. 1).
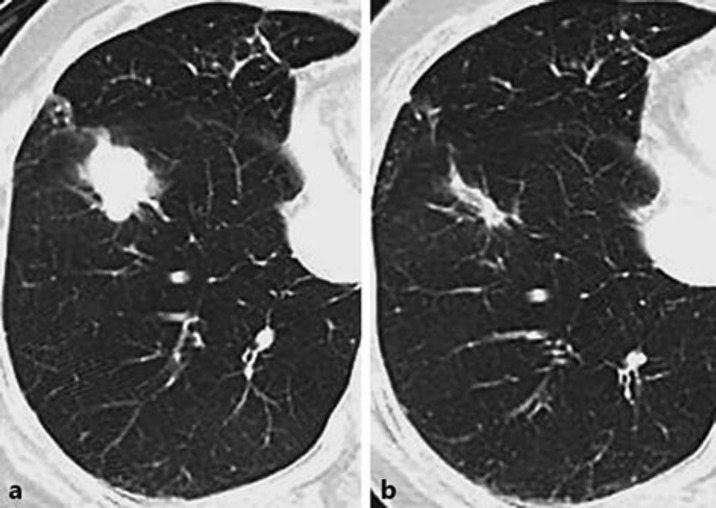
Fig. 1.
Chest computed tomography showed right hilar lymphadenopathy and right lower lobe lung mass (a), and these sizes reduced after the 19th cycle of nivolumab (b).
Neurological examinations presented bilateral ptosis and mild muscle weakness that was dominant in the proximal muscle of the upper and lower limbs. Reactivities of the tendon reflex were diminished or absent. Her ptosis improved after exercise. She had a slightly waddling gait. She also had photophobia, dry mouth, and constipation as signs of the autonomic nervous system. She did not have any sensory disturbance.
In an edrophonium test, there were no appreciable changes to her ptosis, but her waddling gait had improved slightly. In an ophthalmic drug test of phenylephrine, an adrenergic α1 receptor agonist, her ptosis had significantly improved with dilation of the pupil. These results suggested that her ptosis was caused by Horner syndrome. Serum acetylcholine receptor (AchR) antibody was negative. Nerve conduction studies of the motor nerves of her limbs detected low-amplitude compound muscle action potentials (CMAP) (Fig. 2a). The CMAP increased more than twice after brief exercise (Fig. 2b). Repetitive nerve stimulations in her right abductor digiti minimi muscle showed a waning phenomenon in 3-Hz repetitive stimulation and a waxing phenomenon in 10- and 20-Hz repetitive stimulations (Fig. 3). Based on these results, we diagnosed LEMS. Thereafter, anti-P/Q-type VGCC antibodies turned out to be positive.
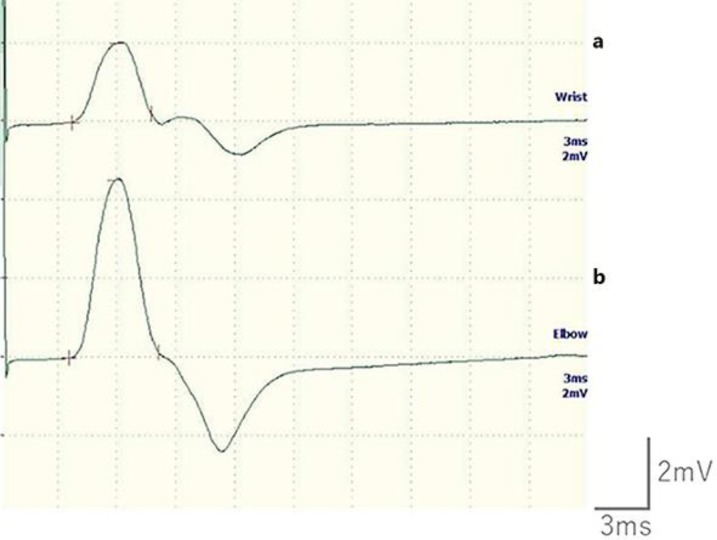
Fig. 2.
