Abstract
OBJECTIVE:
The present study aimed to assess the validity and reliability of Geriatric Depression-15 Scale (GDS-15) in Turkish older adults and to compare the results with Diagnostic and Statistical Manual of Mental Disorders-fifth edition (DSM-5) depression criteria.
METHODS:
A total of 329 outpatients were enrolled. In the first step, the patients underwent the Mini-Mental State Examination. After assessing whether the patients meet the diagnosis of depression based on DSM-5 diagnostic criteria, another researcher applied the long form of GDS. After sorting the items of short form out of the long form, two separate scores were obtained. The scores of GDS-30 and GDS-15 scales were compared with the scores of DSM-5.
RESULTS:
The correlation of GDS-30 with GDS-15 was r=0.966 (p<0.001). The analysis performed considering DSM-5 criteria revealed that the sensitivity, specificity, positive predictive value, and negative predictive value of GDS-15 in determining depression were 92%, 91%, 76%, and 97%, respectively, when the cutoff value was taken as ≥5. The area under the receiver operating characteristics curve [95% confidence interval (CI)] was 0.97 (95% CI=0.947–0.996) for GDS-15 (p<0.001). The Cronbach alpha coefficient for the total scale was 0.920.
CONCLUSION:
GDS-15, just as GDS-30, is a beneficial scale in determining depression in older adults. This study provides an evidence for the validity and reliability of GDS-15 in Turkish elderly population and primary care centers.
Keywords: Depression, DSM-5, GDS-15, geriatrics, Turkey
Depression is a serious health problem in older adults. Although depression is seen in all age groups, geriatric depression may be associated with devastating outcomes such as falls, sleep disorders, cognitive deficiency, malnutrition, self-neglect, and increased risk of morbidity and mortality. Moreover, depression in advanced ages might be the initial sign of other diseases [1]. Therefore, early diagnosis and treatment of depression is important for geriatric practice. However, it is difficult to diagnose geriatric depression because the affective symptoms are uncommon in elderly compared with adults and children, the disease may frequently present itself with cognitive or somatic symptoms, or the clinicians may usually attribute the symptoms to senility or existing comorbidities [2, 3]. Therefore, screening for geriatric depression is important in clinical practice, and screening tools that would enable rapid and reliable detection of depression in older adults are needed.
For this purpose, the initial form of Geriatric Depression Scale (GDS) comprising 30 items was developed by Yesavage JA et al. [4] in 1983, and it was validated for Turkish older adults by Ertan et al. [5]. However, GDS-30 is a time-consuming screening tool for both clinicians and patients. The short form of GDS comprising 15 items (GDS-15), which is effective for the diagnosis of depression in elderly, is more simple, brief, and time-effective than GDS-30. Because of these characteristics, GDS-15 has been validated and is being widely used in many different populations all over the world. America, China, Israel, Greece, United Kingdom, Lebanon, and Brazil are some of the countries where the short form of the scale has been validated [6–12]. The present study aimed to validate GDS-15 and make it available for Turkish older adults.
MATERIALS AND METHODS
Procedure
The study comprised the patients aged ≥65 years who visited a geriatric outpatient clinic of a university hospital between November 2015 and May 2016 for any reason. In the first step, the patients underwent the Mini-Mental State Examination (MMSE) and Cognitive State Test (COST) [13]. After assessing whether the patients meet the DSM-5 diagnostic criteria for depression, another researcher applied the long form of GDS. Sorting the items of the short form out of the long one, two separate scores were obtained. Any translation procedure was not considered necessary during the validation phase as the validation of the long form was done in 1997 by Ertan et al., and the items of short form were sorted out of the long form using exactly the same structures of items.
The protocol for this study was approved by the local Ethics Committee. All participants signed informed consent forms.
