Abstract
Context:
Adolescence is a period of turmoil, leading to several mental health challenges including anxiety and/or depression.
Aims:
To study the prevalence of depression and anxiety among higher school going adolescents and their sociodemographic correlates.
Settings and Design:
This cross-sectional study included 201 schoolgoing adolescents.
Subjects and Methods:
Depression and anxiety were measured using Beck Depression Inventory and Screen for Child Anxiety Related Disorders.
Statistical Analysis Used:
Chi-square test and binary logistic Regression with Hosmer–Lemeshow goodness-of-fit model.
Results:
Overall, 82 (40.8%) showed depression (from mild mood disturbance to severe and extreme depression). Among females, it was 49.3% (vs. 35.9% among males, odds ratio [OR] 2.00; 95% confidence interval [CI]: 1.02–03.97, P = 0.046). Overall, 110 (54.7%) participants had one or the other type of anxiety. Depression among the participants having one or other type of anxiety was 60% (vs. 17.6% without anxiety, OR 7.34; 95% CI: 3.68–14.64, P < 0.0001).
Conclusions:
Depression and anxiety were high among the study participants. Co-existing anxiety and female gender are significantly associated with depression among them. Increasing age, socioeconomic factors, and parental education are other factors influencing depression and anxiety but were statistically not significant.
Keywords: Adolescent, anxiety, depression, mood disturbance, panic disorder, school
INTRODUCTION
Adolescence is an important period of transition in human life. Due to various physical, hormonal, and behavioral changes during this period, it becomes a starting point to many mental health issues including depression and anxiety.[1,2] Furthermore, they can co-exist in an adolescent. Adolescent prevalence rates for mood disorders are estimated to be around 10%, and rates for any anxiety disorders are 24.9%.[1] Anxiety disorders represent one of the most common problems in child and adolescent psychiatry at present time. Globally, as per the 2015 estimates, the level of anxiety disorder in the population was 3.6%.[3] It was more common among females (4.6%) than males (2.6%).[3]
Adolescent depression is a mental and emotional disorder.[2,4] The symptoms include negative and anti-social behaviors, irritability, restlessness, bad mood, aggressiveness, desire or attempts to run away, feelings of not being accepted, lack of cooperation with the family, isolation, carelessness with personal hygiene and self-care, hypersensitivity with social withdrawal, sadness, anhedonia, and typical cognitions (self-blame, deteriorated self-image, and decrease in self-esteem). In addition, they can get involved in many anti-social behaviors such as drug and substance abuse and stealing. They can occasionally get suicide tendencies.[4]
Anxiety disorders among adolescents have been classified into four main types: separation anxiety disorder, generalized anxiety disorder, social phobia, and panic disorder. Separation anxiety disorder is characterized by excessive anxiety focused on fear of separation from attachment figures (parents, grandparents, or other caregivers) and/or the home.[1,4] Generalized anxiety disorder presents as excessive worry across a variety of areas. Social phobia constitutes of anxiety that occurs when the individual is in social or performance situations involving exposure to unfamiliar people or possible scrutiny by others.[4] Panic disorder is discrete, recurrent, uncued episodes of panic associated with at least four of 13 somatic and cognitive symptoms. Therefore, these children require more careful and vigilant observation by their parents.[1,3,4]
Overall, both these conditions are associated with poor quality of life at the adolescent age group and also with significant negative consequences.[1] Also, these can be detected during the early stages if the parents suspect the features of anxiety and depression and treated effectively. If region specific data are available, it will enable to launch and sustain programs to screen and treat such conditions in respective areas. However, there are limited studies done among adolescents in this regard. This study was carried out to assess the prevalence of depression and anxiety disorders among adolescents from higher secondary school students and their socio demographic correlates; along with relationship between anxiety and depression.