The compound muscle action potentials (CMAP) amplitude of the patient's right median nerve was very small (2.03 mV) during relaxation (a); however, the CMAP increased to 4.52 mV soon after her muscles contracted strongly (b).
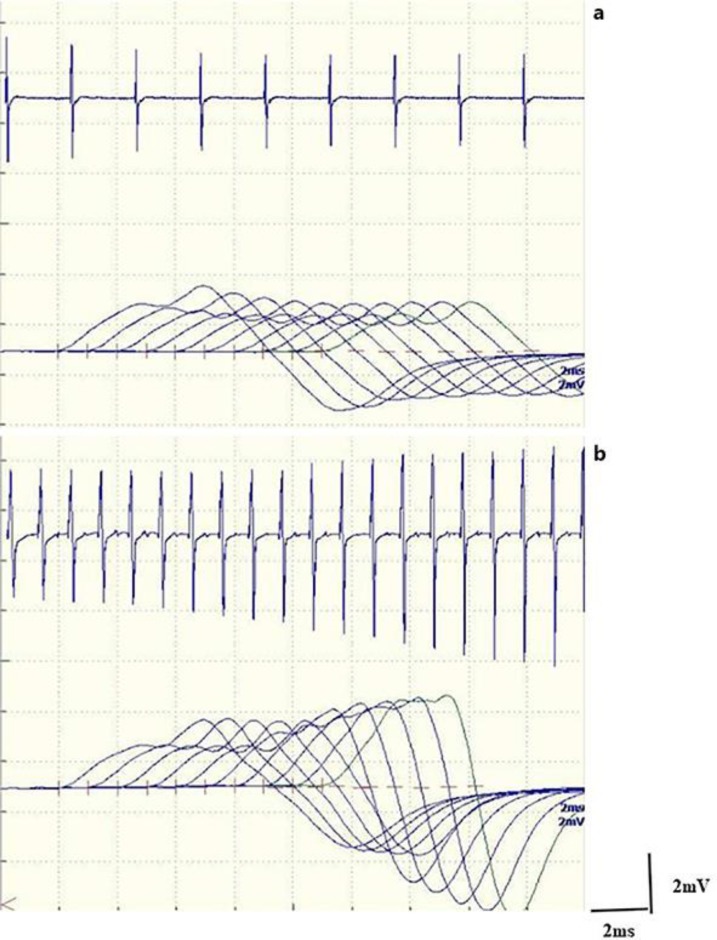
Fig. 3.
A 3-Hz repetitive nerve stimulation test of the patient's right abductor muscle of the little finger showed a gradual amplitude decrease (a), while 10-Hz repetitive nerve stimulation showed a gradual amplitude increase (b).
Her waddling gait improved slightly by an oral cholinesterase inhibitor, pyridostigmine. We restarted nivolumab for lung cancer. However, 6 weeks after the restart of nivolumab, chest CT scan showed ground-glass opacity in the periphery of the right middle lobe and the right lower lobe. We suspected nivolumab-induced interstitial pneumonia, and then discontinued nivolumab. Oral prednisolone (20 mg/day for 7 days) improved the ground-glass opacities but did not change her neurological symptoms. Four months after the definite diagnosis of LEMS, her fatigue and ptosis gradually deteriorated. Additional administration of a cholinesterase inhibitor, ambenonium, failed to improve her symptoms. We switched from pyridostigmine and ambenonium to 3,4-DAP with an anti-acetylcholinesterase inhibitor that was approved by the ethics committee of our hospital. Her ptosis, gait disturbance, and photophobia improved with 15 mg of 3,4-DAP per day. Ten months after the definite diagnosis of LEMS, chest CT detected metastases to mediastinal lymph nodes and confirmed the progression of her lung cancer. Although she received 3,4-DAP that was increased from 15 to 45 mg per day, her symptoms progressed gradually. She could walk independently with a cane indoors 16 months after the diagnosis of LEMS.