Participants
Patients who had cognitive deficiency (Alzheimer disease, frontotemporal dementia, Lewy body dementia, and so on), delirium, or psychotic disorder; have had acute disease within the last two weeks (those with the history of serious disease that impairs general health status such as acute coronary syndrome, acute cerebrovascular accident, and gastrointestinal hemorrhage or staying in the intensive care unit); have been using drugs likely to influence emotional state such as benzodiazepine and antipsychotics; and who were alcohol and substance addicts were excluded. Finally, 329 patients meeting the criteria were enrolled.
Measures
The Geriatric Depression Scale (GDS-30) was developed in 1983 by Yesavage JA et al. [3]. The primary target of this scale, which consists of self-reported 30 questions, is to contain easy-to- answer questions for elderly. While scoring this scale comprising questions with only “yes” or “no” as answers, 1 point is given to each answer that suggest depression and 0 is given for the other answers, and final score is considered as the depression score. The sensitivity and specificity of this initial form consisting of 30 questions were found to be 80% and 100%, respectively, when the cutoff value was taken as 14. A cutoff value of 0–11 was defined as the absence of depression, 11–14 as “probable depression,” and ≥14 as “definite depression” [5].
Geriatric Depression Scale-Short Form (GDS-15): The validity and reliability of this 15-question short form was performed in 1991 by Burke et al. for ease of use [14]. The GDS-15, which was used in the present study, consists of 15 questions inquiring the patient’s mood. Answers are given based on the feelings in the last week; answers are in the form of “yes” or “no” just as in the long form, and 1 point is given either to the answer “yes” or to the answer “no” depending on the question.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) 17.0 as well as Power Analysis and Sample Size (PASS) 2008 Statistical Software (NCSS, Kaysville, UT). Demographic characteristics of participants were analyzed using descriptive statistics. The Kappa consistency test was used to evaluate the consistency between Diagnostic and Statistical Manual of Mental Disorders-fifth edition (DSM-5) criteria and the items of GDS-15. The cutoff scores were assessed by the receiver operating characteristics (ROC) curve. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for different cutoff scores. In all analyses, P<0.05 was considered to indicate statistical significance. A sample size of 153 participants was calculated to ensure that the minimum required size was within a 95% confidence interval (CI) and 5% of the true proportion.
RESULTS
In the present study, a total of 329 participants were evaluated. The mean age was 74.4 years, and 61.4% was female. The characteristics and comorbidities of the participants are demonstrated in Table 1.
TABLE 1.
Characteristics of the participants (n=329)
| Characterictics | Value |
|---|---|
| Age - Mean, (SD) | 74.4 (8.5) |
| Sex % | |
| Female | 61.4 |
| Male | 38.6 |
| Level of education % | |
| <8 years | 61.1 |
| >8 years | 38.9 |
| Marital status % | |
| Married | 55.9 |
| Widowed | 39.2 |
| Unmarried | 3.9 |
| Comorbidities % | |
| Hypertension | 68.4 |
| Hyperlipidemia | 21.0 |
| Coronary artery disease | 20.4 |
| Congestive heart failure | 4.9 |
| Hypothyroidism | 18.2 |
| Chronic obstructive pulmonary disease | 7.0 |
| Having hearing difficult | 9.7 |
| Cataract | 18.2 |
| Hypertension | 68.4 |
| Hyperlipidemia | 21.0 |
The mean score (SD) was 8.21 (7.3) for GDS-30 and 3.21 (3.5) for GDS-15; the mean score of MMSE was 26.6 (2.3). The correlation of GDS-30 (Pearson) with GDS-15 was r=0.966 (p<0.001). Patients with and without depression based on the DSM-5 criteria, GDS-15, and GDS-30 are demonstrated in Table 2. The prevalence of major depression was 24.6% according to DSM-5. Kappa analyses performed for the consistency between the items of DSM-5 and GDS-15 are demonstrated in Table 3. Accordingly, the items 7, 3, and 5 of GDS-15 make the highest contribution to the measuring tool. The Cronbach alpha coefficient for the total scale was 0.920.
TABLE 2.