SUBJECTS AND METHODS
This cross-sectional study was conducted among the adolescent students of two select pre Graduation Institutes (with High School and Science pre-University courses) in the city of Mangaluru, in South India, between July and September 2014. Individuals in the age group of 10–19 years are considered as adolescents.[5] However, for the purpose of this study, adolescents aged 15 years and above were included. The sample size was calculated with anticipated level of depression among adolescents as 38%,[6] 20% relative precision, 95% confidence interval and adding 10% nonresponse error as 201. Approval was obtained from the Institutional Ethics Committee of the Institute in which this study was carried out and necessary permissions were taken from the authorities of the two study schools and colleges each, which were selected using convenient (non-random) sampling technique. The colleges were visited on a preinformed date and the eligible students (aged above 15 years and less than 19 years) were included in the study using purposive sampling. The selected students (110 each from both the selected colleges) were explained about the objectives of the study, assured of confidentiality, and a written informed assent was obtained from each one of them. Also, each study subject was given a parental information sheet and a parental consent form. After obtaining the written informed consent from the parents, data collection was done. The data collection tool included Beck Depression Inventory (BDI-II),[7] and Screen for Child Anxiety Related Disorders.[8] The socioeconomic status was calculated using Modified Kuppuswamy Scale.[9] For analysis purpose, the socioeconomic classes were re-grouped into two as lower middle and below and upper middle and above classes. The subjects were briefed about the study and the questionnaires and invited to fill in the same. Those subjects who were absent on the day of first visit, were contacted again on immediate next working days and those who remained absent at three visits were excluded from the study. The collected data were analyzed using Statistical Package for Social Sciences (SPSS version 11.5 Inc., Chicago, IL, USA). Results were expressed as proportions using appropriate tables. The BDI-II data were categorized as depressed and nondepressed for the analysis. For comparisons across the group, Chi-square test was used. Odds ratios (ORs) were generated (adjusted and unadjusted) using binary logistic regression with Hosmer–Lemeshow goodness-of-fit model and for all comparisons P < 0.05 was considered statistically significant.
RESULTS
Our study included 201 study participants, after approaching 220 eligible adolescents following the consenting process and completion of questionnaire. After excluding those who refused consent and with incomplete responses, the response rate was 91.3%. Study participants' age ranged from 15 to 18 years; mean age being 16.3 years (standard deviation: 0.71). Also, 135 (67.2%) study participants were residing in urban area, 66 (32.8%) were from rural area and 161 (80.1%) of them belonged nuclear family, 24 (11.9%) were from extended and rest belonged to joint family.
Table 1 describes the types and distribution of different types of anxiety wherein 110 (54.7%) were positive for anxiety disorder. As shown in Table 2, 23.9% adolescents had mild mood disturbance, 17.4% of them had borderline depression and 6% had severe depression. When re-categorized the borderline to severe depression as the presence of depression, 82 (40.8%) of the study participants were overall depressed (borderline clinical depression [n = 35], moderate [n = 33], severe [n = 12] and extreme depression [n = 02] combined together).
Table 1.
Distribution of various anxiety disorders in the study population (n=201)
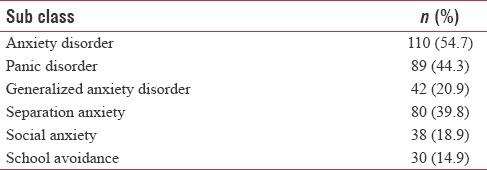
Table 2.
Distribution of Categories of Depression (Beck Depression Inventory-II) in the study population (n=201)
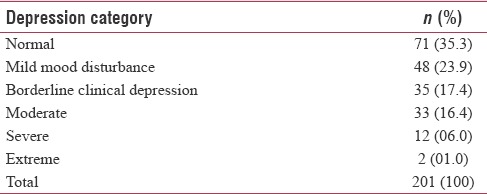
Table 3 describes the univariate analyses of depression and anxiety with the sociodemographic factors among the study participants. The level of depression was higher among females, those aged 17–18 years, participants belonging to low middle and below socioeconomic status and those belonging to nonnuclear type of families. These differences were not found to be statistically significant. The level of depression among the participants having anxiety was 60%, as compared to 17.6% among without the anxiety. This difference was found to be statistically significant (P < 0.0001).
Table 3.
Univariate analysis of depression and Anxiety with associated factors in the study population (n=201)
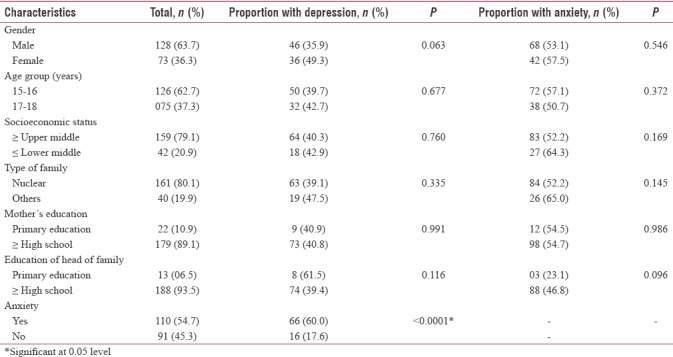
Higher levels of anxiety were seen among females, participants aged 15–16 years, those with mothers' education higher than high school, subjects living in nonnuclear type of families and those belonging to lower socioeconomic status, head of the family with education above primary level. These differences were not found to be statistically significant.