Discussion
To our knowledge, this is the first recorded case of LEMS caused by nivolumab. Our report alerts oncologists to LEMS as a possible neurological irAE due to nivolumab. In our case, it was difficult to distinguish neurological irAE from PNS as the cause of LEMS. We finally considered our LEMS as a neurological irAE, because of the onset time and cancer histology. First, the typical onset time of neurological symptoms due to irAEs and PNS is different. The former usually occurs during the induction phase after a median of 5.5 (range, 1–20) cycles of anti-PD-1 inhibitors [7], while the latter usually occurs before a confirmed diagnosis of malignant tumor [2, 4, 8]. However, the range of these onset times is not specific, but various. Although irAEs, in most cases, appear during ICI treatment [9], late-onset irAEs occasionally happen even after discontinuation of ICI treatment. Neurological symptoms preceded the confirmed diagnosis of malignancy in 84% of Japanese patients with seronegative PNS-LEMS [2]. However, many cases of late-onset PNS have been reported. We also reported a case of paraneoplastic motor neuron disease that had emerged after a remarkable reduction in tumor size by chemotherapy [10]. In this case, the onset time of the neurological symptoms was more than 2 years after the diagnosis of lung cancer and 20 weeks after the introduction of nivolumab. In addition, at that time, nivolumab still maintained PR. Second, regarding PNS-LEMS, squamous cell carcinoma is a rare malignant histology, but SCLC is the most common histology. A Japanese retrospective study of 110 patients with LEMS revealed that 61, 8, and 31% of the patients had SCLC, other malignancies, and nonmalignancy, respectively [2]. A prospective UK observational study showed that, in 26, 8, and 3% of patients with SCLC, neurological symptoms unrelated to LEMS, elevated serum level of VGCC antibodies, and clinically and electro-physiologically confirmed LEMS were observed, respectively [11]. To our knowledge, there are few case reports of pulmonary squamous cell carcinoma with LEMS [12, 13, 14]. Thus, in terms of onset time and histology, neurological irAE was a more reasonable cause of LEMS than PNS.
Notably, our LEMS was gradually progressive even after discontinuation of nivolumab. We did not try strong and long-term immunosuppressive therapy, which has been effectively used in many cases with other neurological irAEs [15]. However, low-dose and short-term corticosteroid was ineffective in our case. Various standard drugs for LEMS, such as pyridostigmine, ambenonium, and 3,4-DAP, relieved her neurological symptoms for a while, but were only temporarily palliative. Thus, irAE-LEMS may be intractable. In conclusion, we describe the first case of LEMS due to nivolumab. LEMS should be considered as a possible neurological irAE.
Statement of Ethics
The patients provided written informed consent for the publication of this report.
Disclosure Statement
The authors declare that they have no conflicts of interest.
Acknowledgments
We are grateful to Professor Masakatsu Motomura at the Department of Clinical Neuroscience and Neurology, Nagasaki University, for his measurement of anti-P/Q-type VGCC antibody. We also thank Dr. Suguru Yamamoto and Dr. Kentaro Masuhiro at the Department of Respiratory Medicine, Osaka Police Hospital, for their management of this patient.
References
- 1.Titulaer MJ, Lang B, Verschuuren JJ. Lambert-Eaton myasthenic syndrome: from clinical characteristics to therapeutic strategies. Lancet Neurol. 2011 Dec;10((12)):1098–107. doi: 10.1016/S1474-4422(11)70245-9. [DOI] [PubMed] [Google Scholar]