Comparisons of the YGDS-15 and YGDS-30 with DSM-5
| Depression | YGDS-15 | YGDS-30 | DSM-5 |
|---|---|---|---|
| No, % | 70.8 | 72.2 | 75.4 |
| Depression, % | 29.2 | 27.8 | 24.6 |
YGDS-15: Yesavage Geriatric Depression Scale 15 item; YGDS-30: Yesavage Geriatric Depression Scale 30 item; n: number of patients
TABLE 3.
The Kappa values for each items of Geriatric Depression Scale-15
| Item | Kappa | |
|---|---|---|
| 1. | Are you basically satisfied with your life? | 0.446* |
| 2. | Have you dropped many of your activities and interest? | 0.564* |
| 3. | Do you feel that your life is empty? | 0.580* |
| 4. | Do you often get bored? | 0.508* |
| 5. | Are you in good spirits most of the time? | 0.572* |
| 6. | Are you afraid that something bad is going to happen to you? | 0.224* |
| 7. | Do you feel happy most of the time? | 0.631* |
| 8. | Do you often feel helpless? | 0.504* |
| 9. | Do you prefer to stay at home, rather than going out and doing new thing? | 0.334* |
| 10. | Do you feel you have more problems with memory than most? | 0.215* |
| 11. | Do you think it is wonderful to be alive now? | 0.244* |
| 12. | Do you feel pretty worthless the way you are now? | 0.539* |
| 13. | Do you feel full of energy? | 0.495* |
| 14. | Do you feel that your situation is hopeless? | 0.482* |
| 15. | Do you think that most people are beter off than you are? | 0.434* |
p<0.001.
ROC analysis for GDS-15 revealed an optimal balance of sensitivity and specificity in distinguishing the patients with depression from those without depression at a cutoff value of 5 points with AUC of 0.971 (95% CI=0.947–0.996), P<0.001 (Fig. 1) and with a sensitivity and specificity of 92% and 91%, respectively (Table 4). The cutoff values show no variation according to the education level and existing comorbidities (Charlson Comorbidity Index) of the participants. The sensitivity, specificity, and PPV and NPV of GDS-15 are presented in Table 4.
Figure 1.
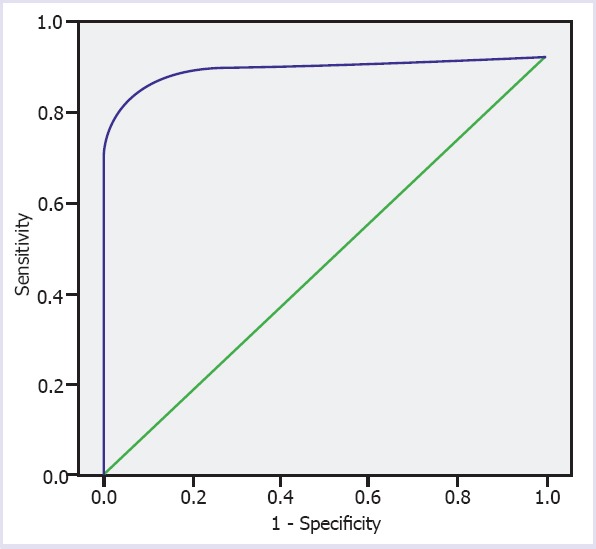
ROC analysis for GDS-15 Receiver operating characteristic curve (ROC) analysis of the YGDS-15 total scores to detect depression (AUC=0.971, p<0.001).
TABLE 4.
Discriminant validity of the YGDS-15 for depression
| Cut-off value | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|
| 4 | 96 | 84 | 64 | 99 |
| 5 | 92 | 91 | 76 | 97 |
| 6 | 87 | 97 | 91 | 95 |
| 7 | 87 | 99 | 100 | 91 |
PPV: Positivepredictivevalue; NPV: Negativepredictivevalue.
DISCUSSION
The present study demonstrated that GDS-15 is a valid and reliable screening tool for depression in elderly Turkish outpatients without cognitive impairment and shows strong correlation with DSM-5 criteria in patients with depression.