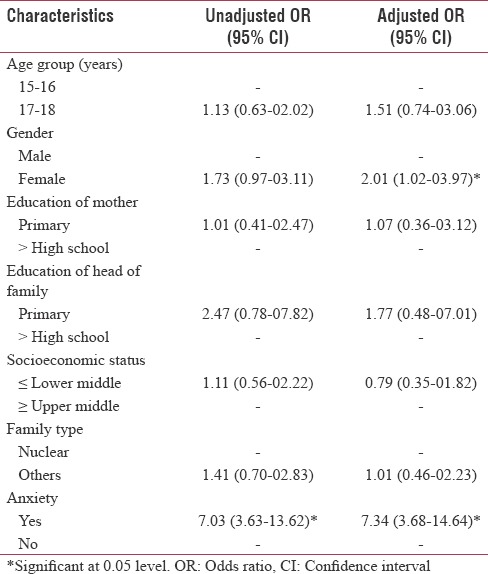
Table 4 depicts the multivariate analyses of the sociodemographic factors and their relationship with depression among the study participants. Females tend to have double the chance of having depression as compared to males (OR: 2.00; 95% confidence interval [CI]: 1.02–03.97). This difference across the gender was found to be statistically significant (P = 0.046). Those subjects with pre-existing anxiety disorder have higher chances of developing or co-existing depression as compared to those without anxiety disorder (OR: 7.34; 95% CI: 3.68–14.64). This association between anxiety and depression was found to be statistically significant (P < 0.001). Higher age group, mothers' education status up to primary level family head with education up to primary education had higher and those in low socioeconomic status had lower chances of having depression; however, these associations were not statistically significant.
Table 4.
Binary logistic regression analysis of factors related to depression in the study population (n=201)
DISCUSSION
Adolescent depression and anxiety are the two common conditions which interfere with the complete growth and development of an individual. Child and adolescent depressive disorders is associated with a range of adverse outcomes including social and educational impairments as well as both physical and mental health problems later in life.[9] Overall, our study showed 40.7% depression with higher level among females. This was similar to the findings of previous studies by Angold et al.[10] and Thapar et al.[11] which also reported that depression was higher among females which attributed to factors such as hormonal changes and exposure to stress. This is important because, the adolescents having high rate of depression would find it difficult to cope up with future life. This may also be associated with adverse outcomes, in addition to decreased educational and work place outputs.
Also, suicidal thoughts were observed in 9% of the subjects in our study. This was lower as compared to a previous study by Strandheim et al.,[12] who in their prospective cohort study, noted baseline suicidal thoughts (boys – 14.2% and girls – 19.5%) and on follow up showed overall 17% suicidal thoughts.