- 2.Nakao YK, Motomura M, Fukudome T, Fukuda T, Shiraishi H, Yoshimura T, et al. Seronegative Lambert-Eaton myasthenic syndrome: study of 110 Japanese patients. Neurology. 2002 Dec;59((11)):1773–5. doi: 10.1212/01.wnl.0000037485.56217.5f. [DOI] [PubMed] [Google Scholar]
- 3.Takamori M. An autoimmune channelopathy associated with cancer: Lambert-Eaton myasthenic syndrome. Intern Med. 1999 Feb;38((2)):86–96. doi: 10.2169/internalmedicine.38.86. [DOI] [PubMed] [Google Scholar]
- 4.Voltz R. Paraneoplastic neurological syndromes: an update on diagnosis, pathogenesis, and therapy. Lancet Neurol. 2002 Sep;1((5)):294–305. doi: 10.1016/s1474-4422(02)00135-7. [DOI] [PubMed] [Google Scholar]
- 5.Lennon VA, Kryzer TJ, Griesmann GE, O'Suilleabhain PE, Windebank AJ, Woppmann A, et al. Calcium-channel antibodies in the Lambert-Eaton syndrome and other paraneoplastic syndromes. N Engl J Med. 1995 Jun;332((22)):1467–74. doi: 10.1056/NEJM199506013322203. [DOI] [PubMed] [Google Scholar]
- 6.Cuzzubbo S, Javeri F, Tissier M, Roumi A, Barlog C, Doridam J, Lebbe C, Belin C, Ursu R, Carpentier AF. Neurological adverse events associated with immune checkpoint inhibitors: Review of the literature. European journal of cancer (Oxford, England: 1990) 2017;73:1–8. doi: 10.1016/j.ejca.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Kao JC, Liao B, Markovic SN, Klein CJ, Naddaf E, Staff NP, et al. Neurological Complications Associated With Anti-Programmed Death 1 (PD-1) Antibodies. JAMA Neurol. 2017 Oct;74((10)):1216–22. doi: 10.1001/jamaneurol.2017.1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miao S, Liao S, Li H, Niu B, Hu H, Qian Y, et al. Retrospective study of paraneoplastic neurological syndromes in a Chinese Han population from Shandong, East China. Int J Neurosci. 2018 Sep;128((9)):821–7. doi: 10.1080/00207454.2018.1430693. [DOI] [PubMed] [Google Scholar]
- 9.Kumar V, Chaudhary N, Garg M, Floudas CS, Soni P, Chandra AB. Current Diagnosis and Management of Immune Related Adverse Events (irAEs) Induced by Immune Checkpoint Inhibitor Therapy. Front Pharmacol. 2017 Feb;8:49. doi: 10.3389/fphar.2017.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minami S, Okazaki T, Hamaguchi M, Shiraishi S, Yamamoto S, Ogata Y, et al. International Cancer Conference Journal. Vol. 3. Springer; 2014. Small-cell lung cancer: a case report on the manifestation of paraneoplastic motor neuron disease after effective tumor shrinkage during chemotherapy; pp. pp 247–251. [Google Scholar]
- 11.Payne M, Bradbury P, Lang B, Vincent A, Han C, Newsom-Davis J, Talbot D. Prospective study into the incidence of Lambert Eaton myasthenic syndrome in small cell lung cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2010;5:34–38. doi: 10.1097/JTO.0b013e3181c3f4f1. [DOI] [PubMed] [Google Scholar]
- 12.Dai Y, Li P, Yan S, Xia X, Li Z, Xia M. Lung squamous carcinoma with two paraneoplastic syndromes: dermatomyositis and Lambert-Eaton myasthenic syndrome. Clin Respir J. 2016 Jul;10((4)):495–9. doi: 10.1111/crj.12229. [DOI] [PubMed] [Google Scholar]
- 13.Katada E, Nakamura T, Watanabe H, Matsukawa N, Ojika K, Sobue G. [Lambert-Eaton myasthenic syndrome associated with pulmonary squamous cell carcinoma and circulating anti-P/Q-type voltage-gated calcium channel antibody] Rinsho shinkeigaku = Clinical neurology. 2010;50:17–19. doi: 10.5692/clinicalneurol.50.17. [DOI] [PubMed] [Google Scholar]
- 14.Tchouhadjian C, Barlesi F, Doddoli C, Escarguel B, Thomas P, Witjas T, et al. [Difficulties associated with Lambert-Eaton syndrome] Rev Mal Respir. 2004 Dec;21((6 Pt 1)):1167–70. doi: 10.1016/s0761-8425(04)71594-6. [DOI] [PubMed] [Google Scholar]
- 15.Suzuki S, Ishikawa N, Konoeda F, Seki N, Fukushima S, Takahashi K, et al. Nivolumab-related myasthenia gravis with myositis and myocarditis in Japan. Neurology. 2017 Sep;89((11)):1127–34. doi: 10.1212/WNL.0000000000004359. [DOI] [PubMed] [Google Scholar]