Similar to the earlier studies, the present study determined significantly high correlation between GDS-15 and GDS-30 and DSM-5 in distinguishing the patients with depression [15–17]. When the cutoff value is taken as ≥5, the sensitivity, specificity, PPV, and NPV of GDS-15, Turkish version, are 92%, 91%, 76%, and 97%, respectively, in successfully distinguished the patients with depression from others. These results are consistent with the cutoff values found in the earlier studies from various countries, which have been performed for the validation of the short form; however, the present study used the same cutoff value with a validation study conducted in the United Kingdom (sensitivity=80%, specificity=77%) [10] and a study conducted in the United States in patients receiving homecare (sensitivity=71.8%, specificity=78.2%) [18]. Contrarily, the cutoff value was 3 (sensitivity=84%, specificity=64%) in a validation study conducted in Puerto Rico in patients aged ≥50 years [19], and it was 6 (sensitivity=81% specificity=75%) in a study from New York [20]. In addition, the present study demonstrated that the cutoff value does not change depending on education and comorbidity in older adults, which may be an advantage while using GDS-15. GDS-15 has several advantages, such as reduced respondent burden, shorter administration time, and less staff time required to help complete the scale over the more widely used GDS-30 or similar longer scales. GDS-15 can be used conveniently instead of GDS-30. These advantages may be important for outpatients as well as for frail and dependent nursing home residents and may enhance working capacity of health professionals.
The prevalence of geriatric depression was reported to be 4.5%–37.4% among patients aged ≥65 years [21, 22]; likewise, the prevalence was demonstrated as 24.6% in the study. Therefore, validated GDS-15 may be quite helpful for our geriatric practice.
The strength of the present study is the larger sample size than the other studies as well as the fact that diagnosis of depression has been made based on the DSM-5 diagnostic criteria. The major limitation is the study group’s consisting of patients of a single outpatient clinic. Accordingly, it is partially representative of the whole population. Enrolling only the cognitively normal older subjects is another limitation, since many elderly people are cognitively impaired. However, it would be extremely important to assess the effectiveness of GDS-15 in such patients, who as well are usually depressed.
CONCLUSION
In conclusion, GDS-15 is a valid and reliable screening tool for geriatric depression and is highly correlated with GDS-30 and DSM-5. It could be used for rapid and reliable detection of depression in elderly Turkish older adults, particularly in primary care.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship contributions: Concept – A.T.I.; Design – A.T.I., P.S.; Supervision – P.S., A.T.I.; Materials – P.S., B.D.; Data collection &/or processing – B.D., P.S.; Analysis and/or interpretation – H.E., P.S., A.T.I.; Writing – P.S., B.D., A.T.I.; Critical review – P.S., A.T.I.
REFERENCES
- 1.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–65. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 2.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004;57:297–305. doi: 10.1016/j.jpsychores.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 5.Ertan T, Eker E, Şar V. Geriatrik depresyon ölçeğinin. Türk yaşlınüfusunda geçerlilik ve güvenilirliği. Nöropsikiyatri Arşivi. 1997;34:62–71. [Google Scholar]
- 6.Chiang KS, Green KE, Cox EO. Rasch Analysis of the Geriatric Depression Scale-Short Form. Gerontologist. 2009;49:262–75. doi: 10.1093/geront/gnp018. [DOI] [PubMed] [Google Scholar]