Overall, in our study, 54.7% had anxiety and females had higher levels than males. This difference in line with the previous studies: Study by Kathleen et al. in 2010 from the United States of America[6] reported that 31.9% had anxiety disorder and it was more common in females. Another study from India by Srinivasa et al. reported 37% of anxiety among students of pregraduation colleges and females had higher levels of all types of anxiety.[13] In our study, lower education level of parents was associated with higher levels of depression and anxiety among the adolescents. Kathleen et al.[6] and Srinivasa et al.[13] also reported that adolescents whose parents with lower education levels were at increased risk for all psychiatric disorders. Subjects whose family head educated up to graduate/postgraduate and professional level were more stable and had less anxiety. In the present study there was no association found between depression and type of family to which the subject belonged. However, there was higher level of anxiety in the subjects from joint family compared to those belonged to nuclear family. Present study showed that 44.3% adolescents were screened positive for panic disorder, 20.9% subjects had generalized anxiety disorder (GAD). Separation anxiety was observed in 39.8% subjects. Social anxiety disorder was seen in 18.9% and 14.9% had significant school avoidance. As per study by Kathleen et al. in 2010[6] showed 54.5% prevalence of GAD and social anxiety disorder was 7.9%. Also, 4.9% of the study subjects had significant school avoidance. Present study showed that panic disorder (45.2%) and separation anxiety (41.1%) was more common in females. Social anxiety (19.5%) and school avoidance (15.6%) was more common in males. GAD was more in subjects whose mothers had lower education level. A study by Srinivasa and Chaithanya also showed that adolescents whose parents were illiterate had more anxiety, 76% belonged to nuclear family, and 89% were from rural areas.[13] A systematic review by Stirling et al. reported the multifactorial association and co-existence of several family and environmental factors.[14]
Hence it is evident that the levels of adolescent depression are high, it is associated with female gender and presence anxiety, whereas other influencing factors being increasing age, low socio economic status, lesser education of the mothers and family heads and nonnuclear type of families. Also the level of anxiety itself was high among the adolescents. This calls for early detection and interventions so that these adolescents are enabled to cope up with next phases of life, without having to go through complications. However according to a systematic review by Roseman et al., there is no major benefit of screening for depression among adolescents, which will have to be undertaken after weighing the benefits and harm specific to a particular population and geo-cultural situation.[15]
CONCLUSIONS
Depression and anxiety levels were high among the study participants. Depression was significantly higher among those with co-existing anxiety and female participants. Other factors associated with depression and also with anxiety were lower socioeconomic status, nonnuclear families, higher age group and education of the mothers and head of the family being till primary level. This calls for an early need of interventions and policies at the Institutional levels to address adolescent depression and anxiety.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Authors express their gratitude to Child Development Centre, Government Medical College, Thiruvananthapuram and School of Distance education, Kerala University for partnering in this study at various stages. Also gratitude to Kasturba Medical College (Manipal Academy of Higher Education), Mangaluru for all the support throughout the study, School Authorities and all the participants of this study.
REFERENCES
- 1.Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, et al. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2012;69:372–80. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry. 2011;52:1015–25. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Estimates of Anxiety and Mental Disorders. [Last accessed on 2018 Aug 08]. Available from: http://www.apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf .
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. DSM-5. Washington, DC: American Psychiatric Publishing; 2013. [Last accessed on 2018 Apr 03]. Available from: https://www.psychiatry.org/psychiatrists/practice/dsm . [Google Scholar]
- 5.Age Group Included in Adolescent Age Group. [Last accessed on 2018 Jun 30]. Available from: http://www.who.int/topics/adolescent_health/en/
- 6.Kathleen RM, Jian-ping H, Marcy B, Sonja AS, Shelli A, Lihong C, et al. Lifetime prevalence of mental disorders in US adolescents: Results from the national comorbidity study-adolescent supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AT Beck, RA Steer, GK Brown. Beck Depression Inventory-II (bdi-ii) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 8.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M, et al. Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–6. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Singh T, Sharma S, Nagesh S. Socio-economic status scales updated for 2017. Int J Res Med Sci. 2017;5:3264–7. [Google Scholar]
- 10.Angold A, Costello EJ, Erkanli A, Worthman CM. Pubertal changes in hormone levels and depression in girls. Psychol Med. 1999;29:1043–53. doi: 10.1017/s0033291799008946. [DOI] [PubMed] [Google Scholar]
- 11.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379:1056–67. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strandheim A, Bjerkeset O, Gunnell D, Bjørnelv S, Holmen TL, Bentzen N, et al. Risk factors for suicidal thoughts in adolescence – A prospective cohort study: The young-HUNT study. BMJ Open. 2014;4:e005867. doi: 10.1136/bmjopen-2014-005867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Srinivasa S, Chaithanya C. Nair, Ravindra LS. A study on prevalence of anxiety disorders among higher secondary school students. J Evolution Med Dent Sci. 2015;4:4473–8. [Google Scholar]
- 14.Stirling K, Toumbourou JW, Rowland B. Community factors influencing child and adolescent depression: A systematic review and meta-analysis. Aust N Z J Psychiatry. 2015;49:869–86. doi: 10.1177/0004867415603129. [DOI] [PubMed] [Google Scholar]
- 15.Roseman M, Saadat N, Riehm KE, Kloda LA, Boruff J, Ickowicz A, et al. Depression screening and health outcomes in children and adolescents: A Systematic review. Can J Psychiatry. 2017;62:813–7. doi: 10.1177/0706743717727243. [DOI] [PMC free article] [PubMed] [Google Scholar]