- 7.Wong MT, Ho TP, Ho MY, Yu CS, Wong YH, Lee SY. Development and inter-rater reliability of a standardized verbal instruction manual for the Chinese Geriatric Depression Scale-short form. Int J Geriatr Psychiatry. 2002;17:459–63. doi: 10.1002/gps.633. [DOI] [PubMed] [Google Scholar]
- 8.Zalsman G, Aizenberg MD, Sigler MD, Nahshoni E, Weizman MD. Geriatric Depression Scale-Short Form–Validity and Reliability of the Hebrew Version. Clin Gerontol. 1998;18:3–9. [Google Scholar]
- 9.Fountoulakis KN, Tsolaki M, Iacovides A, Yesavage J, O'Hara R, Kazis A, et al. The validation of the short form of the Geriatric Depression Scale (GDS) in Greece. Aging (Milano) 1999;11:367–72. doi: 10.1007/BF03339814. [DOI] [PubMed] [Google Scholar]
- 10.Shah A, Phongsathorn V, Bielawska C, Katona C. Screening for depression among geriatric inpatients with short versions of the geriatric depression scale. Int J Geriatr Psychiatry. 1996;11:915–8. [Google Scholar]
- 11.Chaaya M, Sibai AM, Roueiheb ZE, Chemaitelly H, Chahine LM, Al-Amin H, et al. Validation of the Arabic version of the short Geriatric Depression Scale (GDS-15) Int Psychogeriatr. 2008;20:571–81. doi: 10.1017/S1041610208006741. [DOI] [PubMed] [Google Scholar]
- 12.Castelo MS, Coelho-Filho JM, Carvalho AF, Lima JW, Noleto JC, Ribeiro KG, et al. Validity of the Brazilian version of the Geriatric Depression Scale (GDS) among primary care patients. Int Psychogeriatr. 2010;22:109–13. doi: 10.1017/S1041610209991219. [DOI] [PubMed] [Google Scholar]
- 13.Babacan-Yildiz G, Isik AT, Ur E, Aydemir E, Ertas C, Cebi M, et al. COST: Cognitive State Test, a brief screening battery for Alzheimer disease in illiterate and literate patients. Int Psychogeriatr. 2013;25:403–12. doi: 10.1017/S1041610212001780. [DOI] [PubMed] [Google Scholar]
- 14.Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol. 1991;4:173–8. doi: 10.1177/089198879100400310. [DOI] [PubMed] [Google Scholar]
- 15.Yesavage JA, Sheikh JI. 9/Geriatric Depression Scale (GDS) Recent evidence and development of a shorter. Clinical Gerontologist. 1986;5:165–73. [Google Scholar]
- 16.Alden D, Austin C, Studeon R. A correlation between the Geriatric Depression Scale long and short forms. J Gerontol. 1989;44:124–5. doi: 10.1093/geronj/44.4.p124. [DOI] [PubMed] [Google Scholar]
- 17.Lesher EL, Berryhill JS. Validation of the Geriatric Depression Scale-Short Form among inpatients. J Clin Psychol. 1994;50:256–60. doi: 10.1002/1097-4679(199403)50:2<256::aid-jclp2270500218>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 18.Marc LG, Raue PJ, Bruce ML. Screening performance of the 15-item geriatric depression scale in a diverse elderly home care population. Am J Geriatr Psychiatry. 2008;16:914–21. doi: 10.1097/JGP.0b013e318186bd67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robison J, Gruman C, Gaztambide S, Blank K. Screening for depression in middle-aged and older puerto rican primary care patients. J Gerontol A Biol Sci Med Sci. 2002;57:M308–14. doi: 10.1093/gerona/57.5.m308. [DOI] [PubMed] [Google Scholar]
- 20.Friedman B, Heisel MJ, Delavan RL. Psychometric properties of the 15-item geriatric depression scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. J Am Geriatr Soc. 2005;53:1570–6. doi: 10.1111/j.1532-5415.2005.53461.x. [DOI] [PubMed] [Google Scholar]
- 21.Luppa M, Sikorski C, Luck T, Ehreke L, Konnopka A, Wiese B, et al. Age- and gender-specific prevalence of depression in latest-life--systematic review and meta-analysis. J Affect Disord. 2012;136:212–21. doi: 10.1016/j.jad.2010.11.033. [DOI] [PubMed] [Google Scholar]
- 22.Soysal P, Isik AT, Usarel C, Kaya D, Ellidokuz H, Grossberg GT. Validity and reliability of “AM SAD”, a short geriatric depression screening tool, in Turkish elderly people. Bulletin of Clinical Psychopharmacology. 2016;26:175–80. [Google Scholar]


